Abstract
Background:
Using non-pharmacological pain relief methods for reducing labor pain has always been one of the major concerns in obstetrics and gynecology.
Objective:
Comparing the effects of aromatherapy with jasmine and salvia on pain severity and labor outcome in nulliparous women.
Materials and Methods:
In this randomized clinical trial, 156 nulliparous women in labor were randomly selected and divided into salvia, jasmine, and control groups (52 in each group). The study duration was 6 months (from October 2009 to March 2010). Each group underwent aromatherapy using an incense mask for 15 min (distilled water for the control group). Pain severity was measured before and 30 and 60 min after the incense aromatherapy. Also, duration of the first and second stages of labor, first- and fifth-minute APGAR scores of the baby, and the frequency of labor type were measured and recorded in each group.
Results:
In comparison to the other groups, pain severity and duration of the first and second stages of labor were significantly lower in the aromatherapy group of salvia 30 min after the intervention (P = 0.001). However, no significant difference was found among the three groups regarding pain severity 60 min after the aromatherapy, first- and fifth-minute APGAR scores of the baby, and the frequency of labor type.
Conclusions:
The results of the present study indicated that aromatherapy with saliva had beneficial effects on pain relief, shortened the labor stages, and had no negative impact on the baby's APGAR score.
Keywords: Aromatherapy, Jasminum officinale, labor, nulliparous, Salvia officinale
INTRODUCTION
Women usually believe that labor is a physiological process with severe pain.[1] Most women are afraid of labor pain, which results in 8-22% of unnecessary cesarean sections.[2] Compared with vaginal labor, cesarean section is accompanied by increased risk of uterine infections, bleeding, urinary tract infection, and thromboembolism in mothers.[3] Most women require pain relief during their labor, and the pain relief strategies include application of pharmacological and non-pharmacological methods.[4] Labor pain management with minimal complications is one of the major challenges of the health team, and using non-pharmacological methods of pain relief is highly considered by both obstetricians and women.[5]
During the past two decades, interest in the use of Complementary and Alternative Medicine (CAM) has grown in the society. According to the reports of the World Health Organization (WHO), CAM is mostly used for preventive and protective purposes in developed and developing countries.[6] Most users of such therapies are women in their reproduction age[7,8] because women usually avoid pharmacological and invasive treatments and tend to receive complementary therapies for relieving the labor pain.[9] In obstetrics, CAM is usually used as a complementary treatment rather than a basic one.[10,11] The tendency toward using CAM in obstetrics is so high that some countries consider including training the application of these methods in the educational curriculum of nursing and obstetrics students.[12,13,14]
One of the methods in CAM is using aromatherapy which has extensive application in labor and promotion of obstetric services.[15] Aromatherapy has been used in different ways for treating or alleviating different kinds of diseases, such as cancer, to improve the life quality,[16] for treating topical and joint pains in the elderly,[17] improving primary dysmenorrhea,[18,19] improving the moods and increasing the capability of the staff in workplaces,[20] and treating anxiety, depression, and many symptoms of other diseases.[21] Aromatherapy has wide applications in women's health, including reduction of labor pain, treatment of dysmenorrhea, reduction of anxiety and depression, and treatment of vasomotor dysfunctions in menopause,[15,18] and no serious aromatherapy-caused complications have been reported thus far. Therefore, it has an overall acceptability among women.[22]
In general, various aromatherapy essences, including lavender, eucalyptus, salvia, jasmine, and rose, are used in labor.[23] These essences are used in different ways, such as in bathtub, as incense, by inhalation, and in massage.[24] Salvia is an herb with many applications, such as improving the gastrointestinal pain; strengthening the immune system; treating diabetes, diseases of mouth and gums, candidiasis infection, insomnia, premenstrual syndrome (PMS), and hot flashes in postmenopausal women; increasing the uterine contractions; and reducing labor pain.[25,26,27,28] Using the essence of salvia is contraindicated in those suffering from epilepsy during the first trimester of pregnancy and the lactation period and in patients with respiratory allergies.[29] Jasmine also has analgesic, sedative, and anti-depression properties. It has been reported to have dermatological, antiseptic, and anti-inflammatory properties as well.[30,31] Several studies have reported that jasmine reduces the labor pain, but is contraindicated in lactating women or in those with a history of asthma or respiratory allergies.[32] Despite the reported positive effects of aromatherapy and its effect in the reduction of labor pain, these results have not been confirmed in all the studies. Moreover, although women have welcomed aromatherapy, sporadic studies with inadequate number of samples (except in rare cases) have been conducted in this regard.[33,34] Aromatherapy using salvia and jasmine in combination with other essences has been well studied.[15] Public acceptance of aromatherapy and lack of sufficient and satisfactory evidence on the certainty of the effectiveness of this method in labor necessitate the need for further studies.[34] Already some findings have been reported on the pharmacological effects and the mechanism of essential oils, but most of them are from the field of behavioral and emotional sciences. Data regarding the safety and efficacy of these interventions in labor pain management are limited, wherein other complementary therapies have been combined with aromatherapy often.
