Abstract
Background:
Workplace exposures as in clinical work can cause disorders. Some organ systems are at risk. This work may be a risk factor for early symptoms of menopause. The objective of this study was to compare the early symptoms of menopause between hospital personnel who work in clinical and office settings.
Materials and Methods:
This was a historical cohort study conducted on clinical and office workers of hospitals. The study was conducted using a flexible interview conducted with a questionnaire among personnel of age 40 years and above. According to their menopausal status, they were divided into three phases: premenopause, perimenopause, and postmenopause. Symptoms in 10 items were assessed and scored from 1 to 10, and were compared. Data were analyzed with SPSS 16, t-test, and Chi-square tests and were calculated considering P < 0.05 as the significant level. Odds ratios were calculated along with 95% confidence interval.
Results:
Frequency of menopausal symptoms was higher in the clinical group than in the office group. In the clinical group, the odds ratio for menopausal symptoms like flashing and sweating was 1.879 (1.457-2.423) and in the office personnel, it was 0.192 (0.030-1.238). In the clinical group, the odds ratio for anxiety and irritability was 2.029 (1.660-2.481) and in the office personnel, it was 0.116 (0.017-0.779).
Conclusions:
Clinical personnel had higher risk for early menopausal symptoms such as flashing, sweating, anxiety, and irritability. Assessing the health of these personnel may help to improve their reproductive health. The person with reproductive risk factors is not suitable for clinical work.
Keywords: Menopause, clinical worker, office worker
INTRODUCTION
At least half of the employed people are women and they are in their active years, i.e. 20-45 years old.[1,2,3] Statistics have shown that about half of the employees in the Ministry of Health are women and many of them are working in hospital departments such as operation rooms, chemotherapy department, radiology and radiotherapy departments, emergency department, and others. Occupational risk factors for them include physical, chemical, biological, and ergonomic risks such as ionizing radiations, anesthetic gases, chemotherapy agents, ethylene oxide, solvents, and shift work.[4,5]
According to earlier studies, some hazards in healthcare settings include antineoplastic drugs, anesthetic gases, ethylene oxide, mercury, carbon monoxide, organic solvents, environmental tobacco smoke (ETS), electromagnetic field (EMF), mechanical stress, ionizing radiation and video display terminal (VDT), and shift work, especially night work.[6,7,8,9,10,11,12,13,14]
Many studies have reported on the occupational risk factors that affect reproductive system and some of them may cause menopause.[15,16,17]
Fleming and coworkers found that ETS could cause early menopause.[18] Cassou and coworkers showed the effects of mental stress on menopause.[19] Lohr and coworkers found that exposure to solvents such as fluorocarbons could cause menopause and lower the estrogen level.[20]
In perimenopause, ovaries have low performance and produce less estrogen. These changes cause some symptoms that begin in the fifth decade and continue up to sixth decade. Some studies have shown the relationship between the age of menopause and different occupations. The influential factors include type of work, physical exposures, and mental stresses.
Some of the menopausal symptoms are flashing, sweating, irregular menses, low libido, dryness of vagina, and mood disorders.[21]
Rahman and coworkers showed that the mean age of menopause was 51 years in Bangladesh. The most frequent symptoms were fatigue (93%), headache (89%), musculoskeletal and joint problems (76%), mental fatigue (61%), and sleep problem (54%); bladder and heart disorders had the lowest frequency. Fifteen percent of the evaluated women worked outside home.[22]
Metintas and coworkers conducted a study in Turkey and demonstrated that most of the menopausal symptoms were related to aging and chronic diseases; these were related to compounding of symptoms and previous reproductive disorders. They reported fatigue, sleep problems, heart disorders, depression, and anxiety as the most frequent symptoms. Three percent of women in their study were employed.[23] In a similar study conducted in Malaysia, Abdorrahman and coworkers reported that the average age of menopause was 51 years; musculoskeletal and joint problems were common in 80% of women, mental fatigue was reported in 67%, 30% of women had special jobs, and 10.5% had full-time special jobs,[24] and some of them worked in a healthcare setting.
In Pakistan, Mazhar and coworkers demonstrated that the average age of menopause was 48.5 years; 70% of women had menopausal symptoms; 90% had flashing and 89% had sleep problems. Most of their study population consisted of housewives[25] who were exposed to disinfectants and some solvents.
The objective of the present study was to evaluate and compare the menopausal symptoms between those who work in office and in the clinical setting.
