Abstract
Background:
Different therapeutic methods have been applied for the treatment of dysmenorrhea and the method with the lesser side effects is preferred. The aim of this study was to compare the effects of herbal products (fennelin and vitagnus) and mefenamic acid in the treatment of primary dysmenorrhea.
Materials and Methods:
This ouble-blind clinical trial was carried out in 105 students with mild and moderate dysmenorrhea. The students were randomly divided into four groups which received the extracts of fennelin and vitagnus, mefenamic acid, and placebo, respectively. Severity of pain was detected by the Visual Analog Scale (VAS) during one cycle before and two cycles after the intervention. Data were analyzed by SPSS version 16 and (P < 0.05 was considered significant.
Results:
Demographic characteristics of the students were similar in the four groups. There was no significant difference in the mean of severity of dysmenorrhea during one cycle before the intervention between the four groups, but the difference was significant during two cycles after the intervention. Fennelin had similar effects as vitagnus on dysmenorrhea. Mefenamic acid had less effect than both the drugs (P <0.05).
Conclusion:
Fennelin and vitagnus had higher effect than mefenamic acid. Use of these products is suggested for dysmenorrhea.
Keywords: Dysmenorrhea, fennelin, Iran, vitagnus
INTRODUCTION
Dysmenorrhea occurs in around 50%of women with regular menstruation.[1,2] This induces disability in more than 10% of women in their daily activities.[3] Prevalence of dysmenorrhea in adolescents is over 85%[4] but the prevalence rates have been reported to be as high as 90% in women aged 1845 years[5] The prevalence of dysmenorrhea worldwide is similar to that in the US, with the rates ranging from 15.8 to 89.5% and with higher prevalence rates reported in adolescent populations.[6,7,8,9,10,11]
Nonsteroidal anti-inflammatory drugs (NSAIDs) form the basis of treatment and contraceptive pills are also used in treatment.[12] About 10% of patients do not respond to these treatments.
NSAIDs inhibit prostaglandin synthesis, and so, they are important in the treatment of this disease. The effectiveness of these agents has been consistently confirmed, with response rates exceeding 75% in most studies.[13]
Since the effective chemical drugs for primary dysmenorrhea, such as mefenamic acid, acetaminophen, ibuprofen, etc., have side effects including dizziness, nausea, diarrhea, digestive disorders, tc., replacing these drugs with herbal ones which have less side effects can be effective. In this case, many researches have been done. According to these studies, those plants with few side effects are easily accepted among people. Two herbal drops known as vitagnus and fennelin are available in the market. Fennelin contains Foeniculum vulgare extract. The effects of this plant extract on pain, inflammation, and dysmenorrhea were studied by different researchers.[14,15,16,17] Vitagnus contains Vitex agnus extract and there are different studies about its effects on premenstrual syndrome (PMS).[18,19,20] There is no comparative study about these drugs. Therefore, we decided to compare the effects of these herbal drugs on primary dysmenorrhea.
MATERIALS AND METHODS
This study was a clinical trial carried out on female students of Hamadan Medical School, with primary dysmenorrhea assayed by (Visual Analog Scale (VAS) method. The exclusion criteria were: (1) presence of any systemic disease such as liver, kidney, thyroid, orcoagulation disease; (2) hypersensitivity to drug; (3) use of analgesic drugs during the study; and (4) use of oral contraceptive pills (OCP) or intrauterine device (IUD).
Drugs
One hundred and five study participants were divided into four groups. Group 1 received fennelin, 30 drops every 4 h, 1 day before the start of the cycle until the third day; Group 2 received vitagnus, 40 drops once a day in the morning, 1 day before the start of the cycle until the third day; Group 3 received mefenamic acid capsules 250 mg every 4 h, 1 day before the start of the cycle until the third day; and Group 4 received placebo, 30 drops every 4 h, 1 day before the start of the cycle until the third day. Pain was measured and compared by means of VAS.
Each group was assayed for three cycles, one without any drugs and then two cycles with them.
Statistical analysis
Statistical analysis was carried out using SPSS version 16. Analysis of variance (ANOVA) was used to compare pain between different groups.