Thus, the present study aims to compare the effect of aromatherapy with jasmine and salvia on the pain severity and labor outcome in nulliparous women.
MATERIALS AND METHODS
The present randomized clinical trial was conducted on 156 nulliparous women referring to the selected hospitals of Shiraz University of Medical Sciences, Shiraz, Iran due to labor pain. Based on the previous studies conducted on the issue, considering a power of 80% and α = 0.05, a sample size of 156 subjects (52 in each group) was determined for the study.
The study duration was 6 months (from October 2009 to March 2010). The selected women were physically healthy and had no limitations, such as asthma, history of allergy, or cold, for aromatherapy. They were aged between 18 and 30 years and had singleton pregnancy with cephalic presentation of the fetus (confirmed by sonography). They also showed no obstetric indications for cesarean section. All the women were in their 37th week of pregnancy or higher, in the active phase (3-4 cm of dil ation), when entering the study. They also used no methods of analgesia, anesthesia, or sedation during labor, because analgesic methods are not routinely used for labor pain. If the subjects suffered from bleeding, fetal distress, tetanic contractions, or respiratory allergies or needed pain augmentation with oxytocin or analgesic methods, they were excluded from the study. The samples were selected using convenience sampling and were classified into three groups using permuted block randomization. This study was not blinded.
Since it was not possible to conduct a blinded study, the days of intervention were separated. Using lottery draw, the first, second, and third days were allocated to aromatherapy with jasmine fragrance, distilled water (control), and salvia fragrance, respectively.
Due to the exclusion of the samples requiring emergency cesarean section, the number of subjects in the three groups was not equal in the investigation of the duration of labor stages.
The study data were collected using an information form that contained demographic information, current pregnancy characteristics, information on labor process, and possible complications of inhaling the fragrance. Besides, Visual Analog Scale (VAS) was used to measure pain severity. VAS is a ruler-like device which is numbered from 0 to 10, representing no pain and the highest intensity of pain, respectively. VAS has been proved to be reliable[35] and valid for the assessment of labor pain.[36]
Pain severity at 3-4 cm dilatation was measured and recorded before and 30 and 60 min after incense aromatherapy.
Preparation method of jasmine and salvia essences
There are many different species of salvia, such as Salvia officinalis, Salvia Meigan's Magic, and Salvia leucantha.[26]
In the present study, S. officinalis species was used. Flowering branches of this plant were dried and then powdered. The resulting powder was heated with a certain amount of distilled water and the released steam was immediately cooled down. The obtained liquid was a combination of essential oil and the extract. The extract was stored in dark jars in the refrigerator.
Since the boiling points of water and oil are different, the herbal extract, whose boiling point is close to that of water, was used instead of the oil essence in this study.
In order to determine the ingredients of the extract, gas chromatography mass spectrometry (Gc-Mass) analysis was done.
