Abstract
Objective
To compare the Welch Allyn SureSight™ wavefront autorefractor with retinoscopy in normal dogs.
Animals studied
50 privately-owned dogs (100 eyes) of 20 breeds, free of ocular disease. Mean ±SD age 5.7 ± 3.25 years (range: 6 months – 13 years).
Procedures
The refractive error was determined in each eye by two experienced retinoscopists using streak retinoscopy as well as by an autorefractor operated by two different examiners. Measurements were performed before and approximately 30–45 minutes after cycloplegia was induced by cyclopentolate 0.5% and tropicamide 0.5% ophthalmic solutions.
Results
Mean ±SD non-cyclopleged retinoscopy net sphere was −0.55 ± 1.14 (range: −3.75 to 3.5) diopters (D). Mean cyclopleged retinoscopy net sphere was −0.52 ±1.18 (range: −4.25 to 2) D. Mean ± SD non-cyclopleged autorefractor spherical equivalent (SE) was −0.42 ± 1.13D (range: −3.36 to 2.73) D. Mean cyclopleged autorefractor spherical equivalent was 0.10 ±1.47 (range: −5.62 to 3.19) D. Non-cyclopleged autorefraction results were not significantly different from streak retinoscopy (whether non-cyclopleged or cyclopleged, p=0.80, 0.26, respectively). Cyclopleged autorefraction results were significantly different from non-cyclopleged or cyclopleged streak retinoscopy (p<0.0001 in both states). There was no significant difference between non-cyclopleged and cyclopleged streak retinoscopy (p= 0.97).
Conclusions
Non-cyclopleged autorefraction shows good agreement with streak retinoscopy in dogs and may be a useful clinical technique. Cycloplegia does not significantly affect streak retinoscopy results in dogs.
Keywords: Retinoscopy, streak retinoscopy, refractive error, autorefractor, comparison, SureSight™
Introduction
Initiation of the visual process begins with presentation of a clearly focused image on the retina. To permit a focused image, light must be sequentially bent (refracted) by precise degrees as it passes through the ocular media. An unfocused image occurs when the focal point is located either in front of or behind the retina. Although dogs are, on average, within 0.5 diopters (D) of emmetropia, several canine breeds and even families within breeds have been identified as showing a tendency toward ametropia (myopia or hyperopia). (1–5) In addition, the availability of intraocular lenses (IOLs) having only one refractive power creates the possibility that ametropia may be induced in a previously emmetropic eye following cataract surgery with implantation of an IOL. (6,7) Refractive error degrades visual acuity in dogs (8) and a recent report documents that even small degrees of induced refractive error significantly impacts field performance in field trial retrievers. (9)
The owners of performance dogs are becoming increasingly aware of the importance of the optical system on visual performance. Streak retinoscopy remains the gold standard for determining refractive state but the number of veterinarians trained and routinely practicing this technique with animals remains relatively small. The provision of a more easily performed, reliable method for determining refractive state in veterinary patients would likely expand the number of practitioners assessing refractive state which in turn would expand our knowledge base regarding refractive error in animals, improve the delivery of clinical services to clients with performance animals, guide dogs and other working animals, and serve in the diagnostic workup of patients with poor vision.
Automated refractors are commonly used by physician ophthalmologists and optometrists. Wavefront autorefractor models, such as the Welch Allyn SureSight™ autorefractor investigated in this study, offer several practical advantages compared to retinoscopy. They provide rapid results, have a relatively long working distance (0.35 m) which makes them especially useful for use in children, and theoretically better suited for use in animals, and require little training to learn to accurately operate. The device works by calculating the path of reflected light emerging from the eye, projected via a beam-splitter to a Hartmann-Shack sensor. The sensor evaluates whether the light is converging or diverging as it exits the eye based on the distribution of light spots on the matrix camera. (10)
The automated instrument provides a measurement of sphere, cylinder and axis, which correspond to the magnitude of insufficient/excessive refraction, extent of astigmatism (asymmetrical focus), and the orientation of the astigmatism, respectively. The device also provides a “reliability number” expressed as a value between 1 and 9, with a higher number corresponding to a more accurate measurement. The manufacturer recommends repeating measurements associated with a reliability number of five or less. Although astigmatism can be evaluated by streak retinoscopy, such measurement is very challenging in canine patients. Refractive error in dogs is therefore most commonly limited to the measurement of spherical aberration only.
