Abstract
Objective
The ethnic density hypothesis suggests that ethnic density confers greater social support and consequently protects against depressive symptoms in ethnic minority individuals. However, the potential benefits of ethnic density have not been examined in individuals who are facing a specific and salient life stressor. We examined the degree to which the effects of Hispanic ethnic density on depressive symptoms are explained by socioeconomic resources and social support.
Methods
Patients with acute coronary syndrome (ACS, N = 472) completed the Beck Depression Inventory (BDI) and measures of demographics, ACS clinical factors and disease severity, and perceived social support. Neighborhood characteristics, including median income, number of single-parent households, and Hispanic ethnic density, were extracted from the American Community Survey Census (2005 – 2009) for each patient using his/her geocoded address.
Results
In a linear regression analysis adjusted for demographic and clinical factors, Hispanic ethnic density was positively associated with depressive symptoms (β = .09, SE = .04, p = .03). However, Hispanic density was no longer a significant predictor of depressive symptoms when measures of neighborhood socioeconomic disadvantage were controlled. In addition, the effects of Hispanic density were not the same for all groups. The relationship of Hispanic density on depressive symptoms was moderated by nativity status. Among US-born patients with ACS, there was a significant positive relationship between Hispanic density and depressive symptoms, and social support significantly mediated this effect. There was no observed effect of Hispanic density to depressive symptoms for foreign-born ACS patients.
Discussion
Although previous research suggests that ethnic density may be protective against depression, our data suggest that among patients with ACS, living in a community with a high concentration of Hispanic individuals is associated with constrained social and economic resources which are themselves associated with greater depressive symptoms. These data add to a growing body of literature on the effects of racial or ethnic segregation on health outcomes.
Keywords: Ethnic density, post-ACS, depression, residential racial segregation, social support, cardiovascular disease
INTRODUCTION
Ethnic density refers to the proportion of individuals of a given ethnicity in a defined geographic area (Diez Roux & Mair, 2010). The ethnic density hypothesis suggests that ethnic density protects mental health and that this effect is mediated by social support (Yuan et al., 2007). Specifically, greater ethnic density is hypothesized to provide increased opportunities for engagement with others who share similar cultural or ethnic backgrounds, and these interactions are posited to confer social advantages including increased social support (Henderson et al., 2005). In turn, social support may facilitate stress recovery and prevent or mitigate the development of depressive symptoms or other mental health impairments in response to life stress.
The majority of studies (12/16) report a negative relationship of ethnic density to depression among ethnic and racial minority samples (Das-Munshi et al., 2010a; Gerst et al., 2011a; Halpern & Nazroo, 2000a; Hwang et al., 2000a; Leu et al., 2011; Mair et al., 2010b; Mintz & Schuartz, 1964; Neeleman et al., 2001; G V Ostir et al., 2003b; Pickett et al., 2009; Stafford et al., 2011; Walters et al., 2008), although there is evidence to suggest that the magnitude and direction of the effect is not completely uniform across ethnic groups (e.g., Bangladeshi's (Pickett et al., 2009); Mexicans (Lee, 2009a); and African-Americans; (Mair et al., 2010b). We specifically examine Hispanic ethnic density, as there is some evidence that the prevalence of depression may be higher for Hispanics than non-Hispanic individuals (Xie et al., 2008). Four of five studies have found that greater ethnic density is associated with reduced depressive symptoms among Hispanic samples (Gerst et al., 2011a; Lee, 2009a; Mair et al., 2010b; G V Ostir et al., 2003b; Yuan et al., 2007).
Despite the abundance of literature on the effects of ethnic density on depression, there is an absence of data confirming the role of social support as a mediator of this relationship. Of the five studies that have tested social support as a mediator of the relationship of Hispanic ethnic density to depression (Das-Munshi et al., 2010a, b; Halpern & Nazroo, 2000a, b; Roh et al., 2011a; Roh et al., 2011b; Syed & Juan, 2012; Vogt Yuan, 2007), only one revealed an attenuated relationship between ethnic density and depression (and only for Black but not Hispanic individuals) when social support was included in the model. None of the studies of Hispanic ethnic density have provided evidence that increased social support explains the relationship between Hispanic density and depression. There are also mixed findings on the relation of ethnic density to social support. Across ethnic groups, five studies have indicated that ethnic density is positively associated with social support (Das-Munshi et al., 2010a; Halpern & Nazroo, 2000a; Mair et al., 2010b; Roh et al., 2011b; Syed & Juan, 2012), but three others reported no relation between ethnic density and social support.
