Abstract
Background
Bacterial pneumonia in newborns often leads to surfactant deficiency or dysfunction, as surfactant is inactivated or its production/turnover impaired. No data are available in vivo in humans on the mechanism of surfactant depletion in neonatal pneumonia. We studied the kinetics of surfactant's major component, disaturated-phosphatidylcholine (DSPC), in neonatal pneumonia, and we compared our findings with those obtained from control newborn lungs.
Methods
We studied thirty-one term or near-term newborns (gestational age 39.7±1.7 weeks, birth weight 3185±529 g) requiring mechanical ventilation. Fifteen newborns had pneumonia, while 16 newborns were on mechanical ventilation but had no lung disease. Infants received an intratracheal dose of 13C labeled dipalmitoyl-phosphatidylcholine at the study start. We measured the amount and the isotopic enrichment of DSPC-palmitate from serial tracheal aspirates by gas chromatography and gas chromatography-mass spectrometry, respectively, and we calculated the DSPC half-life (HL) and pool size (PS) from the isotopic enrichment curves of surfactant DSPC-palmitate.
Results
The mean DSPC amount obtained from all tracheal aspirates did not differ between the two groups. DSPC HL was 12.7 (6.5–20.2) h and 25.6 (17.9–60.6) h in infants with pneumonia compared with control infants (p = 0.003). DSPC PS was 14.1 (6.6–30.9) mg/kg in infants with pneumonia and 34.1 (25.6–65.0) mg/kg in controls, p = 0.042. Myeloperoxidase (MPO) activity, as a marker of lung inflammation, was 1322 (531–2821) mU/ml of Epithelial Lining Fluid (ELF) and 371(174–1080) mU/ml ELF in infants with pneumonia and in controls, p = 0.047. In infants with pneumonia, DSPC PS and HL significantly and inversely correlated with mean Oxygenation Index (OI) during the study (DSPC PS vs. OI R = −0.710, p = 0.004 and HL vs. OI R = −0.525, p = 0.044, respectively).
Conclusions
We demonstrated for the first time in vivo in humans that DSPC HL and PS were markedly impaired in neonatal pneumonia and that they inversely correlated with the degree of respiratory failure.
Introduction
Pulmonary surfactant plays an important role in the host defense against respiratory infections. Bacterial pneumonia of near-term or term newborns often leads to surfactant deficiency or dysfunction, as surfactant is inactivated, peroxidated, or its secretion is impaired [1]–[3]. Research on the benefits of exogenous surfactant for the treatment of neonatal pneumonia is not well established. Studies on animal models [4]–[6], clinical case reports [7], and non-randomized clinical trials [8]–[10] that included mostly preterm infants, suggested that exogenous surfactant might be useful to infants with bacterial pneumonia. Almost all these studies included infants < 33 weeks gestational age, who received exogenous surfactant for primary surfactant deficient respiratory distress syndrome (RDS) associated with congenital or acquired bacterial pneumonia [11], [12]. Little information is available on term and near-term infants with neonatal pneumonia without RDS. Indirect evidence of a beneficial effect of exogenous surfactant on neonatal pneumonia can be derived from the use of surfactant in infants with meconium aspiration syndrome where surfactant inactivation could be the main mechanism of surfactant deficiency, similar to what is observed in neonatal pneumonia [13]. In these studies, dosing and the means of administration were important aspects of the response to exogenous surfactant [14], [15]. However, a recent Cochrane review underlined the lack of randomized clinical trials (RCTs) supporting or refuting the clinical benefits and safety of exogenous surfactant in neonatal pneumonia [16]. The authors of that review advocated future RCTs on term or near-term infants with proven bacterial pneumonia to test the efficacy of higher or more frequent surfactant doses than those required for replacement therapy in preterm infants with RDS (11). A deeper knowledge of surfactant pharmacokinetics in neonates with bacterial pneumonia not treated with exogenous surfactant would be of great value in designing these trials.
Studies on exogenous surfactant pharmacokinetics have become available only in recent years using DSPC (the most abundant surfactant phospholipid component) labeled with stable isotopes as an indicator of lung surfactant kinetics [17]–[19].
We applied these techniques to evaluate whether alterations of endogenous surfactant kinetics occur in term or near-term neonates with pneumonia and are associated with the severity of the lung disease. This hypothesis, if confirmed, would strengthen the rationale for novel trials with tailored exogenous surfactant doses and/or rates of surfactant administration as treatments for severe neonatal pneumonia.
