Abstract
Introduction
Bariatric surgery as treatment of type 2 diabetes mellitus (T2DM) in morbidly obese patients is becoming common. Although a large number of studies demonstrating high efficacy of bariatric methods in diabetics with body mass index (BMI) < 35 kg/m2 have been published, this promising solution is still not accepted enough even in the era of a diabetes offensive.
Aim
To analyze the dynamics of T2DM remission in patients with BMI < 35 kg/m2 and > 35 kg/m2 after Roux-en-Y gastric bypass (RYGB).
Material and methods
Data of 30 patients with BMI < 35 kg/m2 and 82 with BMI > 35 kg/m2 who underwent RYGB between 2007 and 2010 were collected from a prospectively designed database. The laboratory resolution of T2DM was determined by fasting plasma glucose (FPG ≤ 100 mg/dl) and glycosylated hemoglobin (HbA1c ≤ 6%).
Results
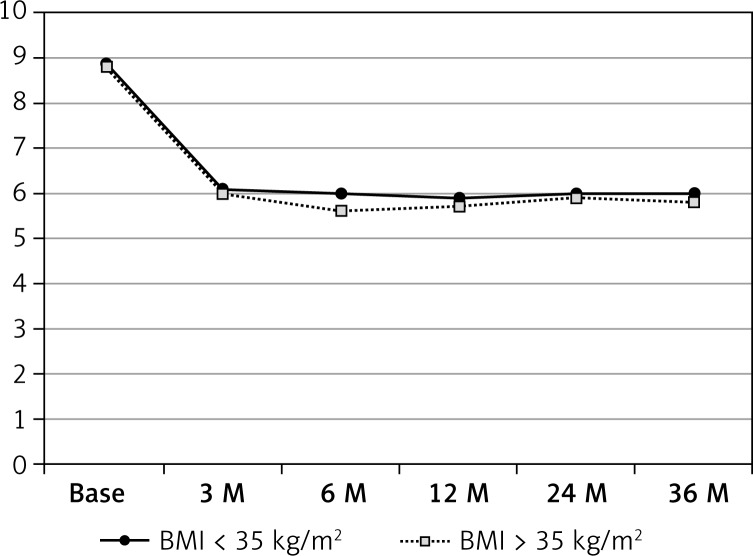
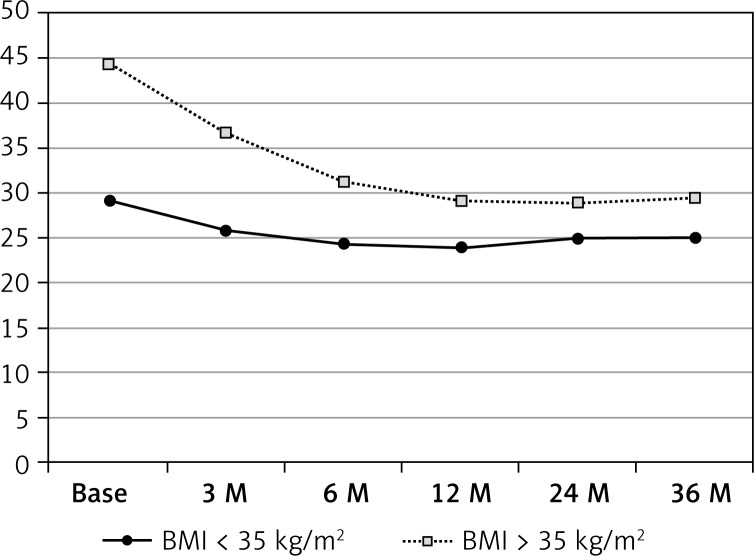
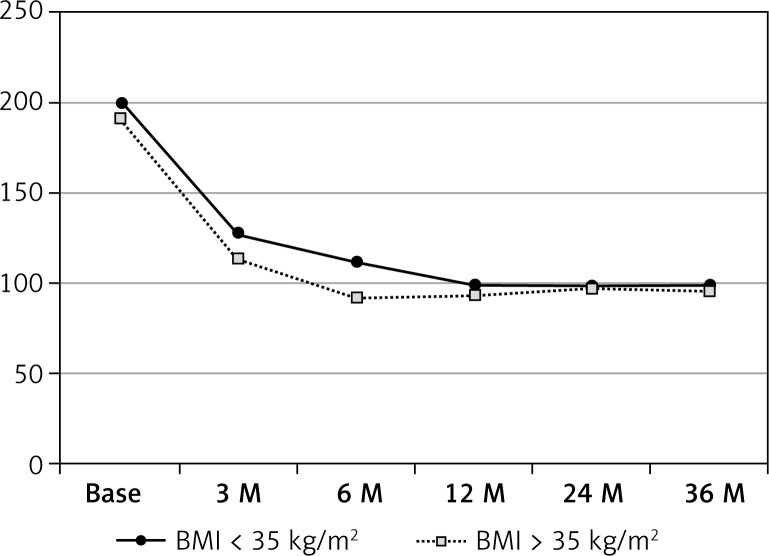
The T2DM regression was observed in 80% of the patients with BMI < 35 kg/m2 and 83% in a group with BMI > 35 kg/m2 1 year after RYGB and about 80% 2 and 3 years after the operation in both groups. Normalization of average HbA1c and FPG was observed in the BMI > 35 kg/m2 group after 3 months, while in the BMI < 35 kg/m2 group it was reached 6 months postoperatively. Changes in main markers of T2DM were parallel with the BMI decrease 3–12 months after RYGB, but early resolution in some patients was observed independently of weight loss.