Gc-Mass is a gas chromatographic analytical method for volatile substances or materials that easily turn into gaseous phase. This method has a high separation ability, accuracy, speed, and diagnostic power. Gc is used to analyze organic materials and medicines. Evaporation pressure and emission of any substance, which depend on its interaction with the fixed phase, specify the retention of that substance in Gc-Mass.[37]
There are also many species of jasmine such as Jasminum officinale, Jasminum sambac, Jasminum flexile, Jasminum primulinum, and Jasminum angustifolium.[38]
J. officinale species was used in this study. Then, its extract was obtained and Gc-Mass analysis was run as mentioned above.
Analysis method of the extract
First, 20 ml of jasmine and salvia extracts was taken with 2 ml of chloroform solution. The resulting material was then dried using sodium sulfate salt and Gc-Mass analysis was performed on the concentrated as well as non-concentrated samples. The results showed that the extract of salvia was full of camphor, while no effective substance was found in the analysis of jasmine extract.
Intervention method
Instructions on the proper use of VAS chart were given to the study subjects individually and all the three groups received the same explanation. Then, 3 ml of the extract under consideration and 5 ml of water were poured in the extract tank of the incense device and its water tank, respectively. In order to avoid the interference of the fragrances, three identical incense devices were used for each group. The tanks were washed after using the device each time, in order to prevent the augmentation of the extract due to the repeated experiments.
The incense device had a mask with a height of 20 cm on which the person was asked to keep her face (the distance between the face and the device was 20 cm). The time needed for evaporation of 5 ml of water was 15 min. The labor room had one ventilation system and the rooms had the same ventilation conditions in all the three groups. Pain severity was measured using the VAS chart before the intervention and 30 min and 60 min after using the incense aromatherapy. Moreover, duration of the first and second stages of labor, first- and fifth-minute APGAR scores of the baby, and type of labor were measured and recorded.
Statistical analyses
Paired t-test was used in order to compare the variables before and after the intervention, and then, the results were analyzed using one-way analysis of variance (ANOVA). If the differences were significant, post-hoc test was used. Moreover, in case the number of samples in the groups was equal or unequal, least significant difference (LSD) and Scheffe tests were used, respectively. All the data analyses were performed using the SPSS statistical software.
Ethical consideration
After obtaining approval of the Research Vice-chancellor of Shiraz University of Medical Sciences and receiving the ethics code from the Ethics Committee and Iranian Registry of Clinical Trials (code: IRCT138811192515N1), the research objectives and methods were explained to the pregnant women who were qualified to enter the study and their written consents were obtained as well.
RESULTS
This study was carried out on 156 nulliparous women and each group consisted of 52 participants. The results showed no significant difference among the three groups in terms of age (P = 0.6), educational level (P = 0.9), gestational age (P = 0.1), and mean score of pain severity before the intervention (P = 0.5).
However, a significant difference was observed among the three groups concerning the mean of labor pain severity 30 min after the intervention. Post-hoc analysis and LSD test showed that those who were treated with salvia incense experienced significantly less pain (P = 0.001) [Table 1].
Table 1.
Comparison of the mean of pain severity before and 30 and 60 min after the intervention in the three groups (dilation 3-4 cm)
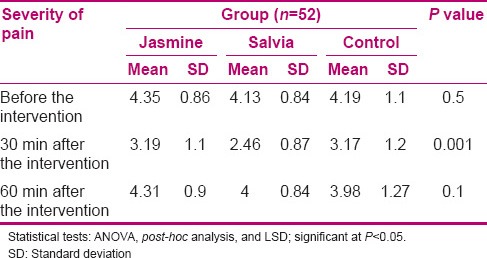
However, comparison of the mean of labor pain severity 60 min after the intervention demonstrated no significant difference among the three groups (P = 0.1) [Table 1].
During the experiment, four participants from the jasmine group, six participants from the salvia group, and seven participants from the control group were excluded from the study due to lack of progress in labor and the need for emergency cesarean. Therefore, the number of participants of the three groups was not equal for measurement of the duration of labor stages.
