Abstract
Cardiovascular imaging and procedures have experienced exponential growth over the past 20 years in terms of new modalities, procedure volume, technological sophistication, and cost. As a result, related quality improvement tools have become multifaceted works in progress. This article briefly summarizes the evolution of the time-honored American College of Cardiology Foundation/American Heart Association clinical practice guidelines versus the newer American College of Cardiology Foundation appropriate-use-criteria guidelines and how these may interact with emerging performance measures, clinical data registries, and cardiovascular laboratory accreditation initiatives.
Keywords: quality assessment, clinical practice guidelines, appropriate-use criteria, patient advocacy

R.F. Stainback, M.D.
Introduction
Quality in cardiovascular (CV) imaging and procedures is a multifaceted topic that may be regarded in terms of “dimensions of care” (Figure 1),1 a “chain of quality,” a “value equation” (Figure 2),2 and a “hierarchical model for diagnostic test efficacy”3 (Figure 3). Among the many medical-community stakeholders, consensus has only recently begun to emerge concerning how various quality constructs should be used in practice. This article briefly summarizes the evolution of the American College of Cardiology Foundation (ACCF)/American Heart Association (AHA) clinical practice guidelines (CPG) versus the newer ACCF appropriate-use-criteria (AUC) guidelines and their relationship to clinical performance measures, emerging clinical data registries, and laboratory accreditation. The CPG and AUC guidelines are continuously informed, updated, and improved by ongoing clinical trials, clinical outcomes, and comparative effectiveness research,4 leading to ever-improved CV quality, but this ongoing cycle remains a work in progress.
Figure 1.

Dimensions of care framework for evaluating quality of cardiovascular imaging. Adapted with permission from J Am Coll Cardiol, Volume 48, Douglas P et al.: Achieving quality in cardiovascular imaging: proceedings from the American College of Cardiology-Duke University Medical Center Think Tank on Quality in Cardiovascular Imaging, pages 2141–51, copyright Elsevier 2006.1
Figure 2.

Value equation for cardiovascular procedures. Was the right procedure done in the right way with the right outcome in a timely fashion? Adapted with permission from J Am Coll Cardiol, Vol. 60, Patel MR et al.: Appropriate use criteria to reduce underuse and overuse: striking the right balance, pages 1885–7, copyright Elsevier 2012.2
Figure 3.

Hierarchical model of diagnostic test evaluation.3 Adapted with permission from J Am Coll Cardiol, Vol. 63, Mark DB et al.: ACC/AHA/ASE/ASNC/HRS/IAC/Mended Hearts/NASCI/RSNA/SAIP/SCAI/SCCT/SCMR/SNMMI 2014 health policy statement on use of noninvasive cardiovascular imaging: a report of the American College of Cardiology Clinical Quality Committee, pages 698–721, copyright Elsevier 2014.4
During the past two decades, practicing physicians have witnessed an exponential growth in CV imaging and procedures in terms of new modalities, procedure volume, and technological sophistication and cost. In many ways, these developments have created a “golden era” of medicine associated with increased survival and quality of life. However, in some cases the wide dissemination of these technological innovations into clinical practice outstripped research directed towards understanding the optimal use of clinical resources.
The publication rate for CPGs and AUC guidelines has accelerated over the last 3 years (see Figure 4), and this can seem overwhelming to clinicians. Now that practitioners and hospitals are asked to address so many quality and reporting tasks, why are the AUC guidelines also needed? The fast pace of new guideline publications reflects technological innovation and outdating of previous documents; moreover, there is a new urgency within the profession to regulate itself regarding the evidence-based use of costly resources, as opposed to having regulations developed by nonexperts.
Figure 4.

Guideline mapping. The listed clinical practice guidelines (CPGs) and appropriate use criteria (AUC) guideline titles are abbreviated to save space. The listed active guidelines are available online at http://www.cardiosource.org/science-and-quality/practice-guidelines-and-quality-standards.aspx or https://my.americanheart.org/professional/StatementsGuidelines/ByTopic/TopicsA-C/ACCAHA-Joint-Guidelines_UCM_321694_Article.jsp. Solid arrows indicate previously published CPGs used to inform AUC clinical scenario development and the technical panel's evidence base for indication rating; dashed arrows indicate CPGs being written concurrently with AUC, which nonetheless informed AUC indication refinement and were then available to inform the AUC technical panel. Retired document (*), update or previous document (year*), unpublished but in progress AUC guideline (**). Shaded boxes: current imaging AUC; shaded dashed boxes: anticipated imaging AUC; SCD: sudden cardiac death; STEMI: ST-elevation myocardial infarction; periop: perioperative; CV: cardiovascular; USA: unstable angina; art: artery; abdom: abdominal; LE: lower extremity; EP: electrophysiology; SPECT/PET: single-photon emission computed tomography/positron emission tomography; CCT/CMR: cardiac computed tomography/cardiac magnetic resonance; TTE: transthoracic echocardiography; TEE: transesophageal echocardiography; US: ultrasound; ICD: implantable cardioverter defibrillation; CRT: cardiac resynchronization therapy; HD: heart disease; ED: emergency department.