Methods
Patients and study design
We conducted a prospective study in the Neonatal Intensive Care Units of the University of Padua and of the Polytechnic University of Marche, Ancona, Italy. We recruited 31 term newborns on mechanical ventilation for severe pneumonia (15 infants) and for major surgery or neurological failure but with no lung disease (16 infants). The study lasted from January 2008 to December 2011.
Eligible infants were late preterm (35 to 36 weeks completed gestation) or term newborns (37 to 41 weeks completed gestation) up to 28 days of life with diagnosis of pneumonia, defined according to the 2008 CDC/NHSN (Centers for Disease Control and Prevention/National Healthcare Safety Network) criteria for pneumonia in infants ≤1 year of age [20]. These are basically limited to clinically defined pneumonia (PNU1), characterized by: i) Chest X-Ray showing new or progressive or persistent infiltrate, consolidation or cavitation or pneumatoceles; ii) Worsening gas exchange (desaturation or rise in oxygen requirement or rise in ventilation demand); iii) At least 3 of the following: temperature instability with no other recognized cause; leukopenia (<4000 WBC/mm3) or leucocytosis (≥15000 WBC/mm3) with left shift (≥10% band cells); new onset of purulent sputum, or change in character of sputum, or increased respiratory secretions, or increased suctioning requirements; apnea, tachypnea, nasal flaring with retraction of chest wall or grunting; wheezing, rales or rhonchi; cough; bradycardia (<100 beats/min) or tachycardia (>170 beats/min).
Inclusion criteria were: a) severe respiratory failure (newborns with pneumonia) requiring mechanical ventilation with a Fraction of Inspired Oxygen, (FiO2) >0.35 and a Mean Airway Pressure, (MAP) >7 cm H2O, and a prediction to be on a ventilator for at least 48 h; b) newborns with no lung disease (controls), requiring mechanical ventilation as a result of major surgery or neurological failure leading to poor airway control; c) the presence of an indwelling arterial line, inserted for close clinical monitoring and gas exchange analysis, required for the severity of respiratory failure. Exclusion criteria were: severe congenital malformations, chromosomal abnormalities, and exogenous surfactant administration at the time of the study.
The protocol was approved by the Ethics Committee of the University of Padua and by the Ethics Committee of the Polytechnic University of Marche, and written informed consent was obtained from both parents of each infant. No external funding sources were granted for this study. Parents were informed that their child was not going to benefit from the study, but that the study results could potentially help other infants with the same clinical condition.
As soon as the mechanical ventilation was started, and after the informed consent was obtained, all study infants received an intratracheal tracer dose (2 mg/kg) of U13C-Dipalmitoyl-Phosphatidylcholine (U13C-DPPC) mixed with a vehicle dose of 2 to 5 mg/kg of porcine surfactant (Curosurf, Chiesi Pharmaceuticals, Parma, Italy) via a small catheter inserted through the endotracheal tube at the carina level, to trace endogenous pulmonary surfactant. Stable isotope tracers are safe for human studies; they were prepared in a sterile way by the hospital pharmacy and the delivering procedure has been performed at several times in both Units with no side effects [17]–[19], [21]–[25].
We collected tracheal aspirates before the administration of the tracer (t = 0), every 6 h for the first 72 h, and then every 12 h for another 4 days or until extubation. The rate and the way of suctioning is standardized in both units for all ventilated patients; for this study we collected the secretions, that otherwise would have been discarded, in Lukens trap at the pre-set time points [21]. We recorded clinical data, vital and ventilator parameters hourly from our computerized bedside monitoring systems, and we performed arterial blood gas analysis every 6 hours to calculate Oxygenation Index (OI) as ((MAP*FiO2/PaO2)*100), and PaO2/FiO2 ratio as indicators of respiratory failure. The rate of monitoring, including arterial gas analysis, were prescribed independently from the study by the attending physician, thus no change was provided in the routine clinical assistance.
