Abstract
Pediatric solid organ transplant recipients are medically fragile and present with complex care issues requiring high-level management at home. Parents of hospitalized children have reported inadequate preparation for discharge, resulting in problems transitioning from hospital to home and independently self-managing their child’s complex care needs. The aim of this study was to investigate factors associated with the transition from hospital to home and chronic illness care for parents of heart, kidney, liver, lung, or multivisceral recipients. Fifty-one parents from five pediatric transplant centers completed questionnaires on the day of hospital discharge and telephone interviews at 3-week, 3-month, and 6-months following discharge from the hospital. Care coordination (p = .02) and quality of discharge teaching (p < .01) was significantly associated with parent readiness for discharge. Readiness for hospital discharge was subsequently significantly associated with post-discharge coping difficulty (p = .02) at 3-weeks, adherence with medication administration (p = .03) at 3-months, and post-discharge coping difficulty (p = .04) and family management (p = .02) at 6-months post-discharge. The results underscore the important aspect of education and care coordination in preparing patients and families to successfully self-manage after hospital discharge. Assessing parental readiness for hospital discharge is another critical component for identifying risk of difficulties in managing post-discharge care.
Keywords: pediatric, solid organ transplant, discharge transition
Introduction
Pediatric transplantation is an international effort; 1,540 children in the United States alone in 2013 underwent solid organ transplant (SOT)(1) billing an average of $425,000 for the transplant hospitalization.(2) Hospital readmissions are another costly component to medical care and recent changes in Medicare reimbursement penalize adult hospitals for high readmission rates.(3) Pediatric institutions are similarly focusing on readmission as a quality indicator.(4) In the pediatric population, there are a small percentage of medically complex children that account for the majority of hospital admission and costs. Furthermore, families of medically complex children with minimal resources including but not limited to access to care and family/caregiver resources may end up with more frequent readmissions.(4)
Pediatric SOT recipients are medically fragile and present with complex care issues requiring high-level management in the home. Parents of hospitalized children, including pediatric SOT recipients, have reported inadequate preparation for discharge, resulting in problems with transition from hospital to home and independently self-managing their child’s complex care needs.(5–8) SOT parents’ understanding of discharge teaching is essential for medication adherence and follow-up care.(9) Inaccurate medication administration and lack of close follow-up with the transplant team can result in unplanned emergency department (ED) visits and inpatient re-hospitalizations, including their associated cost.(10)
A focus on planned, coordinated, and supported discharge transition has resulted in decreased hospital readmission rates and cost of care in adult patients.(11–13) There are several projects focused on improving the ability of adult patients and their families to self-manage at home.(11–15) However, these national discharge transition projects have not addressed the needs of chronic illness in children and their families. Our previous work has reported that parents of pediatric SOT recipients with low readiness for hospital discharge subsequently reported more difficulty coping and adhering to the complex continuing care their children require at 3-weeks following hospital discharge.(16) Research on both discharge transition and family transition longitudinally is not presently addressed in the literature. This study extends the earlier research of this study team with the goal of identifying opportunities to enhance discharge transition care and improve the post-discharge experience and chronic illness management of SOT families.
Aims
The aim of this study was to investigate factors associated with the transition from hospital to home and chronic illness care defined as the first six months following hospital discharge for parents of SOT (heart, kidney, liver, lung, or multivisceral) recipients. Specifically our aims were to determine if:
Aim 1: Pre-discharge hospital care processes, specifically discharge teaching and care coordination are associated with parent perception of readiness for hospital discharge.
Aim 2: Parent readiness for hospital discharge lessens primarily three week post-discharge coping difficulty and secondarily later coping difficulties along with family impact, adherence to medication administration and medical regimen follow-up, and utilization of healthcare resources within the first six months following hospital discharge.
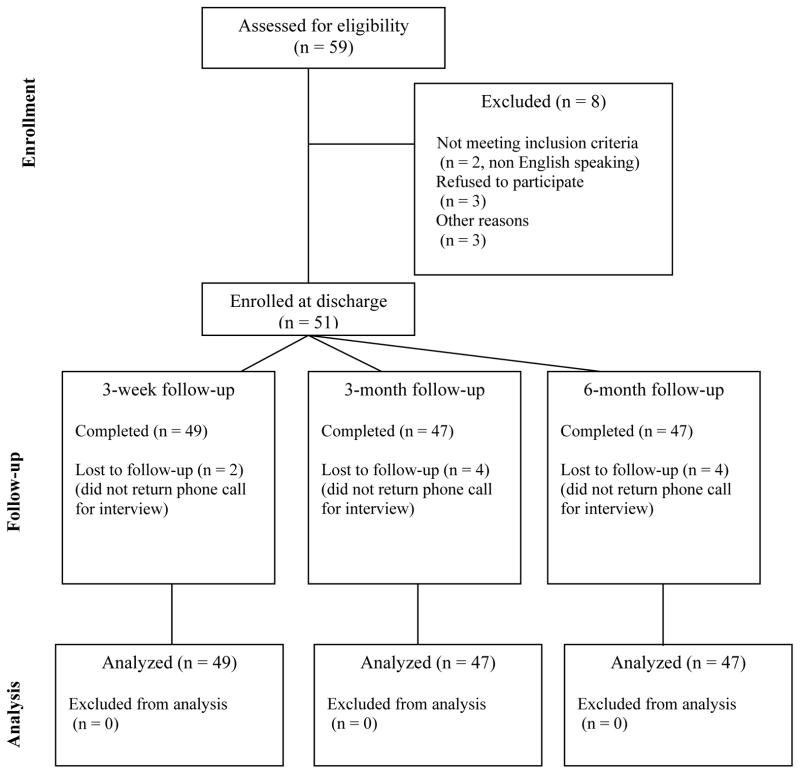
The conceptual framework and diagrammatic representation of the relationships tested to address the research questions are presented in Figure 1.
Figure 1.
Conceptual framework and study diagram
* indicates Meleis’ Transitions Theory components for listed study variables
Methods
Design
The study used an observational, prospective, longitudinal, correlational design replicating and extending the design of an earlier smaller study of a similar parent population.(16) Data from this earlier research was not included in this analysis. For this study, the sampling plan was extended to include additional study centers and SOT types (liver, lung, kidney, heart, and multivisceral) and the follow-up period for assessing family impact of the transplant experience was extended to include assessments at 3 and 6 months post-discharge.
