Abstract
Background:
Although studies have demonstrated significant negative relationships between quality of life (QOL), fatigue, and the most common psychological symptoms (depression, anxiety, stress), the main ambiguity of previous studies on QOL is in the relative importance of these predictors. Also, there is lack of adequate knowledge about the actual contribution of each of them in the prediction of QOL dimensions. Thus, the main objective of this study is to assess the role of fatigue, depression, anxiety, and stress in relation to QOL of multiple sclerosis (MS) patients.
Materials and Methods:
One hundred and sixty-two MS patients completed the questionnaire on demographic variables, and then they were evaluated by the Persian versions of Short-Form Health Survey Questionnaire (SF-36), Fatigue Survey Scale (FSS), and Depression, Anxiety, Stress Scale-21 (DASS-21). Data were analyzed by Pearson correlation coefficient and hierarchical regression.
Results:
Correlation analysis showed a significant relationship between QOL elements in SF-36 (physical component summary and mental component summary) and depression, fatigue, stress, and anxiety (P < 0.01). Hierarchical regression analysis indicated that among the predictor variables in the final step, fatigue, depression, and anxiety were identified as the physical component summary predictor variables. Anxiety was found to be the most powerful predictor variable amongst all (β = −0.46, P < 0.001). Furthermore, results have shown depression as the only significant mental component summary predictor variable (β = −0.39, P < 0.001).
Conclusions:
This study has highlighted the role of anxiety, fatigue, and depression in physical dimensions and the role of depression in psychological dimensions of the lives of MS patients. In addition, the findings of this study indirectly suggest that psychological interventions for reducing fatigue, depression, and anxiety can lead to improved QOL of MS patients.
Keywords: Anxiety, depression, fatigue, multiple sclerosis, quality of life, stress
INTRODUCTION
According to the definition of World Health Organization (WHO), quality of life (QOL) is “the individual's perception of his/her position in life in the context of the culture, value systems in which he/she lives, and in relation to his/her goals, expectations, standards and concerns”.[1]
Studies have identically shown that patients with multiple sclerosis (MS) experience lower QOL compared to healthy control group.[2,3] Fatigue is the most common symptom of MS.[4] In addition to the chronic nature of the disease, lack of prognosis and a definitive therapy besides suffering from it from early adulthood causes several psychological symptoms among which depression, anxiety, and stress are the most common.[5] In recent years, there has been an increase in the number of studies on the relationship between these factors and QOL in MS.[2,3,6,7,8,9,10,11,12,13,14,15,16,17] Overall, these studies have demonstrated significant relationship between fatigue and psychological symptoms with QOL dimensions. In these studies, low QOL has been predicted by fatigue[3,8,9,10,12] and psychological symptoms, especially depression and anxiety.[2,3,6,8,9,10,11,12,14] There is skepticism about the relative importance of these predictors, especially fatigue and depression, as with regard to QOL of MS patients, some researches in which fatigue and depression were studied simultaneously have proved fatigue[12] to be the more powerful predictor and some others have proved depression[10] to be the stronger variable, while anxiety has been relevant only in some QOL studies[6,11] and in others it has not emerged as a significant predictor of QOL.[7] Moreover, there is a shortcoming in the studies of stress in relation to QOL of MS patients. For example, researchers have focused more on the effects of stress on exacerbations and relapses,[18,19,20] new brain magnetic resonance imaging (MRI) lesions,[21] inflammation,[22] radiological disease activity,[23] and depressive symptoms[24] of MS patients and mainly are marginalized the role of stress in reducing the physical and psychological aspects of patients QOL. But in a cross-sectional investigation, we have demonstrated that QOL has a negative correlation with all three symptoms of depression, anxiety, and stress (sequenced based on the degree of significance).[17]
Thus, the major weakness of previous studies is the existence of inconsistency in the findings about the contribution of each of the symptoms of fatigue, depression, anxiety, and stress in predicting the physical and psychological aspects of QOL of MS patients. Furthermore, some of the studies on QOL of MS patients have not attempted to control the confounding factors or have chosen very small sample size of patients.[25] Hence, the present study aims to evaluate the role of each of the mentioned symptoms in predicting the QOL of people with MS.
MATERIALS AND METHODS
Ethical considerations
Conducting the research was approved by the appropriate research committee of University of Guilan. Verbal information about the research study was provided for patients and written informed consent was given by patients. Patients also informed about their right to withdraw from the study at any time if they so desired.