The results of ANOVA regarding the duration of the first and second stages of labor showed that the mean duration of the first stage of labor in the salvia group was significantly less than that of the other groups (P = 0.001) [Table 2]. Also, Scheffe test was used to compare every two groups individually and no difference was observed between jasmine and control groups regarding the mean duration of the first stage of labor (P = 0.4). The mean duration of the second stage of labor was also significantly lower in the salvia group compared to the other groups (P = 0.003) [Table 2].
Table 2.
Comparison of the mean duration of first and second stages of labor in the three groups
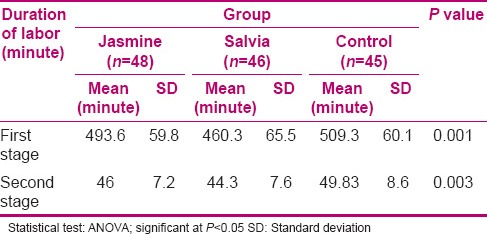
Nevertheless, the results of Scheffe test indicated no significant difference between jasmine and control groups regarding the mean duration of the second stage of labor (P = 0.5).
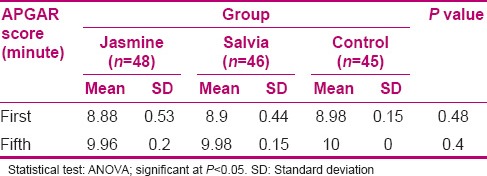
Also, no significant difference was found among the three groups concerning the mean of babies’ first- and fifth-minute APGAR scores (P = 0.4 and P = 0.48, respectively) [Table 3].
Table 3.
Comparison of the mean of the first- and the fifth-minute APGAR scores in the three groups
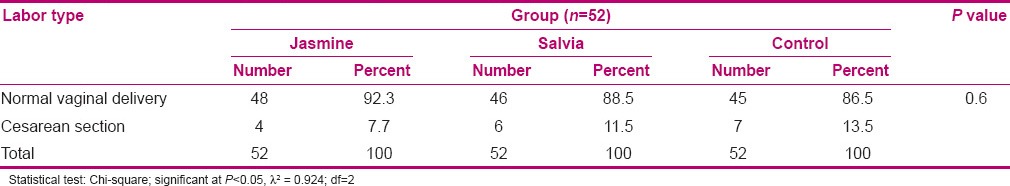
Comparison of the frequency of labor type also revealed no significant difference among the three study groups (P = 0.6) [Table 4].
Table 4.
Comparison of the frequency of labor type in the three groups
DISCUSSION
The first objective of the present study was to compare the effects of aromatherapy with jasmine and salvia on the labor pain severity in nulliparous women. Inhalation technique of aromatherapy using an incense device was applied in this study.
According to the results, 30 min after the intervention, the severity of labor pain showed that salvia incense was effective in causing pain relief; however, this difference was not statistically significant 60 min after the intervention. Burns et al. (2000)[15] studied the effects of aromatherapy on reduction of labor pain, anxiety, and fear in 8058 pregnant women for 8 years (1990-1998). In their study, 60% of the mothers stated that their pain was effectively relieved by salvia and chamomile. Also, their anxiety and fear were reduced by lavender and frankincense,[15] which was consistent with the results of the present study. However, these results have not been observed in the studies with smaller sample sizes.[33]
In the past, Melzak's theory, known as the theory of gate, was used for explaining how pain is controlled by non-pharmacological methods. This theory has been promoted as the theory of neuromatrix in recent years.[34] Neuromatrix theory supports the idea that pain concept and its perception depend on the interaction of mental, physical, and spiritual factors.[39] The major differences between the present study and the one by Burns et al. were the large number of samples, duration of the study, and use of different essences and combining them with each other in the study conducted by Burns et al. (2000).
