Abstract
Background:
Sleep is one of the basic human needs and sleep deprivation causes numerous undesirable effects on the human body and mind, especially in the intensive care unit (ICU) patients. It seems that noise and light are important environmental factors interrupting sleep in these patients. This study was carried out to determine the effect of earplugs and eye mask on Iranian patients’ sleep quality in ICU.
Materials and Methods:
In this cross-over clinical trial, 50 patients in the ICUs of Al-zahra Medical Center in Isfahan in 2012 were selected by convenient sampling method and randomly assigned to two groups. In group A, patients wore earplugs and eye mask in the first night during their sleep and slept without earplugs and eye mask in the second night, and the intervention was conversely conducted in group B. Verran and Snyder-Halpern Sleep Scales were used to measure the patients’ sleep quality. The data were analyzed by paired t-test, independent t-test, one-sample t-test, and one-way analysis of variance (ANOVA) through SPSS version 18.
Results:
Effect of the intervention on sleep effectiveness was positive, and there were significant differences (P < 0.001) between treatment night and control night, and also within each group (P < 0.001). Effect of the interventions on sleep disturbance was positive, and there was a significant difference at treatment night compared to the control night between groups and within each group (P < 0.001). Also, the mean scores for sleep supplementation were measured after the second night, and the results showed the scores significantly increased in the intervention group compared to the control group (P < 0.001, ER = 47, F = 22.1). In addition, carryover effects for sleep efficiency and sleep disturbance were positive, but periodic effects for sleep efficiency and sleep disturbance were negative and positive, respectively.
Conclusions
: Although wearing earplugs and eye mask is a cost-effective and safe method and can improve perceived sleep quality in ICU patients, further research is needed to demonstrate the effect of this method.
Keywords: Earplugs, eye mask, intensive care units, Iran, sleep
INTRODUCTION
Sleep, like food and water, is a basic need for the human beings[1] and plays a major role in the functions of immune system and cognitive and musculoskeletal system.[2]
In fact, sleep is one of the effective factors in individuals’ quality of life, and in addition to its vital role in maintaining body physiologic function, it speeds up the process of healing in injured tissues.[3] Despite many unknown aspects of the role of sleep in health and diseases, lack of sleep is directly associated with poor mental and physical function.[4] Deprivation of sleep can be accompanied with important complications[5] and negatively influences individuals’ and public health.[6]
Research shows that about 56% of the patients are deprived from sleep on their first day of hospitalization,[7] while many of them consider sleep disorders as a natural experience resulting from their hospitalization.[8] Prevalence of sleep disorders in intensive care units (ICUs) is especially notable as sleep is one of the common problems of the patients hospitalized in ICUs.[9,10,11,12,13] Patients hospitalized in ICUs are awake about 50-60% of their sleep time, and at the most in 3-5% of the remaining time, reach the third and fourth stages of sleep, which play the healing stages of sleep.[1] Weinhouse quoting from Rotendy states that 38.5% of saved critical patients who underwent mechanical ventilation for at least 48 h were not able to sleep; 40% of them remembered waking up at midnight and 35% hardly fell asleep during their hospitalization.[14] Nelson et al. mentioned that sleep disorder was the second stressful factor in cancer patients hospitalized in ICUs.[1,15]
In addition, former research showed a tight correlation between sleep disorder and systemic diseases, and mortality.[16] Sleep disorder can also reduce respiratory muscular resistance and interfere with patients’ separation from mechanical ventilation.[17]
In critical care units, numerous factors can attribute to sleep disorder.[18] Noise, light, treatment interventions, pain procedures, and psychological and mental stress are among the few factors which cause sleep disorder in hospitals.[8,19,20] Critical patients face such factors, and despite the intensity of their disease, they experience more caring interventions such as checking the vital signs, X-rays, phlebotomy, and medication.[14] Generally, it can be mentioned that physiologic, psychological, mental and environmental factors play a role in the incidence of sleep deprivation in hospitalized patients. Meanwhile, the basic physiologic factors including medications, pain and disease, and main psychological and mental factors like stress and concerns are the causes for sleep disorder.[8]
Therefore, despite numerous factors which affect sleep disorders, the environment of ICUs is considered to be a possible important factor for sleep disorder.[6] A convenient environment is essential for a quality sleep, but the environment in an ICU is not only strange and unfamiliar for the patient but also contains lots of environmental stimulators which can negatively affect sleep.[21,22]