This study evaluated the accuracy and practical ease of use of the Welch Allyn SureSight™ autorefractor in a range of normal dogs of a variety of breeds and ages. Results generated by the autorefractor were compared to the results obtained by streak retinoscopy performed by experienced retinoscopists. Both techniques were evaluated with eyes in a non-cyclopleged and cyclopleged state.
Materials and Methods
50 dogs (100 eyes) were recruited to participate in this study at the Veterinary Medical Teaching Hospital, University of California, Davis. Owners completed an informed consent form and the study was approved by the University of California, Davis clinical trial review board. Mean dog age was 5.7 (+/− 3.25 S.D) years (range: 6 months – 13 years). Pure and mixed-breed dogs were used, including Labrador Retriever (2), German Shepherd (2), Chihuahua (2), Pit Bull Terrier (2), Border Collie (3), Beagle (2), German Short-Haired Pointer (1), Standard Poodle (1), Greyhound (1), Brittany (1), Yorkshire Terrier (1), English Springer Spaniel (1), Corgi (1), Boston Terrier (1), Bull Terrier (1), Rat Terrier (1), Golden Retriever (1), Shih Tzu (1), Australian Shepherd (3), and Bullmastiff (1). All dogs lacked a history of significant current or previous ophthalmic disease. All dogs underwent ophthalmic examination by a board-certified veterinary ophthalmologist (SRH), which included slit lamp biomicroscopy and binocular indirect ophthalmoscopy after pupil dilation. No dogs had ophthalmic abnormalities that impaired the fundic reflex.
Refractive error was measured using two techniques: streak retinoscopy (technique 1) and autorefraction (technique 2). For technique 1, refractive error of each eye was evaluated by each of two board-certified veterinary ophthalmologists experienced in streak retinoscopy in dogs (RO, CJM) using a retinoscope and retinoscopy bars. The refractive error of the horizontal and vertical meridians was recorded, after correction for working distance (approximately 66 cm, 1.5 D). Results for the horizontal and vertical meridians were averaged to calculate net spherical refractive error.
For technique 2, the refractive error of each eye was measured using the Welch Allyn SureSight™ Autorefractor (operated in “child” mode by an ophthalmology resident (ADG) and a board-certified veterinary ophthalmologist (SRH). During the autorefractor measurement the owner was asked to stand in front of the dog, parallel with the autorefractor, with the intention that the dog would focus upon the owner. The number of measurements obtained via this technique was dependent upon patient compliance and visual fixation on the device. Up to two attempts were made to obtain each measurement. Values were averaged when more than one result was obtained under the same state of cycloplegia. While reliability number was recorded for each measurement, all results were included in analysis irrespective of their associated reliability number. The order in which each technique (1 and 2) was performed was random.
Following non-cyclopleged measurement by each technique, one drop of cyclopentolate 0.5% and one drop of tropicamide 0.5% ophthalmic solutions were applied to both eyes. Both agents were repeated 5 minutes later. Approximately 30 to 45 minutes after the first application of cyclopleged drops all measurements were repeated as described above. Examiners were masked to the results of the others for the duration of the study.
Performing measurements under standardized ambient room light conditions was attempted; however we found that performing autorefractor measurements in dim light conditions made aligning the laser beam with the ocular fundic reflex difficult. This posed a particular challenge in dogs with heavily pigmented irises. Measurements were therefore performed in as dim a light intensity as was practical. Streak retinoscopy was performed in dim light at a fixed intensity of approximately 54 lux.
Technique 2 (autorefraction) values were adjusted to their spherical equivalent. This converts the cylinder measure of astigmatism to their equivalent result describing sphere only. This enabled direct comparison between techniques 1 and 2. Cylinder results between techniques were not compared since these values were not obtained by retinoscopy. Spherical equivalent (SE) was calculated by: Spherical equivalent = Sphere + 0.5 * cylinder
Difference of spherical equivalent (DSE) between techniques 1 and 2 was calculated by subtracting net sphere of technique 1 (retinoscopy) from the spherical equivalent of technique 2 (autorefraction).
