Abstract
Background
It is unclear whether statin agents provide clinical benefit in preventing the relapse of atrial fibrillation (AF) after electrical cardioversion (EC). The purpose of this study was to assess the effect of statin agents on the recurrence of AF after EC by conducting a meta-analysis of randomized controlled trials (RCTs).
Material/Methods
We conducted a systematic literature search of Medline, EMBASE, ISI Web of Science, and Cochrane databases. RCTs comparing clinical endpoint of the recurrence of AF associated with statin administration vs. no statin treatment (placebo or conventional medical therapy) in patients with AF after EC were eligible. Combined results are presented as risk ratios (RRs) with 95% confidence intervals (CIs).
Results
A total of 5 trials with 524 patients were available for analysis. The pooling analysis showed that statin agents significantly reduced the recurrence of AF after EC compared with no statin treatment (RR=0.76, 95% CI 0.63–0.92; p=0.004; I2=44%). The beneficial effect was shown both in AF subjects receiving atorvastatin or rosuvastatin treatment (atorvastatin 80 mg: RR=0.82, p=0.05; atorvastatin 10 mg: RR=0.27, p=0.03; rosuvastatin: RR=0.38, p=0.04) and in younger patients (<65 years; RR=0.58, p=0.0005). Furthermore, the benefit of statin agents on preventing AF recurrence after EC was demonstrated within 3-month follow-up (p=0.03), and the clinical benefit seemed likely to remain until no less than 12 months after EC (p=0.05).
Conclusions
Based on the currently available data, administration of statin agents, especially atorvastatin or rosuvastatin, is beneficial in lowering the frequency of AF recurrence after EC.
MeSH Keywords: Atrial Fibrillation, Electric Countershock, Hydroxymethylglutaryl-CoA Reductase Inhibitors
Background
Atrial fibrillation (AF) is the most common cardiac arrhythmia and is associated with increased morbidity and mortality [1]. It is important to identify appropriate management to prevent AF recurrence and improve these patients’ clinical prognosis. Electrical cardioversion (EC) is commonly used to restore sinus rhythm in patients with AF [2]. The restoration and maintenance of sinus rhythm might prevent electrical and structural remodeling of the atria as well as improve hemodynamic function and quality life [3]. However, among these AF settings successfully receiving EC, about 25% will experience an AF relapse within 1 week after EC [4]. Currently available antiarrhythmic agents have limited efficacy in preventing AF recurrence, and the benefit appears to be offset by their proarrhythmic adverse effects. Thus, there is a growing interest to the “upstream” therapy of AF, such as hydroxymethylglutaryl-CoA reductase inhibitor (statins) [5]. Statins exert diverse cholesterol-independent effects throughout the cardiovascular system, encompassing enhancement of nitric oxide synthesis, improvement of endothelial function, inhibition of inflammatory cytokines, and restoration of impaired autonomic function, which are believed to contribute to the pathogenesis of AF [6–8]. Several relevant meta-analyses have evaluated the relationship between statin therapy and AF recurrence in patients with AF, but they provide conflicting results. Furthermore, they did not specifically investigate the effect of statins on reducing AF recurrence after EC [9–11]. Therefore, we performed a meta-analysis of the available data from RCTs to detect the efficacy of statins in preventing the recurrence of AF in patients with AF successfully undergoing EC.
Material and Methods
Search Strategy
To identify the eligible studies, we systematically searched Medline, EMBASE, ISI Web of Science, and Cochrane databases through Oct 2013 using the search terms statin, HMG-CoA reductase inhibitors, atrial fibrillation, cardioversion, randomized, and human. Searches were restricted to English-language literature. In addition, reference lists of all eligible articles and previous systematic reviews were hand-searched for other relevant papers.