Numerous studies from 1970 showed that ICUs contain high levels of noise, making them stressful for the staffs and patients.[21] Research shows that mean noise in ICU is 53-65 dB and reaches over 80 dB in a 24-h period.[8,14] Meanwhile, based on the guideline published by the World Health Organization (WHO), the optimum standard noise levels during day and night are 35 and 30 dB, respectively, and higher levels can lead to negative effects such as sleep disorders, low atrial O2 saturation, hypertension, and delayed healing, and an increase in the risk of re-hospitalization.[23]
Another important environmental factor causing sleep disorder in ICU is exposure to light.[17] Regular light and dark cycles which are used for regulation of body biologic clock play a major role in sleep and wake-up cycle.[4] Being exposed to light is the initial factor which affects circadian rhythm. On the other hand, nightly secretion of melatonin is prohibited with exposure to light. In recent decades, some research has been conducted in relation to melatonin secretion in patients hospitalized in ICU, which shows these patients suffer from acute sleep deprivation as a result of low nocturnal secretion of melatonin.[17]
ICUs disturb natural light–dark cycle in two ways. Firstly, the patients in these wards may be deprived of natural light due to absence of windows, and secondly, artificial lights may remain on in ICUs during the entire 24 h, while exposures to natural light during day time and darkness during night are essential to preserve a strong circadian rhythm for secretion of melatonin and for patients’ rest.[4] The light in ICUs has been reported to be averagely 5-1400 lux[14,17] and this issue has highlighted the role of the level of light in ICUs as a disturbing factor for sleep and circadian rhythm.[14]
Based on all aforementioned issues, it can be concluded that noise and inappropriate light are directly associated with shortage of sleep, and with regard to the hazardous effects of this shortage, as a known phenomenon, on ICU patients,[24] effective interventions to promote the quality of sleep among these patients are essential.[17] In fact, control of light and noise can control anxiety and improve patients’ sleep through a non-medicational approach.[25]
One of the ways to control light and noise is to use earplugs and eye mask, which are considered not only cost-effective and noninvasive but also convenient to use.[26] Richardson et al.,[26] Wallace et al.,[27] and Fung[17] showed that using tools such as earplugs and eye mask positively affect sleep, and through a cost-effective, convenient, and safe treatment, longer period of sleep with better quality is achieved.
Despite recommendations of using earplugs and eye mask in ICUs, their efficiency has not been proved. On one hand, most of the research in this field has focused on just reduction of environmental noise and not concurrent use of both noise- and light-reducing techniques.[17] On the other hand, use of self-report tools is an applicable method to assess patients’ sleep,[28] and patients’ personal report of sleep (like report of pain) is the best criterion for sleep quality measurement. Although the individuals can best judge about their falling or not falling asleep,[25] most of the research in this field has focused on the use of physiologic tools like polysomnography or actigraphy, while mental investigation tools of sleep quality have been less used. In addition, lack of local studies in this field in ICUs led us to conduct this study to investigate the effect of earplugs and eye mask on patients’ perceived sleep quality in ICU.
MATERIALS AND METHODS
This is a two-group two-step cross-over clinical trial in which the subjects were also the control group. In order to calculate the sample size, the researchers f ound the mean and standard deviation needed to determine the sample size, and based on that, S1 = 19.9, X1 = 32, and S2 = 18.9 and X2 = 42.9 were obtained.[8]
Then, based on the confidence interval of 95% and α =0.05 for the study and with the help of a statistically valid chart and sample size calculation formula, sample size of 24 was obtained for each group. Keeping in mind subjects dropping out, a sample size of 25 was finalized for each group. Next, the researcher selected 50 patients hospitalized in ICUs of the selected hospitals affiliated to Isfahan University of Medical Sciences through convenient sampling, after getting necessary permissions. The selected patients were divided into two groups by random allocation. Inclusion criteria were age >18 years, orientation to time and place, ability to read and speak in Persian and ability to attend the study (wearing earplugs and an eye mask), at least 48 h should have passed after patients’ surgery (if the patient had), no history of head injury (traumatic or pathologic), and lack of sleep chronic disorders and mental diseases.
