Abstract
Background
Use of transversus abdominis plane (TAP) block for postoperative analgesia is continuously increasing. However, few studies have investigated intraoperative effects of TAP block. We aimed to study the effects of TAP block in terms of cost-effectiveness and consumption of inhalation agents.
Material/Methods
Forty patients undergoing laparoscopic cholecystectomy were enrolled in this study. Patients were randomly divided into 2 groups: Group 1 (n=20) patients received TAP block and Group 2 (n=20) patients did not receive TAP block. Standard anesthesia induction was used in all patients. For the maintenance of anesthesia, fractional inspired oxygen (FIO2) of 50% in air with desflurane was used with a fresh gas flow of 4 L/min. All patients were monitored with electrocardiography and for peripheral oxygen saturation (SpO2), end-tidal carbon dioxide (ET), heart rate (HR), noninvasive mean blood pressure (MBP), and bispectral index (BIS). Bilateral TAP blocks were performed under ultrasound guidance to Group 1 patients. The BIS value was maintained at between 40 and 50 during the surgery. The Dion formula was used to calculate consumption of desflurane for each patient.
Results
There was no difference between the groups with respect to demographic characteristics of the patients. Duration of anesthesia, surgery time, and dosage of fentanyl were similar in the 2 groups. However, the cost and consumption of desflurane was significantly lower in Group 1.
Conclusions
Total anesthesia consumption was lower and the cost-effectiveness of anesthesia was better in TAP block patients with general anesthesia than in non-TAP block patients undergoing laparoscopic cholecystectomy.
MeSH Keywords: Anesthetics, Inhalation; Anesthetics, Local; Costs and Cost Analysis
Background
Due to increases in health expenditure, cost control is becoming more and more important. Inhaled anesthetics used in anesthesia departments account for about 20% of total anesthetic agents [1]. Local anesthetic agents decrease the minimum alveolar concentration (MAC) value of inhaled agents [2]. This mechanism of action may cause a decrease in the consumption of inhaled anesthetics. Transversus abdominis plane (TAP) block, which has analgesic efficiency, was firstly defined by Rafi in 2001 and its popularity is growing steadily [3]. TAP block forms a sensorial block by local anesthetic infiltration between the musculus obliquus abdominis internus and musculus transversus abdominis. This block occurs at 7–12 of thoracic intercostal nerves, ilioinguinal, iliohypogastric, and 1–3 of lumbar nerves of lateral cutaneous branches [4].
TAP block given to patients undergoing laparoscopic cholecystectomy for postoperative opioid analgesia resulted in a decrease of postoperative pain scores in the first 24 h [5,6].
Cost-effective studies are important in healthcare economics [7]. When we searched the literature, we could not find any study evaluating the cost-effectiveness of TAP block use in anesthetic practice. We think that TAP block has analgesic effects and decreases the consumption of inhalation agents. We aimed to investigate the cost-effectiveness of TAP block in anesthetic applications in laparoscopic procedures.
Material and Methods
This study was approved by the Afyon Kocatepe University Hospital Ethics Committee (2013/01-4) and written informed consent was obtained from each patient. Forty patients with American Society of Anesthesiologist (ASA) physical status I–II, ages 18–75 years, undergoing laparoscopic cholecystectomy were prospectively enrolled in this study.
Patients with cardiac, endocrinological, neurological diseases, or coagulation disorders, or allergy to local anesthetics were excluded from the study. Operations that started as laparoscopy but transitioned to open surgery for a surgical reason were also excluded.
Saline infusion was initiated as 5–7 ml/kg/h for all patients. Standard general anesthesia procedures were applied to all patients after preoxygenation with 8 L/min oxygen for 3 min. Anesthesia was induced with midazolam HCl 2 mg (i.v.), propofol 2 mg/kg (i.v.), rocuronium bromide 0.6 mg/kg (i.v.), and fentanyl 1.5 μg/kg (i.v.). Anesthesia start time was recorded. Endotracheal intubation was performed after obtaining sufficient muscle relaxation. In all cases, 4 L/min oxygen and air flow with desflurane 4%–9%, considering the BIS value, was performed. The patients were ventilated with a tidal volume of 8 ml/kg and the inspiratory rate was modulated to keep the end-tidal carbon dioxide (ET) at normal values of 30–40 mmHg.