Participants
This study was conducted in 2010 by descriptive cross-sectional method in patients with MS supported by the MS Society of Guilan Province (north of Iran). One hundred and sixty-two patients were selected by consecutive sampling as the study sample. Inclusion criteria included patients diagnosed with MS disease based on McDonald criteria,[26] with the diagnosis confirmed by a neurologist. The existence of MS disease was determined by the symptoms and clinical characteristics of the patient and also by the clinical evidence of lesion in two or more regions of the central nervous system (CNS). In order to confirm the damage, paraclinical measures such as MRI, evoked potential (EP), and cerebrospinal fluid (CSF) levels were used and patients who had a record at MS Society were confirmed of the diagnosis of the disease based on the mentioned findings. The exclusion criteria were: (a) occurrence of severe MS attack, (b) presence of severe cognitive problems due to which the patient was not able to fill in the tools and answer the interviewer, and (c) existence of any debilitating disease or physical issue associated with MS.
Procedure
This research was conducted in the MS Society of Guilan Province and Imam Reza Specialized and Sub-specialized Clinic. At the beginning of sampling, patients who satisfied the inclusion criteria were contacted and referred to the clinic. During the initial assessment, an explanation about the objectives of the study and the methods of research had been given to the patient and his/her family or companion. Also, patients were assured of the confidentiality of the measurements. Finally, after the patient and his/her family or companion signed the consent form, the patient entered the study. Data collection was with the help of a questionnaire and scale which included a section for demographic information and other sections for QOL assessment, fatigue severity, and psychological symptoms of MS patient. Subjects were asked to first fill up the demographic information list and then fill up the questionnaire and scale under the supervision of a psychologist who was present at the study location.
Measurement tools
Demographic variables list for MS patients
In this study, based on the demographic characteristics of patients, data related to age, sex, marital status, education level, personal and family background of visiting a psychologist or a psychiatrist, and duration of MS (in months) were collected.
Short-form health survey questionnaire
This questionnaire was prepared by Ware et al.[27] It includes 36 questions and provides two general measures of function: Physical component summary (PCS) and mental component summary (MCS).[28] Each question is scored from 1 to 100 and scores close to 100 indicate better QOL. In this regard, a study was conducted to confirm the validity and reliability of the Persian translation of Short-Form Health Survey Questionnaire (SF-36).[29] In general, the findings showed that Persian translation of SF-36 is an appropriate measuring tool for assessing health perceptions.
Fatigue severity scale
The Persian version of this tool had been used to measure the fatigue severity. This tool, which was initially created by Krupp to measure the fatigue level of MS patients, is a nine-item scale that examines the amount of fatigue with scores ranging from 1 to 7. The criterion validity of this tool has been reported as 0.68 and the internal consistency coefficient as 0.81.[30] By examining different aspects of the Persian version of Fatigue Severity Scale (FSS), it has been proved that the Persian version is an appropriate psychometric tool for assessing MS patients.[31]
Depression, anxiety, stress scale-21
Persian version of this instrument which was originally presented by Lovibond and Lovibond[32] has been used to assess depression, anxiety, and stress of patients. Espinola-Nadurille et al. have also recommended the use of tools that measure several symptoms in the cases of neurological disorders with psycho-neuro symptoms.[33] This scale has 21 questions and each of three sub-scales includes seven questions, the scores of which are obtained by summing up the scores of related questions. Evidences confirm the preliminary reliability and preliminary construct validity of the Persian translation of Depression, Anxiety, Stress Scale-21 (DASS-21).[34]
Statistical analyses
To describe the data in this study, descriptive statistical indicators like percentiles, mean, and standard deviation were used. In the inferential statistics section, we applied Pearson correlation analysis to test the relation hypotheses. Also, hierarchical regression was used in order to measure the influence of fatigue, depression, anxiety, and stress on PCS and MCS components. Finally, based on the results of this statistical analysis which included non-standardized coefficient (B), standard deviation coefficient (SEB), Beta coefficients (β), R square (R2), and F values, prediction models of PCS and MCS were derived for the psychological symptoms and fatigue.
RESULTS
Based on the inclusion and exclusion criteria, 162 patients of age between 16 and 58 years and with a mean age of 34.07 ± 9.44 years were included in this study. Of these, 29.6% were males and 70.4% were females (MS is more common in women). Marital status indicated that 21% were single, 75.9% married, 0.6% widowed, and 2.5% were divorcees. Moreover, 7.4% of patients had primary school education and 14.7%, 49.7%, and 28.2% had pre-high school, high school, and university education, respectively. Furthermore, findings show that 17.3% of MS patients had records of psychologist or psychiatrist appointments and 10.5% of MS patients stated that one of their family members had visited experts. Finally, average duration of disease in these patients was 56.94 ± 56.08 months.