MATERIALS AND METHODS
Sudy setting
Hospitals located in Mashhad.
Study design and target population
This was a historical cohort study about reproductive disorders conducted on women who were employed in clinical and office settings of hospitals during 2010-2013. The data were taken from personnel medical files and an interview conducted using a questionnaire.
The study population consisted of clinical and office workers of nine hospitals. The author researched and followed them by interview and physical examination during the study period. Simple random sampling method was used according to Refs [1-3]. With α =0.05, power = 80, P1 = 40%, and P2 = 20%, the study population was calculated as 300 for each group (clinical and office workers). Inclusion criteria were personnel working in clinical or office setting of hospitals with at least 5 years of work experience in the same job and premenopausal personnel who were aged 40 years and above. Participants were selected by census method and were divided into three groups: Premenopause; w omen with delayed menses for at least two cycles; perimenopause, women who missed their menses for 1-11 months; and postmenopause, women who missed their menses more than 12 months. Exclusion criteria were hypothalamus-hypophysis diseases, reproductive system surgery, hormone therapy, diabetes, hyperthyroid disease, pheochromocytoma, and cardiovascular diseases. These were taken from special tests in personnel medical files in occupational health center and by an interview.
Participants were evaluated and observed for age, number of pregnancies, and body mass index.
The validity and reliability of the questionnaire designed for the study had been checked with professors’ opinions and a pilot study was also conducted with correlation coefficient 90%. The author - interviewed with perssonel by using a questionnaire and did physical examination in suitable site.
The questionnaire also included questions about non-occupational and occupational risk factors for reproductive disorders. Non-occupational risk factors were age, endocrine disorders, family history, and psychological stress, and occupational risk factors were work stress, physical or mental, exposures to chemicals and physical factors, shift work, and working length. The second part of the questionnaire had items related to menopausal symptoms that included flashing, sweating, heart disorders, sleep problems, mood disorders such as depression, anxiety, and irritability, mental and physical fatigue, low libido, dryness of vagina, bladder problem, and musculoskeletal and joint problem. Each item was given a score of 1-10, and the mean values of scores were compared between the two groups.
For statistical analysis, data were analyzed with SPSS 16. Chi-square and t-test were used to compare qualitative and quantitative variables and P value less than 0.05 was considered as significant. Odds ratios were calculated along with 95% confidence interval.
The study protocol was approved by the ethical committee of Mashhad University of Medical Sciences and the participants’ oral consent was obtained.
RESULTS
Based on the inclusion and exclusion criteria, in this study, participants from clinical and administrative personnel were selected for evaluating their menopausal status. The mean age of menopause for the clinical group was 45.65 ± 1.02 years and the average work experience was 20.54 ± 1.08 years. For the office personnel, the mean age of menopause was 46.10 ± 1.00 years and the average work experience was 21.09 ± 0.90 years. The differences between the mean age of menopause in the two groups and the mean of work experience in the two groups were not significant (P < 0.05).
Body mass indexes were 24.56 ± 0.74 kg/m2 and 25.00 ± 0 kg/m2 for clinical and administrative workers, respectively. The differences between body mass indexes of the two groups were not significant (P < 0.05).
Clinical participants were selected from general, radiology, operation rooms, chemotherapy, and other departments in the hospitals.
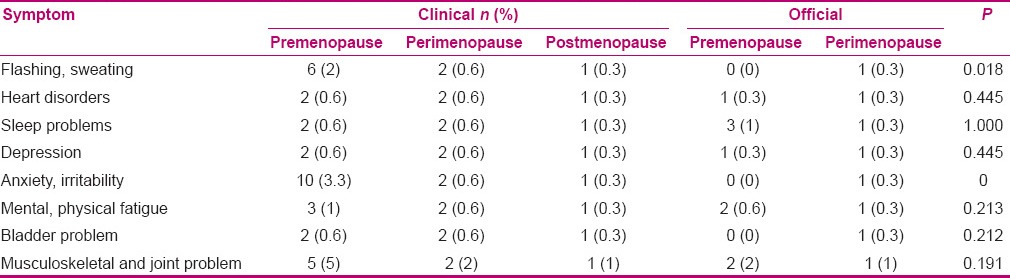
Table 1 shows the frequency of menopausal symptoms and their comparison between the two groups (P < 0.05). Flashing, sweating, and anxiety were more frequent in premenopause, perimenopause, and postmenopause phases of the clinical personnel compared with the office group (P < 0.05). Office group participants in postmenopause phase did not have any symptom and all of them had zer o score.