Exclusion criteria were incidence of any injuries to eyes or ears, existence of allergy to earplugs or eye mask, and patients’ or their families’ interest to leave the research. A written informed consent was obtained from all the subjects before the study started. In group A, after educating patients concerning the correct way of wearing earplugs and eye mask at the first night of treatment (intervention), each patient received a pair of earplugs and an eye mask and was asked to sleep at 10 PM or earlier (if they liked) while wearing the earplugs and eye mask. At the second night (control night), the patients in this group were asked to sleep at 10 PM or earlier (if they liked) without wearing the earplugs and eye mask. In group B, at the first night of study (control night), the patients were asked to sleep at 10 PM or earlier (if they liked), with earplugs and an eye mask.
At the second night (treatment night), after educating the correct way of wearing earplugs and eye mask, each patient received a pair of earplugs and an eye mask and was asked to sleep at 10 PM or earlier (if they liked) while wearing the earplugs and eye mask. Like group A, if the patients were not able to wear earplugs and eye mask, the researcher or his colleagues helped the patients with that. Earplugs and eye mask were removed just in case of a necessity at treatment night, and if earplugs or eye mask were spontaneously removed, the subjects could wear them again themselves; but if the patient was asleep, he or she was not awaken to wear earplugs or eye mask. If the patients intentionally removed the earplugs or eye mask, the decision was up to them to wear those again or not. Measurement of patients’ perceived quality of sleep was conducted using Verran and Snyder-Halpern (VSH) standard tool to measure the quality of sleep, which has been translated into Persian and is a visual linear tool whose validity and reliability have been confirmed in various studies on investigation of sleep quality among the patients hospitalized in ICU.[29,30,31]
This tool defines mental quality of sleep through use of three components of sleep effectiveness, sleep disturbance, and supplemental sleep. Its most important feature is the capability of being completed quickly and comparison of patients’ quality of sleep with their natural sleep.[32] Persian version of this tool was checked and confirmed by 10 academic members of nursing, medical professors, and skillful nurses.
At the beginning, baseline information such as age, sex, level of narcotic medication consumption, mean hours of patients’ sleep before hospitalization, and facilitating tools used by the patients to fall asleep before hospitalization were recorded. Quality of sleep was assessed the day after treatment night and control night at 9 AM by completing the VSH sleep scales.
If the patients were asleep at that time of VSH sleep scales’ completion, it was postponed to the time they were awake.
In this study, to complete VSH questionnaire, the researcher asked the patients to choose a point indicating the quality of their past night sleep somewhere between 0 and 10, while showing a 10-cm line (visual analog scale), in response to each of his questions, so that he could mark it. Then, the distance of the marked point from the point of zero was measured in centimeters and recorded as the score of the related question. Scores of the questions in each component were summed up as the total score of that component. The data were analyzed by SPSS version 18, and P < 0.05 was considered significant. As the design of the present study was cross-over, in order to confirm the results of earplugs and eye mask use in the components of sleep effectiveness and sleep disturbance, carryover effect and periodic effect were determined and analyzed.
As in the measurement of sleep supplementation, actually the effect of quality of the first night sleep on this component was measured and this component was investigated at the end of the study through comparison of the data related to supplemental sleep in the second step of designing the tool, and did not follow the cross-over design. The present study has been derived from the master degree research project of the second author and has been already approved by vice chancellor for research of Isfahan University of Medical Sciences concerning ethical considerations.
RESULTS
A total of 50 subjects (27 women and 23 men) were investigated. Each group contained 25 subjects. At the end of the study, the data obtained from each group and the data of both steps were compared with each other, with regard to the effective demographic information.
Mean sleep effectiveness of the patients in group A in the treatment step and control step were 30.18 and 19.12, respectively.
Paired t-test showed a significant difference in group A patients in the two steps of treatment and control [Table 1].
Table 1.