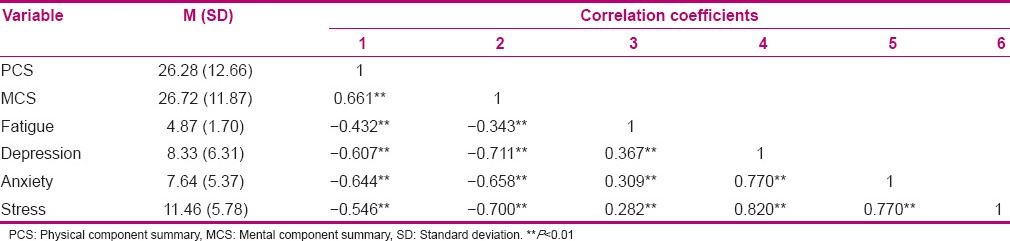
In order to test the hypothesis of supposed relations between PCS, MCS, fatigue, depression, anxiety, and stress, Pearson correlation method was applied. Table 1 indicates the mean, standard deviation, and intercorrelation between variables of the study. As can be seen, there was a high intercorrelation between the variables included in the study (P < 0.01).
Table 1.
Mean, standard deviation, and intercorrelation between variables (N=162)
Hierarchical regression analysis
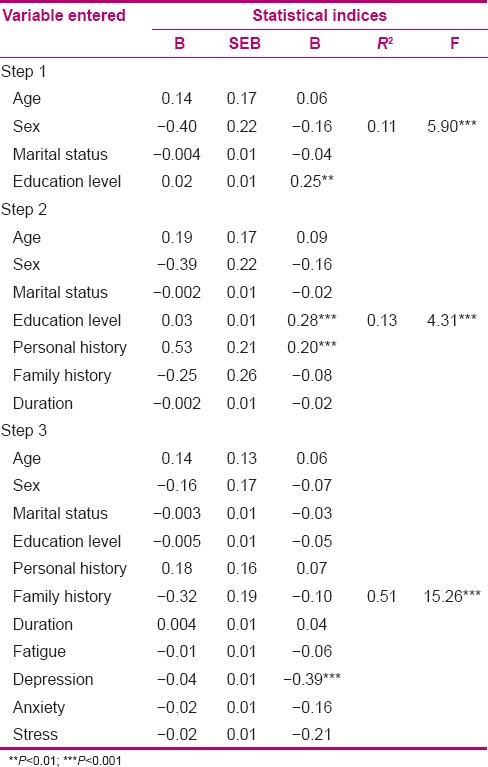
Hierarchical regression analysis was applied to assess the effects of entered variables on PCS and MCS [Tables 2 and 3].
Table 2.
Results of hierarchical regression to assess the effects of included variables on PCS
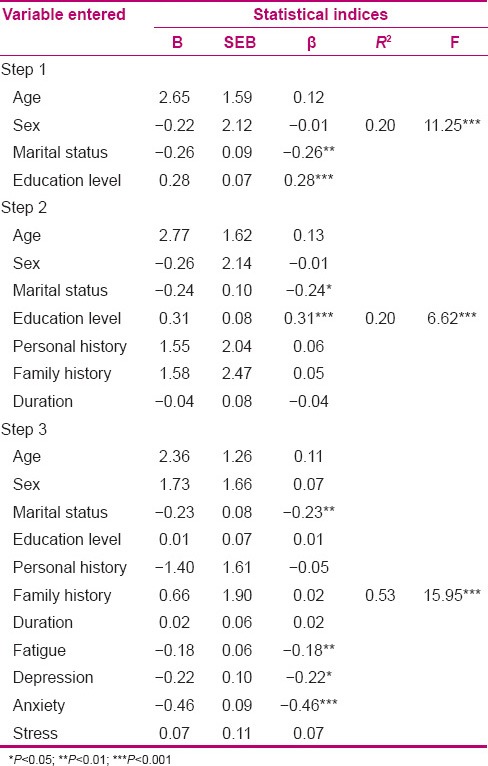
Table 3.