Study selection
Studies were considered for eligibility if: (1) they recruited patients with a diagnosis of persistent AF, and successfully receiving EC; (2) the enrolled participants were randomly assigned to receive either statins (statin treatment group) or placebo/no-statin therapy (the control group); and (3) they reported the efficacy endpoint of the recurrence of AF with or without safety outcomes (e.g., all-cause death or adverse effects). Studies were excluded if they were observational studies or post-hoc analyses of RCTs, or if the information on study design (e.g., randomization methods, allocation concealment, description of withdrawals, or intent-to-treat analysis) was unavailable. Two investigators reviewed all studies and citations in duplicate to identify the potentially eligible studies. Disagreements were resolved by consensus.
Data extraction and quality assessment
Two investigators independently assessed study eligibility and quality and extracted the data on study characteristics, patient demographics, the risk factors of AF, therapy strategy, and follow-up duration. Predefined clinical endpoints were also extracted from each of the eligible studies. All eligible studies were assessed for the following quality criteria: randomization methods, blinding, and description of withdrawals and dropouts. The quality of included trials was evaluated with a 5-point Jadad scale [12].
Statistical analysis
The Mantel-Haenszel methods for fixed-effects models were used to investigate the combinations of the individual studies. Combined results are presented as risk ratios (RRs) with their 95% confidence intervals (CIs). To examine the robustness of the effect, sensitivity analyses were performed by omitting each trial 1 at a time from analysis and thereafter computing overall estimates for the remaining studies. Heterogeneity across studies was quantified using the I-squared statistic with a scale of 0–100% (>50% indicated a statistical between-study inconsistency, and >75% represented very large heterogeneity). Data stratified according to mean age, statin class, left atrial diameters (LAD), and follow-up duration were analyzed by subgroup analyses to verify these clinical factors impacting predefined clinical outcomes. We qualitatively assessed publication bias using the funnel plot method. Pooling analyses were performed with RevMan 5.1 software (The Cochrane Collaboration, Copenhagen, Denmark). A P value of <0.05 was considered statistically significant. This work was organized as the guidelines of Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [13]
Results
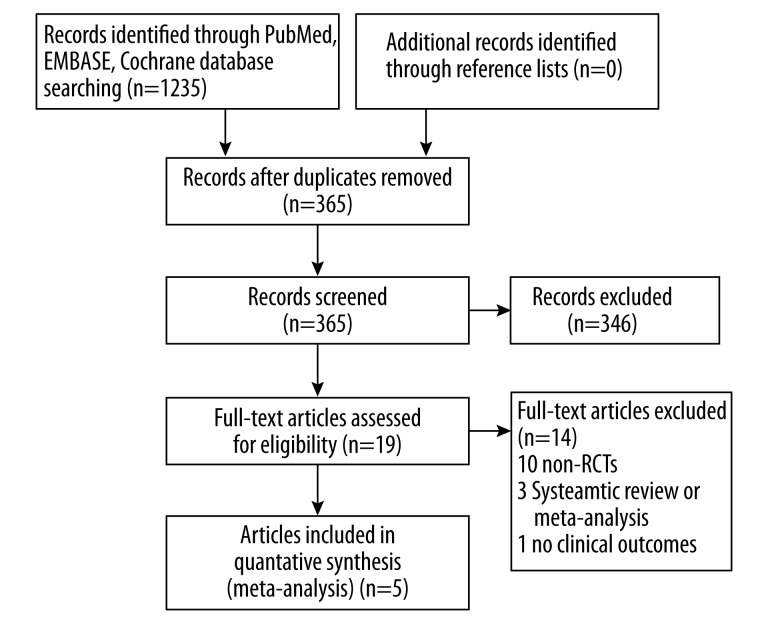
The flow of the selection process for potentially eligible trials and reasons for exclusion are shown in Figure 1. After elaborative screening, 5 studies were eligible for inclusion in the analysis [14–18] and no additional relevant study was identified from the references and citations of the eligible articles.
Figure 1.
Flowchart of selection of studies for inclusion. RCTs – randomized controlled trials.
Study design and baseline characteristics for each of the qualifying trials are shown in Table 1. A total of 524 patients with persistent AF, with the mean follow-up duration ranging from 2 months to 12 months, were included for analysis. All of the AF patients successfully received EC, and the assigned therapy was initiated immediately or 3–6 weeks after randomization and continued throughout the whole follow-up period. Among them, 264 patients were randomly allocated to the statin (atorvastatin, pravastatin, or rosuvastatin) treatment group and 260 to the control group. Left atrial enlargement in the 5 studies had a mean LAD of 41.6–46.1 mm. The level of evidence for each article was graded with a score of 2–5 according to the Jadad quality score (Table 1).