In addition to the inconsistent findings discussed above, there are two gaps in the extant literature on ethnic density and depression. First, the beneficial effects of social support for health may be seen more clearly when social support serves as a buffer against life stress. Studies of community dwelling samples may contain individuals facing varying types and intensities of life stress. Consequently, they may face different needs for social support and receive different levels of benefit from any support they receive. Therefore, the present study focuses on the effects of ethnic density on depression in a sample of individuals all of whom are facing a critical life stressor, an episode of acute coronary syndrome (ACS). ACS is known to be depressogenic (Parker et al., 2008), and findings from Frasure-Smith and colleagues suggest that high levels of social support predicted improvements in depression symptoms over the first year post-ACS in individuals with depression (Frasure-Smith et al., 2000).
Second, ethnic density does not exist in a vacuum. The ability to receive or benefit from the social support of one's ethnic or racial group may depend on the degree to which the members of these groups have access to relevant economic and social resources. For some ethnic/racial groups, high ethnic density co-occurs with low economic resources (Bécares et al., 2013; Williams & Collins, 2001). In these cases, areas with high ethnic density may lack the social and economic capital that protects against negative mental health outcomes, as has been seen in studies of residential racial segregation (Dohrenwend, 1993; Schulz et al., 2006; Schulz et al., 2008; Warheit et al., 1979).
Studies that have attempted to disentangle the effects of ethnic density versus socioeconomic status on depression have not yielded a clear picture of the differential contribution of ethnic density to depression. Most studies (13/16) include a measure of socioeconomic status (SES; usually an individual level indicator of education) as a covariate in analyses of the relationship of ethnic density to depression. Of these studies, nine found that the relationship of ethnic density to depression was significant when education was included in the model (Das-Munshi et al., 2010a; Gerst et al., 2011a; Juang et al., 2006; Leu et al., 2011; Mair et al., 2010b; G V Ostir et al., 2003b; Stafford et al., 2011; Walters et al., 2008; Yuan et al., 2007); whereas four studies found the relationship was no longer significant (Henderson et al., 2005; Lee, 2009a; Roh et al., 2011b; Syed & Juan, 2012). Similarly, when various measures of neighborhood advantage (i.e., neighborhood income, space, household values, etc.) are controlled, most (Gerst et al., 2011a; Halpern & Nazroo, 2000a; Lee, 2009a; Mair et al., 2010b; Neeleman et al., 2001; G V Ostir et al., 2003b; Yuan et al., 2007) but not all studies (Henderson et al., 2005; Mair et al., 2010a; Yuan et al., 2007) have found that the relationship of ethnic density to depression remained significant for at least one ethnic subgroup. Two studies (Mair et al., 2010b; Vogt Yuan, 2007) report that the negative relationship of ethnic density to depressive symptoms disappears when measures of neighborhood advantage are controlled, whereas in a majority of the studies the relationship persists (Das-Munshi et al., 2010a; Gerst et al., 2011a; Halpern & Nazroo, 2000a; Mair et al., 2010b; Mintz & Schuartz, 1964; G V Ostir et al., 2003b; Vogt Yuan, 2007; Walters et al., 2008).
In New York City (NYC), areas with greater Hispanic density are also the areas with more foreign-born Hispanics (Karpati et al., 2004). Therefore, in areas with high Hispanic density, residents share not only ethnicity, but also the challenges associated with both discrimination and acculturation. Despite these challenges, foreign-born individuals are less likely to be depressed than US-born individuals (Alegria et al., 2007; Grant et al., 2004; Vega et al., 1998). Three of the 16 studies of ethnic density and depression examined nativity status as a moderator. The authors of these studies have concluded that ethnic density is associated with depression for US-born minority individuals, but not foreign-born individuals (Hwang et al., 2000a; Mair et al., 2010b; Stafford et al., 2011). However, none of these studies explicitly examine if nativity status influenced the role of social support as a mediator of the relationship of ethnic density to depression.
The overall aim of this study is to examine the effects of ethnic density on social support and depressive symptoms in individuals facing an acute life stressor, an episode of acute coronary syndrome (ACS). ACS is a condition known to be depressogenic and potentially responsive to social support. We examine the degree to which the effects of ethnic density on social support and depressive symptoms persist above and beyond the effects associated with individual and neighborhood socioeconomic conditions. We are specifically interested in understanding the degree to which the relationship of ethnic density to depressive symptoms is mediated by the social support conferred when living with similar others. Therefore, we examine the effects of Hispanic ethnic density on depressive symptoms in both Hispanic and non-Hispanic individuals. As those who are foreign-born may differ from those who are US-born in their need for the social benefits of ethnic density, we examine the moderating effects of nativity status on the relationship of ethnic density to social support and depressive symptoms.