Results of hierarchical regression to assess the effects of included variables on MCS
It can be seen in Table 2 that the total variance of all entered variables was 0.53 (R2) in the third step (P < 0.001, F = 15.95). Yet, it has to be considered that additional variance in the final step, after controlling demographic variables such as age, sex, marital status, education level, personal and family background of visiting a psychologist or a psychiatrist, and duration of MS (in months), was estimated to be 0.33. It means that the main variables of the study have explained 33% of PCS variance, although it has to be noted that among the predictor variables, in the final step, only stress had not emerged as a significant variable (β = 0.07), whereas anxiety was the largest predictor variable at this stage (β = -0.46, P < 0.001) [Table 2].
Table 3 indicates that by considering all included variables, the total variance for MCS of third step was 0.51 (R)2 (F = 15.26, P < 0.001), although additional variance at this step and after controlling demographic variables was 0.38. Also, it has to be noted that among the predictor variables of the study and after controlling demographic factors, only depression stood as the significant predictor for MCS. This shows that depression alone has explained 38% of MCS variance (β = -0.39, P < 0.001) [Table 3].
DISCUSSION
The main objective of the present study was to find the role of psychological factors of depression, anxiety, and stress, and also fatigue in PCS and MCS components (in SF-36) of MS patients. Previous research evidences show that fatigue and psychological symptoms associated with MS are related to decrease in QOL of these patients.[2,6,8,9,10,12,14,17] The findings of these researches are in accordance with the results of this study, as there was a significant relationship between physical and mental aspects of QOL with the factors of fatigue and psychological symptoms [Table 1]. The main interpretation of this finding is that fatigue can strongly influence performing the daily activities and become a major reason for unemployment,[35] as the findings of McCabew and De Judicibus[36] indicated that the pressures lead to changes in the economic situation and dealing with these pressures is momentous for QOL of MS patients. Furthermore, psychological symptoms can affect the self-efficiency and self-worthiness perception of the MS patient because these symptoms can undermine the coping resources of the person. This issue can lead to deterioration in QOL of patients.
Moreover, results show that fatigue, depression, and anxiety are the major predictors of PCS for MS patients, while stress has not turned out to be a significant predictor [Table 2]. Our data conform with the previous reports.[13,37] Also, findings of this study have been verified by Tafillefer et al.[28] A recent study conducted on two groups of patients suffering from chronic fatigue syndrome (CFS) and MS indicated that in both groups, worse PCS in SF-36 was significantly associated with higher fatigue severity, though for none of these groups, MCS was not associated with fatigue severity. Results of this study also revealed that fatigue can only predict PCS and not MCS [Tables 2 and 3]. In accordance with our findings, Papuc and Stelmasiak found that fatigue and depression are the most powerful predictors for QOL of MS patients.[3] A basic explanation for fatigue can be the link between physical damages and fatigue, especially its physical aspects, since because of damage to different regions of brain, thinking and activities demand higher energy than before. On the other hand, muscles with spasticity work against each other; therefore, more force is needed to perform physical activities. It has to be considered that fatigue is caused by cellular MS and is the result of disease process. Demyelination makes it harder for neurons to send signals.[38] In fact, the increase in neuronal activity in cellular tissues, which occurs to compensate the problems, gradually leads to weakness of physical abilities and subsequently results in depletion of PCS in MS patients. Besides, one of the outcomes of depression is the feeling of lack of energy and illness that prevents the patient to endure physical pressures. Moreover, depression is probably associated with focal demyelinating lesions and malfunction of immune system.[39] These complications can lead to functional limitations and generalized disorder in the PCS of patients.
Yet, in this study, anxiety has been identified as the strongest significant predictor for PCS. In an earlier study, Chylova et al.[40] assessed the psychological situation of two groups of MS patients (using SF-36) and stated that anxiety was associated with the physical health situation of younger patients of MS. Although the findings of our study contradict the results of some studies,[7] the differences can be attributed to the tools used in studies. In the latter study, Zung Anxiety Rating Scale (ZARS) was used as a separate tool to measure anxiety,[7] whereas in this investigation, DASS, which assesses the psychological pathology of depression, anxiety, and stress, has been used. This could have affected the quality of findings, although it has to be noted that recent publications of MS have emphasized on the use of multi-symptom measuring tools.[33] Yet, the anxiety of MS patients can be explained by natural etiology theory or by bio-behavioral approaches that consider anxiety as an endogenous product which is created to confront hazardous stimuli and is naturally produced in situations wherein self is endangered - a mechanism that leads to drop in physiological functions and, therefore, decrease in indicators associated with QOL in patients. Also in this study, stress has not been identified as a significant variable for PCS. To explain this finding, it could be said that stress plays a common role in most of the personal and social behaviors of MS patients. Therefore, patients describe stress as “routine symptom”, so that whenever encountered a question from the stress sub-category in DASS, such as “I tended to over-react to situations”, they answered it as an usual experience or with low intensity. It must be noted that personal interpretations of the symptoms by patients play a critical role in their answers and ultimately their level of stress reported.
