Abstract
Introduction
Rising medical care expenditures and the unchanging Medicare reimbursements have placed restraints on the health care delivery system.
Objective
The goal of this study is to identify the magnitude and determinants of discrepancy between hospitalization charges and Medicare re-imbursement observed in the management of Medicare beneficiaries admitted with aneurysmal subarachnoid hemorrhage in the United States.
Methods
Patients entered in the Nationwide Inpatient Sample between 2002 and 2010, with a ruptured intracranial aneurysm who underwent either surgical or endovascular treatment were included in the study. Factors associated with higher discrepancy between hospitalization charges and Medicare re-imbursement were identified.
Results
Discrepancies in hospital charges and Medicare reimbursement associated with endovascular and surgical treatment have increased over the decade. The median discrepancy per patient for Medicare patients aged 65 years and older treated surgically or endovascularly for a ruptured aneurysm from 2009 to 2010 was $177,380. The predictors of higher than median discrepancy(charges versus reimbursement), included Hispanic ethnicity (OR 2.1, 95% CI 1.1–3.9, p = 0.02), urinary tract infection (OR 2.0, 95% CI 1.4–2.8, p = <0.001), pneumonia (OR 3.0, 95% CI 1.8–4.8, p = <0.001), deep vein thrombosis (OR 2.5, 95% CI 1.2–5.2, p = 0.02), and pulmonary embolism (OR 18, 95% CI 2.0–169, pp = 0.01).
Conclusions
There is a growing gap between hospital charges and Medicare reimbursement. If hospitals continue to be reimbursed at significantly lower rates than charges incurred, this current system may be unsustainable due to losses incurred by hospitals.
Abbreviations
- AHRQ
Agency for Healthcare Research and Quality
- CMS
Centers for Medicare and Medicaid services
- NIS
Nationwide Inpatient Sample
Keywords: Aneurysm, charges, hospital, endovascular treatment, Medicare, reimbursement, surgical treatment, subarachnoid hemorrhage
Introduction
Background
Rising medical expenditures and the disproportionately lower increase in Medicare reimbursements have placed restraints on the health care delivery system. The annual national health spending is currently increasing at a rate of 3.9% per year based on the summary statement published by the Centers for Medicare and Medicaid services(CMS) [1]. In 2011, the national health spending had reached 2.7 trillion dollars. In 2018, the national health spending is expected to reach 4.4 trillion dollars and comprise 20.3% of Gross Domestic Product [2]. However, the Medicare budget is projected to decrease as mandated by the sustainable growth rate formula and the sequestration process of the Budget Control Act of 2011 (which requires an estimated 2% cut to Medicare payments across all types of service from 2013 to 2022). The consequent discrepancy between charges associated with hospitalization which forms a major component of medical expenditures and relatively fixed re-imbursement from Medicare based on the DRG system is widely recognized [3–5]. The discrepancy is expected to be the highest in certain patients such as those with subarachnoid hemorrhage in whom high expense endovascular treatments are increasingly used. The discrepancy can lead to hospitals avoiding care of such patients to reduce the associated economic burden. Such discrepancy can also result in restricted treatment choices made by physicians. Further characterization of the aforementioned discrepancy is essential to prevent suboptimal care for patients with subarachnoid hemorrhage.
Objectives
The goal of this study is to identify the magnitude and determinants of discrepancy between hospitalization charges and Medicare re-imbursement observed in the management of Medicare beneficiaries admitted with aneurysmal subarachnoid hemorrhage in the United States.
Methods
Study design and data sources
The analysis is based on the data derived from the Nationwide Inpatient Sample (NIS) data files. The NIS is sponsored by the Agency for Healthcare Research and Quality (AHRQ), and data are collected from approximately 1000 hospitals resulting in a an aggregate of 7–8 million admissions annually. These data provide a 20% stratified sample of acute care community hospital admissions which can be extrapolated for deriving nationwide estimates. These data include patients reimbursed through any of existing payers/programs in the United States including Medicare.