Conclusions
The mid-term observation of patients after RYGB revealed the laboratory remission of T2DM. Ultimate evaluation of T2DM markers 3 years after surgery demonstrates high effectiveness of RYGB in managing T2DM in both groups.
Keywords: type 2 diabetes mellitus, remission, Roux-en-Y gastric bypass, surgical treatment, body mass index below 35 kg/m2
Introduction
Type 2 diabetes mellitus (T2DM) has been recognized as one of the leading plagues of the modern world. While in 1995, there were 135 million people affected by this disease, the approximate prognosis for 2030 seems to be devastating – the number of patients suffering from T2DM is expected to be nearly tripled [1, 2]. In developed countries, diabetes is now the fourth leading cause of death [2]. Type 2 diabetes mellitus is the main medical condition in people with chronic renal failure [2]. It was estimated that more than 2.5 million individuals developed diabetic retinopathy [2]. In Poland alone, annually, about 14 000 patients undergo distal lower limb amputations annually due to diabetes-related micro-angiopathy [3]. People with T2DM are more than twice as likely to have a heart attack or stroke compared to non-diabetics [1, 2]. Estimated global healthcare expenditures to treat and prevent diabetes and its complications are projected to exceed USD 490 billion by the year 2030 [1, 2, 4].
These alarming data call for more intensive diabetes management and encourage the search for new alternatives to current sub-effective therapies [5]. The observation of the postoperative course of bariatric patients with concomitant T2DM demonstrated a very high rate of long lasting resolution of type 2 diabetes already in the late nineties [6, 7]. What was recognized as potentially curative for pathologically obese diabetics could also be beneficial for patients with mild obesity or even overweight, ineffectively treated for T2DM [8]. In March 2011 during the 2nd Congress on Interventional Therapies for T2DM in 2011 in New York, a multidisciplinary team of reputable specialists developed an agenda of research priorities to set a new consensus on the role of gastrointestinal surgery in T2DM treatment in obese and non-obese patients [9].
Since the results of the two most important randomized trials comparing conservative with surgical treatment of T2DM were published in 2012, the number of bariatric procedures for diabetic patients with different body mass index (BMI) has increased worldwide [8–11].
Aim
The aim of the study was to evaluate the impact of Roux-en-Y gastric bypass(RYGB) on diabetes resolution in patients with BMI < and > 35 kg/m2 in a 3-year observation period. We attempted to define the dynamics of change of the main diabetic laboratory markers glycated hemoglobin (HbA1c) and fasting plasma glucose (FPG) during weight loss following surgery.
Material and methods
Data of 112 patients with T2DM who underwent RYGB between September 2007 and December 2010 were collected in a prospectively designed database. Eighty-two of them had BMI higher than 35 kg/m2 (mean BMI = 44.2 kg/m2), and 30 had BMI lower than 35 kg/m2 (mean BMI = 29.1 kg/m2). The BMI value was calculated during the initial visit. Patients were followed up 3, 6, 12, 24 and 36 months postoperatively. There were 21 women and 9 men in the group with BMI < 35 kg/m2 and 50 women and 32 men in the group with BMI > 35 kg/m2. The procedure of RYGB was chosen for all of the patients because of its potential curative metabolic effect in T2DM. Diabetic patients with BMI lower than 35 kg/m2 were referred for surgery by diabetologists due to ineffective conservative treatment of T2DM, while the dominant indication in group BMI > 35 kg/m2 was obesity. The indication criteria for RYGB for morbidly obese individuals are well established worldwide [12]. The conditions that should be met to select patients below 35 kg/m2 BMI for surgical treatment within a clinical study are listed in Table I, following the IDF statement [13]. The preoperative period lasted 3–4 months and was based on cooperation with a psychologist, dietician, diabetologist and bariatric surgeons. During this period at least 2 visits with each of the specialists were obligatory to optimize general conditions of the patients at the time of surgery and prepare them to follow the postoperative dietary indications.
Table I.