RESULTS
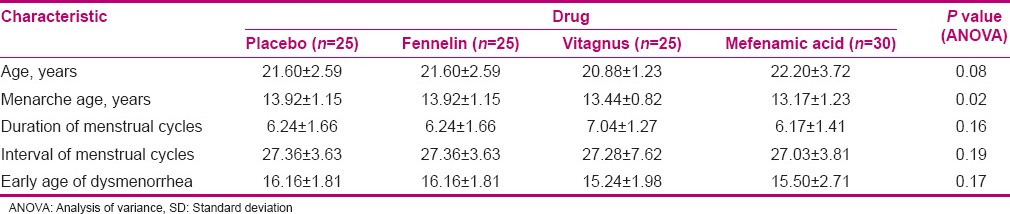
A total of 105 female students aged 18-25 years who complained of primary dysmenorrhea were contacted. Demographic characteristics of research groups are presented in Table 1. As specified in the table, the subjects of the study groups were similar in age, number of days of menstruation, age at first menstruation, and dysmenorrhea interval, and the differences were not statistically significant. But the age at menarche was significantly different (P < 0.05).
Table 1.
Mean and SD of some demographic characteristics of the studied units
Family history of dysmenorrhea, drug use during menstruation, history of exercise, and disruption in the daily chores were not significantly different.
In this study, pain intensity was evaluated within a cycle (zero cycle) before treatment with oral drops, mefenamic acid, and placebo drops, and the mean pain intensity of the four groups was not significantly different at the end of the cycle; but after the intervention (drugs), this difference was significant (P < 0.05) at the end of the first and second cycles [Table 2].
Table 2.
Mean and SD of severity of dysmenorrhea (menstrual cycle zero, one, and two) in the groups of study according to the type of drug

DISCUSSION
Dysmenorrhea and PMS are the common problems occurring in women during childbearing age. Many studies have been conducted on finding the best treatment for these conditions. Most researches have proved the positive effects of different drugs. Administration of NSAIDs is the most commonly used treatment for dysmenorrhea. NSAIDs decrease the menstrual pain by decreasing intrauterine pressure and lowering prostaglandin F2 (PGF2)-alpha levels in menstrual fluid.[21,22,23] Khodakrami et al. examined the effect of combination of three Iranian herbal drugs in the treatment of primary dysmenorrhea. The effects of saffron, celery seed, and anise (SCA) extract were compared with those of mefenamic acid and placebo. The authors showed that both SCA and mefenamic acid have adequate analgesic effects on dysmenorrhea. The SCA was found to be more effective than mefenamic acid for severe pain relief in dysmenorrhea.[24]
Nazarpoor et al. conducted a comparative study between fennelin and mefenamic acid in primary dysmenorrhea. Fennelin showed an effectsimilar to that of mefenamic acid.[18] In other studies, similar effects of vitagnus and fennelin were reported primary dysmenorrhea.[25,26]
In this study, the pain intensity before treatment with herbal oral drops and mefenamic acid capsules and placebo drops in one cycle (zero cycle) was studied. Average pain intensity in the three groups was not significantly different at the end of the zero cycle; but at the end of the first and second cycles of the intervention (drugs), this difference was significant. The study results showed that both drugs were able to reduce pain during treatment. The effects of the two herbal drugs were the same but higher than that of mefenamic acid. The average pain intensity in both herbal drug groups was reduced not only at the end of the first prescription medication but also at the end of the second month after treatment.
In another study, Shahhosaini et al. studied the effect of vitagnus on dysmenorrhea and found that the maximumeffect was induced at the end of the third cycle.[27] No side effects of the herb were reported in this study.
CONCLUSION
Treatment with herbal drops vitagnus, fennelin, and mefenamic acid capsule could reduce dysmenorrheal pain, and the effects of vitagnus and fennelin were higher than that of mefenamic acid. Thus, these herbal medicines are safe and effective for use in dysmenorrhea.
ACKNOWLEDGMENTS
The authors would like to thank Barij Essence Pharmaceutical Company for the preparation of fennelin and placebo drops in this study. This work was financially supported and ethically approved by the Vice-Chancellor for Research, Hamadan University of Medical Sciences, Hamadan, Iran.