Our data showed that only depression is a significant predictor for MCS [Table 3]. This finding agrees with the previous reports on MS patients.[10,15] One of these studies showed depression as the most statistically significant predicting characteristic for MCS in SF-36.[10] Moreover, Füvesi et al. also found that depressed MS patients had their QOL become worse in a significant way.[41] Based on an interpretation of this finding, depression impairs motivation, interest, and collaboration of the patient; this consequently can affect vitality, social function, mental health, and generally MCS. Another interpretation is that depression can distort the viewpoints of people on the world and their health, and change it in a way that deteriorates their evaluation of self.[42]
Overall, the findings revealed the role of anxiety, fatigue, and depression in physical aspects and the role of depression in mental aspects of lives of MS patients. Clinical application of this finding is to suggest rehabilitation interventions that reduce fatigue and destructive mental symptoms and consequently improve the qualitative aspects of life. In this regard, QOL-based psychotherapy, a non-drug, non-attack, and economical therapy toward promotion of physical and mental dimensions of life, can be utilized. By these psychotherapies, we can target the anxiety and fear of progress of the disease in patients and improve their knowledge of the nature of MS and ways to manage it. Moreover, cognitive restructuring programs, training programs for accommodating with physical damages, and cognitive behavioral therapy can be conducted. Note that in these kinds of psychotherapies, MS patients should be encouraged to do more exercises and active pleasurable physical activities. It should be noted that (a) fatigue is described as a multi-dimensional construct with symptoms such as decline in activity, decrease in energy, and slowness of organs and (b) greater extent of functional limitations predicts negative psychological symptoms overtime. It has been previously revealed that exercise program[43] and aerobics[44] can decrease fatigue and depression, improve positive thinking, and enhance participation in social acts, and ultimately have a positive effect on QOL of patients. It is necessary to remember that MS is a progressive and changing disorder, so patients suffering from it experience numerous transforming symptoms. Thus, perceiving QOL in MS is complex.
Samples of this study were not homogenous in terms of level of care, disease severity, amount of hospital measures, quality of care after affliction (especially in family environment), and social support style. Further, in this study, we did not consider the role of drugs that the patients were taking. This issue can play a role in the appearance of symptoms assessed in this research. Also, the presented data are self-reported and this can increase the possibility of biased and tampered answers in several tools. Another limitation of our study is the small size which can affect the results. Thus, the findings of this study should be generalized with caution.
Our data stressed the importance of the factors of fatigue and psychological symptoms in physical and mental aspects of lives of MS patients. Therefore, our study suggests that future researches assess the treatment of fatigue and its psychological symptoms and its effect on QOL. Also, studies should aim more clearly at the possible contributing mechanisms in decreasing QOL of MS patients, such as immunomodulatory drugs, organic brain lesions due to disease, employment, and levels of coping. Finally, we suggest the use of experimental or longitudinal plans which provide the induction of causal relations between QOL and clinical and psychological factors in future researches.
CONCLUSION
This study revealed that PCS and MCS have significant negative relationships with any of the symptoms of fatigue, depression, anxiety, and stress. The results of the statistical analysis, after controlling for demographic and clinical variables, showed that fatigue, depression, and anxiety were the variables that significantly predicted PCS while anxiety appeared to have the strongest significance as a predictor. However, for MCS, only depression was identified as a significant variable. These results further highlight the impact of fatigue and psychological symptoms on QOL dimensions of patients with MS. Thus, based on the findings, management of patients’ psychological and clinical symptoms to improve their QOL through programs such as psychotherapy interventions, exercise, and aerobics is recommended.
ACKNOWLEDGMENT
The authors of this paper would like to thank all MS patients who participated in this study despite having many disease-related problems.
Footnotes
Source of Support: This research has been carried out without the support of any institution/organization
Conflict of Interest: Nil.