Any physician may order noninvasive diagnostic CV testing, such as echocardiography, nuclear imaging, cardiac computed tomography (CT), and/or cardiac magnetic resonance (CMR) imaging. Invasive CV testing and therapeutic procedures are typically requested and/or performed by CV consultants, and these may include diagnostic catheterization, coronary and peripheral intervention, transcatheter aortic valve replacement, shunt closures and other percutaneous interventions, invasive electrophysiologic (EP) testing, arrhythmia ablation, and cardiovascular implantable electronic devices. This sizeable array of CV tests and procedures is represented within the many familiar CPGs (first published in 1984) and the newer AUC guidelines (first published in 2005) listed in Figure 4.
As patient advocates and stewards of medical resources, referring physicians may become more effective by consulting the AUC guidelines, as they have been developed to address patient populations as they are more likely to be encountered in real world practice situations. Before discussing the AUC guidelines, I will provide a brief overview of the CPGs, which are a concomitant and ongoing effort effort to improve CV care delivery.
ACCF/AHA Clinical Practice Guidelines
The familiar ACCF/AHA CPGs have been around for 30 years. The first one was published in 1984 after government regulators requested an evaluation of the available evidence and recommendations for standards to guide permanent pacemaker implantation5 due to concerns about possible overutilization. Since that time, more than 20 additional CPGs (Figure 3) have been published that primarily address diseases (e,g., arrhythmias, heart failure, myocardial infarction, etc.) as opposed to CV imaging and procedures per se. However, certain interventional procedures backed by a large body of scientific evidence (e.g., coronary revascularization and device-based EP procedures) are also represented in the CPGs. Ideally, the best available scientific evidence should inform clinical decision making. To this end, methodology for CPG development has undergone continuous refinement.6–8
Development of a CPG document begins with topic selection followed by a systematic literature search. Further steps include an exhaustive and time-consuming evidence review process, data synthesis, recommendation writing, an external review process, and eventual publication. Recommendations are written according to the time-honored format of class of recommendation (COR) for treatment approaches including the level of evidence (LOE) supporting the recommendation. The CORs for treatment strategies are Class I (benefit >>> risk), Class IIa (benefit >> risk), Class IIb (benefit > risk), and Class III (no benefit or harm). The highest-quality LOE (level A) indicates availability of multiple randomized controlled trials in multiple populations. Level B evidence is intermediate in quality, and level C evidence consists of expert consensus, limited-population studies, case studies, or standard of care.7,8 The CPGs are valuable documents that inform the following “derivative” quality products: performance measures, clinical registry development, AUC guidelines, public health policy legislation, and provider payment policies. One consequence of the rigorous CPG scientific methodology is a lengthy (but improving) development period of up to 2 to 3 years, with heretofore infrequent updates (Figure 4). In recent years, the challenge of avoiding outdated CPGs has been addressed by more rapid turn-around time and when needed “focused updates” (see Figure 4, STEMI 2004, 2007, 2014).
Interestingly, CPGs have not been developed for noninvasive cardiac imaging procedures per se. This is due to a lack of RCTs that support noninvasive cardiac imaging despite widespread acceptance, “standard-of-care” use in many cases, and the fact that CPGs have traditionally addressed primarily disease or interventional therapies. Recommendations for noninvasive cardiac imaging do exist within CPGs of various vintages, but they are not organized in a way that is readily assessable for clinicians or payers. For example, Figure 4 demonstrates that the most up-to-date recommendations for echocardiography appeared in at least 11 CPG guideline documents published between 2002 and 2011. In addition, CPG imaging recommendations have not included imaging recommendations linked to illness severity and follow-up testing. The AUC guidelines were developed, in part, to address these specific concerns.