Inclusion/exclusion criteria for patients with BMI < 35 kg/m2
| Inclusion criteria | Exclusion criteria |
|---|---|
|
|
At each follow-up point apart from the BMI, the most significant markers of glycemia control acknowledged by leading diabetes associations were assessed – glycosylated hemoglobin (HbA1c %) and fasting plasma glucose (FPG mg %) [14]. In all cases, the preoperative HbA1c and FPG were determined. In addition, the type and dose of the antidiabetic drugs and the duration of the disease were noted. HbA1c and FPG levels were measured 3, 6, 12, 24 and 36 months after the surgery. Many other laboratory parameters were estimated regularly after the operation to estimate the efficacy of the treatment and prevent nutritional deficiencies, but have not been presented here not to blur the basic idea of the study.
All patients underwent RYGB. Sixty-five of them underwent a laparoscopic procedure (LRYGB) and 47 an open procedure (ORYGB). Regardless of the approach, the technical aspects of the procedures were the same. The size of the pouch was measured during the obligatory methylene blue test and ranged from 35 ml to 45 ml. Intestinal anastomosis was performed after the exclusion of biliopancreatic limb (BPL) average 109 cm with digestive limb (DL) 154 cm in the BMI > 35 kg/m2 group, and the proportion BPL/DL in the BMI < 35 kg/m2 group was close to the average of 100/100 cm. The size of the limbs was adjusted to the BMI of the patients with BMI > 35 kg/m2 but in some cases the anatomical conditions played the deciding role. Hence the main goal in BMI < 35 kg/m2 patients was not intense weight loss, and the length of both loops was set at about 100 cm.
The follow-up visits were executed by a multidisciplinary team at the above-mentioned time points. The glycemia markers were all assessed in the same laboratory. The National Institutes of Health (NIH) guidelines define normal FPG as ≤ 100 mg % and the “nondiabetic” range of HbA1c as 4.0–6.0 [15]. The laboratory T2DM remission has been established following NIH criteria for patients who discontinued using diabetic medications.
Group characteristics are summarized in Table II.
Table II.
Group characteristics
| Base conditions | BMI < 35 kg/m2 | BMI > 35 kg/m2 | Value of p |
|---|---|---|---|
| Number of cases | 30 | 82 | |
| Male/female | 9/21 | 32/50 | |
| Average age [years] | 46.4 ±11.2 | 48.5 ±10.9 | 0.3920 |
| Patients on insulin therapy [%] | 46.6 | 39.0 | |
| Average disease duration [years] | 7.9 ±3.91 | 6.8 ±3.63 | 0.1678 |
| Average HbA1c [%] | 8.9 ±0.81 | 8.8 ±1.01 | 0.6269 |
| Average FPG [mg%] | 199 ±34.47 | 190 ±41.91 | 0.3112 |
| Average C-peptide level [µg/l] | 1.9 ±0.89 | 2.5 ±1.02 | 0.0053 |
| Average BMI [kg/m2] | 29.1 ±2.15 | 44.2 ±5.49 | < 0.00001 |
| Mean size of pouch [ml] | 45 ±0.99 | 38.5 ±1.02 | 0.0001 |
| Average length of BP/digestive loop [cm] | 98.4/105.9 ±12.53/14.12 | 108.6/154.2 ±13.19/18.20 | 0.004/ < 0.0001 |
The spectrum, methodology and assumptions of the study were accepted by a local bioethical committee at the Medical University of Gdansk, Poland.
Statistical analysis
Statistical analysis was performed with Statistica software licensed for the Medical University of Gdansk. Data at individual time points were compared using t-tests. Statistical significance was considered for p < 0.05.
Results
All 112 patients were followed up according to the schedule of the study. There were no intra- or postoperative deaths. Gastrointestinal leak as the most serious complication was observed in 2 patients from the BMI > 35 kg/m2 group. The first leak was localized in the site of the staple line of the remnant stomach. It required reoperation and closure on the second postoperative day. The stenosis of the pouch-jejunal anastomosis 12 months after the procedure was the reason of late pouch – cutaneous fistula in another case. Endoscopic dilatation of the anastomosis with self-expanding stent implantation and intense parenteral nutrition for 6 weeks was safe and effective in fistula closure. Control endoscopy 1 year after RYGB showed ulceration in the region of anastomosis in 6% to 10% of patients in both groups, which were successfully treated conservatively. All the postoperative complications and the most common adverse events reported during the postoperative follow-up visits are listed in Table III.
Table III.