Comparisons between technique 1 and 2, non-cyclopleged or cyclopleged, eye (left or right), and net DSE versus reliability number were calculated using repeated measures-ANOVA using commercially-available software (SigmaStat 12, Systat Software, Inc. 225 W Washington St., Suite 425 Chicago, IL 60606 USA). A Bonferri correction was used to adjust for multiple comparisons when comparing individual observers. A p value < 0.05 was considered significant.
Results
Technique 1: Retinoscopy
Using pooled results from both examiners, mean ±SD non-cyclopleged retinoscopy net sphere was −0.55 ± 1.14 (range: −3.75 to 3.5) D. Mean cyclopleged retinoscopy net sphere was −0.52 ±1.18 (range: −4.25 to 2) D. There was no significant difference between non-cycloplegednonand cyclopleged net sphere (p= 0.966).
There was no statistically significant inter-observer (RO versus CJM) difference in net sphere under non-cyclopleged or cyclopleged conditions (p=0.52 and p=0.88, respectively). Mean and median inter-observer difference was 0.12 D and 0.0075 D under non-cyclopleged and cyclopleged conditions, respectively, with an overall median difference of 0 D. There was no significant difference between non-cyclopleged or cyclopleged net sphere of the right and left eyes (p=0.56 for both states).
Technique 2: Autorefraction
Using pooled results from both examiners, mean ± SD non-cyclopleged autorefraction spherical equivalent was −0.42 ± 1.13 (range: −3.36 to 2.73) D. Mean cyclopleged autorefractor spherical equivalent was 0.10 ±1.47D. There was a significant difference between non-cyclopleged and cyclopleged spherical equivalent (p < 0.001). There was no significant difference between non-cyclopleged or cyclopleged spherical equivalent of the right and left eyes (p=0.76 and p=0.51 respectively).
There was a statistically significant inter-observer (SRH versus ADG) difference in spherical equivalent under non-cyclopleged and cyclopleged conditions (p<0.0001 for both)). The inter-observer difference averaged 0.84D +/− 1.26 and 0.12D +/− 1.61 under non-cyclopleged and cyclopleged conditions, respectively. Average non-cyclopleged and cyclopleged spherical equivalent for SRH was −0.05 +/− 1.18 (range: −2.56 to 2.69) D and 0.25+/− 1.135 (range: −2.62 to 3.19) D, respectively. Average non-cyclopleged and cyclopleged spherical equivalent for ADG was −0.79 +/− 1.26 (range: −4.53 to 2.94) D and −0.21 +/− 1.22 (range: −3.34 to 2.44) D, respectively.
Retinoscopy vs. Autorefraction
(Table 1) A statistically significant difference was shown when cyclopleged autorefraction was compared to either cyclopleged or non-cyclopleged retinoscopy. There was no statistically significant difference when non-cyclopleged autorefraction was compared to either cyclopleged or non-cyclopleged retinoscopy.
Table 1.
Comparison of results obtained by retinoscopy and autorefraction under different conditions of cycloplegia, shown by the difference of spherical equivalent in diopters.