Performance Measures
Performance measures are “derivative products” of the CPG's that are familiar to clinicians and hospitals, developed by a separate ACCF/AHA task force to further operationalize the CPGs.9 Performance measures are generally class I or III CPG recommendations with level of evidence A that are also measurable (e.g., left ventricular ejection fraction in heart failure), actionable, and strongly associated with improved patient outcomes.7 Quality concerns may be raised if the appropriate CPG recommendations are not provided for patients identified as meeting performance measure criteria. Public reporting and pay-for-performance programs are usually based on performance measures.10 Published performance-measure subjects include coronary artery disease, hypertension, heart failure, atrial fibrillation, and percutaneous coronary intervention. All of these guidelines are available at www.cardiosource.org/Science-and-Quality/Practice-Guidelines-and-Quality-Standards.aspx.
AUC Guidelines
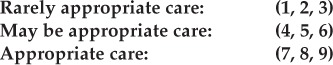
In comparison with the CPGs, the AUC guidelines are relatively new. The first “appropriateness” document, published in 2005,11,12 was in response to concern over the growing utilization and cost of noninvasive CV imaging and recognition that randomized clinical trials supported its use for only 2.5% of CPG recommendations. Figure 4 presents the current and upcoming roster for AUC guidelines. The first “appropriateness” document addressed nuclear cardiology11 followed by cardiac CT, cardiac MR (combined),13 echocardiography 2007 (transthoracic and transesophageal echo),14 and 2008 (stress echo).15 These initial guidelines were intentionally designed to cover only the most commonly encountered clinical scenarios in an attempt to make them more user friendly for clinicians. Because of advances in the clinical literature, the nuclear and echocardiography AUC documents were updated in 200916 and 2011,17 respectively, demonstrating the efficiency of the appropriateness method for rapid revisions. In 2009, “Appropriate Use Criteria” replaced the term “Appropriateness Criteria.”16 The initial appropriateness methods paper from 200512 was updated in 201318 to reflect transition to the term “AUC,” methodological refinements, and the adoption of “rarely appropriate,” “may be appropriate,” and “appropriate” for categorizing clinical scenarios and to address new multimodality AUC guidelines. With regard to detection and risk assessment of stable ischemic heart disease (the most frequent and costly CV condition encountered by physicians), nuclear imaging, stress echo, cardiac CT, cardiac MR, and diagnostic catheterization have all recently been updated within the first multimodality AUC guideline.19
Future AUC documents will address heart valve disease and cardiac structure/function from a similar multimodality imaging standpoint. The multimodality approach is a natural evolution for AUC guidelines because routine clinical evaluation is what leads to suspicion for CV disease. The physician then decides whether CV imaging is needed. In the real world, a physician must then decide which of the imaging modalities (if any) offers reasonable care for a particular patient based on local expertise, availability, diagnostic accuracy (heart rhythm, comorbidities, ability to exercise, body habitus, age, gender, etc.), safety concerns, and proven outcomes.
Methodology
The updated AUC methodology has been described in detail elsewhere,18 but a brief overview is included here. As with the CPGs, the first step in creating an AUC is topic selection. In deciding on a topic, the AUC task force committee considers a number of factors. After the topic has been selected, the AUC task force appoints a writing committee that systematically reviews the available evidence and maps relevant CPG recommendations to the proposed AUC indications (Figure 4). A literature search identifies new clinical evidence not covered in the CPGs and other consensus documents. Subspecialty organizations (e.g., in the fields of echocardiography,20 nuclear cardiology,21 CMR,22 or CCT23) have published an increasing array of modality-specific guidelines and recommendations that are impactful for clinical practice and distinct from the ACCF/AHA CPGs. The AUC writing committee develops an appropriate-use definition specific for the modality or procedure(s) in question, based on the general appropriate-use definition: “
An appropriate diagnostic or therapeutic procedure is one in which the expected clinical benefit exceeds the risks of the procedure by a sufficiently wide margin such that the procedure is generally considered acceptable or reasonable care.”18
The writing group then develops an extensive list of possible indications. A practical indication framework represents the most clinically relevant and common real-world scenarios likely to be encountered in clinical practice. The initial indication draft is critiqued by a diverse review panel consisting of more than 30 individuals, including physician experts and nonexpert referring physicians.