Adverse events and complications
| Variables | BMI < 35 kg/m2 | BMI > 35 kg/m2 |
|---|---|---|
| Number of cases | 30 | 82 |
| Gastrointestinal leak or fistula | 0/30 | 2/82 (2.4%) |
| Anastomotic stenosis | 1/30 | 1/82 (1.2%) |
| Ulceration in anastomosis | 3/30 (10%) | 5/82 (6.1%) |
| Wound infection | 1/30 (3%) | 4/82 (4.9%) |
| Incisional hernia | 0/30 | 2/82 (2.4%) |
| Anemia Hb < 10 g% | 0/30 | 2/82 (2.4%) |
| Pneumonia | 0/30 | 1/82 (1.2%) |
| Hypoglycemic episode | 12/30 (40%) | 31/82 (37.8%) |
| Reoperation | 0/30 | 3/82 (3.6%)^ |
| Endoscopic intervention | 1/30 (3%) | 2/82 (2.4%) |
| Intens. conservative treatm. | 1/30 (3%)* | 2/82 (2.4%)*,# |
| Extensive vomiting | 0/30 | 1/82 (1.2%) |
| Dumping | 1/30 (3%) | 6/82 (7.3%) |
| Reflux symptoms | 0/30 | 1/82 (1.2%) |
| Prolonged diarrhea | 0/30 | 4/82 (4.9%) |
| Malnutrition | 0/30 | 1/82 (1.2%)# |
Patients experienced symptomatic hypoglycemia episode with glucose level < 50 mg/dl and required iv fluid administration and diet correction during 1-day hospital stay
1 patient required re-hospitalization and parenteral and enteral feeding due to symptomatic hypoproteinemia.
One reoperation due to leak, 2 due to incisional hernia
About 40% of the patients in both groups reported clinical symptoms of hypoglycemic episodes but in only 2 patients who required intensive medical treatment accidental plasma glucose was below 50 mg%.
The laboratory regression of T2DM based on HbA1c during the first follow-up visit (3 months after surgery) was observed in 27% of the BMI < 35 kg/m2 group and in 52% of the BMI > 35 kg/m2 group (p = 0.0162). In the vast majority of these patients an FPG level lower than 100 mg% was observed during the hospital stay after surgery. The average HbA1c during the first follow-up visit was 6.1% and 6.0% in the group with BMI < 35 kg/m2 and the group with BMI > 35 kg/m2 respectively (p = 0.362). The decrease of the FPG from the baseline was statistically more significant in the group of patients with BMI > 35 kg/m2: 17% vs. 50% of the cases (p = 0.028). A further decrease in both parameters was observed in both groups at the next follow-up visit 6 months after surgery; statistically significant differences were noted between groups. At this point laboratory regression of T2DM was observed in close to 80% of patients from the BMI > 35 kg/m2 group, while still 13/90 (43%) patients from the BMI < 35 kg/m2 group had HbA1c higher than 6%.
Delayed improvement in HbA1c in relation to FPG seems to reflect the fact that it illustrates glycemia control from previous weeks, rather than the current status as FPG. The values of HbA1c and FPG at the next follow-up visits, 1, 2 and 3 years postoperatively, demonstrated further decrease or stabilization and did not differ between the studied groups. About 80% of all cases presented HbA1c and FPG below or equal to the threshold established as non-diabetic. The average of HbA1c and FPG in both groups did not differ significantly in the two final follow-up visits. The values of the above-mentioned parameters are detailed in Tables IV–VI.
Table IV.
Glycated hemoglobin (HbA1c) change
| HbA1c | –%Δ HbA1c | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| BMI < 35 kg/m2 | SD | BMI > 35 kg/m2 | SD | BMI < 35 kg/m2 vs. BMI > 35 kg/m2 p | BMI < 35 kg/m2 | SD | BMI > 35 kg/m2 | SD | BMI < 35 kg/m2 vs. BMI > 35 kg/m2 p | |
| Base | 8.9 | 0.81 | 8.8 | 1.01 | 0.6269 | |||||
| 3 M | 6.1 | 0.49 | 6.0 | 0.52 | 0.3623 | 31.5 | 3.58 | 31.2 | 2.84 | 0.5630 |
| 6 M | 6.0 | 0.26 | 5.6 | 0.24 | < 0.0001 | 32.5 | 3.41 | 36.4 | 3.40 | < 0.0001 |
| 12 M | 5.9 | 0.15 | 5.7 | 0.29 | 0.0068 | 33.7 | 3.20 | 35.2 | 3.12 | 0.0272 |
| 24 M | 6.0 | 0.49 | 5.9 | 0.37 | 0.2498 | 32.5 | 3.58 | 33.0 | 3.58 | 0.5267 |
| 36 M | 6.0 | 1.21 | 5.8 | 0.81 | 0.3222 | 32.5 | 4.78 | 34.1 | 4.22 | 0.0893 |
Table VI.
Percentage of patients in laboratory T2DM remission
| 3 months | 6 months | 12 months | 24 months | 36 months | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| BMI < 35 kg/m2 | BMI > 35 kg/m2 | BMI < 35 kg/m2 | BMI > 35 kg/m2 | BMI < 35 kg/m2 | BMI > 35 kg/m2 | BMI < 35 kg/m2 | BMI > 35 kg/m2 | BMI < 35 kg/m2 | BMI > 35 kg/m2 | |
| FPG < 100 mg% | 5/30 (16.6%) | 41/82 (50%) | 15/30 (50%) | 65/82 (79.3%) | 24/30 (80%) | 68/82 (82.9%) | 23/30 (76.6%) | 64/82 (78.1%) | 23/30 (76.6%) | 64/82 (78.1%) |
| t-Test | 0.0028 | 0.006 | 0.376 | 0.387 | 0.387 | |||||
| HbA1c < 6% | 8/30 (26.7%) | 43/82 (52%) | 17/30 (56.7%) | 66/82 (81%) | 24/30 (80%) | 68/82 (82.9%) | 24/30 (80%) | 66/82 (80.5%) | 24/30 (80%) | 64/82 (78.1%) |
| t-Test | 0.0162 | 0.008 | 0.376 | 0.460 | 0.282 | |||||
Table V.
