Abstract
Aims
This study compares, from a prospective, observational, non-randomized registry, the post-implant hospitalization rates and associated healthcare resource utilization of cardiac resynchronization therapy-defibrillator (CRT-D) patients with quadripolar (QUAD) vs. bipolar (BIP) left ventricular (LV) leads.
Methods and results
Between January 2009 and December 2012, 193 consecutive patients receiving de novo CRT-D implants with either a QUAD (n = 116) or a BIP (n = 77) LV lead were enrolled at implant and followed until July 2013 at a single-centre, university hospital. Post-implant hospitalizations related to heart failure (HF) or LV lead surgical revision and associated payer costs were identified using ICD-9-CM diagnosis and procedure codes. Italian national reimbursement rates were determined. Propensity scores were estimated using a logistic regression model based upon 11 pre-implant baseline characteristics and were used to derive a 1 : 1 matched cohort of QUAD (n = 77) and BIP (n = 77) patients. Hospitalization rates for the two groups were compared using negative binomial regression and associated payer costs were compared using non-parametric bootstrapping (×10 000) and one-sided hypothesis test. Hospitalization rates of the QUAD group [0.15/ patient (pt)-year] were lower than those of the BIP group (0.32/ pt-year); the incidence rate ratio was 0.46, P = 0.04. The hospitalization costs for the QUAD group (434 ± 128 €/pt-year) were lower than those for the BIP group (1136 ± 362 €/pt-year). The average difference was 718 €/pt-year, P = 0.016.
Conclusions
In this comparative effectiveness assessment of well-matched groups of CRT-D patients with quadripolar and bipolar LV leads, QUAD patients experienced a lower rate of hospitalizations for HF and LV lead surgical revision, and a lower cost burden. This has important implications for LV pacing lead choice.
Keywords: Cardiac resynchronization therapy, Cost-effectiveness, Health economics, Hospitalizations, Left ventricular lead, Quadripolar lead
What's new?
This is the first comparative effectiveness study to evaluate the post-implant hospitalization rates and associated healthcare resource utilization between cardiac resynchronization therapy (CRT) delivered with quadripolar vs. bipolar LV leads.
Patients implanted with a quadripolar LV lead experienced a lower rate of hospitalizations for heart failure and LV lead surgical revision, and a lower cost burden.
The results provide strong evidence that the use of quadripolar leads has a significant positive impact on the clinical outcomes and healthcare resource utilization of CRT patients.
Introduction
Cardiac resynchronization therapy (CRT) is a well-established treatment for heart failure (HF) in patients with severely impaired left ventricular (LV) systolic function and evidence of ventricular dyssynchrony.1,2 Heart failure management is expensive and is associated with hospitalizations and re-hospitalizations.3,4 Cardiac resynchronization therapy has been shown to improve clinical outcomes and has proved to be cost-effective as an adjunct to conventional medical management.3,5–11
Cardiac resynchronization therapy is enabled by LV stimulation via a lead either on the LV epicardial surface, or more commonly, within a tributary of the coronary sinus. Traditionally, CRT has been enabled with bipolar electrode leads. However, unpredictable patient coronary sinus anatomy, phrenic nerve stimulation (PNS), and high LV pacing thresholds can affect and in some cases considerably limit, the long-term success of CRT.12 To address these common problems, quadripolar electrode CRT systems have been designed with the purpose of allowing more choices in the LV lead placement location and programming capability of pacing vectors.
Multiple studies have compared the Quadra CRT system enabled with the Quartet™ LV lead (St Jude Medical, Sylmar) to CRT systems employing bipolar LV leads, and have shown these quadripolar leads to have better implant experience, incur lower post implant complications, and improved haemodynamics.13–17 With the current focus on improved quality and efficiency of healthcare delivery, there is a need for information on the comparative effectiveness of viable alternatives such as CRT quadripolar and bipolar LV leads.
The purpose of this study was to compare for the first time, the post-implant hospitalization rates and associated healthcare resource utilization between CRT delivered with quadripolar vs. bipolar LV leads. We hypothesized that since Quadra CRT systems are associated with lower complications, lower deactivations and replacements, improved haemodynamics, this would manifest in reduced hospitalizations related to HF and LV lead surgical revision than CRT systems enabled with bipolar LV leads. Our primary endpoint was to compare the hospitalization rate for this combined outcome of LV lead procedures and HF hospitalizations. Our secondary endpoint was to compare the associated healthcare resource utilization.