Meleis’ Transitions theory provided an organizing framework for conceptualizing the transition from hospital to home and chronic illness care for parents of pediatric SOT recipients. The four major components of transition theory including Nature of the Transition, Transition Conditions, Nursing Therapeutics, and Patterns of Response(17) are represented by the study variables. The study examined the sequential relationships among pre- and post-discharge variables. The pre-discharge variables of discharge teaching and care coordination align with Nursing Therapeutics and post-discharge variables of readiness for hospital discharge, post-discharge coping difficulty, family impact, adherence to medication administration and medical regimen follow-up, and utilization of healthcare resources align with Patterns of Response. The hospitalization factors as well as parent and child characteristics were collected for descriptive purposes and represent the Nature of the Transition and Transition Conditions components of Transitions Theory (Figure 1).
Sample
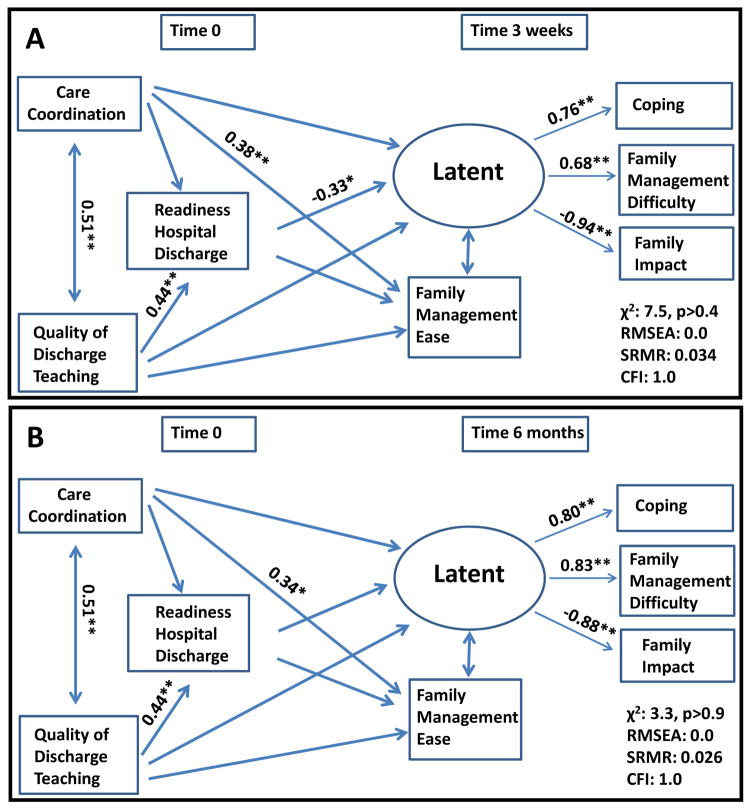
A convenience sample of 51 parents self-identified as the primary caregiver of a child who received a heart, kidney, liver, lung or multivisceral transplant at five major pediatric transplant centers were obtained between July 2010 and January 2012. Four participants were lost to follow-up over the six-month study period (Figure 2). Inclusion criteria consisted of the following: parents 18 years of age or older, English speaking, and a telephone to complete the three post-discharge interviews. Parents were excluded if the child had a previous transplant or extreme co-morbid conditions requiring significant skilled nursing care in the home including but not limited to conditions such as tracheostomy or ventilator dependence.
Figure 2.
Participant Enrollment Attrition Summary
Data Collection Procedures
Following Institutional Review Board approvals at all study sites, eligible parents were identified and contacted by their transplant coordinator to request voluntary participation and obtain informed consent. Parents completed written questionnaires on the day of hospital discharge; additional questionnaires were completed during a phone interview conducted by a research assistant unknown to the participant at three weeks, three months and six months post-discharge. Parents were given a gift card for completion of each portion of the study ($20 for the discharge questionnaire set and $40 for each post-discharge questionnaire set) to acknowledge time spent (20–80 minutes) in completing each data collection time point. The same parent completed all four data collection time points.
The discharge survey packet consisted of six questionnaires completed on the day of hospital discharge. Parents completed five questionnaires including: 1) Parent and Child Demographic Characteristics Form (i.e. parental marital status, age, race and gender), 2) Care Transition Measure,(18) 3) Quality of Discharge Teaching Scale,(19) 4) Parent Readiness for Hospital Discharge Scale,(20) and 5) PedsQL™ Family Impact Module.(21) The transplant coordinator at each institution completed the sixth form titled Hospitalization Characteristics (i.e. type of organ transplant, transplant-related complications including infection or rejection, unplanned return to the operating room, length of hospitalization, as well as number of medications and home medical care needs at the time of discharge). The discharge process was not standardized for purposes of this study, each center completed discharge education and preparation according to their routine process.
The post-discharge survey packet consisted of five questionnaires including: 1) Post Discharge Coping Difficulty Scale,(19) 2) Utilization of Healthcare Resources form, 3) PedsQL™ Family Impact Module,(21) 4) Family Management Measure,(22) and 5) Medical Adherence Measure.(23) Parents were contacted via telephone to schedule the interview on two separate occasions and deemed lost to follow-up if no reply was received. A schematic of study measures and data collection points is displayed in Figure 1.