Tracheal aspirate collection and storage
Tracheal aspirates were obtained as previously described [21], [22]. Briefly, after instillation of 1 ml saline (0.9% NaCl) in the endotracheal tube, the neonate was gently hand-bagged and then tracheal secretions were collected through a Lukens trap. The samples were stored at 4°C for no longer than 3 h and brought to a final volume of 2 ml with 0.9% saline. Tracheal aspirates with visible blood were discarded. After gentle vortexing for 1 minute, 300 µl of tracheal aspirate fluid were freeze-thawed three times in liquid nitrogen and centrifuged at 13,000 rpm (2,325×g) for 45 min at 4°C. The supernatant was collected and stored at −20°C for myeloperoxidase activity (MPO) determination. The remaining tracheal aspirate volume was centrifuged at 400×g for 10 min. The supernatant was recovered and stored at −20°C until analysis.
Analytical methods
Lipids from tracheal aspirates were extracted using Bligh and Dyer's method [26] after addition of the internal standard heptadecanoylphosphatidylcholine. DSPC was isolated from the lipid extract by thin layer chromatography (TLC) [27]. DSPC fatty acids were derivatized as methyl-esters and stored at −20°C. DSPC fatty acid composition was analyzed by gas-chromatography-FID and the 13C enrichment of DSPC-palmitate by gas-chromatography-mass spectrometry (GC-MS Agilent, Milan, Italy). Enrichment values were expressed as mole percent excess (MPE).
MPO activity was measured spectrofotometrically using O-dianisidine and hydrogen peroxide. One unit (U) of MPO activity was defined as that degrading 1 µmol of hydrogen peroxide per minute at 25°C [18].
MPO activity and DSPC amounts were corrected by the urea dilution method and expressed as U/ml of Epithelial Lining Fluid (ELF) [28].
Calculations and statistical analysis
Surfactant DSPC kinetics and pools were calculated from the exponential region of the DSPC 13C-enrichment curves of serial tracheal aspirates as previously described in detail [18], [21]. Statistical analysis was performed using PASW Statistics 18.0 for Windows (SPSS Inc., Chicago, IL). Data are expressed as mean ± SD or median (IQR) according to the variable distribution. Comparisons were made by Student t-test and Mann-Whitney test for continuous variables, and by Chi-square for categorical variables. A p≤0.05 was considered as statistically significant. Spearman's correlation analysis was performed to test the dependency of DSPC HL and PS on ventilator and oxygenation parameters.
Results
We studied 31 term infants: 15 infants with pneumonia and 16 with no lung disease. Clinical characteristics of the two groups were reported in Table 1. Among control infants one had congenital myopathy, 5 had abdominal surgery requiring prolonged sedation and mechanical ventilation and 9 had hypoxic-ischemic encephalopathy with no oxygen dependency and with the need of mechanical ventilation due to neurological failure.
Table 1. Clinical characteristics of study patients.
| Newborns with pneumonia (N = 15) | Newborns with no lung disease (N = 16) | p | |
| Gestational Age (wks) (mean ± SD) | 39.3±1.2 | 40.1±1.9 | 0.239 |
| Birth Weight (g) (mean ± SD) | 3197±711 | 3173±283 | 0.909 |
| Gender (N°females/N°males) | 5/10 | 6/10 | 0.553 |
| Infants studied in centre 1 and 2 (N°/N°) | 4/11 | 7/9 | 0.269 |
| Intubation – study start interval (h) (median(IQR)) | 41(18–75) | 19(10–30) | 0.057 |
| Age at study start (days) (median(IQR)) | 2.3(1.2–3.7) | 2.4(1.1–7.5) | 0.693 |
| CRP at study start (mg/L) (median(IQR)) | 26.1(14.5–50.0) | 2.0(1.0–3.4) | <0.001 |
| CRP during study (mg/L) (median(IQR)) | 29.6(13.1–69.8) | 7.7(3.3–39.5) | 0.022 |
Ventilator and oxygenation parameters were shown in Table 2. We found significant differences between the two groups in CRP (C-Reactive Protein), MAP, FiO2, arterial PaO2, OI and PaO2/FiO2 ratio at the start of the study, according to the study design. The study started 41(18–75) h and 19(10–30) h after intubation in newborns with pneumonia and in the controls, respectively, (p = 0.057). This long time interval from intubation to the study start was necessary to match all the criteria required for the pneumonia diagnosis, and also to leave to the parents a convenient time to give the informed consent (the policy of both institutions is to leave to the parents the time to think about it before giving the consent).