Table 1.
Baseline characteristics of randomized controlled trials included in the meta-analysis.
| Study, year | No. enrolled | Mean age | Men, % | Hypertension, % | Diabetes, % | Mean LVEF,% | Mean left atrial diameter, mm | Statin type | Control group | Mean follow-up duration, months | Jadad score |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Almroth H, 2009 | 234 | 65 | 75 | 47 | 8.5 | NA | 44 | Atorvastatin 80 mg | Placebo | 6 | 5 |
| Ozaydin M, 2006 | 48 | 63 | 60 | 40 | 22.9 | 62 | 45 | Atorvastatin 10 mg | No statin treatment | 3 | 3 |
| Stop AF, 2011 | 64 | 58.5 | 82.9 | 50 | 8 | 48 | 46.1 | Atorvastatin 80 mg | Placebo | 12 | 4 |
| Tveit A, 2004 | 114 | 68 | 77 | 43 | 6.5 | NA | 44 | Pravastatin 40 mg | No statin treatment | 2 | 3 |
| Xia W, 2009 | 64 | 61.5 | 66 | 0 | 0 | 59 | 41.6 | Rosuvastatin 20 mg | No statin treatment | 3 | 2 |
LVEF – left ventricular ejection fraction; NA – not available.
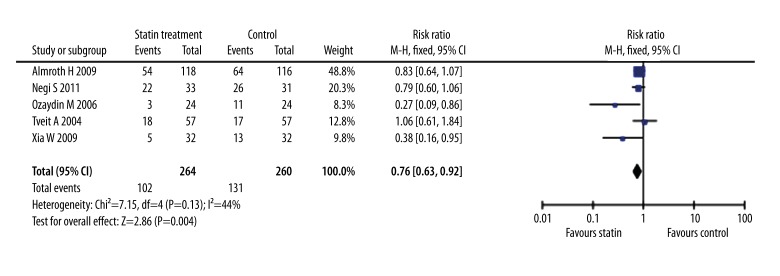
Pooling analyses showed that, compared with the control, statin treatment significantly reduced the recurrence of AF in persistent AF after electrical cardioversion (RR=0.76, 95% CI: 0.63–0.92, p=0.004; I2=44%, Figure 2). When the analysis was restricted to patients over age 65, there was no significant inter-group difference in this clinical endpoint (RR=0.88, p=0.27, Table 2). However, statin therapy was likely to provide a benefit in decreasing the frequency of AF recurrence in patients less than 65 years old (RR=0.58, p=0.0005) and in those with mean LAD of no less than 45 mm (RR=0.64, p=0.006, Table 2). Moreover, administration of atorvastatin regardless of dose as well as rosuvastatin 20 mg daily markedly reduced the incidence of recurrent AF compared with no-statin treatment (atorvastatin 80 mg: RR=0.82, p=0.05; atorvastatin 10 mg: RR=0.27, p=0.03; rosuvastatin 20 mg: RR=0.38, p=0.04, Table 2). In addition, the beneficial effect was similar during 2–3-month follow-up (RR=0.63, p=0.03) and during 6–12-month follow-up (RR=0.82, p=0.05, Table 2). All of the enrolled studies reported the good safety and tolerability of statin treatment, but there were no concrete data available. Thus, pooling analyses of safety endpoint were not performed in this meta-analysis.
Figure 2.
Forest plot of risk ratios of recurrence frequency of AF in patients treated with statin compared with no statin. CI – confidence intervals; MH – Mantel-Haenszel method.
Table 2.