METHODS
Individuals were enrolled in the Prescription Use, Lifestyle, Stress Evaluation (PULSE) study, an ongoing, single cohort, observational, prospective study of 1,087 individuals who presented to Columbia University Medical Center with ACS. Individuals were eligible for the parent PULSE study if they met criteria for ACS (either acute myocardial infarction with or without ST-segment elevation or unstable angina) as verified by study cardiologists. This analysis includes data from the first 500 individuals enrolled. Only individuals who completed the baseline depression assessment and whose census tracts were located using GIS (Geographic Information Software) were included in this substudy (n=472). The institutional review board approved the study, and patients provided written informed consent. The sample was on average 63 years old (standard deviation (SD): 11.17). Approximately one-third were women (34.3%, n = 162); 40% (n = 189) were foreign-born, and one-third self-identified as Hispanic (32.8%, n =155). Sixty percent (n = 285) of patients self-identified as non-Hispanic Whites and 19% as non-Hispanic Black (n = 90).
Hispanic ethnic density
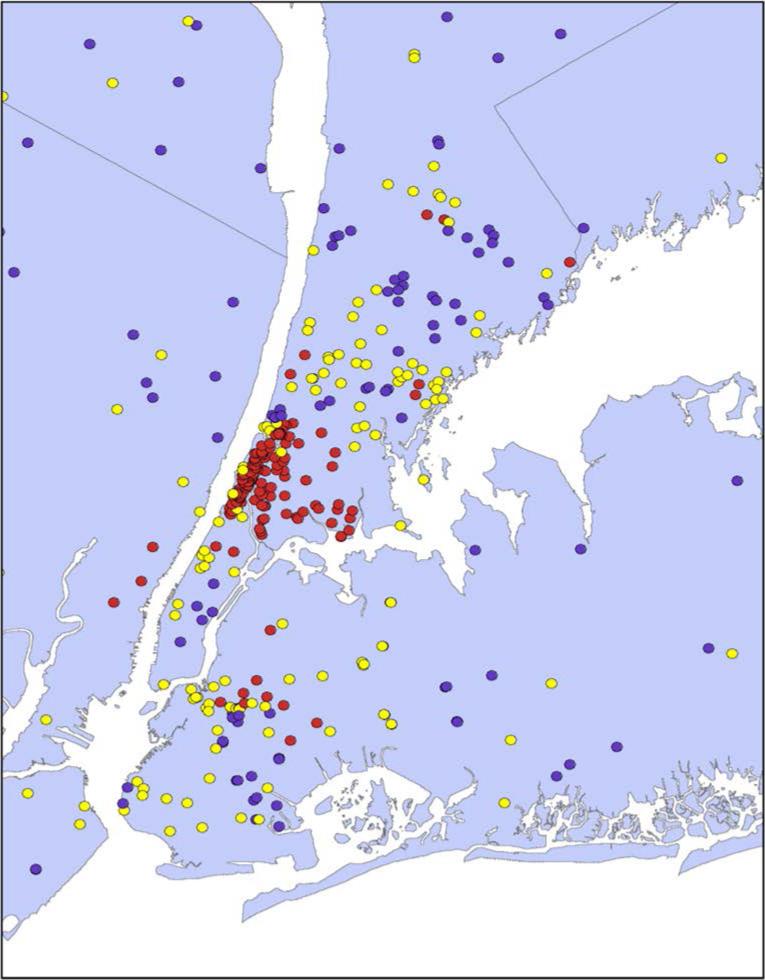
Individuals’ mailing addresses were ascertained during intake. Using GIS, each patient address was assigned a census tract (Figure 1). Density measures were extracted from Census American Community Survey 2005-2009 and matched to each patient-assigned census tract. Individuals were distributed across 363 census tracts. On average, each census tract is populated by 5800 people. Hispanic ethnic density was defined as the percentage of Hispanics living within each census tract.
Figure 1.
Demographic mapping of PULSE N = 472 Post-ACS individuals. Each dot represents 1 patient. Hispanic Density: Red = high; Yellow = moderate; Purple = low
Neighborhood Socioeconomic status
Percent female headed household was defined as the proportion of female-headed households, defined as the number of family households with a woman, related child under 18 years old, and no husband divided by the total number of households within that census tract. Data were extracted from the Census American Community Survey 2005-2009 Median household income was extracted from the 2000 US Census.
Individual Characteristics
Key demographic variables were assessed via interview during the patient's index hospitalization for ACS. Validated Spanish versions of the measures were used for Spanish-speaking individuals whenever possible; if no Spanish version was available, the measures were translated from English to Spanish and back-translated by three independent persons. Variables included patient-reported age, sex, race, and number of years of schooling completed. Patients also reported their nativity status (US-born or foreign-born).