Setting
Different geographic areas of the United States are represented, including the Northeast, Midwest, West, and South. Detailed information about the design of the NIS is available at http://www.hcup-us.ahrq.gov. The NIS includes >100 clinical and nonclinical variables for each hospital stay. The variables include primary and secondary diagnoses, primary and secondary procedures, patient demographics (including age, gender, race/ethnicity), admission and discharge information, and length of stay.
Participants and study size
Data regarding Medicare patients 65 years and older were extracted from the NIS files from 2002 to 2010. Patients with a primary diagnosis of subarachnoid hemorrhage, International Classification of Disease, 9th Revision clinical modifier (ICD-9 CM) code 430 who had procedure codes of surgical treatment (39.51) or endovascular treatment (39.79, 39.72, or 39.52) of cerebral aneurysms were identified. Patients who had both surgical treatment (39.51) and endovascular treatment (39.79, 39.72, or 39.52) procedure codes were excluded in the analysis. The ICD-9 codes for surgical and endovascular treatment of intracranial aneurysmshave been validated in the past [6, 7].
Variables
Patient related variables at admission
Data regarding patient’s demographic and clinical characteristics including age, gender, race/ethnicity, and co-morbid conditions including hypertension, diabetes mellitus, dyslipidemia, congestive heart failure, chronic lung disease, renal failure, and alcohol abuse were acquired from AHRQ co-morbidity data files. We used ICD-9-CM secondary diagnosis codes to identify the co-morbidities of atrial fibrillation (427.30 and 427.31), and nicotine dependence (305.1). All Patient Refined Diagnosis Related Group (APR-DRG) severity of illness was also ascertained. Severity of illness subclasses are based on the patient’s complicating or co-morbid conditions, and are specific to the patient’s baseline APR-DRG. The data elements used to determine the patient’s severity of illness and risk of mortality include the principal and secondary diagnoses coded in the ICD-9-CM, age, sex, and discharge disposition. The subclasses are numbered 1–4 and include minor, moderate, major, and extreme severity of illness [8].
Patient related variables during hospitalization
ICD-9-CM secondary diagnosis codes were also used to identify those with complications such as pneumonia (486, 481, 482.8, and 482.3), urinary tract infection (599.0, 590.9), sepsis (995.91, 996.64, 038, 995.92, and 999.3), deep venous thrombosis (451.1, 451.2, 451.81, 451.9, 453.1, 453.2, 453.8, and 453.9), pulmonary embolism (415.1), myocardial infarction (410.0–410.9), and intracerebral hemorrhage (431–432). We also used ICD-9-CM procedure codes to identify patients who underwent procedures such as cerebral angiography (88.41), tracheostomy (31.10, 31.20, 31.21, or 31.29), mechanical ventilation (9672), transfusion (99.04), intubation (96.04), and gastrostomy (431.1–431.9). We categorized routine discharge as minimal disability, and any other discharge status as moderate to severe disability as described previously [9].
Hospital-related variables
The NIS defines teaching hospitals as hospitals with an American Medical Association approved residency program, hospitals which are members of the Council of Teaching Hospitals (COTH) or hospitals that have a ratio of full-time equivalent interns and residents to beds of .25 or higher [10]. Bed size categories are based on the number of hospital beds, and the categorization into small, medium, and large is dependent on the hospital’s location and teaching status. For example, urban teaching hospitals in the Northeast are categorized as small (1–249 beds), medium (250–425 beds), and large(425+ beds) based on these bed size thresholds.
Quantification of discrepancy
We determined the factors associated with discrepancies in hospital charges and Medicare reimbursement for Medicare patients treated for a ruptured aneurysm using the NIS data from January 1, 2009 to December 31, 2010. The discrepancy was determined by subtracting the Medicare reimbursement rate from the total hospitalization charges. The derived value was dichotomized at the median value to provide two groups of patients based on the magnitude of discrepancy. The median discrepancy for Medicare patients aged 65 years and older treated with surgical or endovascular treatment for a ruptured aneurysm from 2009 to 2010 was found to be $177,380. Age, gender, race/ethnicity, associated diagnoses, procedures performed, length of stay, discharge status, and total hospitalization charges were determined for all cases.