Table 1.
Frequency of menopausal symptoms and their comparison between clinical and administrative personnel
Each item of menopausal symptoms in the questionnaire had a severity score between 1 and 10. Scores of flashing, sweating, heart disorders, sleep problems, mood disorders such as depression, anxiety, and irritability, mental and physical fatigue, bladder problem, and musculoskeletal and joint problem were higher in the clinical group than in the administrative group, but the differences were not statistically significant [Table 2]. For example, the scores of musculoskeletal and joint problem in the two groups were 1.67 ± 2.72 and 1.19 ± 0.84, respectively, with t = 1.681 and P = 0.095. The scores of mental and physical fatigue in the two groups were 1.52 ± 2.00 and 1.33 ± 1.09, respectively, with t = 0.833 and P = 0.406.
Table 2.
Mean of grades of menopausal symptoms and comparison of them between clinical and office personnel
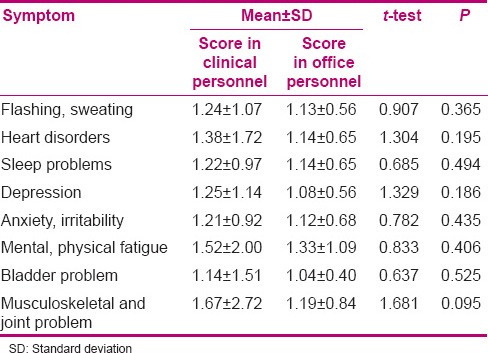
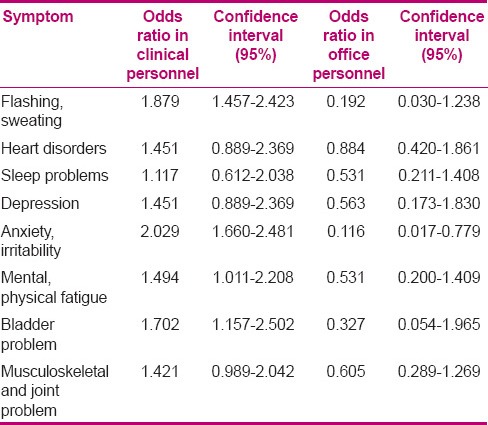
Table 3 shows the comparison of odds ratios of menopausal symptoms between the two groups. According to Table 3, in the clinical group, the odds ratio for menopausal symptoms like flashing and sweating was 1.879 (1.457–2.423) and in the office personnel, it was 0.192 (0.030–1.238). The ratios for anxiety and irritability were 2.029 (1.660–2.481) and 0.116 (0.017–0.779), respectively.
Table 3.
Comparison of odds ratios for menopausal symptoms between clinical and office personnel
DISCUSSION
According to our findings, on comparing the frequency of menopausal symptoms in the three phases of pre-, peri-, and post-menopause, only flashing, sweating, anxiety, and irritability showed significant differences between the two groups. Other symptoms like heart disorders, sleep problems, mood disorders, depression, fatigue, bladder problem, and musculoskeletal and joint problems were also more common in the clinical group, but the differences were not significant [Table 1].
Regarding the severity scores, symptoms such as flashing, sweating, anxiety, irritability, sleep problems, mood disorders, depression, fatigue, bladder problem, and musculoskeletal and joint problems had higher scores in the clinical group, but the differences were not significant. Fatigue and musculoskeletal and joint problems had the highest scores [Table 2].
Similar to this study, Rahman and coworkers reported the most frequent symptoms as follows: fatigue (93%), headache (89%), musculoskeletal and joint problems (76%), mental fatigue (61%), and sleep problem (54%), and bladder and heart disorders had the lowest frequency.[22] Metintas and coworkers also demonstrated in their study that the most frequent symptoms were fatigue, sleep problems, heart disorders, depression, and anxiety; 3% of their participants were employed.[23] Based on the results presented in Table 3, the odds ratios for some of the menopausal symptoms including flashing, sweating, anxiety, and irritability showed the risk for clinical personnel than for administrative personnel.
Abdorrahman and coworkers showed similar frequencies of symptoms as in this study: Musculoskeletal and joints problems (80%), mental fatigue (67%), 30% of participants had special job, and 10.5% had full-time special work,[24] and some of them worked as a healthcare worker.