Comparing the means scores of effectiveness and disturbance within the two groups in the control and treatment nights
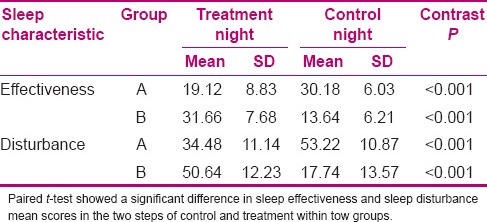
The obtained data related to group A patients’ sleep disturbance showed means of 53.22 in the treatment and 34.48 in the control steps.
Paired t-test showed a significant difference in group A patients in the two steps of treatment and control [Table 1].
Investigation of the data related to group B patients showed that the mean sleep effectiveness was 13.64 and 31.66 in the control and treatment steps, respectively. Paired t-test showed a significant difference in group B patients’ sleep effectiveness in the two steps of control and treatment [Table 1].
The obtained data related to group B patients’ sleep disturbance showed means of 17.74 and 50.64 in the control and treatment steps, respectively. Paired t-test showed a significant difference in group B patients’ sleep disturbance in the two steps of control and treatment [Table 1].
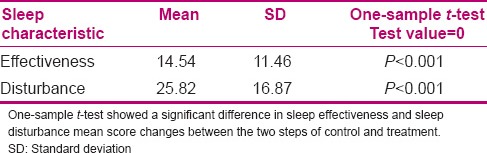
To investigate the main effect of earplugs and eye mask on the components of sleep effectiveness and sleep disturbance in patients of both groups in the two steps of treatment and control, mean score changes of sleep effectiveness and sleep disturbance were investigated by one-sample t-test and compared with score of zero. The results showed a significant difference in the components of sleep effectiveness and sleep disturbance in the two steps of treatment and control [Table 2].
Table 2.
Comparing the mean score changes of effectiveness and disturbance between the two steps of control and treatment
Although the main effect of treatment was very significant, carryover effect in the two groups showed P = 0.03 for sleep effectiveness and P = 0.02 for sleep disturbance, which revealed positivity of this effect in these groups and short period of washout time between the steps of treatment and control. It should be also noted that due to limitations in hospitalization time among conscious patients in ICU, increase in washout time was hardly possible. To investigate positive periodic effect, patients’ mean scores of effectiveness and sleep disturbance in the two groups were compared, and the results revealed the existence of periodic positive effect for the component of sleep disturbance (P < 0.001) and negative effect for sleep effectiveness. Covariance test showed a significant difference in sleep supplementation scores in the two groups in the second step of measurement (P < 0.001, df = 1, ER = 47, F = 22.1). It was such that in group A and group B, the means were 27.1 and 16, respectively. The results of the present study showed that usage of earplugs and an eye mask had a high effect on patients’ sleep supplementation, so that their level of sleep supplementation and daily nap decreased, possibly as a result of an increase in their night sleep. With regard to sleep effects of narcotics, patients’ consumption of narcotics in the two steps of treatment and control were compared. The obtained results showed the level of consumption of these medications was not significantly different (P = 0.282). Of course the mean level of their consumption was lower in the treatment step (2.32 mg) compared to the control step (3.12 mg), and some patients had not even received any narcotics in the treatment step.