The writing group then edits the indications, based upon the review panel members' recommendations. This is a critical step, as the indications are subsequently evaluated by a rating panel (previously known as a technical panel) in accordance with a modified Delphi exercise12,24 and may not afterward be altered or adjusted. The rating panel members consist of “specialists using the technology and other professionals who are referrers, general cardiologists, outcome specialists, and/or generalists who care for germane patient populations, as well as the payer community.”18 Importantly, specialists whose primary area of clinical focus is the subject of the particular AUC document must comprise a minority of the rating-panel members. In the first round of rating, each panelist independently assigns a number to each clinical scenario according to this scale:
Thereafter, a face-to-face meeting is conducted, including all panelists, guided by a writing committee member and an AUC task force liaison representative. The final stage of the face-to-face meeting is a second round of rating after it has been established that the clinical scenarios and evidence are clear to all panel members. Indications then receive a final rating dictated by the median score, and previously described rules are followed to define and address rating dispersion (disagreement).12,24 The published AUC guideline for clinicians includes tables of all indications and their ratings. The published AUC indications only capture the most important clinical variables that describe relevant patient populations. Therefore, the AUC guideline indications must be used in combination with the clinical judgment that follows from a careful history, physical examination, and review of available data by a physician.
Data Registries
Data registries are germane to a discussion of AUC guidelines for the following reasons: in recent years, data registries have been used to assess AUC adherence, and registry data are used for outcomes research that, in turn, influences CPG and AUC guideline development. The National Cardiovascular Data Registry® (NCDR) was initially established in 1997 by the ACCF and multiple subspecialty societal partners.25 The NCDR's stated goal is to provide evidence-based process-of-care outcomes research and quality-of-care solutions (benchmark data, performance measures, site outcomes). More than 2,400 hospitals and nearly 1,000 outpatient providers participate in the NCDR registries.25 Participants must enter detailed patient and procedural data, including demographic information, history, risk factors, physician and facility provider characteristics, other diagnostic test results, treated conditions, equipment used, adverse events, and compliance with ACC/AHA CPGs and/or AUC guidelines, depending on the particular registry. Registry data are available for detailed process-of-care outcomes research and are invaluable for assessing treatment strategies for large patient populations.26
Registry participation comes at a cost in that it requires sites to provide adequately trained individuals to accurately record a large number of data points in an ongoing fashion over time. For example, since its 1998 inception, the CathPCI Registry has received more than 12 million records from 1,577 U.S. centers, and individual reports now consist of 250 data fields.27 Accordingly, streamlining the efficiency and quality of registry data is an ongoing process to avoid systemic errors in data quality and interpretation.28,29
Lab Accreditation
CPG and AUC guideline documents, data registries, health policies, and clinical-care decisions are based on an underlying assumption that the relevant CV imaging procedures are well performed and accurately interpreted. Are these valid assumptions? Within the six-level hierarchical model (Figure 3),3 laboratory accreditation addresses items 1 and 2 (technical and diagnostic accuracy efficacy); the additional elements of patient selection, reporting, and timely communication of results1 are represented in Figure 1. However, lab accreditation has only recently been “required” under certain circumstances. The 2008 Medicare Improvement for Patients and Providers Act (MIPPA) mandated that advanced diagnostic imaging labs run by private outpatient facilities (but not hospital inpatient facilities) be accredited by a CMS-approved accreditation organization by January 1, 2012, in order to bill under part B of the Medicare physician-fee schedule. According to this legislation, advanced diagnostic imaging includes MR, CT, and nuclear imaging (including positron emission tomography). The MIPPA does not address CV ultrasound imaging (echocardiography, peripheral vascular) or interventional procedures (e.g., cardiac catheterization or EP procedures). The framework for CMS oversight of accreditation organizations evaluates those organizations' minimum standards for personnel qualifications, equipment quality assurance, image accuracy, archival and reporting, and patient & personnel safety (including radiation exposure).30 There are now four CMS-approved accreditation organizations: the Intersocietal Accreditation Commission (IAC), American College of Radiology (ACR), Joint Commission and RadSite.31
The IAC32 provides accreditation for vascular ultrasound, vein centers, echocardiography, MR imaging, CT, nuclear cardiology, and carotid artery stenting, with the recent addition of electrophysiology laboratories. The ACR33 provides vascular ultrasound, MR imaging, CT, and nuclear cardiology lab accreditation. In recent years, IAC accreditation has been in a continuous state of development to improve standards and streamline processes. Obstacles to accreditation have been reduced significantly with the advent of web-based lab data submission and recognition of the need for less intrusive but more frequent and meaningful reaccreditation cycles. Ideally, the work and expense of meeting lab structure standards, including a quality improvement process, is offset by improved lab efficiency, more appropriate and accurate test performance, improved physician and patient satisfaction, and improved patient care (outcomes).