REFERENCES
- 1.Bonomi AE, Patrick DL, Bushnell DM, Martin M. Validation of the United States’ version of the World Health Organization Quality of Life (WHOQOL) instrument. J Clin Epidemiol. 2000;53:19–23. doi: 10.1016/s0895-4356(99)00123-7. [DOI] [PubMed] [Google Scholar]
- 2.Patti F, Cacopardo M, Palermo F, Ciancio MR, Lopes R, Restivo D, et al. Health-related quality of life and depression in an Italian sample of multiple sclerosis patients. J Neurol Sci. 2003;211:55–62. doi: 10.1016/s0022-510x(03)00040-6. [DOI] [PubMed] [Google Scholar]
- 3.Papuc E, Stelmasiak Z. Factors predicting quality of life in a group of Polish subjects with multiple sclerosis: Accounting for functional state, socio-demographic and clinical factors. Clin Neurol Neurosurg. 2012;114:341–6. doi: 10.1016/j.clineuro.2011.11.012. [DOI] [PubMed] [Google Scholar]
- 4.Kinkel RP. Fatigue in multiple sclerosis. Reducing the impact through comprehensive management. Int J MS Care. 2000;2:3–12. [Google Scholar]
- 5.McCabe MP. Mood and self-esteem, of persons with multiple sclerosis following an exacerbation. J Psychosom Res. 2005;59:161–6. doi: 10.1016/j.jpsychores.2005.04.010. [DOI] [PubMed] [Google Scholar]
- 6.Stenager E, Knudsen L, Jensen K. Multiple sclerosis: Correlation of anxiety, physical impairment and cognitive dysfunction. Ital J Neurol Sci. 1994;15:97–101. doi: 10.1007/BF02340120. [DOI] [PubMed] [Google Scholar]
- 7.Fruehwald S, Loeffler-Stastka H, Eher R, Saletu B, Baumhackl U. Depression and quality of life in multiple sclerosis. Acta Neurol Scand. 2001;104:257–61. doi: 10.1034/j.1600-0404.2001.00022.x. [DOI] [PubMed] [Google Scholar]
- 8.Amato MP, Ponziani G, Rossi F, Liedl CL, Stefanile C, Rossi L. Quality of life in multiple sclerosis: The impact of depression, fatigue and disability. Mult Scler. 2001;7:340–4. doi: 10.1177/135245850100700511. [DOI] [PubMed] [Google Scholar]
- 9.Janardhan V, Bakshi R. Quality of life in patients with multiple sclerosis: The impact of fatigue and depression. J Neurol Sci. 2002;205:51–8. doi: 10.1016/s0022-510x(02)00312-x. [DOI] [PubMed] [Google Scholar]
- 10.Merkelbach S, Sittinger H, Koenig J. Is there a differential impact of fatigue and physical disability on quality of life in multiple sclerosis? J Nerv Ment Dis. 2002;190:388–93. doi: 10.1097/00005053-200206000-00007. [DOI] [PubMed] [Google Scholar]
- 11.Janssens AC, van Doorn PA, de Boer JB, Kalkers NF, van der Meche FG, Passchier J, et al. Anxiety and depression influence the relation between disability status and quality of life in multiple sclerosis. Mult Scler. 2003;9:397–403. doi: 10.1191/1352458503ms930oa. [DOI] [PubMed] [Google Scholar]
- 12.Benedict RH, Wahlig E, Bakshi R, Fishman I, Munschauer F, Zivadinov R, et al. Predicting quality of life in multiple sclerosis: Accounting for physical disability, fatigue, cognition, mood disorder, personality, and behaviour change. J Neurol Sci. 2005;231:29–34. doi: 10.1016/j.jns.2004.12.009. [DOI] [PubMed] [Google Scholar]
- 13.Pittion-Vouyovitch S, Debouverie M, Guillemin F, Vandenberghe N, Anxionnat R, Vespignani H. Fatigue in multiple sclerosis is related to disability, depression and quality of life. J Neurol Sci. 2006;243:39–45. doi: 10.1016/j.jns.2005.11.025. [DOI] [PubMed] [Google Scholar]
- 14.Patti F, Russo P, Pappalardo A, Macchia F, Civalleri L, Paolillo A. FAMS study group: Predictors of quality of life among patients with multiple sclerosis: An Italian cross-sectional study. J Neurol Sci. 2007;252:121–9. doi: 10.1016/j.jns.2006.10.017. [DOI] [PubMed] [Google Scholar]