Disease severity was calculated using the Charlson Comorbidity Index (an index of 22 medical conditions weighted by patient associated mortality risk) (Charlson et al., 1987).
Perceived social support was assessed using the ENRICHD Social Support Instrument (ESSI). Six items were used to assess tangible (e.g., Is there someone available to help you with daily chores?) and emotional social support (e.g, Is there someone available to you who you can count on to listen to you when you need to talk?), using a Likert scale from 1 (“none of the time”) to 5 (“all of the time”). These items are summed to create a total score, with higher scores indicating greater social support. Cronbach's alpha for the ESSI was .87.
Depression was assessed with the Beck Depression Inventory (BDI-I (Beck et al., 1961) and a total sum of the responses to all items was used as the continuous dependent measure. Cronbach's alpha for the BDI was .84.
Analytic Plan
All analyses were performed using SAS 9.2. The primary independent variable, Hispanic ethnic density, was treated as both a categorical (tertiles) and a continuous variable (percentage Hispanic within a given census tract). We report the continuous effects in the text of the paper, and display categorical results in the table. In every case, if the regression analyses of continuous variables were significant, the categorical results were significant as well. Both ethnic density and depression scores were positively skewed and consequently log transformed. All reported analyses reflect use of transformed variables. With one minor exception as noted in Table 3, there were no significant differences between analyses performed with log transformed versus untransformed measures.
Table 3.
Regression analyses testing Nativity status as a moderator of the relationship of Hispanic Density to Depression for the full group of Post-ACS individuals (N= 472).
| Unadjusted Models | Adjusted Model 1 (individual level factors) | Adjusted Model 2 (individual and neighborhood level factors) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | SE | Beta | R2 | B | SE | Beta | R2 | B | SE | Beta | R2 | |
| Full Sample | ||||||||||||
| † Hispanic Density to Depression | .10 | .03 | .15 | .02** | .09 | .04 | .14 | .01* | .05 | .05 | .08 | .002 |
| Full Sample with Interactions | ||||||||||||
| Nativity status | .33 | .22 | .20 | .005 | .23 | .21 | .14 | .002 | .22 | .21 | .14 | .002 |
| Hispanic Density | .18 | .04 | .27 | .04*** | .13 | .05 | .21 | .02* | .10 | .05 | .15 | .006 |
| Hispanic Density × Nativity status | −.15 | .07 | −.34 | .01* | −.14 | .07 | −.32 | .01* | −.14 | .07 | −.31 | .008* |
| Follow up Analysis | ||||||||||||
| US Born, (Hispanic Density to Depression) | .18 | .04 | .26 | .07** | .13 | .05 | .19 | .02** | .15 | .06 | .22 | .02* |
| Foreign Born, (Hispanic Density to Depression) | .03 | .06 | .03 | - | −.00 | .07 | .00 | - | −.09 | .09 | −.12 | .006 |
Adjusted Model 1 included age, gender, education, nativity status, Charlson disease severity, and Hispanic ethnicity. Adjusted R2 = 11.87%
Adjusted Model 2 included covariates in Model 1, log median household income, and proportion of female headed household. Adjusted R2 = 16.61%
Note with untransformed scores the unadjusted relationship of Hispanic density to depressive symptoms is significant, but the adjusted relationship is not significant in Model 1 or 2.
p < .05
p < .01
p < .001
Initial analyses examine the relationship of ethnic density to demographic variables (i.e., age, gender, race, and nativity status), as well as individual (e.g., education) and neighborhood (e.g., median income, percentage of female headed households) measures of socioeconomic resources.
As preliminary analyses revealed that ethnic density was related to individual sociodemographic variables and neighborhood socioeconomic variables, we create a series of models. To test our primary hypothesis, we examined the main effect of ethnic density on depression using both categorical and continuous measures of ethnic density in unadjusted (Model 1) and adjusted models (Models 2 and 3). In the partially-adjusted model (Model 2) covariates included age, gender, years of education, nativity status, Charlson Comorbidity Index, and Hispanic ethnicity. In the fully-adjusted model (Model 3), we added neighborhood sociodemographic variables to Model 2. We examined potential moderators of the association of ethnic density with depression by including cross-products of Hispanic ethnicity, socioeconomic status, and nativity status with ethnic density.