Fasting plasma glucose (FPG) change
| FPG | –%Δ FPG | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| BMI < 35 kg/m2 | SD | BMI > 35 kg/m2 | SD | BMI < 35 kg/m2 vs. BMI > 35 kg/m2 p | BMI < 35 kg/m2 | SD | BMI > 35 kg/m2 | SD | BMI < 35 kg/m2 vs. BMI > 35 kg/m2 p | |
| Base | 199.1 | 34.47 | 190.4 | 41.91 | 0.3112 | |||||
| 3 M | 127.7 | 24.41 | 113.4 | 28.17 | 0.0154 | 35.9 | 3.91 | 40.4 | 2.82 | 0.0010 |
| 6 M | 111.6 | 17.48 | 91.6 | 8.78 | 0.0001 | 43.9 | 3.30 | 51.8 | 3.24 | < 0000.1 |
| 12 M | 98.5 | 12.47 | 93.4 | 10.86 | 0.0368 | 50.5 | 3.40 | 50.9 | 3.41 | 0.5833 |
| 24 M | 98.4 | 11.99 | 96.5 | 10.18 | 0.3824 | 50.6 | 4.11 | 49.4 | 3.82 | 0.1517 |
| 36 M | 98.9 | 14.73 | 95.2 | 12.75 | 0.1950 | 50.3 | 5.35 | 50.0 | 4.87 | 0.7791 |
The dynamics of change in both diabetic markers observed in all patients after RYGB paralleled the progress in change of BMI. More severe BMI reduction was obviously observed in the group of individuals with morbid obesity. None of treated patients reached the BMI delimited for the underweight (Table VII). The dynamics of change in the investigated parameters are shown in Figures 1–3.
Table VII.
Body mass index (BMI) change
| BMI | –%Δ BMI | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| BMI < 35 kg/m2 | SD | BMI > 35 kg/m2 | SD | BMI < 35 kg/m2 vs. BMI > 35 kg/m2 p | BMI < 35 kg/m2 | SD | BMI > 35 kg/m2 | SD | BMI < 35 kg/m2 vs. BMI > 35 kg/m2 p | |
| Base | 29.1 | 2.15 | 44.2 | 5.49 | < 0.00001 | |||||
| 3 M | 25.8 | 2.04 | 36.8 | 3.98 | < 0.00001 | 11.3 | 1.89 | 16.7 | 1.77 | < 0.00001 |
| 6 M | 24.4 | 1.78 | 31.2 | 4.05 | < 0.00001 | 16.5 | 1.48 | 29.4 | 3.17 | < 0.00001 |
| 12 M | 24.0 | 1.74 | 29.1 | 4.05 | < 0.00001 | 17.5 | 1.32 | 34.2 | 4.37 | < 0.00001 |
| 24 M | 24.9 | 1.84 | 28.9 | 4.54 | < 0.00001 | 14.4 | 1.34 | 34.6 | 4.52 | < 0.00001 |
| 36 M | 25.0 | 2.11 | 29.4 | 5.42 | < 0.00001 | 14.1 | 2.01 | 33.5 | 5.62 | < 0.00001 |
Figure 1.
Dynamics of HbA1c change
Figure 3.
Body mass index (BMI) evolution
Figure 2.
Dynamics of FPG change
Discussion
Type 2 diabetes mellitus is supposed to be the most rapidly expanding disease worldwide that significantly impacts morbidity and mortality [2]. Currently approximately 250 million affected individuals require tight glycemic control to minimize the risk of consequences of macro- and microvascular changes [16, 17]. That number is expected to extend to nearly 300 million in the next 20 years [1, 2]. Moreover, in the general population the lifetime risk of developing T2DM is predicted to rise to 20% [2]. Despite intense research in pharmacology and introduction of advanced multi-agent management, a large number of patients cannot be optimally treated [5, 9, 18, 19]. Furthermore, T2DM is usually considered a relentless chronic and progressive disease because pharmacological treatment cannot ensure a cure, but only a delay in the development of its consequences. The alarming prognosis necessitates the search for more effective anti-diabetic treatment and the introduction of new, promising methods into international guidelines to offer potentially complete remission [20].