| Technique 1 (Retinoscopy) |
Technique 2 (Autorefraction) |
Difference in spherical equivalent (D) |
P value |
|---|---|---|---|
| Cyclopleged | Non-cyclopleged | 0.22 | 0.26 |
| Non-cyclopleged | Non-cyclopleged | 0.22 | 0.80 |
| Non-cyclopleged | Cyclopleged | 0.65 | <0.0001 |
| Cyclopleged | Cyclopleged | 0.62 | <0.0001 |
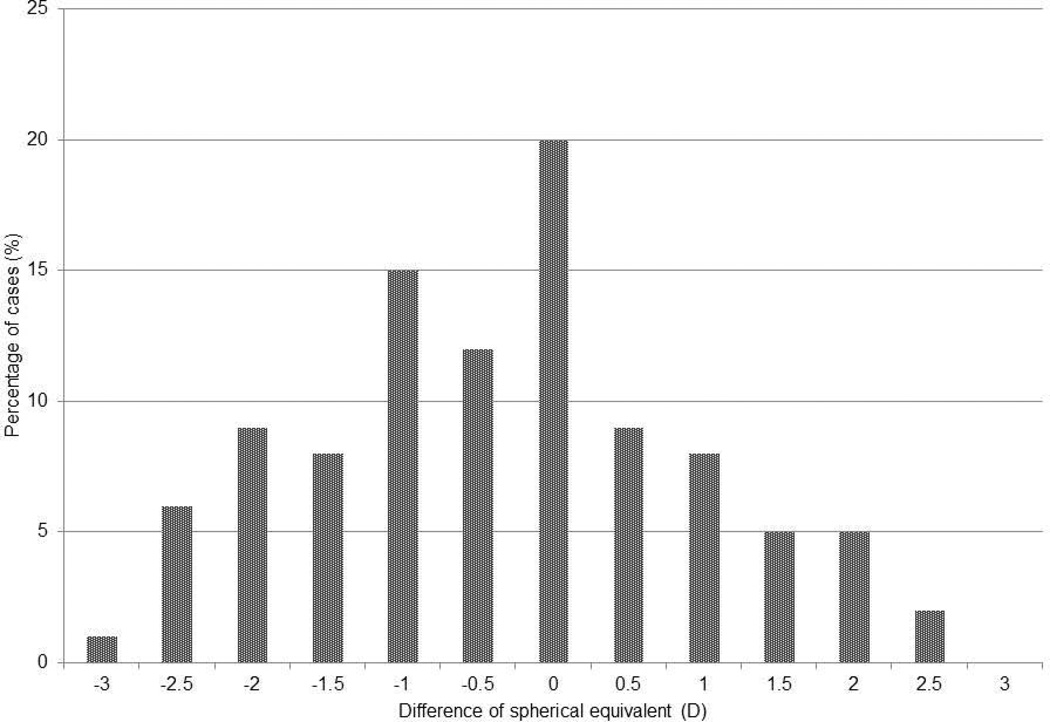
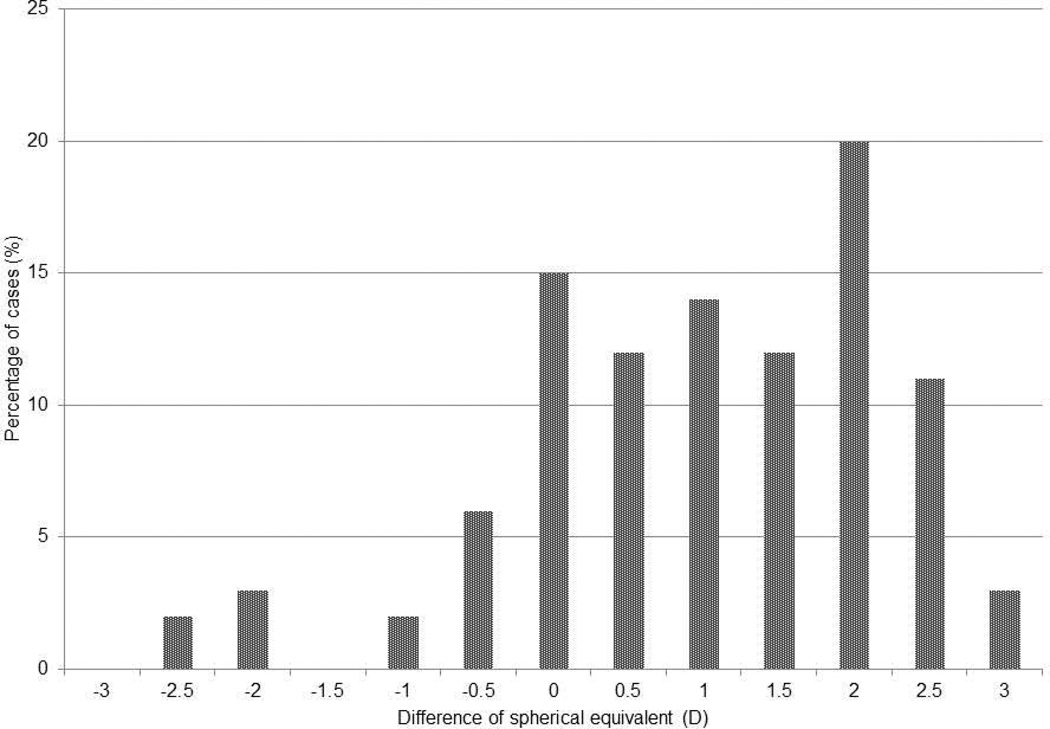
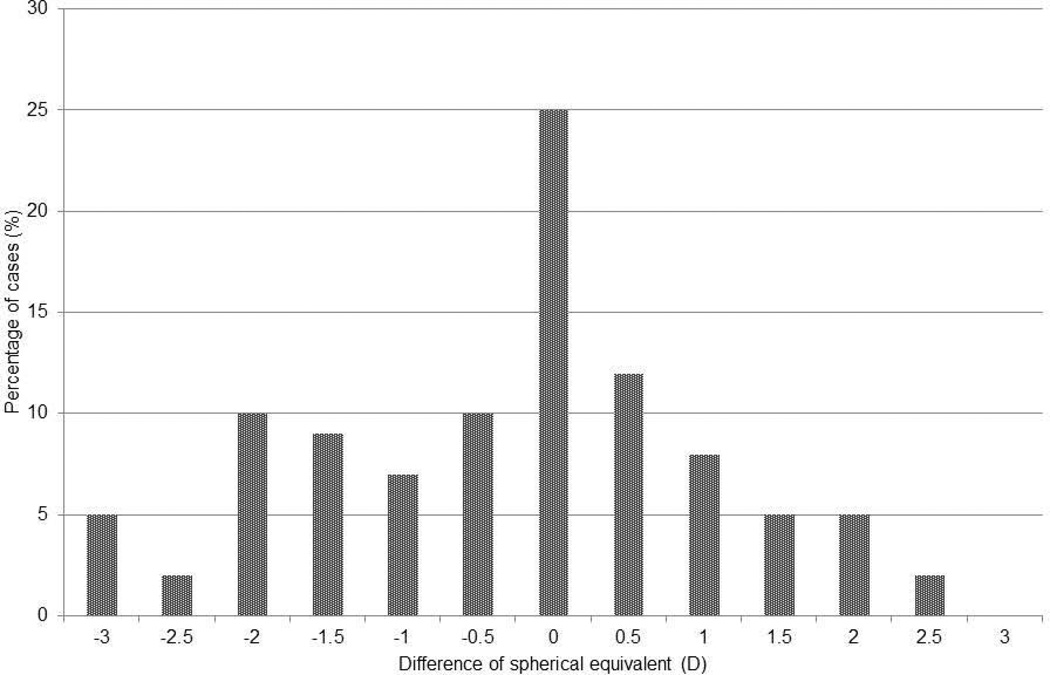
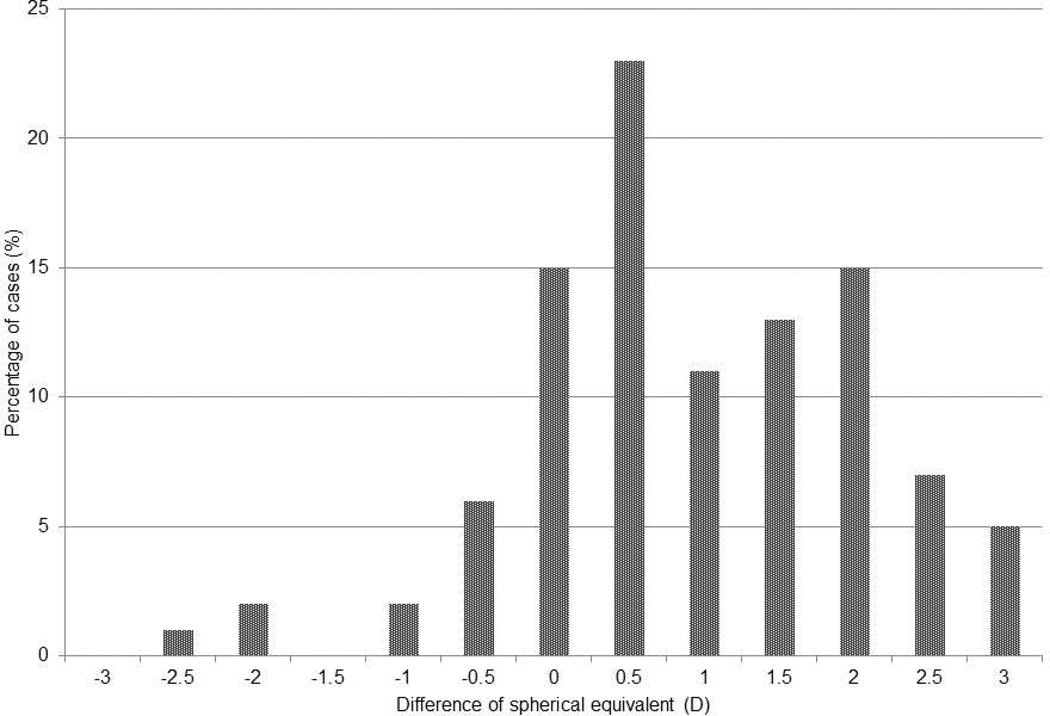
(Figure 1) Better agreement was seen between techniques when autorefraction was performed without cycloplegia, as shown by the greater % of values with DSE closer to zero in fig 1a and c. Mean reliability number was 4.6, 4.4 and 4.5 for SRH, ADG and combined, respectively. There was no significant relationship between DSE and the reliability number generated by the autorefractor (p=0.86 with correlation coefficient of −0.01, non-cyclopleged eyes, and p=0.13 with correlation coefficient −0.14 for cyclopleged eyes).
Figure 1.
Frequency distribution of the difference of spherical equivalents between autorefraction and retinoscopy: a, non-cyclopleged autorefractor versus cyclopleged retinoscopy; b, cyclopleged autorefractor versus non-cyclopleged retinoscopy; c, non-cyclopleged autorefractor versus non-cyclopleged retinoscopy; d, cyclopleged autorefractor versus cyclopleged retinoscopy. Each bar represents the percentage of results differing less than the amount displayed on the x-axis
