Abstract
The progression of mild parkinsonian signs in the absence of idiopathic Parkinson’s disease in aging is unclear. This study aims to identify predictors of the evolution of mild parkinsonian signs in non-demented older adults. Two hundred ten participants (76.25 ± 7.10 years, 57 % women) were assessed at baseline and 1-year follow-up. Mild parkinsonian signs were defined as the presence of bradykinesia, rigidity and/or rest tremor. Depending upon the presence of these features at baseline and follow-up, participants were divided into one of four groups (no, transient, persistent or new-onset mild parkinsonian signs). Physical function was assessed using gait velocity. Ninety-five participants presented with mild parkinsonian signs at baseline. At 1-year follow-up, 59 demonstrated persistent mild parkinsonian signs, while 36 recovered (i.e., transient). Participants with persistent mild parkinsonian signs were older (79.66 ± 7.15 vs. 75.81 ± 7.37 years, p = 0.01) and evidenced slower gait velocity (90.41 ± 21.46 vs. 109.92 ± 24.32 cm/s, p < 0.01) compared to those with transient mild parkinsonian signs. Gait velocity predicted persistence of mild parkinsonian signs, even after adjustments (OR: 0.96, 95 % CI: 0.94–0.98). Fifty-five participants demonstrated new-onset of mild parkinsonian signs. In comparison to participants without mild parkinsonian signs, presence of cardiovascular but not cerebrovascular disease at baseline was associated with new-onset mild parkinsonian signs. Our study reveals that gait velocity was the main predictor of persistent mild parkinsonian signs, whereas cardiovascular disease was associated with new-onset mild parkinsonian signs. These findings suggest a vascular mechanism for the onset of mild parkinsonian signs and a different mechanism, possibly neurodegenerative, for the persistence of mild parkinsonian signs.
Keywords: Mild parkinsonian signs, Aging, Gait, Cardiovascular disease, Cerebrovascular disease
Introduction
Mild parkinsonian signs (MPS) are common in aging even in the absence of idiopathic Parkinson’s disease (PD), with a wide variance in prevalence ranging from 15 to 52 % [1, 2]. Age, criteria employed to define MPS, and cognitive status likely explain the large discrepancy in reported prevalence rates. In previous studies, MPS were associated not only with vascular risk factors [3], depression [4], dementia [5-7], and mortality [1, 8, 9], but also with functional disability [10, 11]. Among functional disability, the use of walking aids was associated with MPS [2].
While previous longitudinal studies have established the relationship of MPS with incident dementia in aging [6, 7, 12, 13], their association with other important clinical outcomes like gait disorders or cardiovascular conditions has not been documented. Recently cerebrovascular lesions, including macro and microinfarcts, were associated with MPS and with parkinsonian gait [14]. Besides vascular lesions and dementia, a pathological study of 744 deceased participants with antemortem MPS assessment demonstrated that nigral neuronal loss, but not nigral Lewy bodies deposition was associated with MPS [15]. However, to our knowledge no study to date has identified risk factors associated with the progression of MPS in aging.
To address this knowledge gap, we conducted a prospective cohort study investigating predictors of MPS in community residing non-demented older adults without PD or other parkinsonian syndromes assessed at baseline and at 1-year follow-up. We hypothesized that vascular pathophysiological mechanisms would be associated with the presence of MPS in the elderly, but the contribution of additional factors related with neurodegenerative processes, would be more likely in older adults with persistent MPS at follow-up.
Methods
Participants
Four hundred thirty-nine non-demented adults aged 65 and older were recruited in an ongoing cohort study entitled Central Control of Mobility in Aging (CCMA) from June 2011 to November 2013, and of whom 264 completed a 1-year follow up. The CCMA longitudinal study aims to determine cognitive and brain predictors of mobility decline and disability in aging. The study procedure has been previously described [16, 17]. Briefly, participants enrolled in the CCMA study are non-demented older adults residing in lower Westchester County who have successfully passed a telephone-screening interview. Participants engage in two in-house evaluations per year, where they receive comprehensive neurological, neuropsychological, and physical examinations. Consensus diagnostic case conferences were conducted to assure that participants did not meet criteria for dementia [18]. Of the 264 participants who completed the 1-year follow-up evaluation, participants without complete neurological examinations (n = 37), idiopathic PD at baseline (n = 7), missing quantitative gait assessments at baseline (n = 6), or prescribed dopamine-blocking agents/neuroleptics (n = 4) were excluded from this analysis. Following exclusions, 210 non-demented older adults were included in the current analysis (mean age: 76.25 ± 7.10 years, 57 % women). The institutional review board of the Albert Einstein College of Medicine approved the experimental procedures and all participants provided written informed consent in accordance with the tenets of the Declaration of Helsinki.