Table 2. Ventilator and oxygenation parameters of patients at study start.
| Newborns with pneumonia (N = 15) | Newborns with no lung disease (N = 16) | p | |
| Ventilator style (N° HFOV/N° SIMV) | 4/11 | 0/16 | 0.043 |
| MAP (cmH2O) (median(IQR)) | 8.2(6.7–12.0) | 5.7(4.8–7.2) | 0.001 |
| FiO2 (mean ± SD) | 0.54±0.25 | 0.22±0.02 | <0.001 |
| OI (median(IQR)) | 5.9(3.3–10.4) | 1.8(1.2–2.8) | <0.001 |
| PaO2/FiO2 (median(IQR)) | 124(90–238) | 334(262–394) | <0.001 |
| Arterial pH (median(IQR)) | 7.36(7.30–7.41) | 7.35(7.31–7.40) | 0.908 |
| Arterial pO2 (median(IQR)) | 62.4(58.1–72.6) | 82.6(65.3–84.0) | 0.014 |
HFOV: High-Frequency Oscillatory Ventilation; SIMV: Synchronized Intermittent Mandatory Ventilation.
Survival to discharge was similar between the two groups (14 out of 15 in the pneumonia group, and 14 out of 16 in the control group, p = 0.525). No newborn was treated with Nitric Oxide and none developed oxygen dependency at 28 days of life.
MPO activity was significantly higher in the tracheal aspirates of newborns with pneumonia compared to those with no lung disease (1322 (531–2821) mU/ml ELF and 371 (174–1080) mU/ml ELF, p = 0.047, respectively) [28].
Mean DSPC concentrations in tracheal aspirates during the study period were not significantly different in the two study groups, being 1.2 (0.4–7.5) mg/ml ELF in the pneumonia group and 2.4 (0.7–3.9) mg/ml ELF in the control group, p = 0.790.
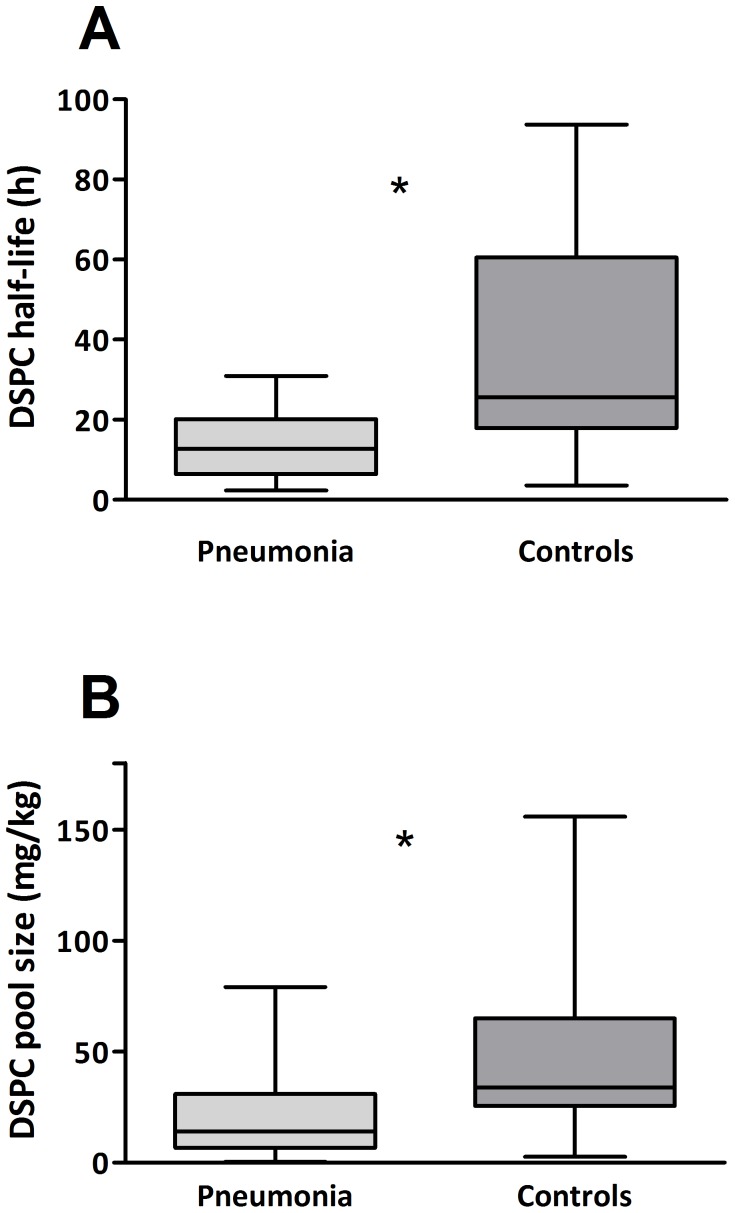
Surfactant DSPC kinetics could be calculated in all study patients. Median DSPC HL was significantly shorter in the pneumonia group compared to the median DSPC HL in the control group (12.7 (6.5–20.2) h and 25.6 (17.9–60.6) h, p = 0.003, respectively, Fig. 1 panel A). Similarly, median DSPC PS was found to be significantly lower in newborns with pneumonia compared to newborns with no lung disease (14.1 (6.6–30.9) mg/kg body weight and 34.1 (25.6–65.0) mg/kg body weight, p = 0.042, respectively, Fig. 1 panel B).