Conclusion
Clinicians may feel overwhelmed by the large number of quality tools and guidelines that have been published over the past few years. The goal of this summary is to contextualize the role of AUC guidelines within the larger framework of CV quality (Figures 1–3), including CPGs, performance measures, CV data registries, and lab accreditation. This review only briefly mentions the critical supporting roles for technical and medical staff training, credentialing, continuing education, equipment quality, and maintenance and the ongoing need for comparative effectiveness research. These additional quality elements fall under the purview of lab-accreditation organizations and/or relevant certification and licensing boards and professional societies, and they are assumed to be operational by physicians who refer patients to imaging or procedure labs. As patient advocates, referring clinicians should inquire about a lab's accreditation status or other quality improvement methods (if not accredited). The referring physician's greatest direct impact on quality is in selecting the most appropriate test for the right patient at the right time. The AUC guidelines provide a logistical framework for informing the ordering physician in this regard. The criteria themselves consist of relatively comprehensive tables of real-world clinical scenarios (indications) representing specific patient subgroups that are frequently encountered. For each AUC indication, a rating of “rarely appropriate,” “may be appropriate,” or “appropriate” is provided. This rating is determined by a methodology that incorporates well-supported CPG recommendations (guidelines mapping) and a scientific process for establishing expert opinion (the modified Delphi process) when scientific evidence or other guidance publications are lacking.
Implementation of the AUC guidelines remains a challenge. The AUC may be used as a tool for sampling the practice patterns of ordering physicians with the goal of spotting potential overuse and underuse. This would appear to be a realistic goal for now. Ultimately, a full complement of up-to-date AUC documents may be used to provide order-entry tools that can be integrated into practice-management systems (electronic health records). However, this application has several potential limitations that must be overcome. The AUC guidelines are intended to provide a starting framework for engaged and informed physicians who take into account the whole picture, including the realities of local practice environments and individual patient preferences. The AUC guidelines have been developed by physicians challenged with “self-regulating” their use of valuable CV-care resources. Such regulation is a complex problem, and solutions should be scientifically based. Although the AUC guidelines are increasingly used to inform various payment policies, they are not billing policies. They are designed to closely track the ACCF/AHA CPG recommendations, and efforts to harmonize related CPG and AUC publication schedules will reduce the issuance of conflicting guidelines. It is assumed that CV testing is performed in accredited laboratories. The AUC guidelines are used to supplement (not replace) well-informed, sound clinical judgment. Although “appropriate” indications frequently represent necessary and reasonable care, they are not always the same as “required” care. Patient preference may be an important consideration in determining whether or not a particular indication leads to testing.
The AUC guidelines and other guidance documents, registries, and standards discussed herein are “living” entities that require continual updating to minimize guidelines based on level of evidence “C,” to minimize rarely appropriate use, and to maximize appropriate use of CV imaging and procedures.
Footnotes
Conflict of Interest Disclosure: The author has completed and submitted the Methodist DeBakey Cardiovascular Journal Conflict of Interest Statement and none were reported.
Funding/Support: The author has no funding disclosures.