Footnotes
Source of Support: Hamadan Medical University
Conflict of Interest: The authors declare that they have no conflicts of interest.
REFERENCES
- 1.Ryan KJ, Berkowitz RL, Barbieri RL, Donaif A. Kistner’ In Gynecology and Women’ Health 1999. In: Ghazijahani B, Ghotbi R, editors. 7th ed. Tehran: Golban Publication; 2005. p. 189. Translated by. [Google Scholar]
- 2.Sadatian SA. Fundamental Affectations of Gynecology. In: Sadatian SA, editor. CMMD. 3rd ed. Tehran: Nore Danesh Publication; 2004. pp. 33–5. [Google Scholar]
- 3.Lindh I, Ellstrom AA, Milsom I. The effect of combined oral contraceptives and age on dysmenorrhoea: An epidemiological study. Hum Reprod. 2012;27:676–82. doi: 10.1093/humrep/der417. [DOI] [PubMed] [Google Scholar]
- 4.Banikarim C, Chacho MR, Kelder SH. Prevalence and Impact of Dysmenorrhea on Hispanic Female Adolescents. Arch Pediatr Adolesc Med. 2000;154:1226–9. doi: 10.1001/archpedi.154.12.1226. [DOI] [PubMed] [Google Scholar]
- 5.Jamieson DJ, Steege JF. The prevalence of dysmenorrhea, dyspareunia, pelvic pain and irritable bowel syndrome in primary care practices. Obstet Gynecol. 1996;87:55–8. doi: 10.1016/0029-7844(95)00360-6. [DOI] [PubMed] [Google Scholar]
- 6.Sharma P, Malhotra C, Taneja DK, Saha R. Problems related to menstruation amongst adolescent girls. Indian J Pediatr. 2008;75:125–9. doi: 10.1007/s12098-008-0018-5. [DOI] [PubMed] [Google Scholar]
- 7.Lee LK, Chen PC, Lee KK, Kaur J. Menstruation among adolescent girls in Malaysia: A cross-sectional school survey. Singapore Med J. 2006;47:869–74. [PubMed] [Google Scholar]
- 8.El-Gilany AH, Badawi K, El-Fedawy S. Epidemiology of dysmenorrhoea among adolescent students in Mansoura, Egypt. East Mediterr Health J. 2005;11:155–63. [PubMed] [Google Scholar]
- 9.Osuga Y, Hayashi K, Kobayashi Y, Toyokawa S, Momoeda M, Koga K, et al. Dysmenorrhea in Japanese women. Int J Gynaecol Obstet. 2005;88:82–3. doi: 10.1016/j.ijgo.2004.09.004. [DOI] [PubMed] [Google Scholar]
- 10.Cakir M, Mungan I, Karakas T, Girisken I, Okten A. Menstrual pattern and common menstrual disorders among university students in Turkey. Pediatr Int. 2007;49:938–42. doi: 10.1111/j.1442-200X.2007.02489.x. [DOI] [PubMed] [Google Scholar]
- 11.Burnett MA, Antao V, Black A, Feldman K, Grenville A, Lea R, et al. Prevalence of primary dysmenorrhea in Canada. J Obstet Gynaecol Can. 2005;27:765–70. doi: 10.1016/s1701-2163(16)30728-9. [DOI] [PubMed] [Google Scholar]
- 12.Dawood MY. Primary Dysmenorrhea Advances in Pathogenesis and management. Obstet Gynecol. 2006;108:824–34. doi: 10.1097/01.AOG.0000230214.26638.0c. [DOI] [PubMed] [Google Scholar]
- 13.Coco AS. Primary dysmenorthea. Am Fam Physician. 1999;6:486–96. [PubMed] [Google Scholar]
- 14.Savino F, Cresi F, Castagno E, Silvestro L, Oggero R. A randomized double-blind placebo-controlled trial of a standardized extract of Matricariae recutita, Foeniculum vulgare and Melissa officinalis (ColiMil) in the treatment of breastfed colicky infants. Phytother Res. 2005;19:335–40. doi: 10.1002/ptr.1668. [DOI] [PubMed] [Google Scholar]