Figure 1. DSPC half-life (HL) and pool size (PS) in the two study groups.
Panel A: Median DSPC HL in the two groups. DSPC HL was significantly shorter in newborns with pneumonia (light grey box) compared with newborns with no lung disease (grey box). Data are expressed as median (IQR). Panel B: Median DSPC PS in the two groups. DSPC PS was significantly lower in newborns with pneumonia (light grey box) compared with newborns with no lung disease (grey box). Data are expressed as median (IQR).
Four out of 15 newborns with pneumonia required High Frequency Oscillatory Ventilation (HFOV), while all newborns in the control group were ventilated by Synchronized Intermittent Mandatory Ventilation (SIMV). Median DSPC HL was 9.7 (6.9–12.3) h in newborns on HFOV and 18.4 (5.2–20.8) h in newborns on SIMV, (p = 0.296). Median DSPC PS was markedly lower in the 4 infants who required HFOV compared to those ventilated with SIMV (3.1 (1.2–7.8) mg/kg body weight and 29.7 (9.3–31.7) mg/kg body weight, respectively, p = 0.036).
In the pneumonia group a significant correlation was found between DSPC PS and mean OI during the study (R = −0.710, p = 0.004) and also between DSPC HL and mean OI during the study (R = −0.525, p = 0.044).
Discussion
In this study, we measured for the first time surfactant DSPC kinetics in newborns with pneumonia and we found that endogenous surfactant DSPC HL and PS were markedly reduced in infants with pneumonia not treated with exogenous surfactant. We used a state of the art method, based on safe stable isotope markers [19], [23], which is applicable in vivo to intubated patients from whom sequential tracheal aspirates can be collected as part of the routine clinical care. We chose to assess the endogenous DSPC kinetics. Therefore we administered 2 to 5 mg/kg surfactant mixed with 13C DPPC, which cannot be considered a surfactant treatment dose. The advantage of using a stable isotope technique lies in the fact that kinetic data are more informative than DSPC concentrations. Measuring DSPC amounts from tracheal aspirates with or without a correction for dilution [28] can be deceiving because of the highly variable contribution of phospholipids from inflammatory cells. In this light, the mean amount of DSPC recovered was not different between the study groups.
The major finding of this study is that DSPC HL was significantly shorter in pneumonia than in controls. Interestingly, these HL values were similar to those reported by our group in the most severe RDS patients who required repeated doses of exogenous surfactant to overcome their respiratory failure [24], suggesting that the DSPC turnover in term or near term pneumonia is at least as fast as in the most severe cases of RDS.
However the efficacy of exogenous surfactant on neonatal pneumonia is still to be determined [16]. Only two non-randomized studies are available on the clinical outcome of neonatal pneumonia treated with exogenous surfactant. The first one included only preterm infants and found no difference in clinical outcome in infants with pneumonia compared with RDS [29]. The second one evaluated preterm and term infants with streptococcus B pneumonia treated with natural surfactant at doses of 100 or 200 mg/kg and found a slower clinical improvement in the pneumonia group compared to RDS [10].