Subgroup analyses based on the data on recurrence of AF.
| Factors | Recurrence of AF | ||
|---|---|---|---|
| No. of studies | RR (95% CI) | P value | |
| Age ≥65 | 2 | 0.88 [0.69, 1.11] | 0.27 |
| Age <65 | 3 | 0.58 [0.42, 0.79] | 0.0005 |
| Atorvastatin 80 mg | 2 | 0.82 [0.67, 1.00] | 0.05 |
| Atorvastatin 10 mg | 1 | 0.27 [0.09, 0.86] | 0.03 |
| Pravastatin 40 mg | 1 | 1.06 [0.61, 1.84] | 0.84 |
| Rosuvastatin 20 mg | 1 | 0.38 [0.16, 0.95] | 0.04 |
| LAD ≥45 mm | 2 | 0.64 [0.47, 0.88] | 0.006 |
| LAD <45 mm | 3 | 0.81 [0.65, 1.02] | 0.07 |
| 2 to 3-month follow-up | 3 | 0.63 [0.42, 0.97] | 0.03 |
| 6 to 12-month follow-up | 2 | 0.82 [0.67, 1.00] | 0.05 |
AF – atrial fibrillation; CI – confidence interval; LAD – left atrial diameter; RR – risk ratio.
Sensitivity analysis by omitting each trial 1 at a time from analysis did not show any relevant influence on the overall results, which further confirmed the findings in direction and magnitude in the present study. Funnel plots were performed and essential symmetry regarding the frequency of recurrent AF was found, suggesting that there was no publication bias in the meta-analysis (Supplementary Material).
Discussion
The present study pooled the available data from RCTs focusing on the relapse of AF associated with statin treatment in patients with persistent AF after EC. The results revealed that statin treatment significantly reduced the recurrence of AF compared with no-statin treatment. Subgroup analyses further showed that the beneficial effect of statin was noted both in AF subjects receiving atorvastatin or rosuvastatin treatment and in the younger patients (<65 years). Furthermore, the benefit of statin agents on preventing AF recurrence after EC was demonstrated within 3-month follow-up, and the clinical benefit seemed likely to remain until no less than 12 months after EC.
The positive effect of statins on reducing cardiovascular morbidity and mortality, which was demonstrated by large clinical trials [19,20], might not be entirely explained by the lipid-lowering effect itself. Alternatively, anti-inflammatory, antiproliferative, and anti-oxidative effects might also play a role [21–23]. Recent studies have demonstrated the possible involvement of inflammation and oxidative stress in the pathogenesis of AF [24], and statins had a potentially positive effect on AF [15,25]. Indeed, treatment with statins significantly reduced the incidence of new-onset AF in primary and secondary prevention [26]. In the condition of AF, patients had increased C-reactive protein (CRP) levels in their blood [27–29] and the blood concentration of CRP seemed likely to be associated with the total amount of time that the patient experienced AF [30]. Statin agents were able to exert anti-inflammatory effect by significantly inhibiting interleukin-6 (IL-6) and tumor necrosis f actor α (TNF-α) production, as well as nuclear factor kappa B (NF-κB) activation [31]. Several studies have indicated that statins might play a role in antiarrhythmic effects through improving endothelial nitric oxide (NO) availability and reducing inflammation, oxidative stress, and neurohormonal activation [32,33].
As in a previous clinical data [34], the present study demonstrated the superior efficacy of statin agents on the recurrence frequency of AF after cardioversion. Moreover, the benefit was more significant, especially in patients receiving atorvastatin or rosuvastatin and in those aged less than 65 years old. However, no relevant studies directly addressing class- or age-related efficacy of statins in preventing AF recurrence after successful EC have been reported to date. The potential mechanism underlying the age-related efficacy of statin remains uncertain. Older patients may not achieve the same improvement in endothelial function and immunomodulation from statin treatment compared with their younger counterparts [6,35]. It could be difficult for older patients to improve clinical outcomes following statin treatment. We therefore needed to further carry out the classification of AF populations to identify the specific patients who could benefit to the greatest extent from statin therapy. In addition, the beneficial effect on statin agents on reducing AF relapse found in the present study was consistent with that observed in a recent meta-analysis [36]. However, of note, there are several differences in methodology between these that meta-analysis and the present study. The previous meta-analysis did not conduct subgroup analyses, sensitivity analyses, and publication bias analyses, which was necessary to confirm the reliability of the conclusions. Also drug-class, age-related, and observation period-related effect of statins were not observed in that study.