Neuromuscular blockade was achieved intraoperatively with intermittent doses of intravenous rocuronium bromide 0.15 mg/kg when the train-of-four ratio reached 25%. Supplementary doses of fentanyl (50 μg) were administered if hemodynamic control could not be achieved within 5 min by a consecutive 2% increase in desflurane concentration in both groups [8]. Following the administration of general anesthesia to patients, they were randomly divided into 2 equal groups as Group I (n=20) and Group II by a computer program (Microsoft Excel; Microsoft Corporation, Redmond, WA, USA). TAP block was applied to patients in Group I but not to patients in Group II. Before each operation, leakage controls of anesthesia circuits and calibration of gas monitors were performed. In both groups, maintenance of anesthesia depth was obtained with bispectral index (BIS) monitoring (A-2000, Aspect Medical Systems, Natick, MA, USA). The BIS value was kept at 40–50 in both groups. When the lower limit of the BIS value was reached, the amount of inhalation agent was decreased. Conversely, when the upper limit of the BIS value was reached, inhalation agent was increased. Thus, equal conditions were maintained to determine the required amount of inhalation agents in both groups. Besides BIS monitoring, all patients were monitored with electrocardiography and for peripheral oxygen saturation (SpO2), ET, heart rate (HR), and noninvasive mean blood pressure (MBP). Neuromuscular function was also evaluated by acceleromyography of the adductor pollicis muscle (Datex-Ohmeda NMT module Helsinki, Finland).
TAP block was performed under ultrasound guidance using a 7–18 MHz broadband linear ultrasound probe (Toshiba Aplio MX ultrasound system, Toshiba Medical Systems, Tustin, California). The blocks were performed by anesthesiologists experienced with the technique and/or by residents under their direct supervision. The external oblique, internal oblique, and transverses abdominis muscles were displayed at the plane of the anterior axillary line between the 12th rib and the iliac crest. After sterilizing the insertion site, a 21-gauge, 100-mm Stimuplex A needle (B. Braun, Melsungen, Germany) was inserted with in-plane technique. The needle was then advanced in a posterolateral direction. When the tip of the needle was located in the space between the internal oblique and transverses abdominis muscles, a total of 15 mL of bupivacaine 0.5% was injected gradually after negative aspiration under direct ultrasound visualization. If spread of the local anesthetic was not adequate after initial injection, the needle was repositioned to optimize spread in the TAP. The contralateral block was performed in the same manner with 15 mL of bupivacaine 0.5% for a total of 30 mL per patient.
Dispersion of the local anesthetic during injection was readily observed with use of ultrasonography. With the observation of the dispersion of the local anesthetic under general anesthesia, TAP block was judged to be effective.
In both groups, heart rate, SpO2, MBP, and BIS values were recorded preoperatively and at the 1st, 3rd, 6th, 10th, 15th, 20th, 25th, 30th, 35th, 40th, 45th, 60th, and 90th minutes of intubation. ET values were recorded at the same times (except preoperatively) after intubation. Total fentanyl consumption of the patients was recorded. The%MAC values were recorded at the measurement time points after the first minute of intubation and when a gas increase or decrease was deemed necessary.
Total consumed inhalation agent amounts were calculated using the operation time and the MAC values, and the cost difference was determined. The formula [9] used for this calculation was:
where P is vaporizer concentration (%), F is fresh gas flow (L/min), T is anesthesia time (min), M is molecular weight (g), C is unit price (//mL), and d is density (g/mL): C=0.2 $/mL; M=168 g; d=1.47 g/mL at 20-C.
Statistical analysis
SPSS software version 20.0 (Statistical Package for the Social Sciences Inc, Chicago, IL, USA) was used for statistical analysis. Distribution of variables was evaluated with the Kolmogorov-Smirnov test. Variables are expressed as mean (±) standard deviation (SD) or median (minimum-maximum) according to normal or non-normal distribution, respectively. Nominal variables were expressed as percentage. The t-test was used to compare parametric variables between groups if variables were normally distributed. The Mann-Whitney U test was used to compare 2 groups when the variables were not normally distributed. Statistical significance level was set at P<0.05.
Results
Forty patients were enrolled in this study. There was no significant difference between the groups in terms of weight, age, height, sex, and BMI of the patients. ASA classifications of the patients were similar in both groups (p>0.05) (Table 1).
Table 1.
Characteristics of patients in Group 1 and Group 2.
| Group 1 | Group 2 | P | |
|---|---|---|---|
| Age, years | 53.45±13.22 | 44.80±10.60 | 0.028 |
| Weight, kg | 78.10±5.53 | 76.75±7.63 | 0.526 |
| Height, cm | 167.15±4.46 | 168.00±7.42 | 0.663 |
| Sex, male/female | 9/11 | 10/10 | 0.752 |
| ASA, (I /II) | 11/9 | 14/6 | 0.327 |
| BMI, kg/m2 | 27.99±2.34 | 27.33±3.51 | 0.485 |
All values are presented as Mean±Standard Deviation (SD), otherwise indicated. BMI – Body mass index.