A significant amount of evidence demonstrates that bariatric operations, particularly methods bypassing the duodenum and part of the jejunum such as gastric bypass (RYGB) and biliopancreatic diversion (BPD), rapidly and significantly ameliorate T2DM, leading to remission of disease in a majority of cases. These observations are not limited to pathologically obese patients [21–25]. The results of the two most important randomized studies, published in 2012 by Schauer et al. and Mingrone et al., highlighted the great curative potential of bariatric procedures – RYGB and BPD – to be far more effective than traditional medical treatment [10, 11]. Patients enrolled in the studies represented not only the morbidly obese diabetics, but also individuals with BMI < 35 kg/m2. Although the rate of laboratory remission of treated patients with BMI between 25 kg/m2 and 55 kg/m2 was 50–75%, the dynamics of change in HbA1c and FPG were presented as a cumulative value without presenting the results of patients with BMI < 35 kg/m2 and BMI > 35 kg/m2 [10, 11].
In our study, extraction of the BMI < 35 kg/m2 group (mean BMI value = 29.1 kg/m2 vs. 44.2 kg/m2 in BMI > 35 kg/m2 group) allowed us to expose the differences in dynamics of change of T2DM resolution parameters. Although the dynamics of decrease of HbA1c and FPG were initially significantly more intense in BMI > 35 kg/m2 patients (corresponding with higher weight loss), this difference ceased 1 year after RYGB. Considering the relatively high percentage of patients who demonstrated rapid laboratory glycemic control and improvement during hospital stay after surgery, it seems that weight loss is not the only factor influencing T2DM remission. Bariatric surgery therefore seems to have metabolic effects independent of weight loss induced changes. The ultra-low caloric diet and the effect of incretins were indicated as the most important mechanisms of early resolution of hyperglycemia after RYGB unrelated to weight loss [26, 27]. The incretins represented mainly by glucagon-like peptide 1 (GLP-1) are supposed to be responsible for increase of native insulin secretion, suppression of glucagon, improvement of peripheral insulin susceptibility and slowed down motility of the stomach with concomitant appetite reduction [28]. The shortened alimentary tract and accelerated passage of non-absorbed nutrients after RYGB and BPD induce the activity of these intestinal hormones [27]. Apart from that, the hypothesis of anti-incretins inactivation by duodenum bypass should also be considered as one of the mechanisms leading to resolution of T2DM [26–29].
About 80% of all studied cases regardless of BMI demonstrated laboratory complete resolution of T2DM 1–3 years after surgery. It means that the strict diabetes remission criteria recommended by ADA for HbA1c ≤ 6% and FPG ≤ 100 mg% were achieved without anti-diabetic medications [14, 15]. In the remaining group of patients it was still necessary to continue oral medical treatment or (in only 3 cases) insulin therapy, but with significantly reduced doses. Those patients had initially long-lasting T2DM with long-lasting insulin or combined therapy up to 15 years. One female with BMI 28 kg/m2 in consequence of unintended pregnancy restored the glucose intolerance and required insulin therapy 24 months after RYGB. However, a few months after delivery the glycemia control improved and HbA1c was 6.5% with only per oral medications at the last follow-up visit.
Another interesting correlation observed in the study was faster and more pronounced remission of T2DM in patients with longer biliopancreatic limb [30]. This will be a subject of a separate study requiring a larger group of patients. This observation has already been addressed by other researchers, but the ultimate conclusion is not definitive [8, 9].
As found by Fried et al. in a meta-analysis or previously in a reputable SOS study, we believe that laboratory remission of T2DM after bariatric surgery not only results in normalization of glycemia but also prevents complications induced by diabetes and reduces the mortality [8, 19, 21].
Presented postoperative complications and adverse effects were analyzed by the surgical team progressively. In the last consecutive 60 cases there was no complication observed at all. In the BMI < 35 kg/m2 group no serious complications were noted in the perioperative period. That would be consistent with the observation that a high BMI is correlated with a higher rate of major complications after bariatric procedures [31, 32]. The postoperative hypoglycemic episodes reported by almost 40% of patients were easily controlled with the help of simple dietary methods. Only 2 patients (one in each group) required 1-day hospital admission with intense intravenous glucose supplementation in the early postoperative period. Nevertheless, the frequency of severe hypoglycemia after RYGB was lower than in the same individuals during insulin therapy. Additionally, the episodes qualitatively compared favorably with the previous events and were described by the patients as milder, shorter and easier to control with sweet snacks. In the STAMPEDE trial 56% of patients reported hypoglycemia episodes after RYGB, while they were observed in 81% of patients in the group treated pharmacologically [10, 33].
Even though the mechanism of glycemia regulation after RYGB still seems to be unclear, the clinical observations proved its unquestionable effectiveness with acceptable safety [9, 16, 22, 34–36]. It seems certainly that surgical treatment of T2DM particularly engaging gastrointestinal bypassing methods should not only be the subject of further studies but also be considered as a valid therapeutic option for mild and morbidly obese diabetic patients.