The analysis was adjusted for the following factors: age, gender, race/ethnicity, co-morbid conditions (hypertension, diabetes mellitus, dyslipidemia, atrial fibrillation, congestive heart failure, chronic lung disease, renal failure, nicotine dependence), in-hospital complications (pneumonia, deep venous thrombosis, urinary tract infection, sepsis, pulmonary embolism, myocardial infarction), in-hospital procedures (endovascular treatment of the aneurysm, surgical treatment of the aneurysm, cerebral angiography, intubation, gastrostomy, tracheostomy, mechanical ventilation, blood transfusion), hospital bed size, and teaching status.
We also examined the yearly trends in the proportion of procedures (endovascular versus surgical) performed and in the mean discrepancy between charges versus re-imbursement rate using the NIS data from 2002 to 2010. In comparing total hospital charges between the years, we assumed a 3% annual inflation rate for each year and adjusted the charges in the linear mixed model. We also compared the discrepancy in the subgroup of patients based on whether they were treated with surgical or endovascular treatment.
Statistical analysis
The software program SAS 9.1 (SAS Institute, Inc., Cary, NC) was used to convert raw counts generated from the NIS database into weighted counts to provide national estimates, following HCUP recommendations. We used univariate analysis, the chi-square test for categorical data, and the t-test for continuous data to identify differences in study variables and endpoints between patient groups based on discrepancy of charges versus re-imbursements. We compared the demographic characteristics (age, gender, race/ethnicity), co-morbid conditions, in hospital complications, and discharge status (none to mild disability, moderate to severe disability) among patients who had less than versus greater than the median discrepancy between charges versus reimbursement.
The effect of length of stay on charges was determined using linear mixed models adjusted for the following patient and hospital specific factors: age, gender, race/ethnicity, co-morbidities, in hospital complications, hospital bed size, and teaching status of the hospital.
Results
Participants
From 2002 to 2010, a total of 18,794 Medicare patients aged 65 years and older were admitted with aneurysmal subarachnoid hemorrhage that was treated with surgical or endovascular treatment. Of the 18,794 patients admitted, 8,499 underwent surgical treatment and 10,295 patients underwent endovascular treatment of the ruptured aneurysm.
Main results and descriptive data
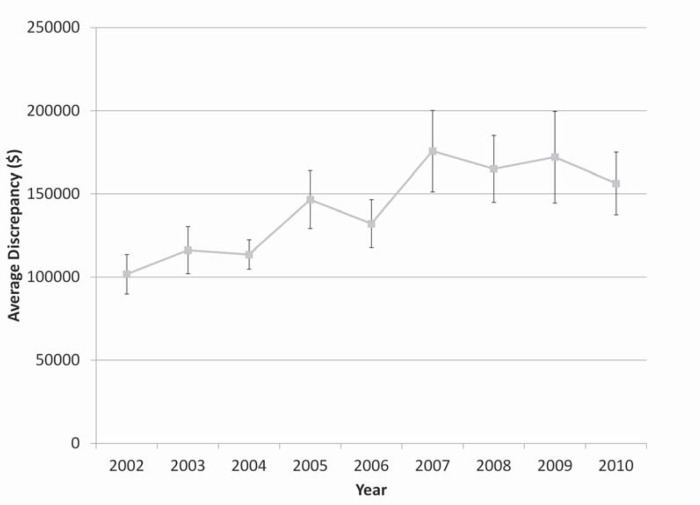
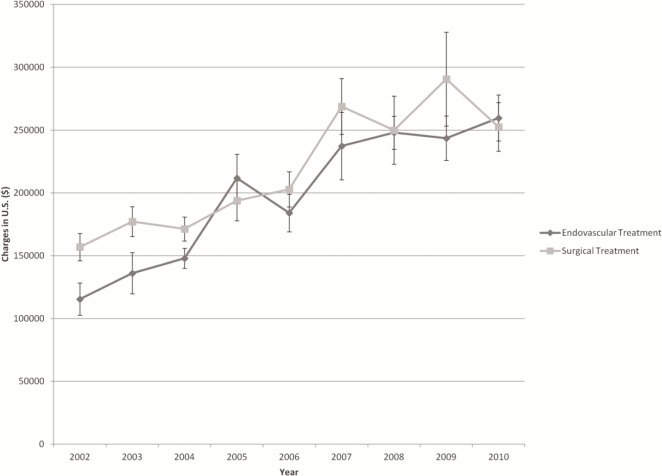