Next we examined contextual effects on social support by evaluating the relationship of individual and neighborhood sociodemographic variables to social support. To test the hypothesis that perceived social support is a pathway through which ethnic density is associated with depression, mediation analyses were performed using bootstrapping described by Preacher and Hayes (Preacher & Hayes, 2008). We calculate the confidence intervals using two methods designed to correct for potential bias (i.e., bias-corrected or bias-corrected and accelerated (BCA)). We further tested moderated mediation, hypothesizing that the role of individual- and neighborhood-level mediators of the relationship of Hispanic ethnic density to depression may differ by ethnicity (Hispanic versus Non-Hispanic), SES, and, nativity status (foreign-born versus US-born),
RESULTS
Demographic characteristics of the sample are presented in Table 1. Intercorrelations of individual- and neighborhood-level sociodemographic variables are presented in Table 2.
Table 1.
Demographic characteristics, perceived social support, self-reported depression, and neighborhood characteristics for the full sample and by Hispanic density, gender, and nativity status
| Hispanic Density |
Gender |
Nativity status |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Characteristics | Overall (N=472) | Low (n=160) | Moderate (n=155) | High (n=157) | p b | Male (n=310) | Female (n=162) | p c | US Born (n=277) | Foreign Born (n=189) | p c |
| Age, Mean (SD) | 63.5 (11.2) | 65.5 (10.5) | 63.8 (11.3) | 61.1 (11.4) | .002 | 62.8 (11.1) | 64.9 (11.3) | .71 | 64.5 (11.1) | 61.8 (11.0) | .01 |
| Female | 162 (34.3) | 49 (30.6) | 47 (30.3) | 66 (42.0) | .05 | - | - | - | 90 (32.5) | 71 (37.6) | .26 |
| Foreign born | 189 (40.0) | 29 (18.1) | 53 (34.2) | 107 (68.2) | <.001 | 118 (38.7) | 71 (43.8) | .26 | - | - | - |
| Hispanic | 155 (32.8) | 9 (5.6) | 29 (18.7) | 117 (74.5) | <.001 | 91 (29.4) | 64 (39.5) | .03 | 32 (11.6) | 123 (65.1) | <.001 |
| Black | 90 (19.1) | 20 (12.5) | 32 (20.6) | 38 (24.2) | .03 | 46 (14.8) | 44 (27.2) | <.001 | 46 (16.6) | 42 (22.2) | .13 |
| White | 285 (60.4) | 130 (81.3) | 94 (60.6) | 61 (38.9) | <.001 | 197 (63.5) | 88 (54.3) | .05 | 207 (74.7) | 75 (39.7) | <.001 |
| Years in school, Mean(SD) | 13.2 (4.2) | 15.3 (3.1) | 13.6 (3.9) | 10.7 (4.3) | <.001 | 13.8 (4.3) | 12.1 (3.8) | .03 | 14.6 (3.5) | 11.2 (4.4) | <.001 |
| Beck Depression Inventory, Mean(SD) | 9.2 (7.2) | 7.3 (5.4) | 9.5 (6.7) | 11.0 (8.8) | <.001 | 7.5 (5.7) | 12.7 (8.6) | <.001 | 8.9 (6.7) | 9.7 (8.1) | .26 |
| Perceived Social Support, Mean(SD) | 26.3 (4.9) | 27.0 (4.6) | 26.3 (4.3) | 25.5 (5.5) | .02 | 26.7 (4.8) | 25.5 (4.9) | .02 | 26.5 (4.7) | 25.9 (5.1) | .20 |
| Disease Severity, Mean (SD) | 1.7 (1.6) | 1.5 (1.5) | 1.8 (1.6) | 1.8 (1.8) | .16 | 1.4 (1.5) | 2.1 (1.8) | .08 | 1.7 (1.6) | 1.7 (1.7) | .99 |
| Median Household Income, Mean (SD) | $43,314 (27,802) | $61,844 (34,549) | $39,302 (19,623) | $28,390 (12,033) | <.001 | $45,767 (29,981) | $38,620 (22,415) | <.001 | $48,364 (30,564) | $35,847 (21,479) | <.001 |
| Proportion of Female-Headed Households, Mean(SD) | 10.5 (8.6) | 4.8 (4.9) | 7.7 (7.0) | 19.1 (6.1) | <.001 | 9.6 (8.4) | 12.2 (8.8) | .05 | 7.6 (7.5) | 14.6 (8.5) | <.001 |
Hispanic density tertiles are defined as: Low Hispanic ethnic density < 7.2% Hispanic, Moderate Hispanic ethnic density 7.2% > 32.2% Hispanic, and High Hispanic ethnic density > 32.2%)
Data are given as number (percentage) of study patients unless otherwise indicated
p-values are based on the analysis of variance for continuous measures
p-values are based on the x2 test for categorical measures
Table 2.