References
- 1.Douglas P, Iskandrian AE, Krumholz HM, Gillam L, Hendel R, Jollis J et al. Achieving quality in cardiovascular imaging: proceedings from the American College of Cardiology-Duke University Medical Center Think Tank on Quality in Cardiovascular Imaging. J Am Coll Cardiol. 2006 Nov 21;48(10):2141–51. doi: 10.1016/j.jacc.2006.06.076. [DOI] [PubMed] [Google Scholar]
- 2.Patel MR. Appropriate use criteria to reduce underuse and overuse: striking the right balance. J Am Coll Cardiol. 2012 Nov 6;60(19):1885–7. doi: 10.1016/j.jacc.2012.07.044. [DOI] [PubMed] [Google Scholar]
- 3.Fryback DG, Thornbury JR. The efficacy of diagnostic imaging. Med Decis Making. 1991 Apr–Jun;11(2):88–94. doi: 10.1177/0272989X9101100203. [DOI] [PubMed] [Google Scholar]
- 4.Mark DB, Anderson JL, Brinker JA, Brophy JA, Casey DE, Jr, Cross RR et al. ACC/AHA/ASE/ASNC/HRS/IAC/Mended Hearts/NASCI/RSNA/SAIP/SCAI/SCCT/SCMR/SNMMI 2014 health policy statement on use of noninvasive cardiovascular imaging: a report of the American College of Cardiology Clinical Quality Committee. J Am Coll Cardiol. 2014 Feb 25;63(7):698–721. doi: 10.1016/j.jacc.2013.02.002. [DOI] [PubMed] [Google Scholar]
- 5.Frye RL, Collins JJ, DeSanctis RW, Dodge HT, Dreifus LS, Fisch C et al. Guidelines for permanent cardiac pacemaker implantation, May 1984. A report of the Joint American College of Cardiology/American Heart Association Task Force on Assessment of Cardiovascular Procedures (Subcommittee on Pacemaker Implantation) Circulation. 1984 Aug;70(2):331A–9A. [PubMed] [Google Scholar]
- 6.American Heart Association [Internet] Dallas, TX: American Heart Association; c2104. Methodology Manual and Policies from the ACCF/AHA Task Force on Practice Guidelines; 2010 Jun [cited 2014 Jun 11]. Available from: https://my.americanheart.org/professional/StatementsGuidelines/PoliciesDevelopment/Development/Methodologies-and-Policies-from-the-ACCAHA-Task-Force-on-Practice-Guidelines_UCM_320470_Article.jsp. [Google Scholar]
- 7.Antman EM, Peterson ED. Tools for guiding clinical practice from the American Heart Association and the American College of Cardiology: what are they and how should clinicians use them? Circulation. 2009 Mar 10;119(9):1180–5. doi: 10.1161/CIRCULATIONAHA.109.856757. [DOI] [PubMed] [Google Scholar]
- 8.Jacobs AK, Kushner FG, Ettinger SM, Guyton RA, Anderson JL, Ohman EM et al. ACCF/AHA clinical practice guideline methodology summit report: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013 Jan 15;61(2):213–65. doi: 10.1016/j.jacc.2012.09.025. [DOI] [PubMed] [Google Scholar]
- 9.Spertus JA, Eagle KA, Krumholz HM, Mitchell KR, Normand SL, American College of Cardiology Foundation, American Heart Association Task Force on Performance Measures American College of Cardiology and American Heart Association methodology for the selection and creation of performance measures for quantifying the quality of cardiovascular care. Circulation. 2005 Apr 5;111(13):1703–12. doi: 10.1161/01.CIR.0000157096.95223.D7. [DOI] [PubMed] [Google Scholar]
- 10.Bonow RO, Masoudi FA, Rumsfeld JS, Delong E, Estes NA, 3rd, Goff DC, Jr et al. ACC/AHA classification of care metrics: performance measures and quality metrics: a report of the American College of Cardiology/American Heart Association Task Force on Performance Measures. Circulation. 2008;118(24):2662–6. doi: 10.1161/CIRCULATIONAHA.108.191107. [DOI] [PubMed] [Google Scholar]
- 11.Brindis RG, Douglas PS, Hendel RC, Peterson ED, Wolk MJ, Allen JM et al. ACCF/ASNC appropriateness criteria for single-photon emission computed tomography myocardial perfusion imaging (SPECT MPI): a report of the American College of Cardiology Foundation Quality Strategic Directions Committee Appropriateness Criteria Working Group and the American Society of Nuclear Cardiology endorsed by the American Heart Association. J Am Coll Cardiol. 2005 Oct 18;46(8):1587–605. doi: 10.1016/j.jacc.2005.08.029. [DOI] [PubMed] [Google Scholar]
- 12.Patel MR, Spertus JA, Brindis RG, Hendel RC, Douglas PS, Peterson ED et al. ACCF proposed method for evaluating the appropriateness of cardiovascular imaging. J Am Coll Cardiol. 2005 Oct 18;46(8):1606–13. doi: 10.1016/j.jacc.2005.08.030. [DOI] [PubMed] [Google Scholar]
- 13.Hendel RC, Patel MR, Kramer CM, Poon M, Hendel RC, Carr JC et al. ACCF/ACR/SCCT/SCMR/ASNC/NASCI/SCAI/SIR 2006 appropriateness criteria for cardiac computed tomography and cardiac magnetic resonance imaging: a report of the American College of Cardiology Foundation Quality Strategic Directions Committee Appropriateness Criteria Working Group, American College of Radiology, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, American Society of Nuclear Cardiology, North American Society for Cardiac Imaging, Society for Cardiovascular Angiography and Interventions, and Society of Interventional Radiology. J Am Coll Cardiol. 2006 Oct 3;48(7):1475–97. doi: 10.1016/j.jacc.2006.07.003. [DOI] [PubMed] [Google Scholar]