Figure 1 shows that the discrepancies in hospital charges and Medicare reimbursement associated with endovascular and surgical treatment have increased over the decade. The hospital charges associated with endovascular treatment have increased almost twofold from 2002 to 2010. From 2002 to 2010, when adjusted for inflation, the charges for hospitalization for patients with ruptured aneurysms have increased from $152,131 to $191,974 for surgical treatment and from $111,983 to $197,373 for endovascular treatment. The hospital charges increased at an average rate of 2.9% per year for surgical treatment and at a rate of 7.3% per year for endovascular treatment. However, the reimbursement rate has not increased at this rate resulting in further discrepancy between hospital charges and reimbursement as shown in Figure 2.
Figure 1. Mean discrepancy between hospital charges and Medicare reimbursement among Medicare patients aged 65 years and older admitted with a ruptured aneurysm treated with surgical or endovascular treatment, 2002–2010. Error bars represent the standard error.
Figure 2. Mean discrepancy between hospital charges and Medicare reimbursement among Medicare patients aged 65 years and older admitted with a ruptured aneurysm and either treated with surgical treatment or endovascular treatment, 2002–2010. Error bars represent the 95% confidence interval.
The median discrepancy between hospital charges and Medicare reimbursement for patients treated for aneurysmal subarachnoid hemorrhage from 2009 to 2010 was $177,380. Table 1 compares patients whose discrepancy was less than or equal to versus greater than the median discrepancy. There were no significant age or gender differences associated with higher discrepancy. Hispanic ethnicity was associated with higher discrepancy with a higher proportion of patients of Hispanic ethnicity in the higher discrepancy group compared with the lower discrepancy group, 10.8% versus 4.7%, p = 0.002. Of all the co-morbid conditions evaluated in Table 1, congestive heart failure had a significant association with higher charges versus reimbursement discrepancy (odds ratio [OR] 1.7, 95% CI 1.0–2.8, p = 0.05). Surprisingly, nicotine dependence was associated with lower discrepancy. Patients in the higher charges versus reimbursement discrepancy group had a higher number of in hospital complications such as pneumonia, deep venous thrombosis, urinary tract infection, sepsis, pulmonary embolism, or myocardial infarction. Undergoing endovascular treatment compared with surgical treatment was not associated with a significant difference in discrepancy. Hospital procedures such as intubation (OR 2.2, 95% CI 1.4–3.3, p < 0.001), gastrostomy (OR 7.2, 95% CI 4.7–11.0, p = 0.001), mechanical ventilation (OR 3.9, 95% CI 2.6–5.8, p < 0.001), and blood transfusion (OR 3.0, 95% CI 1.9–4.6, p < 0.001) were more commonly performed in the higher charges versus reimbursement discrepancy group.