Discussion
Retinoscopy is the “gold standard” method for objectively evaluating refractive error in humans and veterinary patients. Consistent with previous studies, we demonstrated that, when performed by experienced examiners, the repeatability of results using this technique in dogs is excellent. (6) We also objectively verified that cycloplegia does not affect the results of streak retinoscopy in dogs.
When non-cyclopleged autorefraction was compared to streak retinoscopy, the difference was statistically insignificant. This suggests that if further study supports autorefraction as a useful tool for estimating refractive error in dogs, it should be performed in non-cyclopleged eyes. In contrast, cyclopleged autorefraction produced results that were statistically different to those obtained through retinoscopy. The reason for this is unclear. Although autorefractors are designed for use in non-cyclopleged eyes, results in children using other autorefractor models indicated improved accuracy with cycloplegia. (11) Results of non-cyclopleged and cyclopleged eyes using the SureSight™ autorefractor have not been compared in children, to the author’s knowledge. It was suggested that cycloplegia improves the accuracy of autorefraction in children by eliminating the effect of accommodation. Excellent agreement between results of streak retinoscopy in non-cyclopleged and cyclopleged dogs indicates that this is probably a less important consideration in dogs. While we cannot explain the inaccuracy of cyclopleged autorefraction, we found that subjectively, the autorefractor provided readings more quickly, with less adjustment of focal distance in the smaller, non-dilated pupil. We theorize that a smaller pupil maintained focus on the same aspect of the fundic reflex, while a dilated pupil resulted in more movement artifact and variable results.
A statistically significant difference was found between results obtained by the two examiners using the auto-refractor. Interestingly, a greater interobserver difference was seen when measurements were taken under non-cyclopleged conditions. This deserves further study with a greater number of examiners. Operation of the Welch Allyn SureSight™ autorefractor was basic and readings could be obtained after minimal practice. Although not objectively evaluated, the average time to obtain two measurements from each eye was around 2–3 minutes. This was similar to the time required to obtain retinoscopy readings. The high-pitched noise emitted by the device, intended to guide focus by the operator and stimulate fixation by the patient, increased avoidance behaviour (looking away, becoming less compliant) in some of the dogs.