The shorter DSPC HL likely led in infants with pneumonia to a significant reduction of surfactant PS, which was about one third of that measured in newborns with healthy lungs (controls). This is a novel result. Hallman et al. [30] and Griese et al. [31] reported PS estimates in preterm newborns with RDS of about 16 mg/kg. Values ranging from 1 to 15 mg/kg were found in preterm infants with RDS before exogenous surfactant [19], [21], [24], [25]; in adults with ARDS we found that surfactant PS was markedly and significantly lower than in controls [23]. Since pneumonia shares a certain pathophysiology with ARDS [32], it is not surprising to find similar alterations of surfactant pools, mediated by alveolar-capillary leaks of proteinaceous edema and inflammatory cells that contribute to surfactant inactivation and catabolism [3], [33], [34]. The significant increase of MPO activity that we found in infants with pneumonia supports this hypothesis. Whether exogenous surfactant can counteract the lack of endogenous surfactant pool in the acute phase of ARDS in infants is still debated. The only blinded, randomized, controlled study performed in ALI/ARDS pediatric patients who received natural surfactant (calfactant) relative to placebo (77 surfactant treated and 75 placebo) reported an immediate improvements in oxygenation and a significant survival advantage for patients receiving surfactant treatment.(33).
Four study infants with pneumonia received HFOV as rescue treatment for respiratory failure not responding to conventional ventilation. Interestingly these infants, who had the most severe degree of respiratory failure, had the most severe impairment of DSPC kinetics, with a significantly lower DSPC PS compared with controls. We hypothesize that the use of HFOV may not be responsible for the DSPC kinetic alterations, since the open lung concept, as an alternative ventilatory strategy, is reported to be a protective strategy for lung injury [35]–[37].
We also found that mean OI significantly correlated with DSPC PS and DSPC HL. Conversely, mean OI did not correlate with gestational age, the age at the start of the study, duration of mechanical ventilation and MPO activity. It will be difficult to ascertain whether FiO2 and mechanical ventilation play significant and independent roles in surfactant kinetics, or are proxies for respiratory severity. Mechanical ventilation and oxygen exposure may act as injury promoters in critically ill patients [38], inducing cytokine upregulation in both healthy and injured lungs [39]. Animal studies could help address this issue.
A limitation of our study is that the control infants were on mechanical ventilation for neuromuscular causes, prolonged sedation or neurological impairment. Although we acknowledge that the gold standard “controls” would have been infants spontaneously breathing room air, our study provides the best estimation of endogenous surfactant kinetics that can be obtained in humans with healthy lungs.
To our knowledge, this is the first report in neonatal pneumonia to show decreased surfactant DSPC PS and HL associated with disease severity in term or near-term newborn not treated with exogenous surfactant. The effect of exogenous surfactant administration on the endogenous surfactant kinetics is still unknown.
As we found comparable DSPC kinetic alterations in infants with the most severe RDS cases, who required multiple surfactant administrations [24], we speculate that higher doses of exogenous surfactant or shorter redosing time intervals than those used in neonatal RDS may be more appropriate for the treatment of the most severe cases of neonatal pneumonia.
Conclusions
In this study we reported the endogenous surfactant kinetics of late preterm and term newborns with pneumonia. DSPC HL and PS were markedly impaired in newborns with pneumonia. DSPC HL and PS were associated with oxygen requirement, which is a proxy for severity of lung disease. Further studies are required to confirm whether exogenous surfactant therapy could prolong DSPC HL, increase DSPC PS, and improve clinical outcome in neonatal pneumonia.
Funding Statement
The authors have no support or funding to report.
References
- 1. Zuo YY, Veldhuizen RA, Neumann AW, Petersen NO, Possmayer F (2008) Current perspectives in pulmonary surfactant—inhibition, enhancement and evaluation. Biochimica et biophysica acta 1778:1947–1977. [DOI] [PubMed] [Google Scholar]
