Abstract
Seborrheic dermatitis is an inflammatory eruption that tends to distribute on the sebaceous areas of the body and is rarely described as a paraneoplasia. Here we report a case with a responsive seborrheic dermatitis-like eruption of the head which resulted in generalized erythroderma. Intensive examinations detected concurrent malignant lymphoma.
Key words: Seborrheic dermatitis, Paraneoplastic syndrome, Peripheral T cell lymphoma
Case Report
An 81-year-old woman recognized pruritic scaly erythemas on the scalp 2 months before the visit to our hospital. Her medical history included nephrosis syndrome that had been treated with oral cyclosporine 100 mg/day for 8 years. The results of routine blood work before the onset of skin eruptions had been normal. Although the head erythemas appeared to be seborrheic dermatitis (SD) [1], the lesions did not respond to topical steroidal lotion. When she visited our hospital, the eruption had disseminated to the trunk and extremities, resulting in generalized erythroderma (fig. 1). Laboratory tests showed white blood cells 13,900/μl (normal 3,500–9,800), hemoglobin 11.9 mg/dl (normal 11.3–15.5), platelets 271,000/μl (normal 155,000–365,000), eosinophils 19.0%, atypical lymphocytes 2.0%, lactate dehydrogenase 517 IU/l (normal 176–353) and soluble interleukin-2 receptor 1,510 U/ml (normal <550); human T-lymphotropic virus type I antibody was negative. A skin biopsy of the erythema of the trunk showed that lymphocytes and eosinophils had infiltrated dominantly to the superficial perivascular space. There was no superficial dermal infiltrate of lymphocytes. A biopsy of her scalp lesion indicated only spongiotic dermatitis with parakeratosis. There was no atypical folliculotropic cell infiltration around follicles (fig. 2). Polymerase chain reaction and flow cytometry of the skin specimens failed to detect malignant cells. However, atypical lymphocytes (basket cells) were detected in the peripheral blood and bone marrow (fig. 3). Flow cytometry of the blood and bone marrow specimens showed that malignant cells were positive for CD2, CD3, CD4, CD5, CD7, CD25 and CD45RA. Positron emission tomography-computed tomography revealed abnormal enhancement of axillary and inguinal lymph nodes and bone marrow. We consulted a hematologist and peripheral T cell lymphoma not otherwise specified (PTCL-NOS), stage IV according to Ann Arbor [2] was diagnosed. PTCL can cause SD-like dermatitis that gradually develops into auto-sensitization dermatitis. As chemotherapy was dismissed considering her age, we administered fexofenadine 120 mg/day and oral prednisolone 20 mg/day so as to alleviate erythroderma and pruritus. Although most of the eruptions improved within a week, pruritus persisted. We added pregabalin 50 mg/day according to the recommendation by Yosipovitch [3], which reduced pruritus dramatically. The amount of daily oral steroid was tapered to 5 mg over 4 months, maintaining remission of cutaneous symptoms.
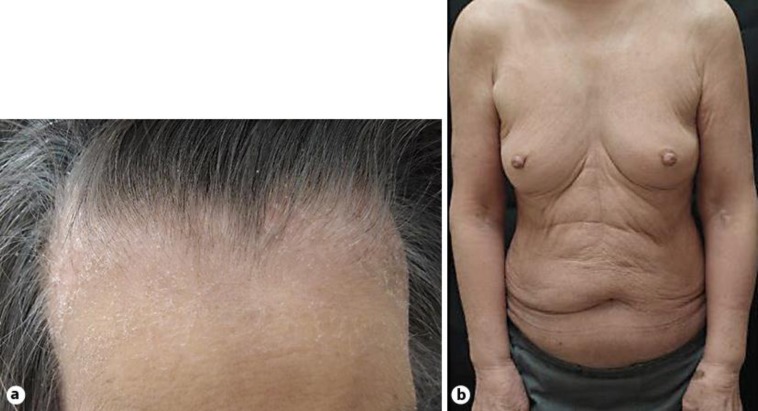
Fig. 1.
a Scaly erythemas on the patient's head. b Generalized erythroderma of the trunk and extremities.
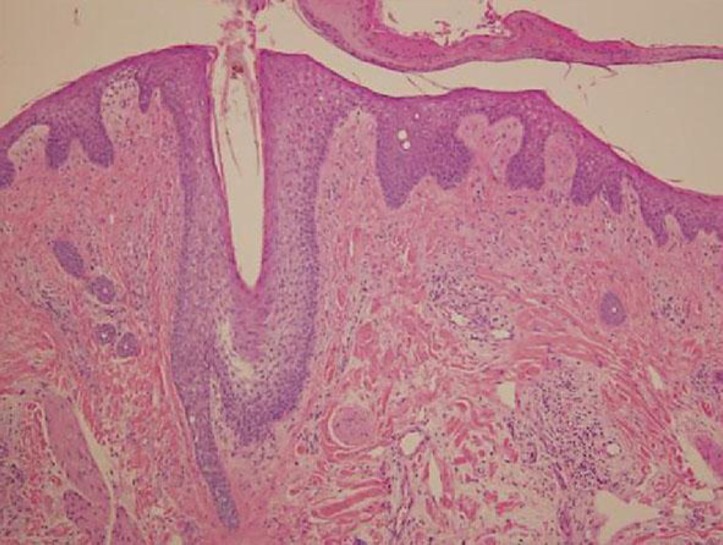
Fig. 2.