- 14.Douglas PS, Khandheria B, Stainback RF, Weissman NJ, Brindis RG, Patel MR et al. ACCF/ASE/ACEP/ASNC/SCAI/SCCT/SCMR 2007 appropriateness criteria for transthoracic and transesophageal echocardiography: a report of the American College of Cardiology Foundation Quality Strategic Directions Committee Appropriateness Criteria Working Group, American Society of Echocardiography, American College of Emergency Physicians, American Society of Nuclear Cardiology, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, and the Society for Cardiovascular Magnetic Resonance endorsed by the American College of Chest Physicians and the Society of Critical Care Medicine. J Am Coll Cardiol. 2007 Jul 10;50(2):187–204. doi: 10.1016/j.jacc.2007.05.003. [DOI] [PubMed] [Google Scholar]
- 15.Douglas PS, Khandheria B, Stainback RF, Weissman NJ, Peterson ED, Hendel RC et al. ACCF/ASE/ACEP/AHA/ASNC/SCAI/SCCT/SCMR 2008 appropriateness criteria for stress echocardiography: a report of the American College of Cardiology Foundation Appropriateness Criteria Task Force, American Society of Echocardiography, American College of Emergency Physicians, American Heart Association, American Society of Nuclear Cardiology, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, and Society for Cardiovascular Magnetic Resonance: endorsed by the Heart Rhythm Society and the Society of Critical Care Medicine. Circulation. 2008 Mar 18;117(11):1478–97. doi: 10.1161/CIRCULATIONAHA.107.189097. [DOI] [PubMed] [Google Scholar]
- 16.Hendel RC, Berman DS, Di Carli MF, Heidenreich PA, Henkin RE, Pellikka PA et al. ACCF/ASNC/ACR/AHA/ASE/SCCT/SCMR/SNM 2009 Appropriate Use Criteria for Cardiac Radionuclide Imaging: A Report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, the American Society of Nuclear Cardiology, the American College of Radiology, the American Heart Association, the American Society of Echocardiography, the Society of Cardiovascular Computed Tomography, the Society for Cardiovascular Magnetic Resonance, and the Society of Nuclear Medicine. J Am Coll Cardiol. 2009 Jun 9;53(23):2201–29. doi: 10.1016/j.jacc.2009.02.013. [DOI] [PubMed] [Google Scholar]
- 17.Douglas PS, Garcia MJ, Haines DE, Lai WW, Manning WJ, Patel AR et al. ACCF/ASE/AHA/ASNC/HFSA/HRS/SCAI/SCCM/SCCT/SCMR 2011 Appropriate Use Criteria for Echocardiography. A Report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, American Society of Echocardiography, American Heart Association, American Society of Nuclear Cardiology, Heart Failure Society of America, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, Society of Critical Care Medicine, Society of Cardiovascular Computed Tomography, and Society for Cardiovascular Magnetic Resonance Endorsed by the American College of Chest Physicians. J Am Coll Cardiol. 2011 Mar 1;57(9):1126–66. doi: 10.1016/j.jacc.2010.11.002. [DOI] [PubMed] [Google Scholar]
- 18.Hendel RC, Patel MR, Allen JM, Min JK, Shaw LJ, Wolk MJ et al. Appropriate use of cardiovascular technology: 2013 ACCF appropriate use criteria methodology update: a report of the American College of Cardiology Foundation appropriate use criteria task force. J Am Coll Cardiol. 2013 Mar 26;61(12):1305–17. doi: 10.1016/j.jacc.2013.01.025. [DOI] [PubMed] [Google Scholar]
- 19.Wolk MJ, Bailey SR, Doherty JU, Douglas PS, Hendel RC, Kramer CM et al. ACCF/AHA/ASE/ASNC/HFSA/HRS/SCAI/SCCT/SCMR/STS 2013 multimodality appropriate use criteria for the detection and risk assessment of stable ischemic heart disease: a report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, American Heart Association, American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Failure Society of America, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2014;63(4):380–406. doi: 10.1016/j.jacc.2013.11.009. [DOI] [PubMed] [Google Scholar]
- 20.American Society of Echocardiography [Internet] Morrisville, NC: American Society of Echocardiography; c2014. Guidelines and Standards; c2014 [cited 2014 Jun 11]. Available from: http://www.asecho.org/clinical-information/guidelines-standards/ [Google Scholar]
- 21.American Society of Nuclear Cardiology [Internet] Bethesda, MD: American Society of Nuclear Cardiology; c2011–2014. Clinical Guidelines and Quality Standards; c2009–2012 [cited 2014 Jun 11]. Available from: http://www.asnc.org/content_184.cfm?navID=73. [Google Scholar]
- 22.Society for Cardiovascular Magnetic Resonance [Internet] Mt. Royal, NJ: Society for Cardiovascular Magnetic Resonance; c2014. Documents and Guidelines; c2007–2013 [cited 2014 Jun 11]. Available from: http://www.scmr.org/Education/documents-and-guidelines.html. [Google Scholar]
- 23.Society of Cardiovascular Computed Tomography. Guidelines, Appropriate Criteria and Expert Consensus Documents. http://www.scct.org/tools/guidelines.cfm. Accessed April 10, 2014, 2014.