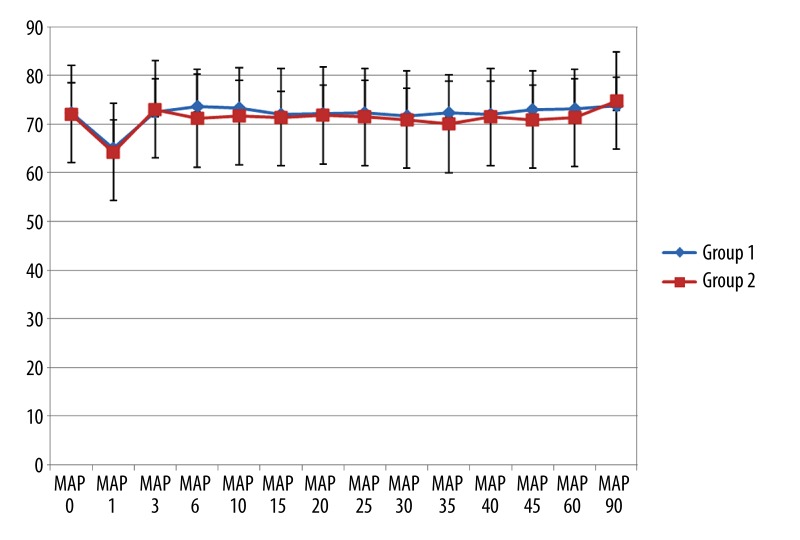
There were no differences in MAP values preoperatively and at the 1st, 3rd, 6th, 10th, 15th, 20th, 25th, 30th, 35th, 40th, 45th, 60th, and 90th minutes intraoperatively in both groups (p>0.05) (Figure 1).
Figure 1.
Course of mean arterial pressure (MAP) during surgery in both groups.
Heart rate, SpO2, and BIS values measured preoperatively and at the 1st, 3rd, 6th, 10th, 15th, 20th, 25th, 30th, 35th, 40th, 45th, 60th, and 90th minutes intraoperatively and end-tidal CO2 values measured at the same times intraoperatively were similar in both groups (p>0.05).
In both groups there were no differences in terms of duration of anesthesia, surgery time, or dosage of fentanyl consumption intraoperatively (p>0.05). The amount of desflurane consumption and cost of desflurane were significantly lower in patients of Group 1 (p<0.05) (Table 2).
Table 2.
Durations of anaesthesia and surgical procedures, total dosage of anaesthetics and cost of desflurane.*
| Group 1 | Group 2 | P | |
|---|---|---|---|
| Duration of anaesthesia, min | 91.15±10.78 | 90.90±9.81 | 0.939 |
| Duration of surgical procedure | 77.35±10.08 | 76.90±9.06 | 0.883 |
| Total Fentanyl, μg | 119.55±10.37 | 124.70±17.31 | 0.261 |
| Total Desflurane, ml | 102.35±10.55 | 121.90±11.69 | 0.0001 |
| Cost of Desflurane, USD | 20.47±2.11 | 24.38±2.33 | 0.0001 |
| Minimum Alveolar Concentration | 5.93±014 | 7.08±0.21 | 0.0001 |
All values are presented as Mean±Standard Deviation (SD), otherwise indicated.
Discussion
We found that consumption and cost of anesthetic gases were lower in TAP block patients after general anesthesia induction than in other patients undergoing laparoscopic cholecystectomy.
In recent years, the use of TAP block for postoperative analgesia after laparoscopic cholecystectomy has become increasingly popular. Various studies have been done concerning the effects of TAP block on postoperative pain and postoperative opioid consumption [5,6,10,11]. However, very few studies have investigated the effects of TAP block in the intraoperative period. El-Dawlaty et al. [5] investigated the effects of TAP block on sufentanyl use and postoperative analgesia. They gave 1 MAC of sevoflurane with additional doses of sufentanyl according to the hemodynamic data of the patients in both groups. They showed that intraoperative sufentanyl use was significantly lower in the TAP block group than the non-TAP block group [5]. Similarly, when opioid doses were similar between the groups in our study, the total doses of desflurane were lower in the TAP block group compared to the non-TAP block group. The dose of fentanyl used intraoperatively was 119.55±10.37 μg in Group 1, and 124.70±17.31 μg in Group 2. Lu et al. [8] and Gautam et al. [12] used similar doses of intraoperative fentanyl in colorectal surgery and laparoscopic surgery, respectively.