There was no atypical folliculotropic cell infiltration around follicles. The biopsy of the scalp lesion indicated only spongiotic dermatitis with parakeratosis. Hematoxylin and eosin stain, ×100.
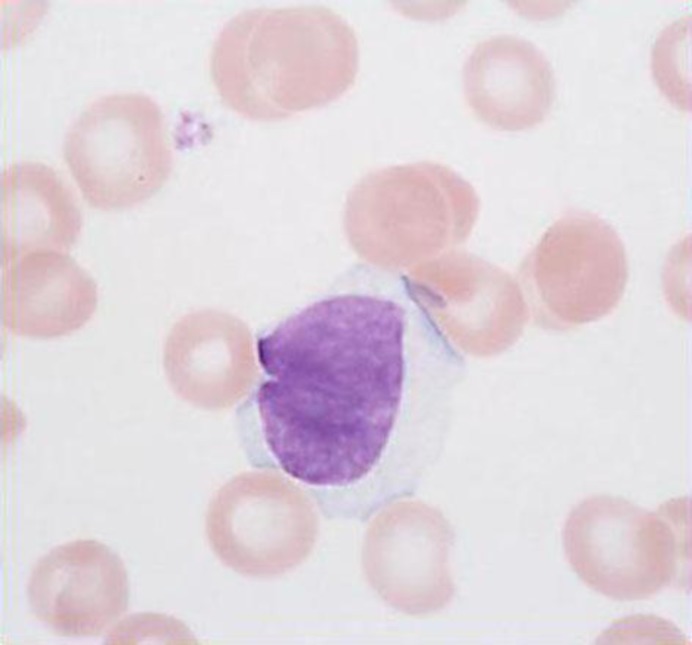
Fig. 3.
Atypical lymphocytes (basket cells) were detected in the peripheral blood and bone marrow. No flower cells were observed.
Discussion
Few publications have described SD as a paraneoplastic syndrome in cases with lung cancer and lymphoma [4, 5, 6]. The diagnosis of paraneoplastic syndrome usually requires concurrent onset and parallel course with malignancy at least. Although we could not confirm whether the severity of the SD would parallel that of PTCL, SD seems to be a paraneoplasia since the onset of the SD coincided with that of PTCL and the SD was resistant to ordinary topical therapy.
Hematologic malignancies are often accompanied by severe pruritus. For chronic paraneoplastic pruritus, antidepressant and anticonvulsive drugs such as gabapentin are anecdotally effective [3]. Although the mechanisms of pruritus as well as the antipruritic effect of anticonvulsive agents are not clear, they probably inhibit central itch pathways. We used low-dose pregabalin that worked and accelerated the improvement of SD. This may be an important option for severe paraneoplastic pruritus.
In this case, simple SD and subsequent auto-sensitization dermatitis were suspected at first. However, the SD was too resistant to ordinal therapy and developed to erythroderma. Complete blood count revealed the presence of lymphoma that became an important clue to diagnosis. The differential diagnosis was folliculotropic mycosis fungoides. However, this possibility was ruled out by the results of pathological examinations.
Disclosure Statement
The authors report no conflicts of interest. There were no funding sources.
References
- 1.Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook's Textbook of Dermatology. ed 8. Oxford: Blackwell; 2010. pp. 23.29–23.34. [Google Scholar]
- 2.Lister TA, Crowther D, Sutcliffe SB, Glatstein E, Canellos GP, Young RC, Rosenberg SA, Coltman CA, Tubiana M. Report of a committee convened to discuss the evaluation and staging of patients with Hodgkin's disease: Cotswolds meeting. J Clin Oncol. 1989;7:1630–1636. doi: 10.1200/JCO.1989.7.11.1630. [DOI] [PubMed] [Google Scholar]
- 3.Yosipovitch G. Chronic pruritus: a paraneoplastic sign. Dermatol Ther. 2010;23:590–596. doi: 10.1111/j.1529-8019.2010.01366.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kokturk A, Ikizoglu G, Kaya TI, Baz K, Ulubas B, Apa DD. Seborrhoeic dermatitis-like manifestation of lung cancer evolving into erythrodermia. J Eur Acad Dermatol Venereol. 2004;18:381–382. doi: 10.1111/j.1468-3083.2004.00901.x. [DOI] [PubMed] [Google Scholar]
- 5.Venkateswaran S, Garg BR, Reddy BS, Narasimhan R. Cutaneous lymphoma mimicking seborrhoeic dermatitis. Indian J Dermatol Venereol Leprol. 1995;61:45–47. [PubMed] [Google Scholar]
- 6.Bittencourt AL, de Oliveira Mde F. Cutaneous manifestations associated with HTLV-1 infection. Int J Dermatol. 2010;49:1099–1110. doi: 10.1111/j.1365-4632.2010.04568.x. [DOI] [PubMed] [Google Scholar]