Mild parkinsonian signs and clinical assessment
Comprehensive neurological examination included assessment for clinical gait abnormalities [19], MPS, and medical illnesses. MPS were systematically ascertained in participants by the clinician using the motor evaluation portion (Part III) of the original version of the Unified Parkinson’s Disease Rating Scale (UPDRS) [20]. Severity indices for individual MPS were calculated by summing clinician ratings (0–4) within 3 core domains: (1) bradykinesia in extremities and body (UPDRS#23-26, 31); (2) rigidity in extremities and neck (UPDRS#22); and (3) rest tremor in extremities (UPDRS#20). A total MPS score was subsequently created, both at baseline and at follow-up, by adding the severity indices of the individual MPS. As in our previous work, we aimed to identify early markers of abnormal motor aging by taking a sensitive approach to define MPS based on the presence of any one feature of MPS [21], but more stringent methods have previously been employed [7, 10]. For the MPS severity score, the Cronbach’s α of 0.85 indicated good internal consistency, with excellent internal consistency for bradykinesia (0.90) and tremor (0.90), and good internal consistency for rigidity (0.88). The inter-rater reliability of MPS across the two clinicians revealed good inter-rater reliability (kappa, 0.60–0.90).
Of the 210 participants, 95 had MPS and 115 had no MPS at baseline. We examined the evolution of MPS in this cohort, by dividing participants with MPS at baseline (e.g., MPS+) into two groups: (i) MPS at baseline and at 1-year follow-up (persistent MPS group) and (ii) MPS at baseline but not at 1-year follow-up (transient MPS group). Further, to investigate potential contributors to MPS development, we divided participants without MPS at baseline (e.g., MPS−) into two groups: (iii) no MPS at baseline and at 1-year follow-up (absent MPS group) and (iv) no MPS at baseline and onset of new MPS at 1-year follow-up (new onset MPS group; Fig. 1).
Fig. 1.

Classification of eligible participants based on MPS status. Flowchart of CCMA participants based on presence or absence of mild parkinsonian signs at baseline and 1-year follow-up
CCMA = Central Control of Mobility in Aging study; MPS=Mild Parkinsonian Signs
The clinician documented the presence of depression, medical illnesses, cardiovascular disease, cerebrovascular disease, and cardiovascular risk factors, as these have been previously associated with MPS [22]. The geriatric depression scale (GDS [23]) was used to measure depression. Global health status summary scores (range 0–10) were obtained from dichotomous rating of diabetes, chronic heart failure, arthritis, hypertension, depression, stroke, Parkinson’s disease, chronic obstructive pulmonary disease, angina, and myocardial infarction [24, 25]. History of vascular diseases and medical illnesses were obtained through clinical interview. Vascular diseases were categorized as vascular risk factors (any one of diabetes, hypertension, hypercholesterolemia, BMI > 30, and smoking), cardiovascular disease (any one of myocardial infarction, angina, arrhythmia, and chronic heart failure), and cerebrovascular disease (any one of stroke or transient ischemic attacks). Vascular severity scores were also calculated by summing the presence of conditions within each of the three vascular domains.
Physical and cognitive function
Quantitative gait assessments were conducted by a research assistant (blinded to the MPS status) as described in our previous studies [24, 26, 27]. Gait velocity (cm/s) was measured using an instrumented walkway with embedded pressure sensors (GAITRite, CIR Systems, Havertown, PA). The GAITRite system is widely used in clinical and research settings and has excellent psychometric properties. For the purposes of this study, we only report gait velocity because it can be measured ubiquitously with a stopwatch over a fixed distance and does not require the use of instrumented methods.
Global cognitive status was assessed using Repeatable Battery for Assessment of Neuropsychological Status (RBANS) total score. The RBANS, a brief cognitive test with alternate forms, measures immediate and delayed memory, attention, language, and visuo-spatial abilities, which also provides a total index score [28].
Statistics
Descriptive statistics (mean and SD) were calculated for all four MPS groups. Data were inspected descriptively and graphically and the normality of model assumptions was formally tested. Separate analyses were conducted for individuals with and without MPS at baseline. That is, within the MPS− group, individuals who never demonstrated MPS (e.g., absent group) were compared to those who developed MPS at follow-up (e.g., new onset MPS group). Similarly, within the MPS+ group, those that continued to demonstrate MPS at 1-year follow-up (e.g., persistent MPS group) were compared to those who did not demonstrate MPS at follow-up (e.g., transient MPS group).