Interrelations among neighborhood and individual level sociodemographic factors and depression
| Education Level |
Disease Severity |
Perceived Social Support |
Log Median Income |
Log Female Headed Household |
Log Percent Hispanic Density |
Log Depression Severity |
|
|---|---|---|---|---|---|---|---|
| Age | −.01 | .13** | .05 | .15** | −.20** | −.17** | −.06 |
| Education Level | −.12** | .04 | .27** | −.52** | −.48** | −.13** | |
| Disease Severity | .02 | −.05 | .13** | .06 | .17** | ||
| Perceived Social Support | .03 | −.07 | −.12* | −.21*** | |||
| Log Median Income | −.48** | −.50** | −.15** | ||||
| Log Female Headed Household | .72** | .18*** | |||||
| Log Percent Hispanic Density | .15** |
p < .05
p < .01
p < .001
Ethnic density in context: Demographic differences
Census tracts ranged between less than 1% Hispanic to 91% Hispanic. Most of the Hispanic individuals in the study lived in areas in which there were high concentrations of Hispanics (75% lived in high density areas), 19% lived in areas with moderate concentrations of Hispanics, and 6% lived in areas with low concentrations of Hispanic (less than 7%) (χ2 = 191.44, df = 2, p = < .001). Put another way: among Hispanics, 67% lived in areas in which 50% or more of the residents were also Hispanic.
The residents of high density areas differ from those in low and moderate density areas in gender (χ2 = 6.22, df = 2, p = .045), nativity status (χ2 = 83.77, df = 2, p < .001) and education level (F (2,461) = 58.57, p < .001). In this sample, women (vs. men) and foreign-born (vs. US-born) were more likely to live in areas of high Hispanic density versus moderate or low density areas. Education levels also varied by amount of Hispanic density, with high density areas housing individuals with lower mean levels of education than moderate and low density areas.
Ethnic density in context: Socioeconomic effects
Hispanic density was negatively associated with individual and neighborhood measures of SES. In regression analyses, median income predicted about 15% of the variance in Hispanic density (β = -43.23, SE = 4.74, p < .001). The proportion of female-headed households shared about 52% of the variance with ethnic density (p <.001). Differences in income and percent female-headed household by ethnic density category are shown in Table 1.
Individual and neighborhood sociodemographic variations in depression
As shown in Table 1, women had significantly higher levels of depressive symptoms than did men, and those who were Hispanic had significantly higher levels of depressive symptoms than those who were not (p < .001). Education was significantly negatively related to depressive symptoms. Illness severity as assessed by the Charlson Comorbidity Index was positively related to depressive symptoms. Neighborhood factors were also associated with depressive symptoms (see Table 2). Both median income and proportion female headed households served as predictors of depressive symptoms, and together they accounted for about 5% of the variance in depressive symptoms (p < .001).
Main effects of ethnic density on depression: unadjusted and adjusted analyses
In unadjusted analyses, Hispanic ethnic density was positively associated with depressive symptoms (β = .10, SE = .03, p = .001). After adjusting for individual level characteristics, including age, gender, education, nativity status, charlson comorbidity index, and Hispanic ethnicity, the relationship of ethnic density to depressive symptoms remained significant (β = .09, SE = .04, p = .03). However, when we controlled for neighborhood characteristics as well as individual characteristics, the effects of Hispanic density on depressive symptoms were no longer significant (β = .05, SE = .05, p = .30).
Test of potential moderators: Ethnicity, individual and neighborhood SES, and nativity status
Ethnicity
There was no significant interaction between Hispanic ethnic density and ethnicity both with (p > .20) and without (p > .33) adjustment for individual and/or neighborhood characteristics. Hispanic individuals were more depressed than non-Hispanic individuals irrespective of the ethnic density of their neighborhood.
Socioeconomic status
In adjusted models, there was a significant interaction of Hispanic density with individual-level education (p < .05) but these effects were no longer significant controlling for individual and neighborhood level covariates. The interaction of Hispanic density with neighborhood income and percent female-headed household on depression was not significant when the models were adjusted for all other individual and neighborhood covariates (all p's > .12).
Nativity status
The interaction of nativity status and Hispanic density on depressive symptoms was significant and remained so after adjustment for both individual and neighborhood variables (Model 2, p = .02; Model 3, p = .04. See Table 3). Follow-up regression analyses conducted separately by nativity status showed a significant positive relationship between Hispanic density and depressive symptoms for US-born individuals only (p <.001). The effect for US-born individuals remained significant when controlling for individual and neighborhood sociodemographic variables (Model 2, p < .05; Model 3, p < .05). Neither the unadjusted nor adjusted relationships of Hispanic density to depressive symptoms were significant for foreign-born individuals (p > .24).