Table 1. Demographic and clinical characteristics of Medicare patients aged 65 years and older treated for aneurysmal subarachnoid hemorrhage in categories based on the median discrepancy between Medicare reimbursement and hospital charges (NIS 2009–2010).
| Discrepancy between Medicare reimbursement and hospital charges ≤ $177,380 | Discrepancy between Medicare reimbursement and hospital charges > $177,380 | P value | |
|---|---|---|---|
| Overall Number (%) | 3188 | 3256 | |
| Age mean (SD) | 73.9±15 | 73.1±13 | 0.09 |
| Women | 2461(77) | 2575(79) | 0.5 |
| Race/ethnicity | |||
| Whites | 2009(75.3) | 1713(66.3) | 0.03 |
| African Americans | 311(11.6) | 312(12.1) | 0.9 |
| Hispanics | 150(5.6) | 353(13.7) | 0.002 |
| Others | 198(7.5) | 203(7.9) | 0.9 |
| Co-morbid conditions | |||
| Hypertension | 2465(77.3) | 2360(72.4) | 0.1 |
| Diabetes mellitus | 468(14.7) | 565(17.3) | 0.2 |
| Dyslipidemia | 271(8.5) | 163(5.0) | 0.03 |
| Atrial fibrillation | 410(12.8) | 482(14.8) | 0.4 |
| Congestive heart failure | 239(7.5) | 396(12.1) | 0.05 |
| Chronic lung disease | 601(18.8) | 543(16.6) | 0.5 |
| Renal failure | 126(4.0) | 179(5.5) | 0.3 |
| Nicotine dependence | 604(19.0) | 324(10.0) | 0.01 |
| Alcohol abuse | 88(2.7) | 89(2.7) | 0.9 |
| In hospital complications | |||
| Pneumonia | 226(7.1) | 618(19.0) | < 0.001 |
| Deep venous thrombosis | 64(2.0) | 150(4.6) | 0.007 |
| Urinary tract infection | 735(23.0) | 1198(36.8) | < 0.001 |
| Sepsis | 150(4.7) | 356(11.0) | 0.04 |
| Pulmonary embolism | 5(0.1) | 75(2.3) | 0.009 |
| Myocardial infarction | 159(5.0) | 276(8.4) | 0.05 |
| In hospital procedures | |||
| Endovascular treatment | 2137(67.0) | 2159(66.3) | 0.8 |
| Surgical treatment | 1051(33.0) | 1096(33.7) | 0.8 |
| Cerebral angiography | 2365(74.1) | 2484(76.3) | 0.5 |
| Intubation | 679(21.3) | 1206(37.0) | 0.002 |
| Mechanical ventilation | 634(20.0) | 1603(49.2) | < 0.001 |
| Gastrostomy | 220(7.0) | 1136(35.0) | < 0.001 |
| Tracheostomy | 0(0) | 15(0.5) | n/a |
| Blood transfusion | 291(9.1) | 753(23.1) | < 0.001 |
| APRDRG severity of illness | < 0.001 | ||
| Minor loss of function | 109(3.5) | 10(0.3) | |
| Moderate loss of function | 470(14.7) | 112(3.4) | |
| Major loss of function | 1413(44.3) | 783(24.1) | |
| Extreme loss of function | 1195(37.5) | 2350(72.2) | |
| Hospital bed size | 0.03 | ||
| Small | 100(3.3) | 107(3.4) | |
| Medium | 336(10.7) | 158(5.0) | |
| Large | 2696(86.0) | 2896(91.6) | |
| Teaching status | 0.4 | ||
| Non teaching | 520(16.6) | 387(12.2) | |
| Teaching | 2613(83.4) | 2775(87.8) | |
| Hospital regions | 0.004 | ||
| Northeast | 445(14.0) | 587(18.0) | |
| Midwest | 714(22.4) | 560(17.2) | |
| South | 1515(47.5) | 931(28.6) | |
| West | 513(16.1) | 1177(36.2) | |
| Length of stay: Mean in days (SD) | 11.2±15 | 24.4±28 | < 0.001 |
| Hospital charges: Mean in $ (SD) | 131571±101603 | 385894±422787 | < 0.001 |
| Discharge disposition | |||
| None to minimal disability | 943(29.6) | 390(12.0) | < 0.001 |
| Moderate to severe disability | 1397(43.8) | 2383(73.2) | < 0.001 |
| In hospital mortality | 848(26.6) | 481(14.8) | < 0.001 |
Outcome data
Length of stay was higher in the higher charges versus reimbursement discrepancy group compared with the lower discrepancy group, [(mean ± SD) 24.4 ± 28 days versus 11.2 ± 15 days, p < 0.001]. A higher percentage of patients in the lower charges versus reimbursement discrepancy group had none to minimal disability at discharge compared with the higher discrepancy group (29.6% versus 12%, p < 0.001). A higher percentage of patients in the higher charges versus reimbursement discrepancy group had moderate to severe disability at discharge compared to the lower discrepancy group (73.2% versus 43.8%, p < 0.001). In-hospital mortality was higher in the lower discrepancy group compared to the higher discrepancy group.