Conclusions
The short- and mid-term observation of patients after RYGB revealed significant weight/BMI reduction accompanied with T2DM laboratory remission of different dynamics in the groups of patients with BMI < 35 kg/m2 and BMI > 35 kg/m2. The evaluation of laboratory type 2 diabetes mellitus measures 3 years after surgery demonstrates high effectiveness of surgical treatment in managing T2DM regardless of BMI. Considering high both social and economic costs of life-long medical treatment of type 2 diabetes and its complications, surgical metabolic intervention may become a new therapeutic approach.
References
- 1.King H, Aubert RE, Herman WH. Global burden of diabetes, 15-25: prevalence, numerical estimates and projections. Diabetes Care. 1998;21:1414–31. doi: 10.2337/diacare.21.9.1414. [DOI] [PubMed] [Google Scholar]
- 2.IDF Diabetes Atlas 2009; 2011. [Google Scholar]
- 3. www.stopacukrzycowa.com. [Google Scholar]
- 4.Geneva: WHO Diabetes Unit; World Health Organization Health experts accept use of HbA1c for diagnosing diabetes. www.who.int/diabetes. [Google Scholar]
- 5.Lebovitz H. Type 2 diabetes mellitus, current therapies and emergence of surgical options. Nat Rev. 2011;10:1038. doi: 10.1038/nrendo.2011.10. [DOI] [PubMed] [Google Scholar]
- 6.Buchwald H, Estok R, Fahrbach K, et al. Weight and T2DM after bariatric surgery: systematic review and meta-analysis. Am J Med. 2009;122:248–56. doi: 10.1016/j.amjmed.2008.09.041. [DOI] [PubMed] [Google Scholar]
- 7.Pories WJ, Swanson MS, MacDonald KG. Who would have thought it? An operation proves to be the most effective therapy for adult-onset diabetes mellitus. Ann Surg. 1995;222:339–50. doi: 10.1097/00000658-199509000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fried M, Ribaric G, Buchwald JN, et al. Metabolic surgery for the treatment of T2DM in patients with BMI < 35 kg/m2: an integrative review of early studies. Obes Surg. 2010;20:776–90. doi: 10.1007/s11695-010-0113-3. [DOI] [PubMed] [Google Scholar]
- 9.Dellagrave G, Marchesini JC. End to side duodeno-jejunostomy with half-and-half biliopancreatic limb for the treatment of type 2 diabetes: a proposal for a simpler technique. Obes Surg. 2007;17:138–9. doi: 10.1007/s11695-007-9019-0. [DOI] [PubMed] [Google Scholar]
- 10.Schauer PR, Kashyap SR, Wolski K, et al. Bariatric surgery versus intensive medical therapy in obese patients with diabetes. N Engl J Med. 2012;366:1567–77. doi: 10.1056/NEJMoa1200225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mingrone G, Panuzi S, Gaetano A, et al. Bariatric surgery versus conventional medical therapy for type 2 diabetes. N Engl J Med. 2012;366:1577–86. doi: 10.1056/NEJMoa1200111. [DOI] [PubMed] [Google Scholar]
- 12.Fried M, Yumuk V, Opper JM, et al. Interdisciplinary European Guidelines of metabolic and bariatric surgery. Obes Surg. 2014;24:42–55. doi: 10.1007/s11695-013-1079-8. [DOI] [PubMed] [Google Scholar]
- 13.Dixon JB, Zimmet P, Alberti KG, Rubino F. Bariatric surgery: an IDF statement for obese type 2 diabetes. Diabet Med. 2011;28:628–42. doi: 10.1111/j.1464-5491.2011.03306.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.American Diabetes Association. Diagnosis of and classification of diabetes mellitus. Diabetes Care. 2009;32(Suppl 1):S62–7. doi: 10.2337/dc09-S062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Buse JB, Caprio S, Cefalu WT, et al. How do we define cure of diabetes? Diabetes Care. 2009;32:2133–5. doi: 10.2337/dc09-9036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rubino F, Schauer PR, Kaplan LM, Cummings DE. Metabolic surgery to treat type 2 diabetes: clinical outcomes and mechanism of action. Ann Rev Med. 2010;61:393–411. doi: 10.1146/annurev.med.051308.105148. [DOI] [PubMed] [Google Scholar]
- 17.Batsis JA, Sarr MG, Collazo-Clavell ML, et al. Cardiovascular risk after bariatric surgery for obesity. Am J Cardiol. 2008;102:930–7. doi: 10.1016/j.amjcard.2008.05.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Which surgical procedure should be carried out for T2DM. Presented at the IXth Meeting of the Surgical Continuing Education; 17-19 February 2010; University of Malaga, Malaga. [Google Scholar]
- 19.Proczko M, Kaska Ł, Kobiela J, et al. Roux-en-Y gastric bypass in dialysed morbidly obese patients as a preparation for a kidney transplantation: case series. Videosurgery Miniinv. 2013;8:174–7. doi: 10.5114/wiitm.2011.32852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rubino F, Kaplan LM, Schauer PR, Cummings D, the Diabetes Surgery Summit Delegates The Diabetes Surgery Summit Consensus Conference Recommendations for the evaluation and use of gastrointestinal surgery to treat T2DM. Ann Surg. 2010;251:399–405. doi: 10.1097/SLA.0b013e3181be34e7. [DOI] [PubMed] [Google Scholar]