Methodologically, no publication bias and relatively low statistical heterogeneities among the included trials might ensure the robustness of conclusions from the current study. Moreover, there were relatively strict criteria for inclusion in the present meta-analysis, by which we excluded a randomized trial [37] due to the absence of concrete information on study design. However, due to the limited number of studies and the sample size, the findings of subgroup analyses were not sufficiently robust. Thus, the subgroup results should be interpreted with caution. Large-scale studies are required to further verify the findings and conclusions of subgroup analyses in the present study. Moreover, the clinical outcomes of all-cause mortality and cardiovascular death were not reported in the present study’s included RCTs. Therefore, the present meta-analysis did not demonstrate the effect of statin agents on the clinical prognosis of AF after EC.
Conclusions
This study evaluated the current evidence from RCTs comparing clinical efficacy of statin vs. no-statin treatment in lowering AF relapse after EC. Compared with no-statin therapy, statin therapy significantly decreased the frequency of AF recurrence after successful EC in patients with persistent AF. Moreover, the use of atorvastatin or rosuvastatin was associated with the lower risk of AF relapse compared with other statin classes, especially in the younger patients.
Publication bias analysis by funnel plot.
Footnotes
Source of support: Self financing
Statement
No sources of funding to be noted. No conflicts of interest to be noted.
References
- 1.Zografos T, Katritsis D. Inhibition of the renin-angiotensin system for prevention of atrial fibrillation. Pacing Clin Electrophysiol. 2010;33:1270–85. doi: 10.1111/j.1540-8159.2010.02832.x. [DOI] [PubMed] [Google Scholar]
- 2.Wann LS, Curtis AB, Ellenbogen KA, et al. 2011 ACCF/AHA/HRS focused update on the management of patients with atrial fibrillation (update on Dabigatran): a report of the American College of Cardiology Foundation/American Heart Task Force on practice guidelines. Circulation. 2011;123:1144–50. doi: 10.1161/CIR.0b013e31820f14c0. [DOI] [PubMed] [Google Scholar]
- 3.Chen S, Dong Y, Fan J, et al. Rate vs. rhythm control in patients with atrial fibrillation – an updated meta-analysis of 10 randomized controlled trials. Int J Cardiol. 2011;153:96–98. doi: 10.1016/j.ijcard.2011.09.009. [DOI] [PubMed] [Google Scholar]
- 4.Taylor J. CardioPulse: A focused update to the ESC guidelines for the management of patients with atrial fibrillation. Eur Heart J. 2012;33:2623–24. doi: 10.1093/eurheartj/ehs319. [DOI] [PubMed] [Google Scholar]
- 5.Savelieva I, Kakouros N, Kourliouros A, et al. Upstream therapies for management of atrial fibrillation: review of clinical evidence and implications for European Society of Cardiology guidelines. Part II: secondary prevention. Europace. 2011;13:610–25. doi: 10.1093/europace/eur023. [DOI] [PubMed] [Google Scholar]
- 6.Zhang S, Zhang L, Sun A, et al. Efficacy of statin therapy in chronic systolic cardiac insufficiency: a meta-analysis. Eur J Intern Med. 2011;22:478–84. doi: 10.1016/j.ejim.2011.06.003. [DOI] [PubMed] [Google Scholar]
- 7.Li J, Solus J, Chen Q, et al. Role of inflammation and oxidative stress in atrial fibrillation. Heart Rhythm. 2010;7:438–44. doi: 10.1016/j.hrthm.2009.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ferro D, Franciosa P, Cangemi R, et al. Serum levels of vitamin E are associated with early recurrence of atrial fibrillation after electric cardioversion. Circ Arrhythm Electrophysiol. 2012;5:327–33. doi: 10.1161/CIRCEP.111.968248. [DOI] [PubMed] [Google Scholar]