Differences between groups were assessed using independent t tests and Bonferroni corrections were applied to account for multiple comparisons within each domain (e.g., demographics, MPS, vascular, and physical function indices, Table 1). Binary logistic regression analyses were subsequently performed to examine the association of persistent vs. transient MPS (independent variables) with gait velocity, health, vascular, depression, and RBANS total scores (dependent variables) using SPSS version 20 [29]. Unadjusted univariate regressions were conducted first, followed by multivariate regressions adjusted for both age and gender. Similar univariate and multivariate regressions were also conducted for the absent vs. new onset MPS comparison groups.
Table 1.
Baseline characteristics for individuals with MPS
| Persistent (n = 59) | Transient (n = 36) | p value | |
|---|---|---|---|
| Demographics | |||
| Age (years) | 79.66 (7.15) | 75.81 (7.37) | 0.01 |
| Education (years) | 13.95 (3.21) | 15.39 (2.71) | 0.03 |
| % Female | 57.00 | 47.00 | 0.32 |
| GHS score (0–10) | 1.70 (1.10) | 1.75 (1.03) | 0.81 |
| GDS score (0–30) | 5.54 (4.05) | 3.94 (3.22) | 0.04 |
| MPS Indices | |||
| Bradykinesia (% present) | 53.00 | 17.00 | <0.01 |
| Rigidity (% present) | 83.00 | 83.00 | 0.97 |
| Tremor (% present) | 9.00 | 8.00 | 0.98 |
| Vascular | |||
| Vascular risk factor (0–5) | 1.89 (0.98) | 1.90 (1.27) | 0.97 |
| Cardiovascular conditions (0–4) | 0.25 (0.50) | 0.42 (1.25) | 0.43 |
| Cerebrovascular conditions (0–2) | 0.08 (0.28) | 0.12 (0.33) | 0.59 |
| Physical and cognitive function | |||
| Gait velocity (cm/s) | 90.41 (21.46) | 109.92 (24.32) | <0.01 |
| RBANS total score | 90.36 (12.62) | 94.19 (11.92) | 0.15 |
MPS Mild Parkinsonian signs, GHS Global Health Score, GDS Geriatric Depression Scale, RBANS Repeatable Battery for the Assessment of Neuropsychological Status, p values presented in bold survive Bonferroni correction
Results
Baseline characteristics of the sample are provided in Table 1 for individuals with persistent and transient MPS and in Table 2 for those with absent and new onset MPS. Regardless of MPS classification, individuals were deemed relatively healthy and cognitively intact as determined by their global health status (GHS) and RBANS total score. Within the MPS + groups, rigidity was the most common MPS at baseline, followed by bradykinesia, and rest tremor (Table 1). Results from logistic regression adjusted for age and gender revealed that the presence of bradykinesia significantly predicted inclusion in either the transient or persistent MPS group (OR = 0.11, p < 0.01).
Table 2.
Baseline characteristics for individuals without MPS
| Absent (n = 60) | New onset (n = 55) | p value | |
|---|---|---|---|
| Demographics | |||
| Age (years) | 74.12 (5.88) | 75.22 (6.93) | 0.36 |
| Education (years) | 14.40 (2.54) | 15.04 (3.48) | 0.26 |
| % Female | 57.00 | 64.00 | 0.45 |
| GHS score (0–10) | 1.23 (0.93) | 1.47 (1.27) | 0.26 |
| GDS score (0–30) | 3.50 (2.33) | 4.20 (3.36) | 0.20 |
| Vascular | |||
| Vascular risk factor (0–5) | 1.43 (1.06) | 1.45 (1.12) | 0.92 |
| Cardiovascular conditions (0–4) | 0.08 (0.33) | 0.27 (0.49) | 0.02 |
| Cerebrovascular conditions (0–2) | 0.03 (0.18) | 0.19 (0.39) | 0.21 |
| Physical and cognitive function | |||
| Gait velocity (cm/s) | 108.56 (23.22) | 101.15 (23.95) | 0.10 |
| RBANS total score | 90.36 (12.62) | 94.19 (11.92) | 0.15 |
MPS Mild Parkinsonian signs, GHS Global Health Score, GDS Geriatric Depression Scale, RBANS Repeatable Battery for the Assessment of Neuropsychological Status, p value presented in bold survives Bonferroni correction
Of the 95 participants with MPS at baseline, 66 had one MPS and 29 had two MPS. To further confirm the association between MPS status and gait velocity, we conducted a sensitivity analysis using more stringent criteria to determine persistent vs. transient MPS status by requiring the presence of any two (instead of just one) features of MPS at baseline and at follow-up to define persistence. Participants with two features of MPS at baseline but none or one feature of MPS at follow-up were considered in the control group in this sensitivity analysis. Using the same multivariate logistic regression analysis, results confirmed that only gait velocity significantly predicts the progression of MPS (OR = 0.97, p = 0.02), even after controlling for age and gender. Differences in gait velocity were noted at baseline (t = 4.09, p < 0.001) and at follow-up (t = 4.09, p < 0.001) between transient and persistent MPS groups (Fig. 2).