- 21.Sjostrom L, Narbro K, Sjostrom CD, et al. Effects of bariatric surgery on mortality in Swedish obese subjects. NEJM. 2007;357:741–52. doi: 10.1056/NEJMoa066254. [DOI] [PubMed] [Google Scholar]
- 22.Geloneze B, Geloneze SR, Fiori C, et al. Surgery for non-obese type 2 diabetic patients: an interventional study with duodenal-jejunal exclusion. Obes Surg. 2009;19:1077–83. doi: 10.1007/s11695-009-9844-4. [DOI] [PubMed] [Google Scholar]
- 23.Bužga M, Holéczy P, Švagera Z, et al. Effects of sleeve gastrectomy on parameters of lipid and glucose metabolism in obese women – 6 months after operation. Videosurgery Miniinv. 2013;8:22–8. doi: 10.5114/wiitm.2011.31631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Visockiene Z, Brimas G, Abaliksta T, et al. Metabolic changes one year after laparoscopic adjustable gastric banding operation in morbidly obese subjects. Videosurgery Miniinv. 2013;8:13–21. doi: 10.5114/wiitm.2011.30828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Razak Hady H, Dadan J, Gołaszewski P, Safiejko K. Impact of laparoscopic sleeve gastrectomy on body mass index, ghrelin, insulin and lipid levels in 100 obese patients. Videosurgery Miniinv. 2012;7:251–9. doi: 10.5114/wiitm.2011.28979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rubino F, Marescaux J. Effect of duodenal-jejunal exclusion in non-obese animal model of T2DM: a new perspective for an old disease. Ann Surg. 2004;239:1–11. doi: 10.1097/01.sla.0000102989.54824.fc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rubino F, Forgione A, Cummings DE, et al. The mechanism of diabetes control after gastrointestinal bypass surgery reveals a role of the proximal small intestine in the pathophysiology of type 2 diabetes. Ann Surg. 2006;244:741–9. doi: 10.1097/01.sla.0000224726.61448.1b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rubino F. Is type 2 diabetes operable intestinal disease? Diabetes Care. 2008;31(Suppl 2):290–6. doi: 10.2337/dc08-s271. [DOI] [PubMed] [Google Scholar]
- 29.Bose M, Olivian B, Teixeira J, et al. Do incretins play a role in the remission of T2DM after gastric bypass surgery: what are the evidences? Obes Surg. 2009;19:217–29. doi: 10.1007/s11695-008-9696-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kaska Ł, Kobiela J, Proczko M, et al. Does the lenght of the biliary limb influence medium-term laboratory remission of type 2 diabetes mellitus after Roux-en-Y gastrin bypass in morbidly obese patients? Videosurgery Miniinv. 2014;9:31–9. doi: 10.5114/wiitm.2014.40383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Weiner RA, El-Sayes IA, Theodoridou S, et al. Early postoperative complication: incidence, management and impact on length of hospital stay. A retrospective comparison between laparoscopic gastric bypass and sleeve gastrectomy. Obes Surg. 2013;23:2004–12. doi: 10.1007/s11695-013-1022-z. [DOI] [PubMed] [Google Scholar]
- 32.Kaska Ł, Proczko M, Stefaniak T, et al. Redesigning the process of laparoscopic sleeve gastrectomy based on risk analysis resulted in 100 consecutive procedures without complications. Vidoeosurgery Miniinv. 2013;8:289–300. doi: 10.5114/wiitm.2011.34797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Paluszkiewicz R, Kalinowski P, Wróblewski T, et al. Prospective randomized clinical trial of laparoscopic sleeve gastrectomy versus open Roux-en-Y gastric bypass for the management of patients with morbid obesity. Videosurgery Miniinv. 2012;7:225–32. doi: 10.5114/wiitm.2012.32384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gautier JF, Fetita S, Sobngwi E, Salaun-Martin C. Biological actions of incretins GIP and GLP-1 and therapeutic perspectives in patients with T2DM. Diabetes Metab. 2005;31:233–42. doi: 10.1016/s1262-3636(07)70190-8. [DOI] [PubMed] [Google Scholar]
- 35.Mingrone G, Castagneto-Gissey L. Mechanism of early improvement/resolution of type 2 diabetes after bariatric surgery. Diabetes Metab. 2009;35:518–23. doi: 10.1016/S1262-3636(09)73459-7. [DOI] [PubMed] [Google Scholar]
- 36.Hussain A, Mahmood H, El-Hasani S. Can Roux-en-Y gastric bypass provide a lifelong solution for diabetes mellitus? Can J Surg. 2009;52:E269–75. [PMC free article] [PubMed] [Google Scholar]