Study Measures
Quality of Discharge Teaching Scale (QDTS)
Parent perspective on quality of discharge teaching provided by nurses during the hospitalization was measured with the QDTS. The QDTS is an18-item tool consisting of two subscales (content received and delivery). The content received subscale focuses on the amount of discharge education including information about medical care, knowledge about when and how to call the provider, care of the child at home, and parents’ emotions after discharge. The delivery subscale assesses parent perception of the way their child’s nurses provided discharge preparatory education. Parents rate both discharge education content and delivery of teaching received from the nursing staff on a scale of ‘0’ (none or not at all) to ‘10’ (a great deal or always) where higher scores indicate higher quality teaching. The Cronbach’s alpha reliability has ranged from .86 to .93 in samples of parents of solid organ transplant recipients and parents of hospitalized children as well as with the adult population.(16, 19, 24, 25)
Care Transition Measure (CTM)
Care coordination was defined as parent perception of healthcare team activities to ensure patient-centered planning and continuity of healthcare for the child and family in preparation for hospital discharge.(26) The CTM is a 15-item measure with four domains: transfer of information, preparation of patient/caregiver, self-management support, and empowerment to assert preferences.(27) The CTM uses a four-point Likert scale with scores ‘1’ (strongly disagree) to ‘4’ (strongly agree). The mean score for each respondent is linearly transformed to a 0–100 scale. Higher total scores indicate better transitional care coordination while lower scores are indicative of poorer quality care transition.(27)
The CTM was developed and validated in a sample of older adult patients who experienced a transition(27) and administered between 3 and 12 weeks after hospital discharge(14, 18). The Cronbach’s alpha reliability estimate was high (.93) and the CTM was able to successfully discriminate between patients discharged from the hospital who did and did not have a subsequent emergency department visit or re-hospitalization.(18) Wording of the CTM items was modified with permission for this study to specify the items for: 1) parent as respondent and 2) the time of administration as the day of hospital discharge. The Modified CTM had acceptable psychometric properties in a pediatric transplant population with a reported Cronbach’s alpha of .90.(16)
Readiness for Hospital Discharge Scale (RHDS)
The RHDS is a 29-item tool used to assess parents’ perceptions of readiness for discharge and is composed of five subscales: parent’s personal status, child’s personal status, knowledge, coping ability, and expected support. Each item is answered on a scale from ‘0’ (not at all) to ‘10’ (totally) where higher total scores are interpreted as greater readiness for hospital discharge. Cronbach’s alpha reliability estimates in various population groups including adult medical surgical patients, older adults, parents of hospitalized children, and parents of pediatric solid organ transplant recipients are high ranging from .84 to .92.(16, 20, 25, 28, 29) Construct validity was supported with group comparisons and confirmatory factor analysis. Predictive validity was supported as readiness for hospital discharge was associated with post-discharge difficulty coping.(16, 29)
Post Discharge Coping Difficulty Scale (PDCDS)
The PDCDS measures the degree of parental difficulty in coping with stress, recovery, self-care and management, confidence, support, and child adjustment after hospital discharge utilization.(19) The 10-item scale asks parents to rate individual items on a scale of ‘0’ (not at all) to ‘10’ (extremely, completely or a great deal) where higher scores indicate a parent experiencing more difficulty coping. Cronbach’s alpha reliability coefficient was .84 in a sample of parents of hospitalized children and .76 in a sample of parents of solid organ transplant recipients.(16, 28) Construct validity was supported through factor analysis and the predictive validity supported by the association of higher scores of PDCDS related to a higher post-discharge utilization.(28)
Utilization of Healthcare Resources Form
Unplanned utilization of healthcare resources, specifically emergency department and hospital readmission following hospital discharge through six months post-discharge, was obtained by parent report. Frequency of urgent care or emergency department visits and hospital readmissions were recorded in a dichotomous format (yes/no). Parent report was utilized as opposed to medical record review in order to capture all healthcare utilization in the event parents did not utilize a transplant center. Families were given tracking forms for each time phase of the study to help track health care related utilization occurrences.
Family Management
Family management was measured with two tools, PedsQL™ Family Impact Module and Family Management Measure. The PedsQL™ Family Impact Module is a 36-item measure comprised of eight dimensions: parent physical, emotional, social, cognitive functioning, communication, worry, daily activities, and family relationships.(21) Parents rate the degree each item has been a problem as a result of the child’s health on a 5-point scale ranging from ‘0’ (never) to ‘4’ (almost always). The scores are reverse coded and linearly transformed (0–100 scale) where higher scores indicate better parent or family functioning. The PedsQL™ Family Impact Module is able to distinguish between families with children with complex care needs and has a high Cronbach’s alpha of .97.(21)
The Family Management Measure (FaMM) measures how families manage care for a child with a chronic illness and incorporate condition management into everyday routine and family life. The 45-item tool assesses the dimensions of child identity, concern, difficulty, effort, and manageability with subscales score separately.(22) Higher scores indicate a more normal life and more readily manageable condition for the child daily life and condition management ability and parental mutuality subscales. Higher scores for the remaining subscales (condition management effort, family life difficulty, view of condition impact) indicate more effort, difficulty and greater concern to manage the illness.(22) Cronbach’s alpha reliability coefficients for all subscales range from .72 to .90.(22)
Adherence
The Medical Adherence Measure (MAM) is a semi-structured interview with modules to assess adherence to medication and clinic attendance over a 7-day period.(23, 30) Adherence was measured utilizing a dichotomous variable, adherent (yes) or non-adherent (no). Parents reporting any missed medications were classified as non-adherent.
Data Analysis
Analyses were conducted using SPSS version 21.0 .(31) Descriptive analyses were conducted to provide summary information regarding participant characteristics, hospital factors including inpatient complications and medical care needs at the time of hospital discharge, and study measure scale results. Data are summarized as median with range (minimum, maximum).
Spearman rho correlations (ρ) were calculated for the primary study variables measured on a continuous or ordinal scale to allow for a non-linear relationship. Mann-Whitney tests were used to test the differences in readiness for hospital discharge with adherence to medication administration and medical follow-up, emergency department visit and readmission to the hospital. The primary outcome for aim one was parent perception of readiness for hospital discharge. The primary outcome for aim two was three week coping difficulty. Probability levels of p < .05 were used for determining statistical significance in all analyses.
We initially investigated relationships among variables measured on continuous scales with linear regression, although the final model utilized structural equation modeling to better address the complexities of the multiple relationships between variables. Structural equation modeling as well as multilevel modeling were performed in M-PLUS (Version 5.21, Los Angeles, CA: Muthén & Muthén) to examine the study hypotheses. Exploratory factor analysis to investigate latent variables using principal component analysis extraction was completed. The latent outcome variable consists of post-discharge coping (PDCDS) and family management (including PedsQL™ Family Impact total scale and Family Management Measure Condition Management Effort Subscale). Structural equation modelings with the composite latent variable were performed at each time point (3 weeks, 3 months, and 6 months) initially and then for each variable independently. In order to take the longitudinal components into account, multilevel models with a random slope for each of the three variables (PDCDS total scale, PedsQL™ Family Impact Module total scale, and Family Management Measure Managing the Condition Subscale) were examined. For parameter estimations, maximum likelihood with conventional standard errors were used in structural equation modeling and maximum likelihood with standard errors approximated by first-order derivatives were used for the multilevel modeling. The following fit indices were used to evaluate model fit: model chi-square (χ2), root mean square error of approximation, standardized root mean square residual, and comparative fit index.
Results
Sample Description
Table 1 summarizes the sample characteristics. Parents were mostly Caucasian, married and female. Median parent age was 34.5 years (range 19–55) and median age of the transplanted patient was 3.2 years (range 3 weeks to 17.5 years).
Table 1.