DISCUSSION
Intergroup results of the present study showed a significant difference between the mean scores of sleep in the control and treatment groups, so that the score of patients’ nocturnal sleep quality enhanced at the night of wearing earplugs and eye mask, which is consistent with the results of Neyse et al.,[33] Fung,[17] Richardson et al.,[26] Koo and Koh,[34] and Xie et al.[35] In a study conducted by Pongam (2005) in American Sleep Laboratory on 40 healthy individuals to investigate subjects’ sleep quality by polysomnography, wearing earplugs was observed to have improved the subjects’ sleep by 67.6%.[36]
Neyse et al. (2011), in a study in Baghiatollah University of Medical Sciences on the patients hospitalized in ICU, showed that wearing earplugs increased their quality of sleep.[33] Scotto et al., in a study investigating the effect of earplugs on mental experience of sleep among patients hospitalized in cardiac care unit (CCU), reported that sleep satisfaction score was more in the treatment group compared to the control group.[37]
With regard to the cross-over design of the present study, the intergroup effect of earplugs and eye mask usage on sleep effectiveness and sleep disturbance in the two steps of treatment and control was investigated and showed a significant difference. As a result of positivity of carryover effect in the investigation of both components and positivity of periodic effect in the component of sleep disturbance, positive effect of these tools (earplugs and eye mask) on sleep effectiveness and sleep disturbance was not confirmed. These results are in line with those of Martin (2008) who showed usage of earplugs and eye mask had no significant effect on sleep effectiveness and sleep disturbance.[8] Meanwhile, the research conducted using physiologic sleep measurement tools reported different results and recommended the usage of these tools as a strategy to improve patients’ sleep quality. Fung (2010), in a study on healthy individuals hospitalized in an ICU simulated environment through polysomnography, showed that by wearing earplugs and eye mask, not only the quality of sleep increased but also the level of REM sleep and nocturnal melatonin level increased.[17] Wallace (1999) showed that wearing earplugs increased REM sleep.[27]
Although most of the studies have investigated the effect of earplugs on sleep quality and a few have investigated the effect of eye mask on sleep quality, possibly one of the reasons for the inconsistency between this result and those of other studies is the sleep scores of various patients in these two components. In fact, the psychological effect of wearing these tools was so high that patients magnified their sleep scores and reported them. On the other hand, positivity of carryover effect in the present study indicates short washout time between the two steps of treatment and control. In fact, as sleep measurement was conducted by VSH self-report tool in the present study, patients’ consciousness was essential to measure their sleep quality, but conscious patients were often transferred from ICU and this issue made it very difficult to increase the washout time.
As the effect of earplugs and an eye mask on sleep effectiveness and sleep disturbance was not confirmed in the present study, the obtained results concerning sleep supplementation component showed that wearing these tools, in addition to promoting nocturnal sleep quality, reduced day time sleep supplementation, which is not consistent with the study of Martin which reported wearing earplugs had no significant effect on sleep supplementation.[8] Despite the sleeping effect of narcotics, the obtained results showed no significant difference in narcotic consumption levels in the two steps of treatment and control, and on the contrary, their consumption was less in the treatment step which is consistent with the results obtained by Neyse et al.[33] Their results showed no significant difference in sleep medication consumption after wearing earplugs and eye mask.
CONCLUSIONS
With regard to the results of the present study, despite the reported positive effects of earplugs and eye mask on sleep quality of the patients hospitalized in ICU, especially their positive effect on sleep supplementation and reduction of narcotics’ consumption, conducting another study with a larger sample size and a longer washout time seems essential. With regard to the importance of sleep among hospitalized patients in ICU, it is also suggested to use physiologic sleep investigating tools like polysomnography parallel to sleep quality subjective measurement tool, in order to be able to judge more precisely about the efficiency of wearing earplugs and eye mask.
ACKNOWLEDGMENT
We thank the Al-zahra University Hospital for their help.
Footnotes
Source of Support: Isfahan University of Medical Sciences
Conflict of Interest: None declared.
REFERENCES
- 1.Honkus VL. Sleep deprivation in critical care units. Crit Care Nurs Q. 2003;26:179–89. doi: 10.1097/00002727-200307000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Walder B, Haase U, Rundshagen I. Sleep disturbances in critically ill patients. Anaesthesist. 2007;56:7–17. doi: 10.1007/s00101-006-1086-4. [DOI] [PubMed] [Google Scholar]
- 3.Kozier B, Erb G, Berman A, Snyder SJ. 8th ed. Philadelphia: Sunders; 2008. Fundamental concepts and skills for nursing; p. 1162. [Google Scholar]
- 4.Kaplow R, Hardin SR. Massachusets: Jonesand Bartlett; 2008. Critical care nursing; pp. 53–65. [Google Scholar]
- 5.Stanchina ML, Abu-Hijleh M, Chaudhry BK, Carlisle CC, Millman RP. The influence of white noise on sleep in subjects exposed to ICU noise. Sleep Med. 2005;6:423–8. doi: 10.1016/j.sleep.2004.12.004. [DOI] [PubMed] [Google Scholar]
- 6.Murphy K, Delanty N. Sleep deprivation: A clinical perspective. Sleep Biol Rhythms. 2007;5:2–14. [Google Scholar]
- 7.Moeini M, Khadibi M, Bekhradi R, Mahmoudian SA, Nazari F. Effect of aromatherapy on the quality of sleep in ischemic heart disease patients hospitalized in intensive care units of heart hospitals of the Isfahan University of Medical Sciences. Iran J Nurs Midwifery Res. 2010;15:234–9. [PMC free article] [PubMed] [Google Scholar]
- 8.Martin KA. The effect of earplugs on perceived sleep quality of acute care patients. Montana state university: A thesis submitted in partial fulfillment of the requirements for the degree of Master of Nursing. [last accessed on 2008 Apr 20]. Available from: http://www.etd.lib.montana.edu .