In another study, Burns and Blamey used different aromatherapy oils, such as saliva, jasmine, lavender, and lemon, during the labor in various ways, including inhalation, massage, and using the oil in bathtub, for 6 months and reported the positive effects of the extracts in reducing the pain and anxiety in women,[23] which is partly consistent with the findings of the present study. Nonetheless, the main difference was in the application of different methods and combination of the extracts. In some studies, in order to increase the effectiveness of aromatherapy, the length of inhalation or incense is increased.[40] This period was 15 min in the present study. Another factor is dosage of the essential oils.[41] In the present study, 3 ml of the extracts (salvia or jasmine) and 5 ml of water were used, which are considered as effective dosages.[15] Type of aroma is also an important factor. The odor of aroma activates the olfactory nerve cells, eventually motivating the limbic system. Depending on the type of aroma, different neurotransmitters are released from the nerve cells.[40] One of the most important factors mentioned about aromatherapy is its impact on memory because smells stimulate memories, enable people to review the details of events and emotions, and thereby affect the severity of pain perception.[24] Many studies have also indicated anxiety as one of the most important factors that influence the severity of pain perception, and mother's anxiety during labor is the most important psychological factor affecting the severity of labor pain.[42,43] In a study conducted by Rho and Han which investigated the effect of aromatherapy with lavender, chamomile, rosemary, and lemon on anxiety and self-confidence in older women, anxiety decreased and self-confidence increased.[44]
Using aromatherapy oils reduces the stress hormones and increases the secretion of beta-endorphins resulting in reduced level of anxiety and, consequently, reduced pain perception.[15] In some studies reporting the beneficial effects of aromatherapy in reducing the labor pain, aromatherapy was used in combination with other methods, such as massage.[22] For instance, in the study by Dhany et al., application of aromatherapy massage dramatically decreased the use of other methods of analgesia and anesthesia in labor and reduced anxiety in the patients.[45]
The second objective of this study was to compare the effect of aromatherapy with jasmine and salvia on the duration of the first and second stages of labor. The results showed that incense of salvia shortened the duration of the first and second stages of labor.
Hur and Park observed the effect of aromatherapy with lavender and rose on the reduction of labor duration,[46] which was consistent with the results of the present study. The main difference between these studies is in the type of the essence used and its composition. Nevertheless, these results have not been confirmed in other studies with small sample sizes.[47] Burns and Blamey reported decreased pain, increased consciousness, decreased anxiety, and strengthened uterine power as the effects of aromatherapy.[23]
These mechanisms seem to be effective in reducing the duration of labor stages and increasing the cooperation of mothers during labor. Another systematic study reported that application of salvia and jasmine could increase the level of oxytocin as an effective factor in labor initiation. Hence, they are specifically used in post date pregnancies and their overuse may result in hypertonicity of uterus and fetal distress.[48]
The third objective of this study was to compare the effect of aromatherapy on the babies’ first- and fifth-minute APGAR scores. The results showed no significant difference among the three groups regarding the first- and fifth-minute APGAR scores of the babies, which is similar to the findings of the study performed by Burns et al. Other studies have also shown that aromatherapy has no negative effects on the baby's APGAR score.[46] The study results also revealed no significant difference between the groups regarding the frequency of labor type. This result is similar to those of many other studies conducted on the issue.[34,46]
The limitations of this study included not using a combination of essences and not measuring the anxiety level. Besides, aromatherapy was only used as incense. In this method, preparation of the essences is quite time consuming. Moreover, each patient needs a separate tank in this method, which might increase the costs.
CONCLUSION
Results of the present study show that incense aromatherapy with salvia can be effective in reducing the labor pain and has no adverse effects on the baby's APGAR. Of course, further studies with larger sample sizes and diversified combination of aromatherapy essences are recommended in order to compare different methods and measure the anxiety level.
ACKNOWLEDGMENTS
The present article was extracted from the thesis written by Shahla Maghbool and was financially supported by Shiraz University of Medical Sciences (grant number: 4712). The authors would like to thank pregnant mothers who helped them in sampling and performing this research. The authors appreciate the Research Improvement Center of Shiraz University of Medical Sciences, Shiraz, Iran and Ms. A. Keivanshekouh for their help in improving the language of the manuscript.
Footnotes
Source of Support: Shiraz University of Medical Sciences
Conflict of Interest: None declared.