Demographic and Medical Characteristics of the Study Population (n=51)
| N (%) | ||
|---|---|---|
|
| ||
| Organ Type | Liver | 19 (37) |
| Heart | 16 (31) | |
| Kidney | 10 (20) | |
| Multivisceral | 5 (10) | |
| Lung | 1 (2) | |
|
| ||
| Parent Gender | Female | 44 (86) |
| Male | 7 (14) | |
|
| ||
| Parent Age in Years (n=46) | Median | 34.5 |
| Range | 19–55 | |
|
| ||
| Parent and Child Race | White | 41 (81) |
| Black | 8 (16) | |
| Alaskan or American Indian | 2 (4) | |
|
| ||
| Parent Martial Status (n=50) | Married | 36 (72) |
| Single | 12 (24) | |
| Divorced | 1 (2) | |
| Widowed | 1 (2) | |
|
| ||
| Child Gender | Male | 26 (51) |
| Female | 25 (49) | |
|
| ||
| Child Age in Years | Median | 3.2 years |
| Range | 3 weeks to 17.5 years | |
|
| ||
| Inpatient number of days | Median | 14 |
| Range | 4–90 | |
|
| ||
| Unplanned return to Operating Room | Once | 4 (8) |
| Twice | 3 (6) | |
| ≥ Three | 3 (6) | |
|
| ||
| Hospitalization complications | Infection | 7 (14) |
| Rejection | 4 (8) | |
|
| ||
| Number of medications at time of hospital discharge | Median | 10 |
| Range | 5–21 | |
|
| ||
| Additional medical needs at time of hospital discharge | Wound care | 19 (37) |
| Enteral or tube feeding | 17 (33) | |
| Central line care | 15 (30) | |
| Drainage tube | 3 (6) | |
There were 14 individual patients (27%) with one or more complications defined as an unplanned return to the operating room, infection, and/or rejection. Patients were discharged from the hospital with a median of 10 medications (range 5–21). Additional medical care after discharge including wound care, enteral tube feeding, or central line care was reported in 30% of patients (Table 1). Comparisons of demographic and study measures by hospital, organ type, and child’s age revealed no significant differences.
Descriptive Statistics
Descriptive statistics for all measures are reported in Table 2. Parents reported high quality discharge teaching (QDTS) and care transition coordination (CTM) in preparing for the transition to home. On the QDTS, parents reported that nurses listened to their concerns with a median score of 10 (range = 2–10) and assured discharge instructions were understood reporting a median score of 10 (range = 4–10). The RHDS results indicated parents know about taking care of their child’s medical needs after going home reporting a median score of 9 (range = 5–10) and what problems to watch for after going home with a median score of 9 (range = 8–10). The lowest scoring item on the RHDS was amount of stress the parent was feeling on the day of hospital discharge with a median score of 4 (range = 0–10). Parents reported feeling ready to leave the hospital on the day of discharge reflected by the high score on RHDS.
Table 2.
Descriptive statistics for study measures
| Scale | Number of Items | Item Mean (SD) | Item Median (Min-Max) | Cronbach’s Alpha α |
|---|---|---|---|---|
|
| ||||
| Readiness for Hospital Discharge | 29 | 8.6 (0.7) | 8.7 (7.0 – 9.9) | .83 |
|
| ||||
| Quality of Discharge Teaching | 18 | 8.3 (1.4) | 8.6 (3.3–10.0) | .89 |
|
| ||||
| PedsQL™ Family Impact (Discharge) | 36 | 65.3 (15.7) | 67 (36–100) | .95 |
|
| ||||
| Care Transition Measure | 15 | 90 (10) | 96.7 (60–100) | .92 |
|
| ||||
| Post Discharge Coping Difficulty Scale (3-week) | 11 | 2.3 (1.3) | 2.2 (0.0–5.3) | .76 |
|
| ||||
| Family Management Measure (3-week) | ||||
| Child’s Daily Life | 5 | 3.1 (0.8) | 3.0 (1.4–4.8) | .65 |
| Condition Management Ability Scale | 12 | 4.0 (0.4) | 3.9 (3.3–4.9) | .52 |
| Condition Management Effort Scale | 4 | 3.8 (0.8) | 4.0 (2.0–5.0) | .51 |
| Family Life Difficulty | 14 | 2.3 (0.7) | 2.2 (1.0–3.8) | .87 |
| Parent Mutuality Scale | 8 | 4.3 (0.5) | 4.1 (3.1–5.0) | .74 |
| View of Condition Impact Scale | 10 | 2.8 (0.5) | 2.8 (1-3-3.7) | .58 |
| Scale | Heart α | Kidney α | Liver α | Complex α |
|---|---|---|---|---|
|
| ||||
| Readiness for Hospital Discharge | 0.88 | 0.83 | 0.82 | 0.80 |
|
| ||||
| Quality of Discharge Teaching | 0.94 | 0.72 | 0.84 | 0.94 |
|
| ||||
| PedsQL™ Family Impact (Discharge) | 0.90 | 0.95 | 0.97 | 0.95 |
|
| ||||
| Care Transition Measure | 0.94 | 0.94 | 0.89 | 0.95 |
|
| ||||
| Post Discharge Coping Difficulty Scale (3-week) | 0.65 | 0.38 | 0.81 | 0.77 |
|
| ||||
| Family Management Measure (3-week) | ||||
| Child’s Daily Life | 0.64 | 0.82 | 0.67 | 0.49 |
| Condition Management Ability Scale | 0.45 | 0.73 | 0.49 | 0.36 |
| Condition Management Effort Scale | 0.05 | 0.74 | 0.71 | 0.10 |
| Family Life Difficulty | 0.70 | 0.91 | 0.91 | 0.84 |
| Parent Mutuality Scale | 0.60 | 0.88 | 0.81 | 0.71 |
| View of Condition Impact Scale | 0.66 | 0.43 | 0.52 | 0.53 |
Readiness for Hospital Discharge and Quality of Discharge Teaching Scales administered on day of hospital discharge, all other tools administered at 3-weeks following hospital discharge.
Parents reported little difficulty coping after hospital discharge. When asked specifically about difficulty managing their child’s medical conditions, parents reported little difficulty at 3-weeks, median score of 1 (range = 0–6) and 6-months following discharge, median score of 1 (range = 0–7). Parents reported feeling confident in their ability to care for the child’s needs not only at 3-weeks following discharge with a median score of 10 (range = 5–10), but increasingly confident over time as indicated by the higher range at 6-months following discharge median score of 10 (range = 7–10). Worry remained consistent over time as parents reported worry about side effects of medications and medical treatments as well as worry about the child’s future the same at all three post-discharge follow-up time points with a median of 2 (range = 0–4).
Care Process Associations with Readiness for Hospital Discharge
Parent perception of care coordination (rho (ρ) = .34, p = .01) and quality of discharge teaching (ρ = .48, p < .01) were both significantly correlated with readiness for hospital discharge. The proposed relationships of care processes including care coordination and discharge teaching with parent readiness for hospital discharge were supported.
Readiness for Hospital Discharge and Post Discharge Outcomes
Readiness for hospital discharge was significantly correlated with post-discharge coping difficulty (ρ = −.37, p = <.01), impact on family using PedsQL™ Family Impact Module (ρ = 36, p = .01), and family management ease in managing child’s condition (ρ = .49, p < .001) at 3-weeks post discharge. These relationships were not maintained at 3 and 6 months post discharge.