Fig. 2.
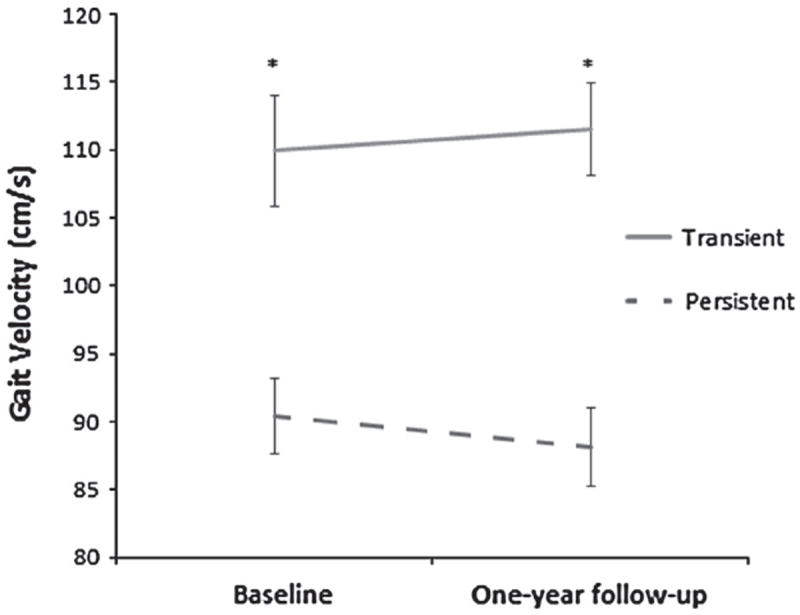
Evolution of Gait Velocity for individuals with transient and persistent mild parkinsonian signs. A depiction of gait velocity for the 95 individuals with transient and persistent mild parkinsonian signs at baseline and 1-year follow up. Participants in transient group (solid grey trace) improved their gait velocity over 1 year from 110 to 112 cm/s, whereas those in the persistent group (dashed grey trace) decreased their gait velocity from 90 to 88 cm/s. Bars represent standard errors of the mean
* p <0.001
Regarding new onset MPS, comparisons between the absent vs. new onset MPS groups revealed that participants in the new onset group demonstrated significantly more cardiovascular disease than those in the absent group (Table 3). This significant difference in severity of cardiovascular disease persisted at both the univariate (OR = 3.31, p = 0.02) and multivariate levels (OR = 3.59, p = 0.03; Table 4).
Table 3.
Predictors of persistent vs. transient mild parkinsonian signs
| Variable | Univariate
|
Multivariate
|
||||||
|---|---|---|---|---|---|---|---|---|
| Odds ratio | 95 % C.I.
|
p value | Odds ratio | 95 % C.I.
|
p value | |||
| Lower | Upper | Lower | Upper | |||||
| Age, years | 1.08 | 1.01 | 1.15 | 0.02 | 1.04 | 0.97 | 1.12 | 0.26 |
| Gender (female) | 1.52 | 0.66 | 3.50 | 0.33 | 1.67 | 0.62 | 4.50 | 0.31 |
| GHS (0–10) | 0.95 | 0.65 | 1.41 | 0.81 | 0.67 | 0.35 | 1.25 | 0.67 |
| GDS (0–30) | 1.13 | 1.00 | 1.29 | 0.06 | 1.11 | 0.96 | 1.28 | 0.16 |
| Vascular risk factor (0–5) | 1.01 | 0.70 | 1.44 | 0.97 | 1.16 | 0.68 | 2.00 | 0.59 |
| Cardiovascular conditions (0–4) | 1.25 | 0.69 | 2.27 | 0.45 | 1.22 | 0.61 | 2.43 | 0.58 |
| Cerebrovascular conditions (0–2) | 1.48 | 0.36 | 6.13 | 0.59 | 2.13 | 0.38 | 13.88 | 0.36 |
| Gait velocity (cm/s) | 0.96 | 0.94 | 0.98 | <0.01 | 0.97 | 0.94 | 0.99 | <0.01 |
| Cognition (RBANS Total Score) | 0.97 | 0.94 | 1.01 | 0.15 | 0.99 | 0.95 | 1.03 | 0.55 |
Table 4.