Lower consumption of desflurane in the TAP block group may be due to multiple mechanisms. During surgery, adequate analgesia and anesthesia should be provided to decrease surgical alerts to the lowest level. Neuroaxial blocks can be applied before the transmission of nosiceptive stimulation of surgical alerts [13]. Eappen et al. [14] demonstrated that thiopental consumption was lower in a spinal anesthesia group in which sedation was performed in addition to spinal anesthesia. They reported that spinal anesthesia reduces nociceptive stimulation directly by deafferentation. Likewise, epidural ropivakain dose-dependently reduces the MAC level of volatile anesthetic [15].
Göktas et al. [16] reported that local anesthetic infiltration after induction anesthesia during rhinoplasty decreased the consumption of desflurane. Furthermore, Lu et al. [8] stated that consumption of desflurane was lower in patients injected with a local anesthetic via epidural catheter than in patients who received saline injection following induction anesthesia in colorectal surgery. Researchers explained this effect as blocking of transmission of sensorial impulses with epidural local anesthetic. In our study, we postulate that TAP block performed just before general anesthesia reduced the MAC value of volatile anesthetics by suppressing surgical alerts from the surgical field.
It is well known that local anesthesics reduce the MAC value of inhalation anesthetics because of their central action after being absorbed from the injection site. Göktaş et al. gave adrenaline and lidocaine to patients in Group 1 or adrenaline alone to patients in Group 2 before rhinoplasty surgery. They showed that the MAC level of desflurane was significantly lower in Group 1 and that decreased values of inhalation agent MAC were caused by systemic absorption of local anesthetics. Another reason for reduction in desflurane consumption might be local anesthetic reduction effects of inhalation anesthetics on the MAC value.
We determined that TAP block applied just after general anesthesia reduced the consumption and cost of desflurane. We suggest that the effects of TAP block occur by 2 different mechanisms: 1) block applied before the surgical alert prevented the transmission of sensorial messages to top centers and 2) local anesthetic reduction effects on the MAC value of inhalation anesthetics.
Limitations of our study are that we could not evaluate the sensorial block level due to the application of the block just after general anesthesia and we did not measure the blood levels of local anesthetics.
The ratio of anesthesia cost to total treatment cost in hospitalized patients is around 5–6%, but there is a still an expectation to decrease this ratio. Johnstone et al. [17] showed that by using an inexpensive medication instead of expensive ones, a 23% savings could be achieved in anesthesia expenses, but in the yearly budget of the hospital, a 23% savings in 5–6% of anesthesia is a very small amount. However, investigation of factors that result in any decrease in anesthesia costs always remains relevant in healthcare economics. In a study of the cost-effectiveness of total intravenous anesthesia versus the balanced anesthesia method, a higher cost was seen in total intravenous anesthesia [18]. In the present study, we preferred the general anesthesia method, standardized the anesthesia depth with BIS, and calculated the cost of the inhalation agents used.
In studies comparing the quality of anesthesia and cost, more credible results can be obtained if anesthesia of equal depth is administered. BIS provides an objective appraisal of anesthesia depth by quantitatively measuring the effect of the anesthetic agent on the central nervous system [19]. Thus, it prevents excessive or inadequate anesthetic consumption. We also used BIS to assess the depth of sufficient anesthesia.
Conclusions
TAP block applied during laparoscopic surgery decreases the consumption and the cost of inhalation agents. We suggest that the cost-effectiveness and the consumption of inhalation agents combined with TAP block should be studied in other surgical procedures.
Footnotes
Source of support: Departmental sources
Conflict of interest
All authors declare that there is no conflict of interest or financial support.