Methods
Study design
This was a prospective, single-centre, observational, non-randomized registry of consecutive patients implanted with cardiac resynchronization therapy-defibrillator (CRT-D) devices and transvenous LV leads at a University-affiliated, tertiary care centre (Policlinico Tor Vergata). The study protocol was approved by the local ethics committee and adhered to the principles outlined in the Declaration of Helsinki. Consecutive patients scheduled for implantation of a CRT-D system between January 2009 and December 2012 were approached for participation at their time of implant. CRT-D systems were implanted per current implant guidelines.18 Left ventricular leads were targeted to the most optimal anatomic branch of the coronary sinus, preferring the lateral or posterolateral regions. Final LV lead position and pacing vector was determined at the discretion of the operator based upon pacing parameters, absence of PNS, and anatomic position. Implantations were performed with patients under local anaesthesia by two approximately 10-year CRT-D implantation experienced electrophysiologists (GBF, LS). The decision to implant a Quartet lead over any other competing lead was not based on each patient's clinical characteristics but on the system available on the day of implantation. In particular, patients were hospitalized according to the first available date for CRT-D implantation, independently on the CRT-D manufacturer previously scheduled for that day. Wherein only bipolar leads were available at the beginning of the study, quadripolar leads were available since January 2010. If that day CRT-D were scheduled with St. Jude Medical devices, patients ended up with a quadripolar lead.
Pre-implant baseline characteristics of all participating patients including age, gender, medical history, and HF status were recorded. All hospital admissions incurred by these patients between their implant date and 31 July 2013 were identified from the billing records. For each hospitalization, the admission date, discharge date, ICD-9-CM (International Classification of Diseases, Ninth Revision, Clinical Modification) diagnoses, and procedure codes were recorded.
The objectives of the study were to compare, in these CRT patients, the hospitalization rates and associated healthcare resource utilization between the two LV lead groups, quadripolar and bipolar. The primary endpoint of this analysis was prospectively defined as the comparison of the combined hospitalization rate for HF hospitalization or LV lead-related surgical revision in the two LV lead groups. The secondary endpoint was the comparison of the associated healthcare resource utilization for these hospitalizations between the two LV lead groups.
Assessment of hospitalization type and cost
Based on the specific ICD-9-CM diagnoses and procedure codes, each hospitalization was objectively categorized as: HF, LV lead-related surgical revision or other. The specific codes used, and their description, are given in detail in the Supplementary data online. Every lead-related hospitalization was checked against medical records to confirm that the chamber of lead-related procedure was indeed the left ventricle.
A diagnosis-related group (DRG) code (version v24, 1 October 2006) for each hospitalization was determined from all diagnoses and procedure codes using Grouper software ‘Applicazioni di codifica 3 M’ (version 6.4.1, April 2011, 3 M Health Information System Italy). Finally, the estimated reimbursement for each hospitalization was obtained for the DRG according to the 2012 Italian national reimbursement rates (National Ministerial Tariffs Ministerial Decree of 18 October 2012).
Study cohort for analysis
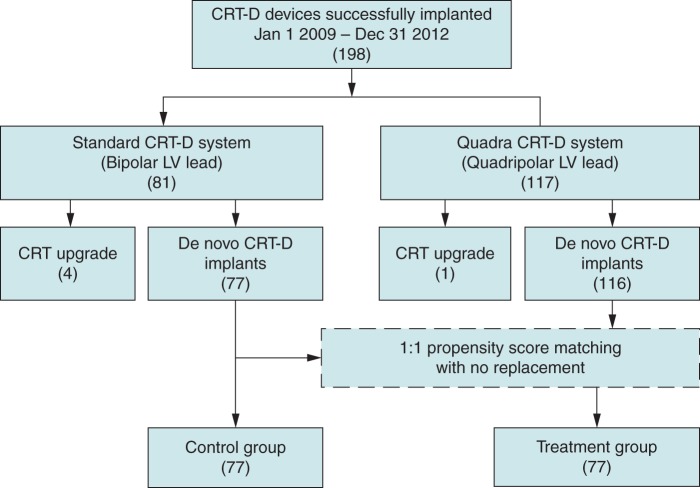
For this analysis, only patients implanted with de novo LV leads were included, whether the implant was a first device implantation or the LV lead was placed as part of an upgrade to CRT-D in patients with a pre-existing permanent pacemaker or a defibrillator. Patients were divided into two groups based on the implanted system: Quadra CRT-D group and Bipolar CRT-D group. The Quadra CRT-D group had a Quartet™ LV lead and a corresponding CRT-D (St. Jude Medical), and the Bipolar CRT-D group had a bipolar LV lead from any manufacturer and a CRT-D device from any manufacturer. Figure 1 shows the distribution of patients.