- 2. Rudiger M, Friedrich W, Rustow B, Schmalisch G, Wauer R (2001) Disturbed surface properties in preterm infants with pneumonia. Biology of the neonate 79:73–78. [DOI] [PubMed] [Google Scholar]
- 3. Malloy JL, Wright JR (2004) In vivo clearance of surfactant lipids during acute pulmonary inflammation. Respiratory research 5:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Song GW, Robertson B, Curstedt T, Gan XZ, Huang WX (1996) Surfactant treatment in experimental Escherichia coli pneumonia. Acta anaesthesiologica Scandinavica 40:1154–1160. [DOI] [PubMed] [Google Scholar]
- 5. Stichtenoth G, Linderholm B, Bjorkman MH, Walter G, Curstedt T, et al. (2010) Prophylactic intratracheal polymyxin B/surfactant prevents bacterial growth in neonatal Escherichia coli pneumonia of rabbits. Pediatric research 67:369–374. [DOI] [PubMed] [Google Scholar]
- 6. Herting E, Gan X, Rauprich P, Jarstrand C, Robertson B (1999) Combined treatment with surfactant and specific immunoglobulin reduces bacterial proliferation in experimental neonatal group B streptococcal pneumonia. American journal of respiratory and critical care medicine 159:1862–1867. [DOI] [PubMed] [Google Scholar]
- 7. Harms K, Herting E (1994) Successful surfactant replacement therapy in two infants with ARDS due to chlamydial pneumonia. Respiration; international review of thoracic diseases 61:348–352. [DOI] [PubMed] [Google Scholar]
- 8. Herting E, Moller O, Schiffmann JH, Robertson B (2002) Surfactant improves oxygenation in infants and children with pneumonia and acute respiratory distress syndrome. Acta Paediatr 91:1174–1178. [DOI] [PubMed] [Google Scholar]
- 9. Gortner L, Pohlandt F, Bartmann P (1990) [Effect of a bovine surfactant in very low birth weight premature infants with congenital pneumonia]. Monatsschrift Kinderheilkunde: Organ der Deutschen Gesellschaft fur Kinderheilkunde 138:274–278. [PubMed] [Google Scholar]
- 10. Herting E, Gefeller O, Land M, van Sonderen L, Harms K, et al. (2000) Surfactant treatment of neonates with respiratory failure and group B streptococcal infection. Members of the Collaborative European Multicenter Study Group. Pediatrics 106:957–964 discussion 1135. [DOI] [PubMed] [Google Scholar]
- 11. Soll RF (2009) Current trials in the treatment of respiratory failure in preterm infants. Neonatology 95:368–372. [DOI] [PubMed] [Google Scholar]
- 12.Seger N, Soll R (2009) Animal derived surfactant extract for treatment of respiratory distress syndrome. The Cochrane database of systematic reviews: CD007836. [DOI] [PubMed]
- 13.El Shahed AI, Dargaville P, Ohlsson A, Soll RF (2007) Surfactant for meconium aspiration syndrome in full term/near term infants. Cochrane database of systematic reviews: CD002054. [DOI] [PubMed]
- 14. Lotze A, Mitchell BR, Bulas DI, Zola EM, Shalwitz RA, et al. (1998) Multicenter study of surfactant (beractant) use in the treatment of term infants with severe respiratory failure. Survanta in Term Infants Study Group. The Journal of pediatrics 132:40–47. [DOI] [PubMed] [Google Scholar]
- 15. Dargaville PA, Mills JF (2005) Surfactant therapy for meconium aspiration syndrome: current status. Drugs 65:2569–2591. [DOI] [PubMed] [Google Scholar]
- 16. Tan K, Lai NM, Sharma A (2012) Surfactant for bacterial pneumonia in late preterm and term infants. Cochrane Database Syst Rev 2:CD008155. [DOI] [PubMed] [Google Scholar]
- 17. Cogo PE, Carnielli VP, Bunt JE, Badon T, Giordano G, et al. (1999) Endogenous surfactant metabolism in critically ill infants measured with stable isotope labeled fatty acids. Pediatric research 45:242–246. [DOI] [PubMed] [Google Scholar]
- 18. Cogo PE, Simonato M, Mariatoffolo G, Stefanutti G, Chierici M, et al. (2008) Dexamethasone therapy in preterm infants developing bronchopulmonary dysplasia: effect on pulmonary surfactant disaturated-phosphatidylcholine kinetics. Pediatric research 63:433–437. [DOI] [PubMed] [Google Scholar]
- 19. Verlato G, Cogo PE, Pesavento R, Gomirato S, Benetazzo A, et al. (2003) Surfactant kinetics in newborn infants with pneumonia and Respiratory Distress Syndrome. Italian Journal of Pediatrics 29:414–419. [Google Scholar]
- 20. Horan TC, Andrus M, Dudeck MA (2008) CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. American journal of infection control 36:309–332. [DOI] [PubMed] [Google Scholar]