Mazhar and coworkers reported that 70% of women had menopausal symptoms, 90% had flashing, and 89% had sleep problems.[25]
According to the reports on perimenopause, ovaries have low performance and produce low estrogen, which can cause symptoms. Symptoms begin in the fifth decade and continue up to mid-sixties and above. Many of these symptoms are harmful.[21] Some studies have reported different ages for menopause related to different jobs, exposure to chemicals, physical exposures, and mental stresses.[2] According to the results, clinical personnel, who did the same work throughout their job experience, had more risk for some menopausal symptoms such as flashing, sweating, anxiety, and irrita bility, despite the fact that clinical and office personnel had approximately the same mean values of age.
Clinical jobs involve exposure to chemicals, solvents, and physical and mental risk factors.
In this study, the exact job analysis was not done in a step-by-step manner and the number of personnel who participated in the study was less. It seems that a study with a larger sample could be more useful.[26,27,28]
According to this study, job analysis and determination of occupational risk factors for clinical personnel were necessary, especially in premenopausal ages.
CONCLUSION
The author found that clinical personnel were at higher risk for early menopausal symptoms such as flashing, sweating, anxiety, and irritability. Assessing the health of these personnel may help to improve their reproductive health. With engineering control methods can make the better work situation. In job pre placement examination and periodic examination, if the person has reproductive risk factorshe or she is not suitable for clinical works but it might be better does assessment in case by case.
ACKNOWLEDGMENT
The author appreciates the support of the Vice-chancellor of Research of Mashhad University of Medical Sciences.
Footnotes
Source of Support: Vice chancellor of research of Mashhad University of Medical Sciences
Conflict of Interest: None declared.
REFERENCES
- 1.Windham GC, Osorio AM. LaDou Joseph Current Occupational and Environmental Medicine. Vol. 4. New York: McGraw-Hill Companies; 2007. Female Reproductive Toxicology; pp. 384–99. [Google Scholar]
- 2.Russi MB, Howarth MV. Occupational medicine in the Healthcare industry. In: Rosentock L, Cullen MR, Brodkin CA, Redlich CA, editors. Textbook of clinical occupational and environmental medicine. Vol. 2. United States of America: Elsevier; 2005. pp. 245–92. [Google Scholar]
- 3.Osorio AM, Windham GC. LaDou Joseph Current Occupational and Environmental Medicine. Vol. 4. New York: McGraw-Hill Companies; 2007. Male Reproductive Toxicology; pp. 400–12. [Google Scholar]
- 4.Bazan JA, Mangino JE. Infection control and postexposure prophylaxis for the pregnant healthcare worker. Clin Obstet Gynecol. 2012;55:571–88. doi: 10.1097/GRF.0b013e31824f3a07. [DOI] [PubMed] [Google Scholar]
- 5.Lawson CC, Rocheleau CM, Whelan EA, Lividoti Hibert EN, Grajewski B, Spiegelman D, et al. Occupational exposures among nurses and risk of spontaneous abortion. (e1-8).Am J Obstet Gynecol. 2012;206:327. doi: 10.1016/j.ajog.2011.12.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kou ZX, Li H, He YH, Yu WL, Jin N, Zhou AS. Analysis on reproductive health status and influencing factors of female workers of pharmaceutical industry in Gansu province. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi. 2011;29:653–6. doi: 10.3760/cma.j.issn.1001-9391.2011.09.005. [DOI] [PubMed] [Google Scholar]
- 7.Izmerov NF, Sivochalova OV, Fesenko MA, Denisov EI, Golovaneva GV. The issues of workers reproductive health protection from harmful occupational and enviromenral exposures. Vestn Ross Akad Med Nauk. 2012;12:47–53. [PubMed] [Google Scholar]
- 8.Taranenko LA, Malutina NN. Congenital abnormalities in children whose parents were exposed to methanol and formaldehyde. Med Tr Prom Ekol. 2012;12:33–5. [PubMed] [Google Scholar]