Predictors of absent vs. new onset mild parkinsonian signs
| Variable | Univariate
|
Multivariate
|
||||||
|---|---|---|---|---|---|---|---|---|
| Odds ratio | 95 % C.I.
|
p value | Odds ratio | 95 % C.I.
|
p value | |||
| Lower | Upper | Lower | Upper | |||||
| Age, years | 1.03 | 0.97 | 1.09 | 0.36 | 0.99 | 0.92 | 1.06 | 0.78 |
| Gender (female) | 1.34 | 0.63 | 2.83 | 0.45 | 1.25 | 0.56 | 2.80 | 0.59 |
| GHS (0–10) | 1.22 | 0.87 | 1.71 | 0.25 | 1.00 | 0.58 | 1.72 | 1.00 |
| GDS (0–30) | 1.09 | 0.96 | 1.24 | 0.19 | 1.10 | 0.95 | 1.28 | 0.20 |
| Vascular risk factor (0–5) | 1.01 | 0.73 | 1.43 | 0.92 | 0.95 | 0.58 | 1.55 | 0.83 |
| Cardiovascular conditions (0–4) | 3.31 | 1.17 | 9.36 | 0.02 | 3.59 | 1.14 | 11.30 | 0.03 |
| Cerebrovascular conditions (0–2) | 2.90 | 0.54 | 15.61 | 0.22 | 2.34 | 0.32 | 16.96 | 0.40 |
| Gait velocity (cm/s) | 0.99 | 0.97 | 1.00 | 0.10 | 0.99 | 0.97 | 1.01 | 0.37 |
| Cognition (RBANS total score) | 0.98 | 0.95 | 1.02 | 0.35 | 0.99 | 0.95 | 1.02 | 0.43 |
Unadjusted univariate and multivariate regressions were performed to examine associations of MPS status (independent variables) with gait velocity, health (GHS), depression (GDS), vascular risk factors, cardiovascular disease, cerebrovascular disease, and cognition (dependent variables). Bold values indicate significant p values
GHS Global Health Score, GDS Geriatric Depression Scale, RBANS Repeatable Battery for the Assessment of Neuropsychological Status
Discussion
Our study shows that MPS is transient in 38 % of healthy older adults, and that gait velocity predicts MPS stability. Furthermore, the presence of cardiovascular disease, but not gait velocity or other selected predictors, was associated with the onset of new MPS at 1-year follow-up.
The etiopathogenesis of MPS is unclear in the elderly, and seems to be multifactorial [22]. MPS could represent an early marker of neurodegenerative disorders like PD or Alzheimer’s disease (AD), a signature of small vascular infarcts [22], or a feature of neuronal loss in the dopaminergic system as suggested by a recent neuropathological study [15]. Although none of these previously suggested causes are reversible, more than one-third of the participants in our study did not present with any MPS at the 1-year follow-up visit. Disappearance of MPS could be attributed to brain plasticity in normal older adults, as the CCMA cohort does not include participants with dementia at baseline. Unfortunately, information on interval rehabilitative efforts that might influence brain recovery and account for the disappearance of MPS in our participants was not available. The potential reversibility of MPS is important to consider for clinicians, because it could suggest that MPS does not necessarily foreshadow an immediate progressive condition.
Among the selected potential predictors of progressive MPS, only gait velocity was associated with persistent MPS at 1-year, even after using more stringent criteria for defining the transient and persistent groups. Gait velocity in the elderly represents a final pathway combining balance, motor, sensory systems, as well as cognition [30]. In addition, the fact that gait velocity predicted persistent MPS is supported by recent findings in non-demented older adults without idiopathic PD: bradykinesia that represents a required feature for parkinsonism has been associated with gait velocity [21]. From a metabolic perspective, gait speed was associated with cholinergic but not dopaminergic denervation in PD patients; [31] suggesting a close relationship between gait and the cholinergic system. No other suspected risk factors than gait speed predicted the persistence of MPS.
In a similar longitudinal aging study investigating MPS and other predictors of dementia, Louis et al. [12] revealed that only MPS predicted dementia, but did not find an interaction with other known risk factors for dementia, including vascular risk factors or APOE-ε4 positive status. Although previous studies have shown that the presence of MPS in non-demented older adults predicted incident dementia [6, 7, 12], cognitive function did not predict the stability nor the appearance of MPS in the present study. This could be explained by the fact that our definition of MPS purposefully did not include the postural instability and gait disturbance (PIGD) items from the UPDRS that were the main contributing factor for incident dementia in the religious order study [6]. Finally, the number of included participants in the present study is likely not large enough to show such a prediction. Taken together, the absence of vascular risk factors as predictors of persistent MPS and the progression of declines in gait velocity could suggest the contribution of underlying neurodegenerative processes, like PD, AD, or other non-vascular parkinsonian syndromes in the persistent MPS group.