- 21. Torresin M, Zimmermann LJ, Cogo PE, Cavicchioli P, Badon T, et al. (2000) Exogenous surfactant kinetics in infant respiratory distress syndrome: A novel method with stable isotopes. Am J Respir Crit Care Med 161:1584–1589. [DOI] [PubMed] [Google Scholar]
- 22. Cogo PE, Zimmermann LJ, Pesavento R, Sacchetto E, Burighel A, et al. (2003) Surfactant kinetics in preterm infants on mechanical ventilation who did and did not develop bronchopulmonary dysplasia. Crit Care Med 31:1532–1538. [DOI] [PubMed] [Google Scholar]
- 23. Cogo PE, Toffolo GM, Ori C, Vianello A, Chierici M, et al. (2007) Surfactant disaturated-phosphatidylcholine kinetics in acute respiratory distress syndrome by stable isotopes and a two compartment model. Respiratory research 8:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Cogo PE, Facco M, Simonato M, De Luca D, De Terlizi F, et al. (2011) Pharmacokinetics and clinical predictors of surfactant redosing in respiratory distress syndrome. Intensive care medicine 37:510–517. [DOI] [PubMed] [Google Scholar]
- 25. Cogo PE, Facco M, Simonato M, Verlato G, Rondina C, et al. (2009) Dosing of porcine surfactant: effect on kinetics and gas exchange in respiratory distress syndrome. Pediatrics 124:e950–957. [DOI] [PubMed] [Google Scholar]
- 26. Bligh EG, Dyer WJ (1959) A rapid method of total lipid extraction and purification. Canadian journal of biochemistry and physiology 37:911–917. [DOI] [PubMed] [Google Scholar]
- 27. Touchstone JCC, JC. Beaver, MK Improved separation of phospholipids in thin layer chromatography. Lipids 15:61–62. [Google Scholar]
- 28. Dargaville PA, South M, Vervaart P, McDougall PN (1999) Validity of markers of dilution in small volume lung lavage. American journal of respiratory and critical care medicine 160:778–784. [DOI] [PubMed] [Google Scholar]
- 29. Brehmer U, Jorch G (1993) [Surfactant therapy in severe neonatal respiratory failure—multicenter study—III. Surfactant therapy in 41 premature infants < 34 weeks with suspected congenital infection (case-control analysis)]. Klinische Padiatrie 205:78–82. [DOI] [PubMed] [Google Scholar]
- 30. Hallman M, Merritt TA, Pohjavuori M, Gluck L (1986) Effect of surfactant substitution on lung effluent phospholipids in respiratory distress syndrome: evaluation of surfactant phospholipid turnover, pool size, and the relationship to severity of respiratory failure. Pediatric research 20:1228–1235. [DOI] [PubMed] [Google Scholar]
- 31. Griese M, Dietrich P, Reinhardt D (1995) Pharmacokinetics of bovine surfactant in neonatal respiratory distress syndrome. American journal of respiratory and critical care medicine 152:1050–1054. [DOI] [PubMed] [Google Scholar]
- 32. Bauer TT, Ewig S, Rodloff AC, Muller EE (2006) Acute respiratory distress syndrome and pneumonia: a comprehensive review of clinical data. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America 43:748–756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Quintero OA, Wright JR (2002) Clearance of surfactant lipids by neutrophils and macrophages isolated from the acutely inflamed lung. American journal of physiology Lung cellular and molecular physiology 282:L330–339. [DOI] [PubMed] [Google Scholar]
- 34. Ikegami M (2006) Surfactant catabolism. Respirology 11 Suppl: S24–27 [DOI] [PubMed] [Google Scholar]
- 35. Hilgendorff A, Aslan E, Schaible T, Gortner L, Baehner T, et al. (2008) Surfactant replacement and open lung concept—comparison of two treatment strategies in an experimental model of neonatal ARDS. BMC pulmonary medicine 8:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. van Kaam AH, de Jaegere A, Haitsma JJ, Van Aalderen WM, Kok JH, et al. (2003) Positive pressure ventilation with the open lung concept optimizes gas exchange and reduces ventilator-induced lung injury in newborn piglets. Pediatric research 53:245–253. [DOI] [PubMed] [Google Scholar]
- 37. van Kaam AH, Dik WA, Haitsma JJ, De Jaegere A, Naber BA, et al. (2003) Application of the open-lung concept during positive-pressure ventilation reduces pulmonary inflammation in newborn piglets. Biology of the neonate 83:273–280. [DOI] [PubMed] [Google Scholar]
- 38. Plataki M, Hubmayr RD (2010) The physical basis of ventilator-induced lung injury. Expert review of respiratory medicine 4:373–385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Halbertsma FJ, Vaneker M, Scheffer GJ, van der Hoeven JG (2005) Cytokines and biotrauma in ventilator-induced lung injury: a critical review of the literature. The Netherlands journal of medicine 63:382–392. [PubMed] [Google Scholar]