Multivariate analysis showed that the predictors of higher discrepancies in hospital charges versus Medicare reimbursement included in-hospital complications and Hispanic ethnicity (OR 2.1, 95% CI 1.1–3.9, p = 0.02). Other predictos of higher charges versus reimbursement discrepancy included urinary tract infection (OR 2.0, 95% CI 1.4–2.8, p < 0.001), pneumonia (OR 3.0, 95% CI 1.8–4.8, p < 0.001), deep vein thrombosis (OR 2.5, 95% CI 1.2–5.2, p = 0.02), and pulmonary embolism (OR 18, 95% CI 2.0–169, p = 0.01). A positive correlation between length of stay and total hospital charges was found, R = 0.4, p < 0.001 after adjusting for potential confounders.
Discussion
The average hospital charges for the 6,443 Medicare patients aged 65 and older admitted with a ruptured aneurysm from 2009 to 2010 were $254,969 for endovascular treated patients and $265,404 for surgically treated patients. These charges are substantially higher than the 2008 average Medicare payment, $36,304 for treatment of subarachnoid hemorrhage patients with co morbidity, and $30,380 without co morbidity [11]. A 125% increase in the hospital charges associated with endovascular treatment and a 60% increase in the hospital charges of surgical treatment of ruptured aneurysms over 8 years was seen in our analysis. The current trend would suggest that the hospital charges may increase disproportionately with endovascular treatment. If this current trend continues, the hospital charges are anticipated to reach $458,297 for endovascular treatment and $269,479 for surgical treatment in next 10 years. Such trends result in ongoing charges versus reimbursement discrepancy among patients treated for ruptured aneurysms.
Another important observation was the large magnitude of gap between Medicare re-imbursement and hospital charges. Under Medicare Part A, Medicare reimburses acute care hospital inpatient stays based upon prospectively set rates. This payment system is called the inpatient prospective payment system and each case is assigned into a disease-related group (DRG). DRGs have different payment weights associated with them which are dependent on the average resources used to treat Medicare patients with that particular DRG. This system of reimbursement is defined by section 1886(d) of the Social Security Act [12]. Although, there are three current reimbursement categories of major complication or comorbidity versus complication or comorbidity versus no major complication and no comorbidity, the differences in re-imbursement are too small to offset the gap between Medicare re-imbursement and hospital charges.
Medicare makes some adjustments to the DRG based reimbursement to partially offset the varying costs associated with the hospital location. Adjustments are also made if the hospital treats a high percentage of low income patients through add-on payments. For example, a hospital that serves a disproportionate share of low income patients can qualify for an increase in Medicare reimbursement. In addition, approved teaching hospitals receive add-on payments for each case known as the indirect medical education adjustment. Furthermore, Medicare has provisions for providing extra payment for outlier cases that may be particularly expensive to protect hospitals from financial losses. This outlier payment is also an add-on to the DRG adjusted base payment rate. However, the widening gap between Medicare re-imbursement and hospital charges is unlikely to be offset by the add-on payments.