References
- 1.Bach A. Costs of sevoflurane in the peri operative setting. Anaesthesist. 1998;47(Suppl 1):S87–96. doi: 10.1007/pl00002505. [DOI] [PubMed] [Google Scholar]
- 2.Senturk M, Pembeci K, Menda F, et al. Effects of intramuscular administration of lidocaine or bupivacaine on induction and maintenance doses of propofol evaluated by Bispectral Index. Br J Anaesth. 2002;89:849–52. doi: 10.1093/bja/aef287. [DOI] [PubMed] [Google Scholar]
- 3.Rafi AN. Abdominal field block: a new approach via the lumbar triangle. Anaesthesia. 2001;56:1024–26. doi: 10.1046/j.1365-2044.2001.02279-40.x. [DOI] [PubMed] [Google Scholar]
- 4.McDonnell JG, O’Donnell BD, Farrell T, et al. Transversus abdominis plane block: a cadaveric and radiological evaluation. Reg Anesth Pain Med. 2007;32:399–404. doi: 10.1016/j.rapm.2007.03.011. [DOI] [PubMed] [Google Scholar]
- 5.El-Dawlatly AA, Turkistani A, Kettner SC, et al. Ultrasound-guided transversus abdominis plane block: description of a new technique and comparison with conventional systemic analgesia during laparoscopic cholecystectomy. Br J Anaesth. 2009;102:763–67. doi: 10.1093/bja/aep067. [DOI] [PubMed] [Google Scholar]
- 6.Ra YS, Kim CH, Lee GY, Han JI. The analgesic effect of the ultrasound-guided transverse abdominis plane block after laparoscopic cholecystectomy. Korean J Anesthesiol. 2010;58:362–68. doi: 10.4097/kjae.2010.58.4.362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vanagas G. Do the cost in recently published papers are measured appropriately? Med Sci Monit. 2004;10(7):LE9–11. [PubMed] [Google Scholar]
- 8.Lu CH, Borel CO, Wu CT, et al. Combined general-epidural anesthesia decreases the desflurane requirement for equivalent A-line ARX index in colorectal surgery. Acta Anaesthesiol Scand. 2005;49(8):1063–67. doi: 10.1111/j.1399-6576.2005.00726.x. [DOI] [PubMed] [Google Scholar]
- 9.Dion P. The cost of anaesthetic vapours. Can J Anaesth. 1992;39:633. doi: 10.1007/BF03008331. [DOI] [PubMed] [Google Scholar]
- 10.Petersen PL, Stjernholm P, Kristiansen VB, et al. The beneficial effect of transversus abdominis plane block after laparoscopic cholecystectomy in day-case surgery – a randomized clinical trial. Anesth Analg. 2012;115:527–33. doi: 10.1213/ANE.0b013e318261f16e. [DOI] [PubMed] [Google Scholar]
- 11.Ortiz J, Suliburk JW, Wu K, et al. Bilateral transversus abdominis plane block does not decrease postoperative pain after laparoscopic cholecystectomy when compared with local anesthetic infiltration of trocar insertion sites. Reg Anesth Pain Med. 2012;37(2):188–92. doi: 10.1097/AAP.0b013e318244851b. [DOI] [PubMed] [Google Scholar]
- 12.Gautam S, Agarwal A, Das PK, et al. Evaluation of the efficacy of methylprednisolone, etoricoxib and a combination of the two substances to attenuate postoperative pain and PONV in patients undergoing laparoscopic cholecystectomy: a prospective, randomized, placebo-controlled trial. Korean J Pain. 2014;27(3):278–84. doi: 10.3344/kjp.2014.27.3.278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ceyhan D, Güleç MS. Is postoperative pain only a nociceptive pain? Agrı. 2010;22(2):47–52. [PubMed] [Google Scholar]
- 14.Eappen S, Kissin I. Effect of subarachnoid bupivacaine block on anesthetic requirements for thiopental in rats. Anesthesiology. 1998;88:1036–42. doi: 10.1097/00000542-199804000-00024. [DOI] [PubMed] [Google Scholar]
- 15.Zhang J, Zhang W, Li B. The effect of epidural anesthesia with different concentrations of ropivacaine on sevoflurane requirements. Anesth Analg. 2007;104(4):984–86. doi: 10.1213/01.ane.0000258765.16164.27. [DOI] [PubMed] [Google Scholar]
- 16.Goktas U, Isik D, Kati I, et al. Effects of lidocaine infiltration on cost of rhinoplasty made under general anesthesia. J Craniofac Surg. 2011;22(6):2176–78. doi: 10.1097/SCS.0b013e318232414c. [DOI] [PubMed] [Google Scholar]
- 17.Johnstone RE, Jozefczk KG. Costs of anesthetic drugs: experience with a cost education trial. Anesth Analg. 1994;78:766–71. doi: 10.1213/00000539-199404000-00026. [DOI] [PubMed] [Google Scholar]
- 18.Epple J, Kubitz J, Schmidt H, et al. Comparative analysis of costs of total intravenous anaesthesia with propofol and remifentanil vs. balanced anaesthesia with isoflurane and fentanyl. Eur J Anaesthesiol. 2001;18:20–28. doi: 10.1046/j.1365-2346.2001.00764.x. [DOI] [PubMed] [Google Scholar]
- 19.Sleigh JW, Andrzejowski J. The bispectral index: a measure of depth of sleep? Anesth Analg. 1999;88(3):659–61. doi: 10.1097/00000539-199903000-00035. [DOI] [PubMed] [Google Scholar]