- 9.Rahimi K, Emberson J, McGale P, et al. Effect of statins on atrial fibrillation: collaborative meta-analysis of published and unpublished evidence from randomised controlled trials. BMJ. 2011;342:d1250. doi: 10.1136/bmj.d1250. [DOI] [PubMed] [Google Scholar]
- 10.Wang Z, Zhang Y, Gao M, et al. Statin therapy for the prevention of atrial fibrillation: a meta-analysis of randomized controlled trials. Pharmacotherapy. 2011;31:1051–62. doi: 10.1592/phco.31.11.1051. [DOI] [PubMed] [Google Scholar]
- 11.Fauchier L, Pierre B, de Labriolle A, et al. Antiarrhythmic effect of statin therapy and atrial fibrillation a meta-analysis of randomized controlled trials. J Am Coll Cardiol. 2008;51:828–35. doi: 10.1016/j.jacc.2007.09.063. [DOI] [PubMed] [Google Scholar]
- 12.Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17:1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 13.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Almroth H, Hoglund N, Boman K, et al. Atorvastatin and persistent atrial fibrillation following cardioversion: a randomized placebo-controlled multicentre study. Eur Heart J. 2009;30:827–33. doi: 10.1093/eurheartj/ehp006. [DOI] [PubMed] [Google Scholar]
- 15.Ozaydin M, Varol E, Aslan SM, et al. Effect of atorvastatin on the recurrence rates of atrial fibrillation after electrical cardioversion. Am J Cardiol. 2006;97:1490–93. doi: 10.1016/j.amjcard.2005.11.082. [DOI] [PubMed] [Google Scholar]
- 16.Negi S, Shukrullah I, Veledar E, et al. Statin therapy for the prevention of atrial fibrillation trial (SToP AF trial) J Cardiovasc Electrophysiol. 2011;22:414–19. doi: 10.1111/j.1540-8167.2010.01925.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tveit A, Grundtvig M, Gundersen T, et al. Analysis of pravastatin to prevent recurrence of atrial fibrillation after electrical cardioversion. Am J Cardiol. 2004;93:780–82. doi: 10.1016/j.amjcard.2003.12.009. [DOI] [PubMed] [Google Scholar]
- 18.Xia W, Yin Z, Li J, et al. Effects of rosuvastatin on asymmetric dimethylarginine levels and early atrial fibrillation recurrence after electrical cardioversion. Pacing Clin Electrophysiol. 2009;32:1562–66. doi: 10.1111/j.1540-8159.2009.02554.x. [DOI] [PubMed] [Google Scholar]
- 19.LaRosa JC, Grundy SM, Waters DD, et al. Intensive lipid lowering with atorvastatin in patients with stable coronary disease. N Engl J Med. 2005;352:1425–35. doi: 10.1056/NEJMoa050461. [DOI] [PubMed] [Google Scholar]
- 20.Sever PS, Dahlof B, Poulter NR, et al. Prevention of coronary and stroke events with atorvastatin in hypertensive patients who have average or lower-than-average cholesterol concentrations, in the Anglo-Scandinavian Cardiac Outcomes Trial – Lipid Lowering Arm (ASCOT-LLA): a multicentre randomised controlled trial. Lancet. 2003;361:1149–58. doi: 10.1016/S0140-6736(03)12948-0. [DOI] [PubMed] [Google Scholar]
- 21.Kargar M, Hadjibabaie M, Gholami K. Simvastatin versus triptorelin in prevention of pain recurrences after surgery for endometriosis. Med Sci Monit. 2013;19:858. doi: 10.12659/MSM.889682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rymarz E, Matysik-Wozniak A, et al. Lipemia retinalis – an unusual cause of visual acuity deterioration. Med Sci Monit. 2012;18(8):CS72–75. doi: 10.12659/MSM.883257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Almassinokiani F, Mehdizadeh A, Sariri E, et al. Effects of simvastatin in prevention of pain recurrences after surgery for endometriosis. Med Sci Monit. 2013;19:534–39. doi: 10.12659/MSM.883967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Issac TT, Dokainish H, Lakkis NM. Role of inflammation in initiation and perpetuation of atrial fibrillation: a systematic review of the published data. J Am Coll Cardiol. 2007;50:2021–28. doi: 10.1016/j.jacc.2007.06.054. [DOI] [PubMed] [Google Scholar]