Key results
In our study, we were able to identify the following factors as predictors of major discrepancy between hospital charges and reimbursement which included in hospital complications such as urinary tract infection, pneumonia, deep vein thrombosis, and pulmonary embolism. In the study of hospital costs associated with the treatment unruptured aneurysms by Brinjiki et al, it was reported that hospital costs were related to whether or not the patient suffered complications leading to morbidity and mortality [13]. Our findings also demonstrate that a higher prevalence of hospital complications are a major contributor to discrepancy between hospital charges and reimbursement. Our study found that Hispanic ethnicity was associated with higher hospitalization charges even after controlling for patient and hospital characteristics, including the All Patient Refined Diagnosis Related Group severity of illness score. Gupta et al found that Hispanic children had higher hospital charges, 21% higher, compared with White children after adjusting for patient and hospital characteristics [14]. Lower income status has also been linked to higher hospitalization and treatment costs [15, 16]. It remains unknown whether the ethnicity and in-hospital complications are a marker of more severe disease such as poor Glasgow Coma Scale (GCS) or Hunt and Hess scores or have direct contribution to the discrepancy between Medicare re-imbursement and hospital charges.
Generalizability
Our study suggests that measures aimed at reducing in hospital complications may reduce the discrepancy between hospital charges and reimbursement. However, if in-hospital complications are a marker of more severe disease, than the effect of reduction in hospital complications may not make a major difference in hospital charges. There is a growing gap between hospital charges and Medicare reimbursement. If hospitals continue to be reimbursed at significantly lower rates than charges incurred, this current system may be unsustainable owing to losses incurred by hospitals. In such an event, the hospitals may choose triage patterns not dictated by medical necessity or reduce the intensity of care provided to subarachnoid hemorrhage patients. To avoid compromising patient care, there appears to be two options. The re-imbursement rate for subarachnoid hemorrhage admission can be increased by Medicare to adequately reimburse the hospitals for charges incurred. Alternatively, admissions with high hospital charges such as subarachnoid hemorrhage could be managed at designated hospitals with additional re-imbursement through add on payments and/or grant programs through CMS.
Limitations
There are several limitations to this study. The NIS does not provide information on the size or location of the aneurysm which may affect the associated costs of treatment. In addition, the hospital charges are given as a total and the individual costs of intervention and treatment of complications cannot be determined. The Hunt and Hess score and Fisher grade of the patients admitted is not recorded in the NIS database. This issue limits the ability to determine the effect that the initial disease severity had on outcome and hospital charges. Hospital charges are the prices hospitals assign to the various services rendered and they do not necessarily represent true hospital costs. The payments that hospitals receive are typically lower than their net charges [17]. However, charges must exceed costs to help cover other hospital expenditures such as indigent care, care rendered that is not reimbursed by insurance companies, costs of replacing equipment, adding technologic improvements, and maintaining the facility [17]. Though the exact difference in hospital charges compared with actual reimbursement received is not known in the study, the study highlights the prominent differences that are currently present.
Interpretation
Our analysis points out a widening gap between Medicare re-imbursement and hospital charges in treatment of subarachnoid hemorrhage patients with ruptured intracranial aneurysms. Further studies need to determine if reduction of hospital complications and/or adjustment in re-imbursement by CMS can reduce the existing gap and encourage hospitals to actively provide specialized programs for subarachnoid hemorrhage patients.
Acknowledgments
Adnan Qureshi has received funding from the National Institutes of Health RO1-NS44976-01A2 (medication provided by ESP Parma), American Heart Association Established Investigator Award 0840053N, National Institute of Health U01-NS062091-01A2, and the Minnesota Medical Foundation, Minneapolis, MN.
Funding Statement
All authors have read and approved the submitted manuscript. Daraspreet Kainth, Malik Adil, Hunar Kainth, Jaspreet Dhaliwal and Adnan Qureshi declare that we have no conflict of interest. Adnan Qureshi has received funding from the National Institutes of Health RO1-NS44976-01A2 (medication provided by ESP Parma), American Heart Association Established Investigator Award 0840053N, National Institute of Health U01-NS062091-01A2, and the Minnesota Medical Foundation, Minneapolis, MN.