REFERENCES
- 1.Lowe NK. The nature of labor pain. Am J Obstet Gynecol. 2002;186:16–24. doi: 10.1067/mob.2002.121427. [DOI] [PubMed] [Google Scholar]
- 2.Saisto T, Kaaja R, Ylikorkala O, Halmesmäki E. Reduced pain tolerance during and after pregnancy in women suffering from fear of labor. Pain. 2001;93:123–7. doi: 10.1016/S0304-3959(01)00302-5. [DOI] [PubMed] [Google Scholar]
- 3.Ronsmans C, Holtz S, Stanton C. Socioeconomic differentials in caesarean rates in developing countries: A retrospective analysis. Lancet. 2006;368:1516–23. doi: 10.1016/S0140-6736(06)69639-6. [DOI] [PubMed] [Google Scholar]
- 4.Jones L, Othman M, Dowswell T, Alfirevic Z, Gates S, Newburn M, et al. Pain management for women in labour: An overview of systematic reviews. Cochrane Database Syst Rev. 2012;14:CD009234. doi: 10.1002/14651858.CD009234.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Simkin P, Bolding A. Update on nonpharmacologic approaches to relieve labor pain and prevent suffering. J Midwifery Womens Health. 2004;49:489–504. doi: 10.1016/j.jmwh.2004.07.007. [DOI] [PubMed] [Google Scholar]
- 6.Bodeker G, Ong CK, Grundy C, Burford G, Shein K. Kobe: WHO Centre; 2005. WHO Global Atlas of Traditional, Complementary and Alternative Medicine; pp. 23–8. [Google Scholar]
- 7.Hall HG, McKenna LG, Griffiths DL. Midwives’ support for Complementary and Alternative Medicine: A literature review. Women Birth. 2012;25:4–12. doi: 10.1016/j.wombi.2010.12.005. [DOI] [PubMed] [Google Scholar]
- 8.Eisenberg DM, Davis RB, Ettner SL, Appel S, Wilkey S, Van Rompay M, et al. Trends in alternative medicine use in the United States, 1990-1997: Results of a follow-up national survey. JAMA. 1998;280:1569–75. doi: 10.1001/jama.280.18.1569. [DOI] [PubMed] [Google Scholar]
- 9.Smith CA, Collins CT, Crowther CA. Aromatherapy for pain management in labour. Cochrane Database Syst Rev. 2011;6:CD009215. doi: 10.1002/14651858.CD009215. [DOI] [PubMed] [Google Scholar]
- 10.Allaire AD, Moos MK, Wells SR. Complementary and alternative medicine in pregnancy: A survey of North Carolina certified nurse-midwives. Obstet Gynecol. 2000;95:19–23. doi: 10.1016/s0029-7844(99)00481-0. [DOI] [PubMed] [Google Scholar]
- 11.Herman PM, Craig BM, Caspi O. Is complementary and alternative medicine (CAM) cost-effective? A systematic review. BMC Complement Altern Med. 2005;5:11. doi: 10.1186/1472-6882-5-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stuttard P, Walker E. Integrating complementary medicine into the nursing curriculum. Complement Ther Nurs Midwifery. 2000;6:87–90. doi: 10.1054/ctnm.1999.0452. [DOI] [PubMed] [Google Scholar]
- 13.Mitchell M, Doyle M. Complementary therapies in the midwifery curriculum. Pract Midwife. 2002;5:40. [PubMed] [Google Scholar]
- 14.Mitchell M, Williams J. Integrating complementary therapies. Pract Midwife. 2006;9:12–5. [PubMed] [Google Scholar]
- 15.Burns EE, Blamey C, Ersser SJ, Barnetson L, Lloyd AJ. The use of aromatherapy in intrapartum midwifery practices an observational study. Complement Ther Nurs Midwifery. 2000;6:33–4. doi: 10.1054/ctnm.1999.0901. [DOI] [PubMed] [Google Scholar]