Does social support mediate the relationship of Hispanic ethnic density to depression?
As shown in Table 2, ethnic density was negatively related to social support, and social support was negatively related to depressive symptoms. However, social support was unrelated to either individual or neighborhood measures of SES.
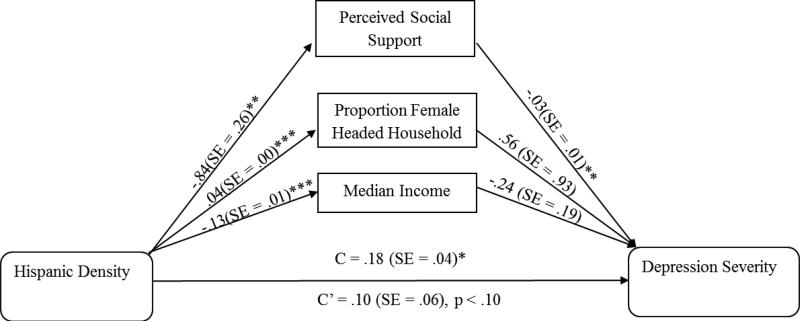
We could not examine social support as a mediator in the full sample because ethnic density was not a significant predictor of depressive symptoms once covariates were included in the analysis. However, the effects of ethnic density to depressive symptoms remained significant for US-born individuals, even when controlling for all individual and neighborhood level covariates. Therefore, to determine if social support mediates the relationship of ethnic density to depressive symptoms in US-born individuals above and beyond the mediating effects of neighborhood level socioeconomic status, we used bootstrapping methods, as recommended by Preacher & Hayes (Preacher & Hayes, 2008). The analyses controlled for all individual level covariates. Mediation analysis revealed that Hispanic density was negatively related to both perceived social support and median income and positively related to proportion of female-headed households (Figure 2). Of the total variance in depressive symptoms explained in the fully-adjusted model, the multiple mediators (neighborhood income, female headed households and social support) accounted for 43.94% of the variance. Perceived social support was the only mediator significantly related to depressive symptoms (BCA 95% CI: .01, .05). The total effect of ethnic density on depressive symptoms was significant (β = .18, SE = .04, p = .01). However, this effect was no longer significant (β = .10, SE = .06, p < .10) with social support included in the model. When all covariates were in the model, social support, alone, accounted for 13% of the variance between Hispanic density and depressive symptoms.
Figure 2.
US born ACS Patients. Model testing perceived social support, neighborhood income and female-headed household as mediators of the association between Hispanic density to Depressive symptoms. The number provided for each path is regression coefficients and standard errors derived from a bootstrap procedure.
DISCUSSION
Although prior literature has, in general, found a negative relationship between ethnic density and depression, research has not confirmed the importance of social support as a mediator. In fact, ethnic density itself is not uniformly associated with increased social support (Henderson et al., 2005; Leu et al., 2011). We hypothesized that the failure to document the role of social support as a mediator of the relationship of ethnic density to depression could be a function of the demands facing the participant sample, affecting their need for social support. To date, no prior studies have specifically examined the effects of ethnic density in a sample of individuals who are facing an acute, depressogenic stressor, and who therefore might be particularly in need of increased support. We examined these relationships in a sample of individuals all of whom had recently been hospitalized for an ACS event, a salient stressor known to be depressogenic. Within this sample, we examined the effects of ethnic density on depressive symptoms, examining the potential mediating role of social support. In addition, we investigated the degree to which the effects of ethnic density on support and depressive symptoms might vary depending on other social and economic characteristics associated with ethnic density.
In contrast to much of the literature (Das-Munshi et al., 2010a; Gerst et al., 2011a; Halpern & Nazroo, 2000a; Hwang et al., 2000a; Leu et al., 2011; Mair et al., 2010b; Mintz & Schuartz, 1964; Neeleman et al., 2001; G V Ostir et al., 2003b; Pickett et al., 2009), our findings indicate that neighborhood levels of Hispanic ethnic density were positively associated with depressive symptoms. Individuals who lived in high Hispanic density neighborhoods had depression scores more than three points higher than those in low density neighborhoods, a difference likely to have clinical relevance (Davidson et al., 2013). The effects were consistent for Hispanic and non-Hispanic individuals.
It may be that the potential benefits associated with ethnic density depend on the socioeconomic and demographic context in which the participants lived. In this sample, individuals who lived in areas of high ethnic density were more likely to be foreign-born, to be women, and to have lower levels of education. Nativity status, greater family responsibilities, and limited education can all present barriers to economic achievement.