- 15.Namavar Jahromi B, Tartifizadeh A, Khabnadideh S. Comparison of fennel and mefenamic acid for the treatment of primary dysmenorrhea. Int J Gynaecol Obstet. 2003;80:153–7. doi: 10.1016/s0020-7292(02)00372-7. [DOI] [PubMed] [Google Scholar]
- 16.Choi EM, Hwang JK. Antiinflammatory, analgesic and antioxidant activities of the fruit of Foeniculum vulgare. Fitoterapia. 2004;75:557–65. doi: 10.1016/j.fitote.2004.05.005. [DOI] [PubMed] [Google Scholar]
- 17.Modaress Nejad V, Asadipour M. Comparison of the effectiveness of fennel and mefenamic acid on pain intensity in dysmenorrhoea. East Mediterr Health J. 2006;12:423–7. [PubMed] [Google Scholar]
- 18.Döll M. The premenstrual syndrome: Effectiveness of Vitex agnus castus. Med Monatsschr Pharm. 2009;32:186–91. [PubMed] [Google Scholar]
- 19.Ma L, Lin S, Chen R, Wang X. Treatment of moderate to severe premenstrual syndrome with Vitex agnus castus (BNO 1095) in Chinese women. Gynecol Endocrinol. 2010;26:612–6. doi: 10.3109/09513591003632126. [DOI] [PubMed] [Google Scholar]
- 20.Ma L, Lin S, Chen R, Zhang Y, Chen F, Wang X. Evaluating therapeutic effect in symptoms of moderate-to-severe premenstrual syndrome with Vitex agnus castus (BNO 1095) in Chinese women. Aust N Z J Obstet Gynaecol. 2010;50:189–93. doi: 10.1111/j.1479-828X.2010.01137.x. [DOI] [PubMed] [Google Scholar]
- 21.Milsom I, Andersch B, Sundell G. The effect of flurbiprofen and naproxen sodium on intra-uterine pressure and menstrual pain in patients with primary dysmenorrhea. Acta Obstet Gynecol Scand. 1988;67:711–6. doi: 10.3109/00016349809004294. [DOI] [PubMed] [Google Scholar]
- 22.Chan WY, Fuchs F, Powell AM. Effects of naproxen sodium on menstrual prostaglandins and primary dysmenorrhea. Obstet Gynecol. 1983;61:285–91. [PubMed] [Google Scholar]
- 23.Dawood MY, Khan-Dawood FS. Clinical efficacy and differential inhibition of menstrual fluid prostaglandin F2alpha in a randomized, double-blind, crossover treatment with placebo, acetaminophen, and ibuprofen in primary dysmenorrhea. Am J Obstet Gynecol. 2007;196:31–5. doi: 10.1016/j.ajog.2006.06.091. [DOI] [PubMed] [Google Scholar]
- 24.Khodakrami N, Moatar F, Ghahiri A, Shahdan S. The Effect of an Iranian Herbal Drug on PrimaryDysmenorrhea: A Clinical Controlled Trial. J Midwifery Womens Health. 2009;54:401–4. doi: 10.1016/j.jmwh.2008.12.006. [DOI] [PubMed] [Google Scholar]
- 25.NazarPoor S, Azimi H. Comparison of fennel and mefenamic acid for the treatment of primary dysmenorrheal. J Mazand Univ Med Sci. 2006;17:54–61. [Google Scholar]
- 26.Modares Nejad V, Motamedi B, Asadi Pour M. Comparison between the Pain-Relief Effect of Fennelin and Mefenamic Acid on Primary Dysmenorrhea. J Rafsanjan Univ Med Sci. 2006;5:1–6. [Google Scholar]
- 27.Shah Hosseini Z, Amin GH, Salehi Sormaghi MH, Danesh MM, Abedian K. Double blind study of anti-primary dysmenorrhea effects of Vitagnus. J Mazendaran Univ Med Sci. 2005;15:15–21. [Google Scholar]