- 16.Fellowes D, Barnes K, Wilkinson S. Aromatherapy and massage for symptom relief in patients with cancer. Cochrane Database Syst Rev. 2008;8:CD002287. doi: 10.1002/14651858.CD002287.pub2. [DOI] [PubMed] [Google Scholar]
- 17.Yip YB, Tam AC. An experimental study on the effectiveness of massage with aromatic ginger and orange essential oil for moderate-to-severe knee pain among the elderly in Hong Kong. Complement Ther Med. 2008;16:131–8. doi: 10.1016/j.ctim.2007.12.003. [DOI] [PubMed] [Google Scholar]
- 18.Han SH, Hur MH, Buckle J, Choi J, Lee MS. Effect of aromatherapy on symptoms of dysmenorrhea in college students: A randomized placebo-controlled clinical trial. J Altern Complement Med. 2006;12:535–41. doi: 10.1089/acm.2006.12.535. [DOI] [PubMed] [Google Scholar]
- 19.Ou MC, Hsu TF, Lai AC, Lin YT, Lin CC. Pain relief assessment by aromatic essential oil massage on outpatients with primary dysmenorrhea: A randomized, double-blind clinical trial. J Obstet Gynaecol Res. 2012;38:817–22. doi: 10.1111/j.1447-0756.2011.01802.x. [DOI] [PubMed] [Google Scholar]
- 20.Heuberger E, Ilmberger J. The influence of essential oils on human vigilance. Nat Prod Commun. 2010;5:1441–6. [PubMed] [Google Scholar]
- 21.Hongratanaworakit T. Aroma-therapeutic effects of massage blended essential oils on humans. Nat Prod Commun. 2011;6:1199–204. [PubMed] [Google Scholar]
- 22.Tillett J, Ames D. The uses of aromatherapy in women's health. J Perinat Neonatal Nurs. 2010;24:238–45. doi: 10.1097/JPN.0b013e3181ece75d. [DOI] [PubMed] [Google Scholar]
- 23.Burns E, Blamey C. Complementary medicine: Using aromatherapy in childbirth. Nurs Times. 1994;90:54–60. [PubMed] [Google Scholar]
- 24.Goldberg L. 2nd edn. Cheltenham: Nelson Thornes Ltd; 2001. Massage and aromatherapy: A practical approach; pp. 63–5. [Google Scholar]
- 25.Schwiertz A, Duttke C, Hild J, Müller HJ. In vitro activity of essential oils on microorganisms isolated from vaginal infections. Int J Aromatherapy. 2006;16:169–74. [Google Scholar]
- 26.Clebsch B, Barner CD. Portland, Oregon: Timber Press; 2003. The new book of Salvias: Sages for every garden; pp. 16–22. [Google Scholar]
- 27.Perry NS, Bollen C, Perry EK, Ballard C. Salvia for dementia therapy: Review of pharmacological activity and pilot tolerability clinical trial. Pharmacol Biochem Behav. 2003;75:651–9. doi: 10.1016/s0091-3057(03)00108-4. [DOI] [PubMed] [Google Scholar]
- 28.Bommer S, Klein P, Suter A. First time proof of sage's tolerability and efficacy in menopausal women with hot flushes. Adv Ther. 2011;28:490–500. doi: 10.1007/s12325-011-0027-z. [DOI] [PubMed] [Google Scholar]
- 29.Shinde P, Patil P, Bairagi V. Herbs in pregnancy and lactation: A review appraisal. IJPSR. 2012;3:3001–6. [Google Scholar]
- 30.Hongratanaworakit T. Stimulating effect of aromatherapy massage with jasmine oil. Nat Prod Commun. 2010;5:157–62. [PubMed] [Google Scholar]
- 31.Rapini RP, Bolognia JL, Jorizzo JL. Vol. 2. St. Louis: Mosby; 2007. Dermatology; pp. 225–30. [Google Scholar]
- 32.Price SH, Price L. 4th ed. London: Elsevier Churchill Livingstone; 2012. Aromatherapy for health professionals; pp. 443–5. [Google Scholar]
- 33.Hur MH, Oh HY, Park YS. Effects of aromatherapy on labor pain and perception of childbirth experience. Korean J Women Health Nurs. 2005;11:135–41. [Google Scholar]