The clinical profile of the MPS between the persistent and transient groups was different. Although rigidity was present in 83 % of participants in both groups, bradykinesia was the discriminative feature between the two groups, with the highest prevalence in the persistent group. Interestingly, in a study examining the association of MPS and white matter disease in the elderly, bradykinesia was independently related with the presence of the lacunar infarcts [32]. Regarding the complex link between MPS and cerebrovascular disease, the presence of cerebrovascular disease did not predict the stability or onset of new MPS, whereas cardiovascular disease did predict the new onset of MPS. Cardiovascular conditions, like atrial fibrillation, precede cerebrovascular conditions and constitute very well known risk factors for cerebrovascular conditions [33]. This chronological sequence could explain why cardiovascular but not cerebrovascular diseases predict MPS. An alternative explanation could refer to the fact that cardiovascular diseases outweigh cerebrovascular diseases. Regarding the pathophysiology of vascular parkinsonism and its high prevalence in older adults [34], it is likely that vascular mechanisms are key contributors to the appearance of MPS in aging.
As a limitation, the short follow-up period and the relative small sample size, especially in the transient MPS group, could mask some additional predictors, like cognitive functions. These results should be replicated in a larger prospective cohort with longer follow-up intervals. In addition to the good internal consistency and inter-rater reliability of MPS in this study, the differences observed at baseline between the transient and persistent MPS groups (i.e. slower gait velocity in the persistent group compared to the transient group); the fact that applying more stringent criteria does not modify the results; and the fact that gait velocity decreases in the persistent group and increases in the transient group all suggest that our findings are consistent and not due to a reliability issue.
In conclusion, we observed that MPS may be reversible in the elderly and that gait velocity predicts the progression of MPS. Regarding new onset of MPS in aging, cardiovascular disease constitutes the main predictor. Our results suggest vascular mechanisms as the trigger of MPS in aging that are potentially reversible. However, for the progression of MPS, additional investigations are required to determine the pathophysiological mechanisms, possibly neurodegenerative, underlying gait velocity.
Highlights.
MPS can be reversible in healthy older adults.
Slow gait velocity was the main predictor of persistent MPS in normal aging.
Cardiovascular disease was associated with onset of new MPS.
Acknowledgments
Research was supported by funding from the National Institute on Aging (R01AG036921-01A1 & R01AG044007-01A1). Special thanks to all of the CCMA research assistants for their assistance with data collection.
Funding This study was supported by funds from the National Institutes of Health, National Institute on Aging (R01AG036921-01A1 & R01AG044007-01A1). Gilles Allali is supported by a Grant from the Geneva University Hospitals.
Footnotes
Conflicts of interest No competing interests to report.
Ethical standards The institutional review board of the Albert Einstein College of Medicine approved the experimental procedures and all participants provided written informed consent in accordance with the tenets of the Declaration of Helsinki.
Contributor Information
Jeannette R. Mahoney, Department of Neurology, Division of Cognitive and Motor Aging, Albert Einstein College of Medicine, Yeshiva University, 1165 Morris Park Avenue, Room 325, Bronx, New York 10461, USA
Joe Verghese, Department of Neurology, Division of Cognitive and Motor Aging, Albert Einstein College of Medicine, Yeshiva University, 1165 Morris Park Avenue, Room 325, Bronx, New York 10461, USA.
Roee Holtzer, Department of Neurology, Division of Cognitive and Motor Aging, Albert Einstein College of Medicine, Yeshiva University, 1165 Morris Park Avenue, Room 325, Bronx, New York 10461, USA; Ferkauf Graduate of Psychology, Yeshiva University, Bronx, New York, USA.
Gilles Allali, Email: gilles.allali@hcuge.ch, Gilles.Allali@einstein.yu.edu, Department of Neurology, Division of Cognitive and Motor Aging, Albert Einstein College of Medicine, Yeshiva University, 1165 Morris Park Avenue, Room 325, Bronx, New York 10461, USA; Department of Clinical Neurosciences, Geneva University Hospitals and University of Geneva, Geneva, Switzerland.