Readiness for hospital discharge was not significantly associated with medication adherence at 3 weeks (p = .62) or 6 months (p = .38) post discharge, but was associated with medication adherence at 3 months post discharge (p = .03). Readiness for hospital discharge was not significantly correlated with emergency department visits at 3 weeks (p = .75), 3 months (p = .45) or 6 months (p = .39) after discharge from the hospital. Furthermore, readiness for hospital discharge was not significantly correlated with readmission to the hospital at 3 weeks (p = .34), 3 months (p = .81) or 6 months (p = .07) after discharge from the hospital.
The care process of quality of discharge teaching was not significantly directly correlated with any of the post-discharge outcomes measured, although care coordination was significantly correlated with post-discharge outcomes of Family Management child life subscale (ρ =.42, p < .01) and Family Management family life difficulty subscale (ρ = −.33, p = .02) at 3-weeks following hospital discharge. The relationship between care coordination and the family management measures were not maintained at 3 or 6 months post-discharge. Correlations are displayed in Table 3.
Table 3.
Correlation matrix for study variables
| CTM | RHDS | QDTS | PDCDS | Family Impact | FMMc | FMMfd | |
|---|---|---|---|---|---|---|---|
|
| |||||||
| QDTS | .54** | .48** | na | nd | nd | nd | nd |
|
| |||||||
| CTM | na | .34* | nd | nd | nd | nd | nd |
|
| |||||||
| PDCDS | |||||||
| 3 weeks | −.24 | −.37** | −.19 | na | −.68** | −.51** | .39** |
| 3 months | −.19 | −.25 | −.12 | −.69** | −.41** | .48** | |
| 6 months | −.13 | −.03 | −.08 | −.66** | −.31** | .37* | |
|
| |||||||
| Family Impact | |||||||
| 3 weeks | .24 | .36* | .22 | na | na | .66** | −.63** |
| 3 months | .17 | .27 | .15 | .62** | −.61** | ||
| 6 months | .17 | .19 | .11 | .54** | −.44** | ||
|
| |||||||
| FMMc | |||||||
| 3 weeks | .42** | .49** | .17 | na | na | na | na |
| 3 months | .14 | .28 | −.11 | ||||
| 6 months | .19 | .27 | −.01 | ||||
|
| |||||||
| FMMfd | |||||||
| 3 weeks | −.33* | −.27 | −.14 | na | na | na | na |
| 3 months | −.15 | −.10 | −.04 | ||||
| 6 months | −.13 | −.12 | −.07 | ||||
Notes: QDTS = Quality of Discharge Teaching Scale, CTM = Care Transition Measure, RHDS = Readiness for Hospital Discharge Scale, PDCDS = Post-Discharge Coping Difficulty Scale, FMMc = Family Management Measure Child’s Life Subscale, FMMfd = Family Management Measure Family Life Difficulty Subscale,
= p<.05,
=p<.01
Structural Equation Analysis
Readiness for hospital discharge increases as quality of discharge teaching increases (estimate of coefficient = 0.44, SE = 0.13, p < .01), although care coordination is not significant when included in the model (estimate of coefficient = 0.08, SE = 0.14, p = .58). Care coordination increases (estimate of coefficient = 0.30, SE = 0.13, p = 0.02) as readiness for hospital discharge increases when included separately.
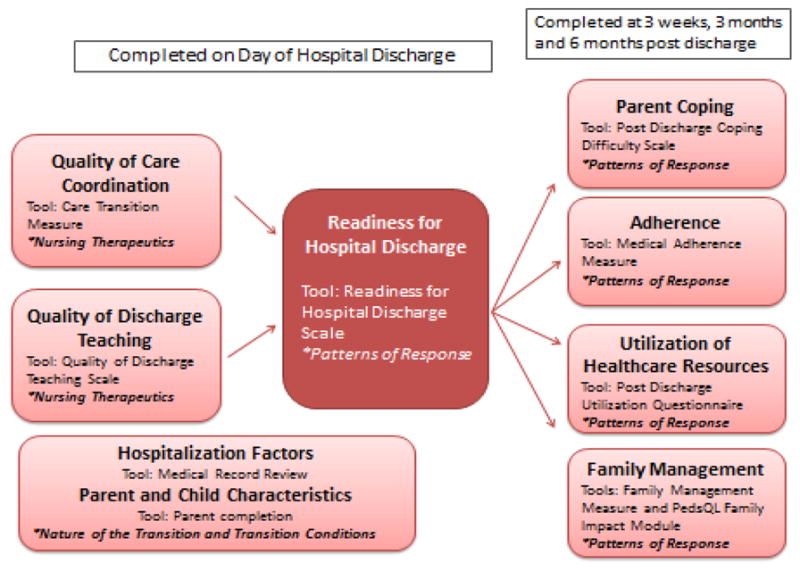
The latent group of post-discharge variables (Post Discharge Coping Difficulty Scale, Family Management Measure Managing Condition Effort Subscale and Family Impact total score) was significant with PDCDS p < .01, Family Management Measure Managing Condition Effort p < .01and PedsQL™ Family Impact Module p < .01. The structural equation standardized model at 3-weeks following hospital discharge indicated that Family Management condition management ability subscale increases as care coordination increases (estimate of coefficient = 0.38, SE = 0.14, p < .01). Moreover, the latent variable is negatively associated with readiness for hospital discharge (estimate of coefficient= −0.33, SE= 0.15, p = .03). The significant relationships identified through structural equation modeling are displayed in Figure 3A. When modeling for post discharge coping alone, as readiness for hospital discharge increases post discharge coping difficulty decreases (estimate of coefficient = −0.32, SE = 0.14, p = 0.02).
Figure 3.
Structural Equation Modelings showing significant effects with magnitude and significance level
*p<0.05
**p<0.01
There were no significant relationships identified utilizing structural equation modeling standardized model at 3-months following discharge. At 6-months following hospital discharge the standardized model results indicate that higher readiness for hospital discharge is related to improved Family Management ability and shown in Figure 3B (estimate of coefficient = 0.34, SE = 0.15, p = 0.03). Multilevel modeling for post-discharge coping (PDCDS) with random slope indicates that post-discharge coping difficulty decreased with higher readiness scores (estimate of coefficient = −0.24, SE = 0.12, p = 0.04).
Discussion
The sample for this study represents a range of a parents experiencing SOT and due to the sample composition, the results provide evidence of the commonalities of experience for these parents and not the specific medical care experiences associated with the specific organ type. The results of the study provide evidence that parent perception of readiness for hospital discharge is influenced by pre-discharge hospital care processes including care coordination and discharge teaching for parents of SOT recipients. Discharge teaching is the cornerstone for discharge preparation and safe transition home.(32–34) Knowledge and understanding of discharge instructions including medications have been targeted areas of study in the adult population(35) and lack of knowledge and medication discrepancies can lead to medical complications.(36) Quality of discharge teaching was not associated with readiness for hospital discharge for parents of pediatric SOT recipients in a smaller sample size,(16) but rose to significance in this larger study sample that also included parents of lung and multivisceral transplant recipients who have increased complexity of medical care.