- 34.Burns E, Zobbi V, Panzeri D, Oskrochi R, Regalia A. Aromatherapy in childbirth: A pilot randomised controlled trial. BJOG. 2007;114:838–44. doi: 10.1111/j.1471-0528.2007.01381.x. [DOI] [PubMed] [Google Scholar]
- 35.Gaston-Johansson F. Measurement of pain: The psychometric properties of the Pain-O-Meter, a simple, inexpensive pain assessment tool that could change health care practices. J Pain Symptom Manage. 1996;12:172–81. doi: 10.1016/0885-3924(96)00128-5. [DOI] [PubMed] [Google Scholar]
- 36.Mårtensson L, Stener-Victorin E, Wallin G. Acupuncture versus subcutaneous injections of sterile water as treatment for labour pain. Acta Obstet Gynecol Scand. 2008;87:171–7. doi: 10.1080/00016340701797799. [DOI] [PubMed] [Google Scholar]
- 37.Amirav A, Gordin A, Poliak M, Alon T, Fialkov AB. Gas Chromatography Mass Spectrometry with Supersonic Molecular Beams. J Mass Spectrom. 2008;43:141–63. doi: 10.1002/jms.1380. [DOI] [PubMed] [Google Scholar]
- 38.Singh AK. New Delhi: New India Publishing; 2006. Flower Crops: Cultivation and Management; pp. 43–7. [Google Scholar]
- 39.Trout KK. The neuromatrix theory of pain: Implications for selected nonpharmacologic methods of pain relief for labor. J Midwifery Womens Health. 2004;49:482–8. doi: 10.1016/j.jmwh.2004.07.009. [DOI] [PubMed] [Google Scholar]
- 40.Fayazi S, Babashahi M, Rezaei M. The effect of inhalation aromatherapy on anxiety level of the patients in preoperative period. Iran J Nurs Midwifery Res. 2011;16:278–83. [PMC free article] [PubMed] [Google Scholar]
- 41.Kyle G. Evaluating the effectiveness of aromatherapy in reducing levels of anxiety in palliative care patients: Results of a pilot study. Complement Ther Clin Pract. 2006;12:148–55. doi: 10.1016/j.ctcp.2005.11.003. [DOI] [PubMed] [Google Scholar]
- 42.Lang AJ, Sorrell JT, Rodgers CS, Lebeck MM. Anxiety sensitivity as a predictor of labor pain. Eur J Pain. 2006;10:263–70. doi: 10.1016/j.ejpain.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 43.Curzik D, Jokic-Begic N. Anxiety sensitivity and anxiety as correlates of expected, experienced and recalled labor pain. J Psychosom Obstet Gynaecol. 2011;32:198–203. doi: 10.3109/0167482X.2011.626093. [DOI] [PubMed] [Google Scholar]
- 44.Rho KH, Han SH, Kim KS, Lee MS. Effects of aromatherapy massage on anxiety and self-esteem in korean elderly women: A pilot study. Int J Neurosci. 2006;116:1447–55. doi: 10.1080/00207450500514268. [DOI] [PubMed] [Google Scholar]
- 45.Dhany AL, Mitchell T, Foy C. Aromatherapy and Massage Intrapartum Service Impact on Use of Analgesia and Anesthesia in Women in Labor: A Retrospective Case Note Analysis. J Altern Complement Med. 2012;18:932–8. doi: 10.1089/acm.2011.0254. [DOI] [PubMed] [Google Scholar]
- 46.Hur MH, Park MH. Effects of Aromatherapy on Labor Process, Labor Pain, Labor Stress Response and Neonatal Status of Primipara: Randomized Clinical Trial. Korean J Obstet Gynecol. 2003;46:776–83. [Google Scholar]
- 47.Calvert I. Ginger: An essential oil for shortening labour? Pract Midwife. 2005;8:30–4. [PubMed] [Google Scholar]
- 48.Evans M. Postdates pregnancy and complementary therapies. Complement Ther Clin Pract. 2009;15:220–4. doi: 10.1016/j.ctcp.2009.09.002. [DOI] [PubMed] [Google Scholar]