- 15.Brola W, Fudala M, Czernicki J. Effect of depression on quality of life of patients with multiple sclerosis. Med Rehabil. 2007;11:1–5. [Google Scholar]
- 16.Alshubaili AF, Awadalla AW, Ohaeri JU, Mabrouk AA. Relationship of depression, disability, and family caregiver attitudes to the quality of life of Kuwaiti persons with multiple sclerosis: A controlled study. BMC Neurol. 2007;7:31. doi: 10.1186/1471-2377-7-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Salehpoor GH, Kafi SM, Rezaei S, Hosseininezhad M, Salehi I. The relation between fatigue severity with psychological symptoms and quality of life in patients Multiple Sclerosis (MS) Zahedan J Res Med Sci (ZJRMS) 2012;14:80–6. [Google Scholar]
- 18.Ackerman KD, Heyman R, Rabin BS, Anderson BP, Houck PR, Frank E, et al. Stressful life events precede exacerbations of multiple sclerosis. Psychosom Med. 2002;64:916–20. doi: 10.1097/01.psy.0000038941.33335.40. [DOI] [PubMed] [Google Scholar]
- 19.Mitsonis CI, Zervas IM, Mitropoulos PA, Dimopoulos NP, Soldatos CR, Potagas CM, et al. The impact of stressful life events on risk of relapse in women with multiple sclerosis: A prospective study. Eur Psychiatry. 2008;23:497–504. doi: 10.1016/j.eurpsy.2008.06.003. [DOI] [PubMed] [Google Scholar]
- 20.Brown RF, Tennant CC, Sharrock M, Hodgkinson S, Dunn SM, Pollard JD. Relationship between stress and relapse in multiple sclerosis: Part I. Important features. Mult Scler. 2006;12:453–64. doi: 10.1191/1352458506ms1295oa. [DOI] [PubMed] [Google Scholar]
- 21.Mohr DC, Goodkin DE, Bacchetti P, Boudewyn AC, Huang L, Marrietta P, et al. Psychological stress and the subsequent appearance of new brain MRI lesions in MS. Neurology. 2000;55:55–61. doi: 10.1212/wnl.55.1.55. [DOI] [PubMed] [Google Scholar]
- 22.Mohr DC, Pelletier D. A temporal framework for understanding the effects of stressful life events on inflammation in patients with multiple sclerosis. Brain Behav Immun. 2006;20:27–36. doi: 10.1016/j.bbi.2005.03.011. [DOI] [PubMed] [Google Scholar]
- 23.Yamout B, Itani S, Hourany R, Sibaii AM, Yaghi S. The effect of war stress on multiple sclerosis exacerbations and radiological disease activity. J Neurol Sci. 2010;288:42–4. doi: 10.1016/j.jns.2009.10.012. [DOI] [PubMed] [Google Scholar]
- 24.Aikens JE, Fischer JS, Namey M, Rudick RA. A replicated prospective investigation of life stress, coping, and depressive symptoms in multiple sclerosis. J Behav Med. 1997;20:433–45. doi: 10.1023/a:1025547431847. [DOI] [PubMed] [Google Scholar]
- 25.Phillips LH, Saldias A, McCarrey A, Henry JD, Scott C, Summers F, et al. Attentional lapses, emotional regulation and quality of life in multiple sclerosis. Br J Clin Psychol. 2009;48:101–6. doi: 10.1348/014466508X379566. [DOI] [PubMed] [Google Scholar]
- 26.McDonald WI, Compston A, Edan G, Goodkin D, Hartung HP, Lublin FD, et al. Recommended diagnostic criteria for multiple sclerosis: Guidelines from the International Panel on the Diagnosis of Multiple Sclerosis. Ann Neurol. 2001;50:121–7. doi: 10.1002/ana.1032. [DOI] [PubMed] [Google Scholar]
- 27.Ware JE, Jr, Sherbourne CD. Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–83. [PubMed] [Google Scholar]
- 28.Taillefer SS, Kirmayer LJ, Robbins JM, Lasry JC. Psychological correlates of functional status in chronic fatigue syndrome. J Psychosom Res. 2002;53:1097–106. doi: 10.1016/s0022-3999(02)00566-4. [DOI] [PubMed] [Google Scholar]
- 29.Motamed N, Ayatollahi AR, Zare N, Sadeghi-Hassanabadi A. Validity and reliability of the Persian translation of the SF-36 version 2 questionnaire. East Mediterr Health J. 2005;11:349–57. [PubMed] [Google Scholar]