Care coordination continues to be a crucial component for care of complex children within the home environment(37) as well as a national priority in the adult population(11–13, 38) yet, to date, less attention has been paid to the experience of discharge transition in the pediatric population. Parents’ perception of how well their care is coordinated is imperative to feeling ready for discharge and has important implications for parents of complex chronically ill children.(16) Education and care coordination are the fundamental components to reducing readmission rates in an adult hospital.(39) In the adult population, the CTM tool has been used in the post-discharge period to measure care coordination across the discharge transition, however it appears to have some utility for evaluation pre-discharge when patient reports of poor coordination are actionable in advance of discharge.
Exploring the relationships of readiness for hospital discharge and post discharge outcomes including coping, impact on family, adherence and utilization of healthcare resources were another aim of the study. Parents who were more ready to leave the hospital reported less difficulty coping and less impact on the family unit at three weeks following hospital discharge. Sustained improvement to family management and coping was noted at six months following hospital discharge for parents reporting higher readiness to leave the hospital. A parent feeling ready to leave the hospital enhances their ability to cope and overall decreases impact on the entire family. Family coping is essential to transplant care as significant stress has been documented in caregivers of transplant candidates.(40, 41) Parents of pediatric SOT recipients reported adjusting to a new normal including watching for complications as a critical component of coping after discharge in a qualitative study.(42) Assessment of family coping continues to be a meaningful endeavor by transplant programs as poor coping ability may lead to non-adherence with medication and medical follow-up regimen.
Adherence to the medication regimen was associated with readiness for discharge at the 3-month follow-up time point but not at the 3-week or 6-month follow-up. The ability to adhere to the medication regimen, central to the success of organ transplant, posed the biggest challenge at 3 months post discharge in relation to readiness for hospital discharge. There is no gold standard for measuring adherence highlighting the difficulties associated with measuring accurately.(43) This study measured adherence by self–report making this result challenging to interpret; however the results points to the importance of hospital discharge for the lengthy transition to continuing chronic care management.
Individual transplant centers participating in the study followed their respective standard post-discharge follow-up protocols. While the sample size was too small for accurately evaluating relationships of study variables to post-discharge utilization, the results did point to the possibility of an association of parent perception of readiness for hospital discharge with subsequent hospital readmission in the 6 months following discharge from the hospital. Further research with a larger sample size is indicated to ascertain if readiness to leave the hospital can serve as a risk indicator for hospital readmission and criterion for implementation of transitional support services. Studies with adult heart failure patients have shown that close follow-up by telephone or video phone resulted in prolonging time to readmission at 3 months post-discharge.(44)
Transplant patients are considered to have a chronic illness and deal on a daily basis with long-term medical follow-up and the recurring shift from illness-focused to health-focused needs.(45) Patient self-management plays a crucial role in assuring patients are equipped to handle the day-to-day medical management as well as stressors of having a chronic illness.(46) The study results underscore the important role of education and care coordination in preparing patients and families to successfully self-manage during the immediate transition to home recovery and chronic care management.
Strengths and Limitations
Strengths of this study include linking hospital processes inclusive of discharge teaching and care coordination with post-discharge outcomes, aligning with current national initiatives to improve patient centered outcomes and readmission reduction under the auspices of the Affordable Care Act.(3) Meleis’ Transitions Theory provided a framework to consider the discharge to home and chronic illness care process for patients and families.
A methodological limitation to the study is the fact that cause and effect relationships cannot be determined because it is not a randomized controlled trial design. This study is an observational correlational design looking at associations between hospital care processes, discharge teaching and care coordination, and post-discharge outcomes. However, the study does provide evidence of relationships that could be further explored in a larger randomized controlled trial design.
Further limitations include the need to use multiple centers to achieve enrollment of the study sample of children meeting study criteria should be considered in interpretation of the study findings. The individual organ groups represent an even smaller sample size, therefore the results must be considered within the group of pediatric solid organ transplant recipients and not individual organ types. The small sample size restricted the number of variables that could be included in regression analyses leading to analyses utilizing structural equation modeling. Furthermore, a minimum of 150 cases per model has been recommended, although structural equation modeling should not be ruled out for smaller samples.(47) In this case we only had one latent variable, the models were not complicated with regards to number of parameters estimated, and the measures of fit were good. The results will need validation.
Measurement of the constructs, many of which had been validated in the pediatric solid organ transplant population previously,(16) was a limitation. The Family Management Measure did not perform psychometrically as expected in this sample as only two of the six subscales reported a Cronbachs alpha greater than 0.7.(22) The tool has been validated for parents of children with a chronic illness and may not be appropriate for the situation of pediatric SOT recipients. Results related to the Family Management Measure should be interpreted cautiously. Further investigation of adherence following hospital discharge is indicated in order to further explore the relationship of readiness for hospital discharge and non-adherence. The use of multiple forms of adherence assessment as well as qualitative methodology may help to further elucidate the difficulties families face with medication administration in both the immediate and long-term time points following transplant.
Conclusion
The study revealed that better pre-discharge processes including discharge teaching and care coordination are associated with a parent feeling ready to take their child home from the hospital. Subsequently, parents who felt more ready to leave the hospital had less difficulty coping and overall impact of the illness of the family. Research in SOT has historically reviewed the clinical aspects of post-transplant medical management. The results of this study target the need for a quality of life focus in SOT(48) and support national efforts directed toward coordinated and planned discharge transitions. Care processes including discharge teaching and care coordination set the stage for readiness for discharge and the subsequent post-discharge outcomes for the parents and family of pediatric SOT recipients. Analyses of the concurrent qualitative component of this study and research with larger samples will further clarify these relationships and the overall role of family coping and successful management of the child’s chronic illness condition in the post-discharge period. Extension of this work should incorporate healthcare team perception of readiness for hospital discharge and the relationship to parent perception, consideration of family and patient needs as appropriate to patient age, and measurement of additional transplant-specific outcomes such as incidence of rejection. Parents of SOT recipients experience a dual transition in managing the acute and long-term needs of their child. The role of the transplant team should focus on the intersection of medical management and parent coping during both the acute transition to home and subsequent transition to chronic illness care.
Acknowledgments
This research is also supported by the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant Number 8UL1TR000055.
This research was supported by a grant from Children’s Research Institute Pilot Innovative Research Award.