Figure 1.
Study cohort.
Since this was an observational registry, we sought to match the baseline characteristics of the Quadra and Bipolar CRT-D groups. For this purpose, propensity scores were estimated for each patient using multivariate logistic regression. The propensity score for each patient is the conditional probability of having a specific lead type given the individual's baseline characteristics. Eleven pre-implant baseline characteristics were utilized: age, gender, ejection fraction, NYHA class, coronary artery disease, atrial fibrillation, hypertension, diabetes, previous cardiac surgery, valvular disease, and primary prevention. The multivariate logistic regression model was evaluated for goodness of fit based on the Hosmer and Lemeshow test.19
Propensity scores were used to match each Bipolar patient to the Quadra patient with the most similar baseline characteristics using a greedy match. Since there were more Quadra patients than Bipolar patients and to keep the groups as large as possible, no Bipolar patients were excluded as part of the matching scheme; only the poorest-matching Quadra patients were excluded from the final comparison groups. The standardized difference was calculated for each covariate. The sum of the absolute value of the standardized difference for all of the baseline characteristics before and after the match was used to assess the improvement in covariate balance achieved due to the matching procedure. The categorical covariates were summarized as percentages and compared using χ2 analysis or Fisher's exact test. Continuous data are reported as mean ± standard deviation and were compared with the Student's t test (if normally distributed) or the Wilcoxon-rank sum or signed rank test (if non-normally distributed). Statistical significance was deemed present if P < 0.05. The analysis was conducted in Revolution R version 6.0 (Revolution Analytics, Mountain View).
The matching based on propensity scores provided the treatment and control groups for analysis. The control group included all Bipolar CRT-D implants with de novo bipolar LV lead implants. The treatment group included a matched set of Quadra CRT-D patients. All analyses of the study endpoints were conducted on these two groups.
Statistical analysis
The primary endpoint of comparing the combined hospitalization rate for HF or LV lead surgical revision was evaluated by modelling the hospitalization data using a negative binomial regression adjusted for varying lengths of follow-up for each patient. The likelihood ratio test that compared the fit between the negative binomial regression and the Poisson regression (the null model) along with the estimated dispersion parameter and its associated 95% confidence interval using the negative binomial model was provided as evidence of model fit for the negative binomial model. SAS software version 9.4 was used to perform the statistical analyses (SAS Institute, Inc.).
The secondary endpoint of comparing the healthcare resource utilization for the HF and LV lead surgical revision was evaluated using the non-parametric bootstrap method. This is a data-based simulation method for assessing statistical precision,20,21 and allows a comparison of arithmetic means without making assumptions about the cost distribution. Each hospitalization was associated with a national reimbursement rate based on the DRG code and the length of stay. For this healthcare resource utilization analysis, two metrics were determined for each patient: Follow-up time (TBi or TQ) and total cost for hospitalizations that occurred during the follow-up time (CBi or CQ). Bootstrapping is based on how values of the cost difference would vary if the sampling process could be repeated many times. This involves re-sampling from the data set with replacement while preserving the original structure of the data (i.e. same size, same number in each treatment group). Ten thousand replicated data sets were generated using the treatment and control groups, and for each population, the cost difference COSTBIP–COSTQUAD was determined.
The cost of the hospitalizations for the patients in the Quadra and Bipolar group was normalized to their respective aggregate follow-up time. A one-sided hypothesis test was evaluated with the null hypothesis that COSTQUAD is not less than COSTBIP. The probability that the estimated cost difference is positive was estimated from the bootstrap estimates.
In addition to the primary endpoint of comparing the hospitalization rates for HF or LV lead surgical revision, we also determined the hospitalization rates for (i) HF hospitalizations, (ii) hospitalizations not related to HF and LV lead surgical revision, and (iii) all cause hospitalizations; this was determined using negative binomial regression. In addition to the secondary endpoint comparing the healthcare resource utilization for HF or LV lead surgical revision, we also determined the healthcare resource utilization for solely HF hospitalizations; this was done using the non-parametric bootstrap method. Additional hospitalization characteristics were also compared across the two LV lead groups: length of stay per hospitalization, compared using a Wilcoxon rank sum test; the days in hospital per patient, compared using non-parametric bootstrap. Incidence rate of mortality was reported as a ratio of number of deaths over the follow-up time.22
Results
Patient demographics
Between January 2009 and December 2012, 198 patients were successfully implanted with CRT-D systems. A total of 117 patients were implanted with the Quartet™ 1458Q model LV lead and corresponding Quadra CRT-D device (Promote™ Q, Unify Quadra™ from St. Jude Medical), and 81 patients were implanted with bipolar LV leads from four different manufacturers and corresponding CRT-D pulse generators. Of these implants, 99% of the Quadra and 95% of the Bipolar patients had de novo LV leads, respectively.