References
- 1.Bennett DA, Beckett LA, Murray AM, Shannon KM, Goetz CG, Pilgrim DM, Evans DA. Prevalence of parkinsonian signs and associated mortality in a community population of older people. N Engl J Med. 1996;334(2):71–76. doi: 10.1056/NEJM199601113340202. [DOI] [PubMed] [Google Scholar]
- 2.Louis ED, Schupf N, Marder K, Tang MX. Functional correlates of mild parkinsonian signs in the community-dwelling elderly: poor balance and inability to ambulate independently. Mov Disord. 2006;21(3):411–416. doi: 10.1002/mds.20735. [DOI] [PubMed] [Google Scholar]
- 3.Louis ED, Luchsinger JA. History of vascular disease and mild parkinsonian signs in community-dwelling elderly individuals. Arch Neurol. 2006;63(5):717–722. doi: 10.1001/archneur.63.5.717. [DOI] [PubMed] [Google Scholar]
- 4.Uemura Y, Wada-Isoe K, Nakashita S, Nakashima K. Depression and cognitive impairment in patients with mild parkinsonian signs. Acta Neurol Scand. 2013;128(3):153–159. doi: 10.1111/ane.12089. [DOI] [PubMed] [Google Scholar]
- 5.Richards M, Stern Y, Marder K, Cote L, Mayeux R. Relationships between extrapyramidal signs and cognitive function in a community-dwelling cohort of patients with Parkinson’s disease and normal elderly individuals. Ann Neurol. 1993;33(3):267–274. doi: 10.1002/ana.410330307. [DOI] [PubMed] [Google Scholar]
- 6.Wilson RS, Schneider JA, Bienias JL, Evans DA, Bennett DA. Parkinsonianlike signs and risk of incident Alzheimer disease in older persons. Arch Neurol. 2003;60(4):539–544. doi: 10.1001/archneur.60.4.539. [DOI] [PubMed] [Google Scholar]
- 7.Louis ED, Tang MX, Mayeux R. Parkinsonian signs in older people in a community-based study: risk of incident dementia. Arch Neurol. 2004;61(8):1273–1276. doi: 10.1001/archneur.61.8.1273. [DOI] [PubMed] [Google Scholar]
- 8.Mitchell SL, Rockwood K. The association between parkinsonism, Alzheimer’s disease, and mortality: a comprehensive approach. J Am Geriatr Soc. 2000;48(4):422–425. doi: 10.1111/j.1532-5415.2000.tb04701.x. [DOI] [PubMed] [Google Scholar]
- 9.Waite LM, Grayson DA, Piguet O, Creasey H, Bennett HP, Broe GA. Gait slowing as a predictor of incident dementia: 6-year longitudinal data from the Sydney older persons study. J Neurol Sci. 2005;229–230:89–93. doi: 10.1016/j.jns.2004.11.009. [DOI] [PubMed] [Google Scholar]
- 10.Louis ED, Tang MX, Schupf N, Mayeux R. Functional correlates and prevalence of mild parkinsonian signs in a community population of older people. Arch Neurol. 2005;62(2):297–302. doi: 10.1001/archneur.62.2.297. [DOI] [PubMed] [Google Scholar]
- 11.Fleischman DA, Wilson RS, Schneider JA, Bienias JL, Bennett DA. Parkinsonian signs and functional disability in old age. Exp Aging Res. 2007;33(1):59–76. doi: 10.1080/03610730601006370. [DOI] [PubMed] [Google Scholar]
- 12.Louis ED, Tang MX, Schupf N. Mild parkinsonian signs are associated with increased risk of dementia in a prospective, population-based study of elders. Mov Disord. 2010;25(2):172–178. doi: 10.1002/mds.22943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Israeli-Korn SD, Massarwa M, Schechtman E, Strugatsky R, Avni S, Farrer LA, Friedland RP, Inzelberg R. Mild cognitive impairment is associated with mild parkinsonian signs in a door-to-door study. J Alzheimers Dis. 2010;22(3):1005–1013. doi: 10.3233/jad-2010-101230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Buchman AS, Leurgans SE, Nag S, Bennett DA, Schneider JA. Cerebrovascular disease pathology and parkinsonian signs in old age. Stroke. 2011;42(11):3183–3189. doi: 10.1161/strokeaha.111.623462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Buchman AS, Shulman JM, Nag S, Leurgans SE, Arnold SE, Morris MC, Schneider JA, Bennett DA. Nigral pathology and parkinsonian signs in elders without Parkinson disease. Ann Neurol. 2012;71(2):258–266. doi: 10.1002/ana.22588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Holtzer R, Wang C, Verghese J. Performance variance on walking while talking tasks: theory, findings, and clinical implications. Age. 2013 doi: 10.1007/s11357-013-9570-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Holtzer R, Mahoney J, Verghese J. Intraindividual variability in executive functions but not speed of processing or conflict resolution predicts performance differences in gait speed in older adults. J Gerontol A Biol Sci Med Sci. 2013 doi: 10.1093/gerona/glt180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Holtzer R, Goldin Y, Zimmerman M, Katz M, Buschke H, Lipton RB. Robust norms for selected neuropsychological tests in older adults. Arch Clin Neuropsychol. 