References
- Office of the Centers for Medicare and Medicaid Services. NHE projections 2008–2018. 2009 Forecast summary and selected tables (available from: http://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/downloads/proj2008.pdf) [PubMed]
- Office of the Centers for Medicare and Medicaid Services. National Health expenditures projections 2011–2021. 2011 Forecast summary and selected tables (available from: http://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/Downloads/Proj2011PDF.pdf)
- Gundlach CA, Faulkner TP. Charge and reimbursement analysis for intensive care unit patients in a large tertiary teaching hospital. DICP. 1991;25(11):1231–5. doi: 10.1177/106002809102501113. [DOI] [PubMed] [Google Scholar]
- Reiter KL, Holmes GM, Broyles IH. Medicare, swing beds, and critical access hospitals. Med Care Res Rev. 2013;70(2):206–17. doi: 10.1177/1077558712463247. [DOI] [PubMed] [Google Scholar]
- Wilensky GR. Health economics. Stud Health Technol Inform. 2010;153:179–93. [PubMed] [Google Scholar]
- Hoh BL, et al. Length of stay and total hospital charges of clipping versus coiling for ruptured and unruptured adult cerebral aneurysms in the Nationwide Inpatient Sample database 2002 to 2006. Stroke. 2010;41(2):337–42. doi: 10.1161/STROKEAHA.109.569269. [DOI] [PubMed] [Google Scholar]
- Hoh BL, et al. In-hospital morbidity and mortality after endovascular treatment of unruptured intracranial aneurysms in the United States, 1996-2000: effect of hospital and physician volume. AJNR Am J Neuroradiol. 2003;24(7):1409–20. [PMC free article] [PubMed] [Google Scholar]
- APR-DRG Classification. (available from: http://www.ahrq.gov/qual/mortality/Hughessumm.pdf) [Google Scholar]
- Qureshi AI, et al. Thrombolytic treatment of patients with acute ischemic stroke related to underlying arterial dissection in the United States. Arch Neurol. 2011;68(12):1536–42. doi: 10.1001/archneurol.2011.213. [DOI] [PubMed] [Google Scholar]
- HCUP Nationwide Inpatient Sample. 2010 Design of the Nationwide Inpatient Sample (available from: http://www.hcup-us.ahrq.gov/db/nation/nis/DataElements_NIS_2002_Hospital.pdf)
- Society of Neurointerventional Surgery. Coding and Payment Guide: Neurovascular Treatment of Aneurysms (available from: http://www.bostonscientific.com/templatedata/imports/collateral/Reimbursement/Neurology/2008/NVUS1621_Rev01_hospital_guide_2008_final.pdf)
- Centers for Medicare & Medicaid Services Acute Inpatient Prospective Payment System. 2010 (available from: http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/index.html?redirect=/acuteinpatientpps/05_dsh.asp)
- Brinjikji W, et al. Hospitalization costs for endovascular and surgical treatment of unruptured cerebral aneurysms in the United States are substantially higher than medicare payments. AJNR Am J Neuroradiol. 2012;33(1):49–51. doi: 10.3174/ajnr.A2739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta RS, et al. Predictors of hospital charges for children admitted with asthma. Ambul Pediatr. 2006;6(1):15–20. doi: 10.1016/j.ambp.2005.07.001. [DOI] [PubMed] [Google Scholar]
- Gendo K, et al. Resource costs for asthma-related care among pediatric patients in managed care. Ann Allergy Asthma Immunol. 2003;91(3):251–7. doi: 10.1016/S1081-1206(10)63526-0. [DOI] [PubMed] [Google Scholar]
- Durham CA, et al. 2010The impact of socioeconomic factors on outcome and hospital costs associated with femoropopliteal revascularization J Vasc Surg 523600–6. (discussion 606–7.) [DOI] [PubMed] [Google Scholar]
- Finkler SA. The distinction between cost and charges. Ann Intern Med. 1982;96(1):102–9. doi: 10.7326/0003-4819-96-1-102. [DOI] [PubMed] [Google Scholar]