Using the 116 de novo Quadra patients and 77 de novo Bipolar CRT-D patients, the propensity scores were generated using multivariate logistic regression. All covariates were available for each patient; the only exception was the unavailable ejection fraction for one patient in the quadripolar group. This single variable was imputed as an average of the entire population. The model showed no evidence of lack of fit based on the Hosmer and Lemeshow test (χ2 = 5.2, P = 0.73). The one-to-one match without replacement yielded 77 matched treatment group patients for the 77 control group patients. The groups were similar with respect to baseline characteristics (Table 1). The sum of the absolute value of the standardized difference before the match was 111.4 when compared with 73.1 after the match, a reduction that indicates improvement in covariate balance due to the matching procedure. The propensity scores for the matched population were 0.58 ± 0.09 vs. 0.58 ± 0.10 (P = 0.60) for the treatment and control groups, respectively.
Table 1.
Baseline characteristics of the control and treatment groups
| Treatment group (Quadra) (77) | Control group (Bipolar) (77) | P value | |
|---|---|---|---|
| Demographics | |||
| Age (years) | 69.4 ± 9.8 | 69.6 ± 9.4 | 0.86 |
| Gender (male) | 61 (79.2%) | 60 (77.9%) | 0.95 |
| LVEF (%) | 25.6 ± 6.1 | 25.6 ± 6.9 | 0.93 |
| NYHA (class) | 2.7 ± 0.6 | 2.7 ± 0.6 | 0.69 |
| Follow-up (years) | 1.65 ± 0.8 | 1.84 ± 1.2 | 0.005 |
| Comorbidities | |||
| CAD | 40 (51.9%) | 43 (55.8%) | 0.79 |
| Hypertension | 68 (88.3%) | 68 (88.3%) | 1.00 |
| History of AF | 15 (19.5%) | 16 (20.8%) | 0.87 |
| Diabetes | 24 (31.2%) | 29 (37.7%) | 0.55 |
| Primary prevention | 72 (93.5%) | 68 (88.3%) | 0.80 |
| Previous cardiac surgery | 13 (16.9%) | 14 (18.2%) | 0.85 |
| Valvular disease | 40 (51.9%) | 36 (46.8%) | 0.71 |
| Medications | |||
| Nitrates | 11 (14.3%) | 11 (14.3%) | 1.00 |
| Diuretics | 72 (93.5%) | 72 (93.5%) | 1.00 |
| β-Blockers | 62 (80.5%) | 63 (81.8%) | 0.94 |
| ARBs/ACE | 65 (84.4%) | 67 (87.0%) | 0.89 |
| Aldosterone antagonists | 47 (61.0%) | 38 (49.4%) | 0.43 |
ACE, angiotensin-converting enzyme; AF, atrial fibrillation; ARBs, angiotensin II receptors blockers; CAD, coronary artery disease; EF, ejection fraction; LV, left ventricular.
Post-implant hospitalizations
The two groups were followed for an average of 1.75 ± 1.04 years. During this follow-up period, 13 treatment group patients had 17 hospitalization stays for HF or LV lead surgical revision, and 18 control patients had 39 such hospitalization stays. The event rates were significantly lower for the treatment group patients (0.15 vs. 0.32 events/patient-year) with an incidence rate ratio of 0.46, P = 0.04. The negative binomial regression provided a statistically significantly better fit when compared with the same model using Poisson regression (likelihood ratio test, P < 0.0001). The dispersion parameter estimated by the negative binomial regression was 3.7, with a 95% confidence interval (1.9, 7.5), providing additional evidence that the negative binomial regression was the appropriate model.