2008;23(5):531–541. doi: 10.1016/j.acn.2008.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Verghese J, Lipton RB, Hall CB, Kuslansky G, Katz MJ, Buschke H. Abnormality of gait as a predictor of non-Alzheimer’s dementia. N Engl J Med. 2002;347(22):1761–1768. doi: 10.1056/NEJMoa020441. [DOI] [PubMed] [Google Scholar]
- 20.Fahn SER. Unified Parkinson’s Disease Rating Scale. MacMillan Healthcare Information; Florham Park: 1987. [Google Scholar]
- 21.Allali G, Verghese J, Mahoney JR. Contributions of mild parkinsonian signs to gait performance in the elderly. Age. 2014;36(4):9678. doi: 10.1007/s11357-014-9678-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Louis ED, Bennett DA. Mild Parkinsonian signs: an overview of an emerging concept. Mov Disord. 2007;22(12):1681–1688. doi: 10.1002/mds.21433. [DOI] [PubMed] [Google Scholar]
- 23.Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, Adey M, Leirer VO. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res. 1982;17(1):37–49. doi: 10.1016/0022-3956(82)90033-4. [DOI] [PubMed] [Google Scholar]
- 24.Holtzer R, Verghese J, Xue X, Lipton RB. Cognitive processes related to gait velocity: results from the Einstein aging study. Neuropsychology. 2006;20(2):215–223. doi: 10.1037/0894-4105.20.2.215. [DOI] [PubMed] [Google Scholar]
- 25.Verghese J, Kuslansky G, Holtzer R, Katz M, Xue X, Buschke H, Pahor M. Walking while talking: effect of task prioritization in the elderly. Arch Phys Med Rehabil. 2007;88(1):50–53. doi: 10.1016/j.apmr.2006.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Verghese J, Wang C, Lipton RB, Holtzer R, Xue X. Quantitative gait dysfunction and risk of cognitive decline and dementia. J Neurol Neurosurg Psychiatry. 2007;78(9):929–935. doi: 10.1136/jnnp.2006.106914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Verghese JHR, Lipton RB, Wang C. Quantitative gait markers and incident fall risk in older adults. J Gerontol A Biol Sci Med Sci. 2009;64:896–901. doi: 10.1093/gerona/glp033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Duff K, Humphreys Clark JD, O’Bryant SE, Mold JW, Schiffer RB, Sutker PB. Utility of the RBANS in detecting cognitive impairment associated with Alzheimer’s disease: sensitivity, specificity, and positive and negative predictive powers. Arch Clin Neuropsychol. 2008;23(5):603–612. doi: 10.1016/j.acn.2008.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Corp I. SPSS Statistics for Windows. 20.0. IBM Corp.; Armonk, NY: Released 2011. [Google Scholar]
- 30.Snijders AH, van de Warrenburg BP, Giladi N, Bloem BR. Neurological gait disorders in elderly people: clinical approach and classification. Lancet Neurol. 2007;6(1):63–74. doi: 10.1016/S1474-4422(06)70678-0. [DOI] [PubMed] [Google Scholar]
- 31.Bohnen NI, Frey KA, Studenski S, Kotagal V, Koeppe RA, Scott PJ, Albin RL, Muller ML. Gait speed in Parkinson disease correlates with cholinergic degeneration. Neurology. 2013;81(18):1611–1616. doi: 10.1212/WNL.0b013e3182a9f558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.de Laat KF, van Norden AG, Gons RA, van Uden IW, Zwiers MP, Bloem BR, van Dijk EJ, de Leeuw FE. Cerebral white matter lesions and lacunar infarcts contribute to the presence of mild parkinsonian signs. Stroke. 2012;43(10):2574–2579. doi: 10.1161/strokeaha.112.657130. [DOI] [PubMed] [Google Scholar]
- 33.Wolf PA, Dawber TR, Thomas HE, Jr, Kannel WB. Epidemiologic assessment of chronic atrial fibrillation and risk of stroke: the Framingham study. Neurology. 1978;28(10):973–977. doi: 10.1212/wnl.28.10.973. [DOI] [PubMed] [Google Scholar]
- 34.Kalra S, Grosset DG, Benamer HT. Differentiating vascular parkinsonism from idiopathic Parkinson’s disease: a systematic review. Mov Disord. 2010;25(2):149–156. doi: 10.1002/mds.22937. [DOI] [PubMed] [Google Scholar]