- 25.Young-Xu Y, Jabbour S, Goldberg R, et al. Usefulness of statin drugs in protecting against atrial fibrillation in patients with coronary artery disease. Am J Cardiol. 2003;92:1379–83. doi: 10.1016/j.amjcard.2003.08.040. [DOI] [PubMed] [Google Scholar]
- 26.Fauchier L, Clementy N, Babuty D. Statin therapy and atrial fibrillation: systematic review and updated meta-analysis of published randomized controlled trials. Curr Opin Cardiol. 2013;28:7–18. doi: 10.1097/HCO.0b013e32835b0956. [DOI] [PubMed] [Google Scholar]
- 27.Paoletti R, Gotto AM, Jr, Hajjar DP. Inflammation in atherosclerosis and implications for therapy. Circulation. 2004;109:III20–26. doi: 10.1161/01.CIR.0000131514.71167.2e. [DOI] [PubMed] [Google Scholar]
- 28.Chung MK, Martin DO, Sprecher D, et al. C-reactive protein elevation in patients with atrial arrhythmias: inflammatory mechanisms and persistence of atrial fibrillation. Circulation. 2001;104:2886–91. doi: 10.1161/hc4901.101760. [DOI] [PubMed] [Google Scholar]
- 29.Kumagai K, Nakashima H, Saku K. The HMG-CoA reductase inhibitor atorvastatin prevents atrial fibrillation by inhibiting inflammation in a canine sterile pericarditis model. Cardiovasc Res. 2004;62:105–11. doi: 10.1016/j.cardiores.2004.01.018. [DOI] [PubMed] [Google Scholar]
- 30.Yao SY, Chu JM, Chen KP, et al. Inflammation in lone atrial fibrillation. Clin Cardiol. 2009;32:94–98. doi: 10.1002/clc.20290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nordmann AJ, Briel M. Statins: pleiotropic, but less than previously thought. Eur Heart J. 2012;33:1551–52. doi: 10.1093/eurheartj/ehs027. [DOI] [PubMed] [Google Scholar]
- 32.Adam O, Neuberger HR, Bohm M, et al. Prevention of atrial fibrillation with 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitors. Circulation. 2008;118:1285–93. doi: 10.1161/CIRCULATIONAHA.107.760892. [DOI] [PubMed] [Google Scholar]
- 33.Reilly SN, Jayaram R, Nahar K, et al. Atrial sources of reactive oxygen species vary with the duration and substrate of atrial fibrillation: implications for the antiarrhythmic effect of statins. Circulation. 2011;124:1107–17. doi: 10.1161/CIRCULATIONAHA.111.029223. [DOI] [PubMed] [Google Scholar]
- 34.Siu CW, Lau CP, Tse HF. Prevention of atrial fibrillation recurrence by statin therapy in patients with lone atrial fibrillation after successful cardioversion. Am J Cardiol. 2003;92:1343–45. doi: 10.1016/j.amjcard.2003.08.023. [DOI] [PubMed] [Google Scholar]
- 35.Tang WH, Francis GS. Statin treatment for patients with heart failure. Nat Rev Cardiol. 2010;7:249–55. doi: 10.1038/nrcardio.2010.29. [DOI] [PubMed] [Google Scholar]
- 36.Loffredo L, Angelico F, Perri L, et al. Upstream therapy with statin and recurrence of atrial fibrillation after electrical cardioversion. Review of the literature and meta-analysis. BMC Cardiovasc Disord. 2012;12:107. doi: 10.1186/1471-2261-12-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Demir K, Can I, Koc F, et al. Atorvastatin given prior to electrical cardioversion does not affect the recurrence of atrial fibrillation in patients with persistent atrial fibrillation who are on antiarrhythmic therapy. Med Princ Pract. 2011;20:464–49. doi: 10.1159/000327674. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Publication bias analysis by funnel plot.