Forty percent of the treatment group patients had 61 all-cause hospitalizations, whereas 47% of the control patients had 93 hospitalizations for any cause. The event rates were not statistically different for the treatment group (0.62 vs. 0.88 events/patient-year) with an incidence rate ratio of 0.70, P = 0.13. Hospitalizations not related to HF and LV lead surgical revision were not statistically significantly different between the treatment and control groups (0.43 vs. 0.49 events/patient-year) with an incidence rate ratio of 0.89, P = 0.14. This indicates that the majority of difference between the hospitalization rates between the two groups may be attributable to HF hospitalizations. Among all the hospitalizations, HF was the most frequent cause of hospitalization in both groups, with 26% of the treatment group hospitalizations being attributable to HF, vs. 39% in the control group. The mortality rates for the treatment and control groups were 0.087 vs. 0.090 for the entire follow-up period with an incidence rate ratio of 0.95 (0.38, 2.29), indicating no significant difference in mortality rate between the two groups. Hospitalization rates and hospitalization characteristics are reported in detail in Table 2 and in the Supplementary data online.
Table 2.
Hospitalization rates for each group and comparison of event rates
| Events per patient year (95% CI) |
Incidence rate ratio (95% upper confidence limit) | P value (one-sided) | ||
|---|---|---|---|---|
| Treatment group (Quadra) | Control group (Bipolar) | |||
| Primary endpoint | ||||
| HF hospitalizations and LV lead surgical revision | 0.15 (0.08, 0.26) | 0.32 (0.20, 0.53) | 0.46 (0.97) | 0.04 |
| Additional hospitalization rates | ||||
| HF hospitalizations | 0.14 (0.08, 0.24) | 0.28 (0.17, 0.45) | 0.49 (1.04) | 0.06 |
| Other hospitalizations not related to HF and LV lead surgical revision | 0.43 (0.29, 0.64) | 0.49 (0.33, 0.72) | 0.89 (1.53) | 0.14 |
| All cause hospitalization | 0.62 (0.42, 0.90) | 0.88 (0.61, 1.26) | 0.70 (1.19) | 0.13 |
All event rates derived using negative binomial regression.
LV, left ventricular.
The treatment group patients had a cost burden of 434 ± 128 €/patient (pt)-year, while the control group had a cost burden of 1136 ± 362 €/pt-year, representing a 62% decrease of €718/pt-year in the treatment group (P = 0.016; Table 3). Figure 2 illustrates the cumulative probability function showing the likelihood of cost difference between the two groups considering hospitalizations due to HF and LV lead surgical revision. For this outcome, there was a 98.4% probability that Quadra therapy exhibited reduced costs compared with bipolar LV lead CRT therapy. The length of stay per hospitalization for HF and LV lead surgical revision were statistically similar between the treatment (5.9 ± 4.8 days) and control groups (4.9 ± 4.6), P = 0.46. On average, the treatment group spent 0.7 ± 0.3 days per patient year in the hospital for HF or LV lead surgical revision, whereas the control group spent 1.2 ± 0.4 days per patient year in the hospital per patient (P = 0.13).
Table 3.
Hospitalization costs for the two groups
| Treatment group (Quadra) | Control group (Bipolar) | Cost difference €/pt-year | P value | |
|---|---|---|---|---|
| Secondary endpoint | ||||
| HF hospitalizations and LV lead surgical revision cost (€/pt-year)a | 434 ± 128 | 1136 ± 362 | €718 | P = 0.016 |
| HF hospitalizations only | ||||
| HF hospitalizations cost (€/pt-year)a | 434 ± 128b | 1059 ± 356 | €650 | P = 0.03 |
aNon-parametric bootstrap model based.
bIf a hospitalization included both HF diagnosis and LV procedure, the total cost for the hospitalization is used.
Figure 2.
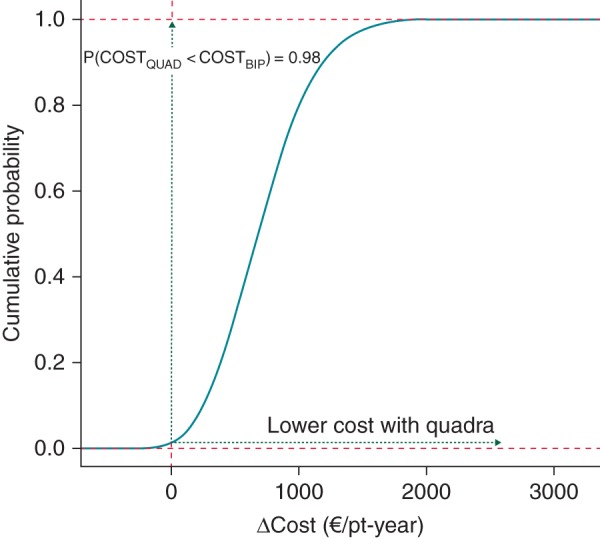
Cumulative probability function showing the likelihood of cost difference (ΔC) between treatment and control groups. ΔC = Cost difference. P(CostQUAD < CostBIP): Probability of cost for Quadra being lower than Bipolar.