- 24.RAND Corporation [Internet] Santa Monica, CA: RAND Corporation; c1994–2014. Fitch K, Bernstein SJ, Aguilar MD, Burnand B, LaCalle JR, Lazaro P, et al. The RAND/UCLA Appropriateness Method User's Manual; c2001 [Cited 2014 Jun 11]. Available from: http://www.rand.org/pubs/monograph_reports/MR1269.html. [Google Scholar]
- 25.National Cardiovascular Database Registry [Internet] Washington, DC: American College of Cardiology Foundation; c2014. Available from: https://www.ncdr.com/webncdr/ [Google Scholar]
- 26.Masoudi FA, Ponirakis A, Yeh RW, Maddox TM, Beachy J, Casale PN et al. Cardiovascular care facts: a report from the national cardiovascular data registry: 2011. J Am Coll Cardiol. 2013 Nov 19;62(21):1931–47. doi: 10.1016/j.jacc.2013.05.099. [DOI] [PubMed] [Google Scholar]
- 27.Moussa I, Hermann A, Messenger JC, Dehmer GJ, Weaver WD, Rumsfeld JS et al. The NCDR CathPCI Registry: a US national perspective on care and outcomes for percutaneous coronary intervention. Heart. 2013 Mar;99(5):297–303. doi: 10.1136/heartjnl-2012-303379. [DOI] [PubMed] [Google Scholar]
- 28.Al-Khatib SM, Hellkamp A, Curtis J, Mark D, Peterson E, Sanders GD et al. Non-evidence-based ICD implantations in the United States. JAMA. 2011 Jan 5;305(1):43–9. doi: 10.1001/jama.2010.1915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Steinberg JS, Mittal S. The federal audit of implantable cardioverter-defibrillator implants: lessons learned. J Am Coll Cardiol. 2012 Apr 3;59(14):1270–4. doi: 10.1016/j.jacc.2011.12.026. [DOI] [PubMed] [Google Scholar]
- 30.U.S. Government Accountability Office [Internet] Washington, D.C.: U.S. Government Accountability Office; c2014. Medicare Imaging Accreditation: Establishing minimum national standards and an oversight framework would help ensure quality and safety of advanced diagnostic imaging services; 2013 May 31 [cited 2014 Jun 11]. Available from: http://www.gao.gov/products/gao-13-246. Accessed April 10, 2014, 2014. [Google Scholar]
- 31.Centers for Medicare & Medicaid Services [Internet] Baltimore, MD: Centers for Medicare & Medicaid Services; c2014. CMS approves three national organizations to accredit suppliers of advanced imaging services [press release]; 2010 Jan 28 [cited 2014 Jun 11]. Available from: https://www.cms.gov/Newsroom/MediaReleaseDatabase/Press-releases/2010-Press-releases-items/2010-01-28.html. [Google Scholar]
- 32.Intersocietal Accreditation Commission [Internet] Ellicott City, MD: Intersocietal Accreditation Commission; c2014. Getting Started with IAC Accreditation; c2014 [cited 2014 Jun 11]. Available from: http://www.intersocietal.org/iac/accreditation/gettingstarted.htm. [Google Scholar]
- 33.American College of Radiology [Internet] Reston, VA: American College of Radiology; c2014. Accreditation; c2014 [cited 2014 Jun 11]. Available from: http://www.acr.org/quality-safety/accreditation. [Google Scholar]