- 30.Krupp LB, LaRocca N, Muir-Nash J, Steinberg AD. The fatigue severity scale. Application to patients with multiple sclerosis and systemic lupus erythematosus. Arch Neurol. 1989;46:1121–3. doi: 10.1001/archneur.1989.00520460115022. [DOI] [PubMed] [Google Scholar]
- 31.Azimian M, Shahvarughi Farahani A, Dadkhah A, Fallahpour M, Karimlu M. Fatigue Severity Scale: The Psychometric Properties of the Persian-version in patients with Multiple Sclerosis. Res J Biol Sci. 2009;4:974–7. [Google Scholar]
- 32.Lovibond SH, Lovibond PF. 2nd ed. Sydney: Psychology Foundation; 1995. Manual for the depression anxiety stress scales. [Google Scholar]
- 33.Espinola-Nadurille M, Colin-Piana R, Ramirez-Bermudez J, Lopez-Gomez M, Flores J, Arrambide G, et al. Mental disorders in Mexican patients with multiple sclerosis. J Neuropsychiatry Clin Neurosci. 2010;22:63–9. doi: 10.1176/jnp.2010.22.1.63. [DOI] [PubMed] [Google Scholar]
- 34.Bayani AA. Reliability and preliminary evidence of validity of a Farsi version of the depression anxiety stress scales. Percept Mot Skills. 2010;111:107–14. doi: 10.2466/08.13.PMS.111.4.107-114. [DOI] [PubMed] [Google Scholar]
- 35.Bol Y, Duits AA, Hupperts RM, Vlaeyen JW, Verhey FR. The psychology of fatigue in patients with multiple sclerosis: A review. J Psychosom Res. 2009;66:3–11. doi: 10.1016/j.jpsychores.2008.05.003. [DOI] [PubMed] [Google Scholar]
- 36.McCabew MP, De Judicibus M. The Effects of Economic Disadvantage on Psychological Well-being and Quality of life among people with multiple sclerosis. J Health Psychol. 2005;10:163–73. doi: 10.1177/1359105305048562. [DOI] [PubMed] [Google Scholar]
- 37.MacAllister WS, Christodoulou C, Troxell R, Milazzo M, Block P, Preston TE, et al. Fatigue and Quality of Life in Pediatric Multiple Sclerosis. Mult Scler. 2009;15:1502–8. doi: 10.1177/1352458509345902. [DOI] [PubMed] [Google Scholar]
- 38.Lisak D. Overview of symptomatic management of Multiple Sclerosis. J Neurosci Nurs. 2001;33:224–30. doi: 10.1097/01376517-200110000-00002. [DOI] [PubMed] [Google Scholar]
- 39.Mao P, Reddy PH. Review: Is multiple sclerosis a mitochondrial disease? Biochim Biophys Acta. 2010;1802:66–79. doi: 10.1016/j.bbadis.2009.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chylova M, van Dijk GP, Rosenberger J, Nagyova I, Gavelova M, Gdovinova Z, et al. Depression, anxiety and health status in patients with multiple sclerosis. Eur Psychiatry. 2009;24:S901. [Google Scholar]
- 41.Fuvesi J, Bencsik K, Losonczi E, Fricska-Nagy ZS, Matyas K, Meszaros E, et al. Factors influencing the health-related quality of life in Hungarian multiple sclerosis patients. J Neurol Sci. 2010;293:59–64. doi: 10.1016/j.jns.2010.03.007. [DOI] [PubMed] [Google Scholar]
- 42.Mitchell AJ, Benito-Leon J, Gonzalez JM, Rivera-Navarro J. Quality of life and its assessment in multiple sclerosis: Integrating physical and psychological components of wellbeing. Lancet Neurol. 2005;4:556–66. doi: 10.1016/S1474-4422(05)70166-6. [DOI] [PubMed] [Google Scholar]
- 43.Mostert S, Kesserling J. Effects of a short-term exercise training program on aerobic fitness, fatigue, health perception and activity level of subjects with Multiple Sclerosis. Mult Scler. 2002;8:161–8. doi: 10.1191/1352458502ms779oa. [DOI] [PubMed] [Google Scholar]
- 44.Petajan JH, Gappmaier E, White AT, Spencer MK, Mino L, Hicks RW. Impact of aerobic training on fitness and quality of life in multiple sclerosis. Ann Neurol. 1996;39:432–41. doi: 10.1002/ana.410390405. [DOI] [PubMed] [Google Scholar]