- 9.Beecroft JM, Ward M, Younes M, Crombach S, Smith O, Hanly PJ. Sleep monitoring in the intensive care unit: Comparison of nurse assessment, actigraphy and polysomnography. Intensive Care Med. 2008;34:2076–83. doi: 10.1007/s00134-008-1180-y. [DOI] [PubMed] [Google Scholar]
- 10.Figueroa-Ramos MI, Arroyo-Novoa CM, Lee KA, Padilla G, Puntillo KA. Sleep and delirium in ICU patients. Intensive Care Med. 2009;35:781–95. doi: 10.1007/s00134-009-1397-4. [DOI] [PubMed] [Google Scholar]
- 11.Patel M, Chipman J, Carlin BW, Shade D. Sleep in the intensive care unite setting. Crit Care Nurs Q. 2008;31:309–18. doi: 10.1097/01.CNQ.0000336816.89300.41. [DOI] [PubMed] [Google Scholar]
- 12.Friese RS, Bruns B, Sinton CM. Sleep Deprivation after septic insult increases mortality Independent of Age. J Trauma. 2009;66:50–4. doi: 10.1097/TA.0b013e318190c3a1. [DOI] [PubMed] [Google Scholar]
- 13.Zolfaghari M, Farokhnezhad AP, Asadi NA, Ajri KM. Modification of Environmental Factors on Quality of Sleep among Patients Admitted to CCU. Hayat. 2012;18:61–8. [Google Scholar]
- 14.Weinhouse GL, Schwab RJ. Sleep in the Critically ill Patients. Sleep. 2006;29:707–16. doi: 10.1093/sleep/29.5.707. [DOI] [PubMed] [Google Scholar]
- 15.Nelson JE, Meier DE, Oei EJ, Nierman DM, Senzel RS, Manfredi PL, et al. Self-reported symptom experience of critically ill cancer patients receiving intensive care. Crit Care Med. 2001;29:277–82. doi: 10.1097/00003246-200102000-00010. [DOI] [PubMed] [Google Scholar]
- 16.Bijwadia JS, Ejaz MS. Sleep and critical care. Curr Opin Crit Care. 2009;15:25–9. doi: 10.1097/MCC.0b013e3283220dc7. [DOI] [PubMed] [Google Scholar]
- 17.Hu RF, Jiang XY, Zeng YM, Chen XY, Zhang YH. Effects of earplugs and eye masks on nocturnal sleep, melatonin and cortisol in a simulated intensive care unit environment. [Last accessed on 2012 Jan 10];Crit Care. 2010 14:R66. doi: 10.1186/cc8965. Available from: http://www.ccforum.com/content/14/2/R66 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hardin KA. Sleep in the ICU: Potential mechanisms and clinical implications. Chest. 2009;136:284–94. doi: 10.1378/chest.08-1546. [DOI] [PubMed] [Google Scholar]
- 19.BaHammam A. Sleep in acute care units. Sleep Breath. 2006;10:6–15. doi: 10.1007/s11325-005-0044-8. [DOI] [PubMed] [Google Scholar]
- 20.Shilo L, Dagan Y, Smorjik Y, Weinberg U, Dolev S, Komptel B, et al. Effect of melatonin on sleep quality of COPD intensive care patients: A pilot study. Chronobiol Int. 2000;17:71–6. doi: 10.1081/cbi-100101033. [DOI] [PubMed] [Google Scholar]
- 21.Hamilton D, Sheply M. Amsterdam, Netherlands: Elsevier; 2010. Design for critical care; p. 182. [Google Scholar]
- 22.Drouot X, Cabello B, Ortho MP, Brochard L. Sleep in the intensive care unit. Sleep Med Rev. 2008;12:391–403. doi: 10.1016/j.smrv.2007.11.004. [DOI] [PubMed] [Google Scholar]
- 23.Sole M, Klein D, Moseley M. 5th ed. Amsterdam, Netherlands: Elsevier; 2009. Critical care nursing; p. 11. [Google Scholar]
- 24.Khalil M. Sleep assessment in critically ill patients. The Journal of the Intensive Care Society. 2008;9:42–5. [Google Scholar]