- 9.Rocheleau CM, Lawson CC, Waters MA, Hein MJ, Stewart PA, Correa A, et al. Inter-rater reliability of assessed prenatal maternal occupational exposures to solvents, polycyclic aromatic hydrocarbons, and heavy metals. J Occup Environ Hyg. 2011;8:718–28. doi: 10.1080/15459624.2011.627293. [DOI] [PubMed] [Google Scholar]
- 10.Bodaghabadi M. Relationship between occupational exposure to anaesthetic gases and spontaneous abortion. Gynecol Endocrinol. 2004;18:346. [Google Scholar]
- 11.Sitarek K, Stetkiewicz J, Wąsowicz W. Evaluation of reproductive disorders in female rats exposed toN-methyl-2-pyrrolidone. Birth Defects Res B Dev Reprod Toxicol. 2012;95:195–201. doi: 10.1002/bdrb.21001. [DOI] [PubMed] [Google Scholar]
- 12.Flora G, Gupta D, Tiwari A. Toxicity of lead: A review with recent updates. Interdiscip Toxicol. 2012;5:47–58. doi: 10.2478/v10102-012-0009-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Simon SL, Linet MS. Radiation-exposed populations: Who, why, and how to study. Health Phys. 2014;106:182–95. doi: 10.1097/HP.0000000000000006. [DOI] [PubMed] [Google Scholar]
- 14.Shuhaiber S, Einarson A, Radde IC, Sarkar M, Koren G. A prospective - Controlled study of pregnant Veterinary Staff exposed to in haled anaesthetics and X-rays. Int J Occup Med Environ Health. 2002;15:363–73. [PubMed] [Google Scholar]
- 15.Aminian O, Sharifian SA, Mehrdad R, Khademi A, Assadi SN. Anesthetic gases and spontaneous abortion: A historical cohort study. Arch Iran Med. 2008;11:122–4. [Google Scholar]
- 16.Talamanca IF. Reproductive problems among women health care workers: Epidemiologic evidence and preventive strategies. Epidemiol Rev. 2000;2:249–60. doi: 10.1093/oxfordjournals.epirev.a018037. [DOI] [PubMed] [Google Scholar]
- 17.Assadi SN. Recommendations in health protection and fitness for work for nuclear medicine specialists. Iran J Nucl Med. 2010;18:88–9. [Google Scholar]
- 18.Fleming LE, Levis S, Leblanc WG, Dietz NA, Arheart KL, Wilkinson JD, et al. Earlier age at menopause, work, tobacco smoke exposure. Menopause. 2008;15:1103–8. doi: 10.1097/gme.0b013e3181706292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cassou B, Mandereau L, Aegerter P, Touranchet A, Derriennic F. Work-related Factors Associated with Age at Natural Menopause in a Generation of French Gainfully Employed Women. Epidemiology. 2007;166:429–38. doi: 10.1093/aje/kwm104. [DOI] [PubMed] [Google Scholar]
- 20.Lohr A, Jackson T, Javins B. Environmental chemical exposure associated with early onset menopause. Medical news. 2011. [Last cited on 2011 Apr 4]. Available from: http://www.Medicalnewstoday.com/articles .
- 21.34 menopause symptoms. 2011. [Last cited on 2011 Apr 4]. Available from: http://www.34-menopause-symptoms.com .
- 22.Rahman S, Salehin F, Iqbal A. Menopausal symptoms assessment among middle age women in Kushtia, Bangladesh. BMC Res Notes. 2011;4:188. doi: 10.1186/1756-0500-4-188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Metintas S, Arykan I, Kalyoncu C, Ozalp S. Menopause rating scale as a screening tool in rural Turkey. Rural Remote Health. 2010;10:1230. [PubMed] [Google Scholar]
- 24.Rahman SA, Zainudin SR, Karmun VL. Assessment of menopausal symptoms using MRS among middle age women in kuching, Sarawak, Malaysia. Asia Pac Fam Med. 2010;9:1–6. doi: 10.1186/1447-056X-9-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mazhar SB, Rasheed S. Menopause rating scale (MRS): A simple tool for assessment of climacteric symptoms in Pakistani women. Ann Pak Inst Med Sci. 2009;5:158–61. [Google Scholar]
- 26.Assadi SN. Is being a health-care worker a risk factor for women's reproductive system? Int J Prev Med. 2013;4:852–7. [PMC free article] [PubMed] [Google Scholar]
- 27.Assadi SN. Cardiovascular disorders risk factors in different industries of Iran. Int J Prev Med. 2013;4:728–33. [PMC free article] [PubMed] [Google Scholar]
- 28.Assadi SN, Esmaily H, Mostaan L. Comparison of sensory-neural hearing between firefighters and office workers. Int J Prev Med. 2013;4:115–9. [PMC free article] [PubMed] [Google Scholar]