Acknowledgements
Welch Allyn, 4341 State Street Road, Skaneateles Falls, NY, kindly provided a SureSight™ autorefractor for use during this study.
Sources of funding: This study supported in part by Research to Prevent Blindness, NEI core grant NEI P30EY12576, National Science Foundation Office of Emerging Frontiers in Research and Innovation grant EFRI 0937847, the Comparative Ophthalmic Research Laboratories, and a generous donation by Pat Stoffers & family in memory of Sophie.
Footnotes
Limitations of this study include the relatively small sample size. This, as well as the statistically significant difference between results from individual examiners indicates that further study with a greater number of dogs and operators is required before this device can be considered useful in dogs. Cycloplegia does not significantly alter streak retinoscopy in dogs.
References
- 1.Kubai MA, Bentley E, Miller PE, et al. Refractive states of eyes and association between ametropia and breed in dogs. American Journal of Veterinary Research. 2008;69(7):946–951. doi: 10.2460/ajvr.69.7.946. [DOI] [PubMed] [Google Scholar]
- 2.Williams LA, Kubai MA, Murphy CJ, et al. Ocular components in three breeds of dogs with high prevalence of myopia. Optometry and Vision Science. 2011;88(2):269–274. doi: 10.1097/OPX.0b013e3182058ff0. [DOI] [PubMed] [Google Scholar]
- 3.Murphy CJ, Zadnik K, Mannis MJ. Myopia and refractive error in dogs. Investigative Ophthalmology and Visual Science. 1992;33(8):2459–2463. [PubMed] [Google Scholar]
- 4.Black J, Browning SR, Collins AV, et al. A canine model of inherited myopia: familial aggregation of refractive error in labrador retrievers. Investigative Ophthalmology and Visual Science. 2008;49(11):4784–4789. doi: 10.1167/iovs.08-1828. [DOI] [PubMed] [Google Scholar]
- 5.Mutti DO, Zadnik K, Murphy CJ. Naturally occurring vitreous chamber-based myopia in the Labrador retriever. Investigative Ophthalmology and Visual Science. 1999;40(7):1577–1584. [PubMed] [Google Scholar]
- 6.Davidson MG, Murphy CJ, Nasisse MP, et al. Refractive state of aphakic and pseudophakic eyes of dogs. American Journal of Veterinary Research. 1993;54(1):174–177. [PubMed] [Google Scholar]
- 7.Gift BW, English RV, Nadelstein B, et al. Comparison of capsular opacification and refractive status after placement of three different intraocular lens implants following phacoemulsification and aspiration of cataracts in dogs. Veterinary Ophthalmology. 2009;12(1):13–21. doi: 10.1111/j.1463-5224.2009.00667.x. [DOI] [PubMed] [Google Scholar]
- 8.Murphy CJ, Mutti DO, Zadnik K, et al. Effect of optical defocus on visual acuity in dogs. American Journal of Veterinary Research. 1997;58(4):414–418. [PubMed] [Google Scholar]
- 9.Ofri RD, Hollingsworth SR, Groth AD, et al. The effect of optical defocus on the performance of field trial retrievers. American Journal of Veterinary Research. doi: 10.2460/ajvr.73.4.546. in press. [DOI] [PubMed] [Google Scholar]
- 10.Iuorno JD, Grant WD, Noel LP. Clinical comparison of the Welch Allyn SureSight handheld autorefractor versus cycloplegic autorefraction and retinoscopic refraction. Journal of American Association for Pediatric Ophthalmology and Strabismus. 2004;8(2):123–127. doi: 10.1016/j.jaapos.2003.10.006. [DOI] [PubMed] [Google Scholar]
- 11.Choong YF, Chen AH, Goh PP. A comparison of autorefraction and subjective refraction with and without cycloplegia in primary school children. American Journal of Ophthalmology. 2006;142(1):68–74. doi: 10.1016/j.ajo.2006.01.084. [DOI] [PubMed] [Google Scholar]