Discussion
To our knowledge, this is the first published evaluation of the hospitalization rates and costs of CRT-D with quadripolar vs. bipolar LV leads. The primary finding of this single-centre, prospective study is that patients implanted with quadripolar LV leads exhibited a 54% reduced rate of hospitalization specific to HF and LV lead surgical revision, and reduced total healthcare resource utilization by 62%. Quadra patients exhibited 0.17 fewer hospitalizations/pt-year than patients with bipolar leads, and this was accompanied with a statistically significant cost saving of € 718/pt-year. The hospitalization rate specific to HF and LV procedures was significantly reduced in Quadra patients, providing evidence regarding the effectiveness of this therapy.
Our analysis has several strengths. Both groups were provided optimal medical therapy, and programming of the CRT-D devices was provided according to the standard of care and the capabilities of the devices. The analysis was based on consecutive implanted patients and uses established methods for cost-effectiveness analysis.20 Our study represents the longest reported follow-up experience with Quadra implants, and the resource utilization was collected over a mean of a 1.75-year period from CRT-D implantation. We utilized an objective method for identifying the hospitalization type, based upon billing records. We utilized propensity scores to match the two groups of patients with the most similar baseline characteristics using a greedy match, allowing for comparison of the primary and secondary endpoints in a matched population.
Economic analyses commonly use cost data from randomized controlled trials to inform healthcare policy decisions. However, CRT-D patients in clinical trials may not be representative of those in everyday practice since only selected patients participate in those trials. These limitations raise questions about the generalizability of the published literature when using cost data from trials to inform health care policy decisions. The present analysis represents a prospective, real world clinical experience with a large number of patients outside the realm of randomized controlled trials. However, whether this single-centre experience might be universally applicable to other settings remains to be determined.
It is notable that the hospitalization rate specific to HF and LV procedures was significantly reduced with quadripolar leads, providing hard evidence regarding the effectiveness of this therapy. An LV lead positioned at an effective location is a prerequisite for effective CRT. Use of quadripolar leads facilitates targeting pacing at more proximal regions of coronary venous branches, to consistently and safely target basal and mid ventricle pacing sites while maintaining a more distal and stable lead position. Previous studies suggest that placement of the LV lead along an area corresponding to the greatest electrical or mechanical delay improves CRT outcomes.23–25 More pacing configurations over a wider LV area with the use of the four electrodes along a quadripolar lead is helpful to identify the best pacing configuration while minimizing the likelihood of developing PNS. It is reasonable to consider that quadripolar leads' programming flexibility might translate into more favourable clinical outcomes.
Of note, this study utilized a specific quadripolar LV lead and pulse generator from a single manufacturer and may not reflect other lead designs that were not tested or evaluated in this analysis. While additional multipolar LV leads are currently under investigation, only the Quartet™ lead had CE Mark approval at the time of this study.
Limitations
Our study also has potential limitations. (i) Considering that both patients' age and HF severity increase and that, besides, the incidence of LV-related complications may decrease during follow-up, it is not clear whether or not the relative benefit of one lead vs. the others remains constant over the long term. (ii) Although the decision of using a Quartet lead over any other lead was mainly based on lead availability on the day of implantation, the choice of system was not randomized. However, while this issue represents a potential bias, the patient characteristics in both groups were well balanced and not different. (iii) Our resource utilization comparison does not include emergency department visits since in the Italian medical system, the costs incurred by the emergency department are included in hospital administration operations, and not billed for separately. In addition, our cost analysis has been done from a payer perspective, and not a societal perspective, hence does not take into consideration comparison of health resources such as productivity loss and caretaker burden. (iv) Finally, the experience observed with our patients may not be applicable to other universal settings given that our results are derived from a single centre in Italy. Therefore, additional large-scale randomized studies with longer surveillance data will be needed to validate findings reported in this study regarding this therapy's effectiveness and costs. Despite these limitations, our analysis is robust and the results represent to date the only and the best estimate of comparative-effectiveness of CRT-D patients implanted with quadripolar vs. bipolar LV leads.
Conclusion
This prospective study is the first comparative effectiveness study to evaluate hospitalization rates and costs of CRT-D with quadripolar vs. bipolar LV leads and provides strong evidence that the use of a quadripolar lead may have a significant positive impact on clinical outcomes and healthcare resource utilization.