Footnotes
Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
Author Contributions
S. Lerret was the primary author for this manuscript and was responsible for the following: concept and study design, data collection, data analysis and statistics, data interpretation, drafting article, critical revision of article, and approval of article for submission. Funding was secured by Children’s Research Institute Pilot Innovative Research Award.
M. Weiss was responsible for the following: assistance with concept and study design, data interpretation, critical revision of article, and approval of article for submission.
P. Simpson was responsible for the following: Study design, data analysis, data interpretation, article revision, and approval of article for submission.
M. Nugent was responsible for the following: Data analysis, data interpretation, article revision, and approval of article for submission.
G. Stendahl, S. Chapman, J. Menendez, K. Neighbors, K. Amsden, L. Williams, M. Nadler were responsible for the following: data collection, article revision, and approval of article for submission.
E. Alonso was responsible for the following: article revision and approval of article for submission.
References
- 1.Sharing UNfO. Transplants in the US By Recipient Age and Organ Type: Based on Optn Data as of December 3, 2013. no date. [Google Scholar]
- 2.Bentley TS, Hanson SG, Hauboldt RH. U.S. organ and tissue transplant cost estimates. Milliman Research Report. 2011;2011 [Google Scholar]
- 3.Kocher RP, Adashi EY. Hospital readmissions and the Affordable Care Act: Paying for corridnated quality care. JAMA. 2011;306:1794–1795. doi: 10.1001/jama.2011.1561. [DOI] [PubMed] [Google Scholar]
- 4.Srivastava R, Keren R. Pediatric readmissions as a hospital quality measure. JAMA. 2013;309:396–398. doi: 10.1001/jama.2012.217006. [DOI] [PubMed] [Google Scholar]
- 5.Benning CR, Smith A. Psychosocial needs of family members of liver transplant patients. Clinical Nurse Specialist. 1994;8:280–288. [PubMed] [Google Scholar]
- 6.Bent KN, Keeling A, Routson J. Home from the PICU: Are parents ready? American Journal of Maternal Child Nursing. 1996;21:80–84. doi: 10.1097/00005721-199603000-00011. [DOI] [PubMed] [Google Scholar]
- 7.Snowdon WW, Kane DJ. Parental needs following the discharge of a hospitalized child. Pediatric Nursing. 1995;21:425–428. [PubMed] [Google Scholar]
- 8.Baker AL. The transition home for preterm infants: Parent’s perceptions. Neonatal Network. 1991:65. [Google Scholar]
- 9.Steinberg TG, Diercks MJ, Millspaugh J. An evaluation of the effectiveness of a videotape for discharge teaching of organ transplant recipients. Journal of Transplant Coordination. 1996;6:59–63. doi: 10.7182/prtr.1.6.2.e720443244wxv3p1. [DOI] [PubMed] [Google Scholar]
- 10.Fine RN, Webber SA, Olthoff KM, Kelly DA, Harmon WE. Pediatric solid organ transplantation. Malden: Blackwell Publishing; 2007. [Google Scholar]
- 11.Naylor MD, Brooten D, Campbell R, et al. Comprehensive discharge planning and follow-up of hospitalized elders: A randomized clinical trial. JAMA. 1999;281:613–620. doi: 10.1001/jama.281.7.613. [DOI] [PubMed] [Google Scholar]
- 12.Jack BW, Chetty VK, Anthony D, et al. A reengineered hospital discharge program to decrease rehospitalization: A randomized trial. Annals of Internal Medicine. 2009;150:178–187. doi: 10.7326/0003-4819-150-3-200902030-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Naylor MD, Brooten D, Campbell RL, Maislin G, McCauley KM, Schwartz JS. Transitional care of older adults hospitalized with heart failure: A randomized, controlled trial. Journal of the American Geriatrics Society. 2004;52:675–684. doi: 10.1111/j.1532-5415.2004.52202.x. [DOI] [PubMed] [Google Scholar]
- 14.Coleman EA, Smith JD, Frank JC, Min SJ, Parry C, Kramer AM. Preparing patients and caregivers to participate in care delivered across settings: The care transitions intervention. Journal of the American Geriatrics Society. 2004;52:1817–1825. doi: 10.1111/j.1532-5415.2004.52504.x. [DOI] [PubMed] [Google Scholar]
- 15.Coleman EA, Parry C, Chalmers SA, Min SJ. The care transition intervention: Results of a randomized clinical trial. Archives of Internal Medicine. 2006;166:1822–1828. doi: 10.1001/archinte.166.17.1822. [DOI] [PubMed] [Google Scholar]
- 16.Lerret SM, Weiss ME. Parents of pediatric solid organ transplant recipients and the transition from hospital to home following solid organ transplant. Pediatric Transplantation. 2011;15:606–616. doi: 10.1111/j.1399-3046.2011.01536.x. [DOI] [PubMed] [Google Scholar]
- 17.Meleis AI, Sawyer LMI, EO, Messias DK, Schumacher K. Experiencing transitions: An emerging middle-range theory. Advances in Nursing Science. 2000;23:12–28. doi: 10.1097/00012272-200009000-00006. [DOI] [PubMed] [Google Scholar]
- 18.Coleman EA, Mahoney E, Parry C. Assessing the quality of preparation for posthospital care from the patient’s perspective: The care transitions measure. Medical Care. 2005;43:246–255. doi: 10.1097/00005650-200503000-00007. [DOI] [PubMed] [Google Scholar]
- 19.Weiss M, Johnson NL, Malin S, Jerofke T, Lang C, Sherburne E. Readiness for discharge in parents of hospitalized children. Journal of Pediatric Nursing. 2008;23:282–295. doi: 10.1016/j.pedn.2007.10.005. [DOI] [PubMed] [Google Scholar]
- 20.Weiss ME, Piacentine LB. Psychometric properties of the readiness for hospital discharge scale. Journal of Nursing Measurement. 2006;14:163–180. doi: 10.1891/jnm-v14i3a002. [DOI] [PubMed] [Google Scholar]
- 21.Varni JW, Sherman SA, Burwinkle TM, Dickinson PE, Dixon P. The PedsQL™ family impact module: Preliminary reliability and validity. Health and Quality of Life Outcomes. 2004;2:Article 55. doi: 10.1186/1477-7525-2-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Knafl K, Deatrick J, Gallo A, et al. Assessment of the psychometric properties of the family management measure. Journal of Pediatric Psychology. 2011;36:494–505. doi: 10.1093/jpepsy/jsp034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zelikovsky N, Schast AP. Eliciting accurate reports of adherence in a clinical interview: Development of the medical adherence measure. Pediatric Nursing. 2008;34:141–146. [PubMed] [Google Scholar]