- 25.Morton PG, Fontaine DK. 9th ed. Philadelphia: Lippincott Williams and Wilkins; 2009. Critical care nursing; p. 23. [Google Scholar]
- 26.Richardson A, Allsop M, Coghill E, Turnock C. Earplugs and eye masks: Do they improve critical care patients’ sleep. Nurs Crit Care. 2007;12:278–86. doi: 10.1111/j.1478-5153.2007.00243.x. [DOI] [PubMed] [Google Scholar]
- 27.Wallace CJ, Robins J, Alvord LS, Walker JM. The effect of earplugs on sleep measures during exposure to simulated intensive care unit noise. Am J Crit Care. 1999;8:210–9. [PubMed] [Google Scholar]
- 28.Bourne RS, Mills GH, Minelli C. Melatonin therapy to improve nocturnal sleep in critically ill patients: Encouraging results from a small randomised controlled trial. [Last accessed on 2012 Jan 10];Critical Care. 2008 12:R52. doi: 10.1186/cc6871. Available from: http://ccforum.com/content/12/2/R5 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Snyder-Halpern R, Verran JA. Instrumentation to describe subjective sleep characteristics in healthy subjects. Res Nurs Health. 1987;10:155–63. doi: 10.1002/nur.4770100307. [DOI] [PubMed] [Google Scholar]
- 30.Topf M, Thompson S. Interactive relationships between hospital patients’noise-induced stress and other stress with sleep. Heart Lung. 2001;30:237–43. doi: 10.1067/mhl.2001.116592. [DOI] [PubMed] [Google Scholar]
- 31.Kroon K, West S. Appears to have slept well: Assessing sleep in an acute care setting. Contemp Nurse. 2000;9:284–94. doi: 10.5172/conu.2000.9.3-4.284. [DOI] [PubMed] [Google Scholar]
- 32.Bourne RS, Minelli C, Mills GH, Kandler R. Clinical review: Sleep measurement in critical care patient: Research and clinical implications. Crit Care. 2007;11:226. doi: 10.1186/cc5966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Neyse F, Daneshmandi M, Sadeghi M, Ebadi A. The effect of earplugs on sleep quality in patients with acute coronary syndrome. Iran J Crit Care Nurs. 2011;4:127–34. [Google Scholar]
- 34.Koo YJ, Koh HJ. Effects of eye protective device and ear protective device application on sleep disorder with coronary disease patients in CCU. Department of Nursing, Andong Science College. Taehan Kanho Hakhoe Chi. 2008;38:582–92. doi: 10.4040/jkan.2008.38.4.582. [DOI] [PubMed] [Google Scholar]
- 35.Xie H, Kang J, Mills GH. Clinical review: The impact of noise on patients’ sleep and the effectiveness of noise reduction strategies inintensive care units. Crit Care. 2009;13:208. doi: 10.1186/cc7154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pongam S. The effect of music on sleep efficiency amonge patient during admission in the coronary care unite: mahidol university. 2005. [Last accessed on 2012 Dec 17]. Available from: http://li.mahidol.ac.th/thesis/2548/./4536555.pdf .
- 37.Scotto CJ, McClusky C, Spillan S, Kimmel J. Earplugs improve patients’ subjective experience of sleep in critical care. Nurs Crit Care. 2009;14:180–4. doi: 10.1111/j.1478-5153.2009.00344.x. [DOI] [PubMed] [Google Scholar]