Supplementary data
Conflicts of interest: G.B.F., L.S., and A.N. received lecture fees from St Jude Medical. R Bharmi, N. Dalal, and A Pollastrelli are employees of St. Jude Medical. The remaining authors have no disclosures.
Funding
Funding to pay the Open Access publication charges for this article was provided by St. Jude Medical Italia.
Acknowledgements
The authors thank Cecilia Rubaudo and Enrico Romano for their assistance in the preparation of this manuscript.
References
- 1.Bristow MR, Saxon LA, Boehmer J, Krueger S, Kass DA, De Marco T, et al. Cardiac-resynchronization therapy with or without an implantable defibrillator in advanced chronic heart failure. N Engl J Med. 2004;350:2140–50. doi: 10.1056/NEJMoa032423. [DOI] [PubMed] [Google Scholar]
- 2.Cleland JG, Daubert JC, Erdmann E, Freemantle N, Gras D, Kappenberger L, et al. Cardiac Resynchronization-Heart Failure (CARE-HF) Study Investigators. The effect of cardiac resynchronization on morbidity and mortality in heart failure. N Engl J Med. 2005;352:1539–49. doi: 10.1056/NEJMoa050496. [DOI] [PubMed] [Google Scholar]
- 3.Nichol G, Kaul P, Huszti E, Bridges JF. Cost-effectiveness of cardiac resynchronization therapy in patients with symptomatic heart failure. Ann Intern Med. 2004;141:343–51. doi: 10.7326/0003-4819-141-5-200409070-00102. [DOI] [PubMed] [Google Scholar]
- 4.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the medicare fee-for-service program. N Engl J Med. 2009;360:1418–28. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 5.Feldman AM, de Lissovoy G, Bristow MR, Saxon LA, De Marco T, Kass DA, et al. Cost effectiveness of cardiac resynchronization therapy in the Comparison of Medical Therapy, Pacing, and Defibrillation in HeartFailure (COMPANION) trial. J Am Coll Cardiol. 2005;46:2311–21. doi: 10.1016/j.jacc.2005.08.033. [DOI] [PubMed] [Google Scholar]
- 6.Banz K on behalf of the Eucomed CRT Steering Committee. Cardiac resynchronization therapy (CRT) in heart failure—a model to assess the economic value of this new medical technology. Value Health. 2005;8:128–39. doi: 10.1111/j.1524-4733.2005.03092.x. [DOI] [PubMed] [Google Scholar]
- 7.Fox M, Mealing S, Anderson R, Dean J, Stein K, Price A, et al. The clinical effectiveness and cost-effectiveness of cardiac resynchronisation (biventricular pacing) for heart failure: systematic review and economic model. Health Technol Assess (Rockv) 2007;11:iii–iv. doi: 10.3310/hta11470. ix–248. [DOI] [PubMed] [Google Scholar]
- 8.Maniadakis N, Ekman M, Calvert MJ, Freemantle N, Karamalis M, Vardas P, et al. Cost effectiveness of cardiac resynchronization therapy in Greece: an analysis based on the Cardiac REsychronization in Heart Failure trial. Europace. 2011;13:1597–603. doi: 10.1093/europace/eur188. [DOI] [PubMed] [Google Scholar]
- 9.Linde C, Mealing S, Hawkins N, Eaton J, Brown B, Daubert JC. Cost-effectiveness of cardiac resynchronization therapy in patients with asymptomatic to mild heart failure: insights from the European cohort of the REVERSE (Resynchronization Reverses remodeling in Systolic Left Ventricular Dysfunction) Eur Heart J. 2011;32:1631–9. doi: 10.1093/eurheartj/ehq408. [DOI] [PubMed] [Google Scholar]
- 10.Neyt M, Stroobandt S, Obyn C, Camberlin C, Devriese S, De Laet C, et al. Cost-effectiveness of cardiac resynchronisation therapy for patients with moderate-to-severe heart failure: a lifetime Markov model. BMJ Open. 2011;1:e000276. doi: 10.1136/bmjopen-2011-000276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Boriani G, Diemberger I, Biffi M, Martignani C. Cost-effectiveness of cardiac resynchronisation therapy. Heart. 2012;98:1828–36. doi: 10.1136/heartjnl-2012-301845. [DOI] [PubMed] [Google Scholar]