- 24.Weiss ME, Piacentine LB, Lokken L, et al. Perceived readiness for hospital discharge in adult medical-surgical patients. Clinical Nurse Specialist. 2007;21:31–42. doi: 10.1097/00002800-200701000-00008. [DOI] [PubMed] [Google Scholar]
- 25.Bobay K, Jerofke T, Weiss M, Yakusheva O. Age-related differences in perception of quality of discahrge teaching adn readiness for hospital discharge. Geriatric Nursing. 2010;31:178–187. doi: 10.1016/j.gerinurse.2010.03.005. [DOI] [PubMed] [Google Scholar]
- 26.Coordination NCoC. Toward a care coordination policy for America’s older adults. 2008. [Google Scholar]
- 27.Coleman EA, Smith JD, Frank JC, Eilertsen TB, Thiare JN, Kramer AM. Development and testing of a measure desinged to assess the quality of care transitions. International Journal of Integrated Care. 2002;2:1–9. doi: 10.5334/ijic.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Weiss M, Johnson NL, Malin S, Jerofke T, Lang C, Sherburne E. Readiness for discharge in parents of hospitalized children. Journal of Pediatric Nursing. 2008;23:282–295. doi: 10.1016/j.pedn.2007.10.005. [DOI] [PubMed] [Google Scholar]
- 29.Weiss M, Yakusheva O, Bobay K. Nurse and patient perceptions of discharge readiness in relation to post discharge utilization. Medical Care. 2010;48:482–486. doi: 10.1097/MLR.0b013e3181d5feae. [DOI] [PubMed] [Google Scholar]
- 30.Zelikovsky N, Schast AP, Palmer J, Meyers K. Perceived barriers to adherence among adolescent renal transplant candidates. Pediatric Transplantation. 2008;12:300–308. doi: 10.1111/j.1399-3046.2007.00886.x. [DOI] [PubMed] [Google Scholar]
- 31.SOFTWARE] Sc. SPSS. 15.0. Chicago: SPSS Inc; 2006. [Google Scholar]
- 32.Smith J, Liles C. Information needs before hospital discharge of myocardial infarction patients: A comparitive, descriptive study. Journal of Clinical Nursing. 2007;16:662–671. doi: 10.1111/j.1365-2702.2006.01689.x. [DOI] [PubMed] [Google Scholar]
- 33.Maloney LR, Weiss ME. Patients’ perceptions of hospital discharge informational content. Clinical Nursing Research. 2008;17:200–219. doi: 10.1177/1054773808320406. [DOI] [PubMed] [Google Scholar]
- 34.Clark PA, Drain M, Gesell SB, Mylod DM, Kaldenberg DO, Hamilton J. Patient perceptions of quality in discharge instruction. Patient Education and Couseling. 2005;59:56–68. doi: 10.1016/j.pec.2004.09.010. [DOI] [PubMed] [Google Scholar]
- 35.Cumbler E, Wald H, Kutner J. Lack of patient knowledge regarding hospital medications. Journal of Hospital Medicine. 2010;5:83–86. doi: 10.1002/jhm.566. [DOI] [PubMed] [Google Scholar]
- 36.Corbett CF, Setter SM, Daratha KB, Neumiller JJ, Wood LD. Nurse identified hospital to home medication discrepancies: Implications for improving transitional care. Geriatric Nursing. 2010;31:188–196. doi: 10.1016/j.gerinurse.2010.03.006. [DOI] [PubMed] [Google Scholar]
- 37.Looman WS, Presler E, Erickson MM, et al. Care coordination for children with complex special health care needs: The value of the advanced practice nurse’s enhanced scope of knowledge and practice. Journal of Pediatric Health Care. 2013;27:293–303. doi: 10.1016/j.pedhc.2012.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Daly BJ, Douglas SL, Kelley CG, O’Toole E, Montenegro H. Trial of a disease managment program to reduce hospital readmissions of the chronically critically ill. Chest. 2005;128:507–517. doi: 10.1378/chest.128.2.507. [DOI] [PubMed] [Google Scholar]
- 39.Markley J, Andow V, Sabharwal K, Wang Z, Fennell E, Dusek R. A project to reengineer discharges reduces 30-day readmission rates. American Journal of Nursing. 2013;113:55–64. doi: 10.1097/01.NAJ.0000431922.47547.eb. [DOI] [PubMed] [Google Scholar]
- 40.Zelikovsky N, Schast AP, Jean-Francois D. Parent stress and coping: Waiting for a child to receive a kidney transplant. Journal of Clinical Psychology in Medical Settings. 2007;14:320–329. [Google Scholar]
- 41.Bolden L, Wicks MN. The clinical utility of the Stress Process Model in family caregivers of liver transplant candidates. Progress in Transplantation. 2008;18:74–79. doi: 10.1177/152692480801800203. [DOI] [PubMed] [Google Scholar]
- 42.Lerret SM, Weiss ME, Stendahl G, et al. Transition from hospital to home following pediatric solid organ transplant: Qualitative findings of parent experience. Pediatric Transplantation. 2014;18:527–537. doi: 10.1111/petr.12269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fine RN, Becker Y, DeGeest S, et al. Nonadherence consensus conference summary report. American Journal of Transplantation. 2009;9:35–41. doi: 10.1111/j.1600-6143.2008.02495.x. [DOI] [PubMed] [Google Scholar]
- 44.Wakefield BJ, Ward MM, Homan JE, et al. Evaluation of home telehealth following hospitalizaiton for heart failure: A randomized trial. Telemedicine and e-Health. 2008;14:753–760. doi: 10.1089/tmj.2007.0131. [DOI] [PubMed] [Google Scholar]
- 45.Paterson BL. The shifting perspectives model of chronic illness. Journal of Nursing Scholarship. 2001;33:21–26. doi: 10.1111/j.1547-5069.2001.00021.x. [DOI] [PubMed] [Google Scholar]
- 46.De Geest S, Dobbels F, Gordon E, De Simone P. Chronic illness management as an innovative pathway for enhancing long-term survival in transplantation. American Journal of Transplantation. 2011;11:2262–2263. doi: 10.1111/j.1600-6143.2011.03714.x. [DOI] [PubMed] [Google Scholar]
- 47.Holbert RL, Stephenson MT. Structural equation modeling in the communication sciences, 1995–2000. Human Communication Research. 2002;28:531–551. [Google Scholar]
- 48.Bartosh SM, Ryckman FC, Shaddy R, Michaels MG, Platt JL, Sweet SC. A national conference to determine reserach priorities in peidatirc solid organ transplantation. Pediatric Transplantation. 2008;12:153–166. doi: 10.1111/j.1399-3046.2007.00811.x. [DOI] [PubMed] [Google Scholar]