- 12.Biffi M, Moschini C, Bertini M, Saporito D, Ziacchi M, Diemberger I, et al. Phrenic stimulation: a challenge for cardiac resynchronization therapy. Circ Arrhythm Electrophysiol. 2009;2:402–10. doi: 10.1161/CIRCEP.108.836254. [DOI] [PubMed] [Google Scholar]
- 13.Forleo GB, Della Rocca DG, Papavasileiou LP, Molfetta AD, Santini L, Romeo F, et al. Left ventricular pacing with a new quadripolar transvenous lead for CRT: early results of a prospective comparison with conventional implant outcomes. Heart Rhythm. 2011;8:31–7. doi: 10.1016/j.hrthm.2010.09.076. [DOI] [PubMed] [Google Scholar]
- 14.Forleo GB, Mantica M, Di Biase L, Panattoni G, Della Rocca DG, Papavasileiou LP, et al. Clinical and procedural outcome of patients implanted with a quadripolar left ventricular lead: early results of a prospective multicenter study. Heart Rhythm. 2012;9:1822–8. doi: 10.1016/j.hrthm.2012.07.021. [DOI] [PubMed] [Google Scholar]
- 15.Tomassoni G, Baker J, Corbisiero R, Love C, Martin D, Niazi I, et al. Postoperative performance of the quartet® left ventricular heart lead. J Cardiovasc Electrophysiol. 2013;24:449–56. doi: 10.1111/jce.12065. [DOI] [PubMed] [Google Scholar]
- 16.Sperzel J, Dänschel W, Gutleben KJ, Kranig W, Mortensen P, Connelly D, et al. First prospective, multi-centre clinical experience with a novel left ventricular quadripolar lead. Europace. 2012;14:365–72. doi: 10.1093/europace/eur322. [DOI] [PubMed] [Google Scholar]
- 17.Calò L, Martino A, De Ruvo E, Minati M, Fratini S, Rebecchi M, et al. Acute echocardiographic optimization of multiple stimulation configurations of cardiac resynchronization therapy through quadripolar left ventricular pacing: a tailored approach. Am Heart J. 2014;167:547–54. doi: 10.1016/j.ahj.2013.12.028. [DOI] [PubMed] [Google Scholar]
- 18.Vardas PE, Auricchio A, Blanc JJ, Daubert JC, Drexler H, Ector H, et al. Guidelines for cardiac pacing and cardiac resynchronization therapy. The task force for cardiac pacing and cardiac resynchronization therapy of the European Society of Cardiology. Developed in collaboration with the European Heart Rhythm Association. Europace. 2007;9:959–98. doi: 10.1093/europace/eum189. [DOI] [PubMed] [Google Scholar]
- 19.Hosmer DW, Lemeshow S. Applied logistic regression. 2nd ed. New-Jersey: Wiley-Blackwell; 2012. Assessing the fit of the model; pp. 143–203. [Google Scholar]
- 20.Barber JA. Thompson analysis of cost data in randomised controlled trials: an application of the non-parametric bootstrap. Stat Med. 2000;19:3219–36. doi: 10.1002/1097-0258(20001215)19:23<3219::aid-sim623>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 21.Nixon RM, Wonderling D, Grieve RD. Non-parametric methods for cost-effectiveness analysis: the central limit theorem and the bootstrap compared. Health Econ. 2010;19:316–33. doi: 10.1002/hec.1477. [DOI] [PubMed] [Google Scholar]
- 22.Rothman KJ. Epidemiology an introduction. London: Oxford University Press; 2002. pp. 130–43. [Google Scholar]
- 23.Singh JP, Fan D, Heist EK, Alabiad CR, Taub C, Reddy V, et al. Left ventricular lead electrical delay predicts response to cardiac resynchronization therapy. Heart Rhythm. 2006;3:1285–92. doi: 10.1016/j.hrthm.2006.07.034. [DOI] [PubMed] [Google Scholar]
- 24.Gold MR, Birgersdotter-Green U, Singh JP, Ellenbogen KA, Yu Y, Meyer TE, et al. The relationship between ventricular electrical delay and left ventricular remodelling with cardiac resynchronization therapy. Eur Heart J. 2011;32:2516–24. doi: 10.1093/eurheartj/ehr329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zanon F, Baracca E, Pastore G, Fraccaro C, Roncon L, Aggio S, et al. Determination of the longest intra-patient left ventricular electrical delay may predict acute hemodynamic improvement in cardiac resynchronization therapy patients. Circ Arrhythm Electrophysiol. 2014;7:377–83. doi: 10.1161/CIRCEP.113.000850. [DOI] [PubMed] [Google Scholar]