Ethnic density was also negatively associated with neighborhood socioeconomic resources. Across the sample as whole, the association of ethnic density to depression was fully accounted for by neighborhood level SES (i.e., median income and proportion female headed household). These findings suggest that in our sample, ethnic density co-occurs with a range of other individual- and neighborhood-level characteristics that may add to the overall stress burden facing the participants. The limited economic resources may mitigate the ability of ethnic density alone to buffer the effects of stress on depression. These findings are consistent with those of LaVeist et al (LaVeist, 2011) who argues that the sociodemographic characteristics of a neighborhood (i.e., place) may be more important than the individual's race in contributing to health disparities.
Consistent with much previous literature (Das-Munshi et al., 2010a; Halpern & Nazroo, 2000a; Hwang et al., 2000a; Roh et al., 2011b; Syed & Juan, 2012), we found that social support was not a significant mediator of the relationship of ethnic density to depression for the sample as a whole. But the effects of ethnic density on social support and depression were not the same for all subgroups within the sample. Prior literature suggested that nativity status might moderate the effects of ethnic density on depression (Hwang et al., 2000a; Mair et al., 2010b; Stafford et al., 2011), with protective effects seen more clearly among foreign-born individuals. We found a significant interaction of nativity status and ethnic density, even when controlling for all individual- and neighborhood-level sociodemographic characteristics. Hispanic density was positively related to depressive symptoms for those who were US-born, but not for those who were foreign-born. This finding suggests that ethnic density may be related to mental health through different pathways for US-born vs. foreign-born individuals. In support of this notion, tests of mediation revealed that social support, but not SES, mediated the relationship of ethnic density to depressive symptoms in US-born individuals. For those who were US-born, ethnic density was negatively associated with social support. There was no relationship of ethnic density to social support or depressive symptoms for foreign-born individuals.
Our findings on the relationship of ethnic density to depressive symptoms among US-born individuals are consistent with the overall literature on the relationship of racial residential segregation to mental health among African American samples (Acevedo-Garcia, 2000; Lester, 2000; Peterson & Krivo, 1999). Residential racial segregation (RRS) shares some common conceptual characteristics with ethnic density, as RRS is sometimes quantified as the proportion of Black Americans residing in a neighborhood (Kramer & Hogue, 2009). RRS has been associated with higher levels of a variety of mental health complaints (Dohrenwend, 1993; Schulz et al., 2006; Schulz et al., 2008; Warheit et al., 1979). At least a portion of the health effects associated with RRS are likely to be a function of the level of socioeconomic disadvantage which co-occurs with segregation for some minority groups.
For US-born individuals, there may be a bidirectional relationship between density and depression. Depression may be a barrier to movement to more advantaged areas; those with higher levels of depression may not have the motivational or financial resources to leave more dense and disadvantaged areas (Ludwig et al., 2012). This barrier may be a particular problem for those with concomitant medical illness, such as ACS. On the other hand, for foreign-born Hispanic individuals, the problem may be more complex. In this case, the social capital available in neighborhoods high in ethnic density may partly compensate for the low levels of socioeconomic resources. In future studies of the relationship of ethnic density to health, it may be important to examine the degree to which individuals choose to live in areas of high ethnic density or believe they face significant barriers to residential mobility.
In the presence of a significant stressor such as an acute medical illness, the hardships associated with living in impoverished neighborhoods may undermine the ability to develop or benefit from supportive relationships (Brondolo et al., 2012). This hypothesis is consistent with data suggesting that social support does not reliably buffer individuals from the depressogenic effects of race-related stress (Brondolo et al., 2009). The presence of high levels of stress may actually erode social relationships (Broudy et al., 2007). Structural interventions to support the development of social and economic capital in high stress communities may thus be required.
Limitations
This study featured a single-site, cross-sectional design, and participants were primarily from northern Manhattan and the South Bronx, areas which have high levels of Hispanic ethnic density. Yet, there are clusters of moderate Hispanic density and low Hispanic density clusters all throughout the tri-state region. This patient population represents individuals who came to Columbia University Medical Center (CUMC). Individuals not treated at CUMC may have different social and demographic resources (e.g., travelling resources). This study was unable to evaluate concordant and discordant ethnicity matches due to sample size (i.e. stratified analysis of Hispanics within high, moderate, and low Hispanic density neighborhoods compared to Non-Hispanics within high, moderate, and low Hispanic density neighborhoods). However, the influences of neighborhood-level effects on mental health outcomes, above individual- level demographics were clear. Similarly, our sample sizes for other ethnic groups were too small for analyses and our focus on differences between Hispanic and non-Hispanic individuals did not allow us to conduct more fine-grained analyses within the non-Hispanic group.
Future research should consider whether depression is a barrier to residential mobility (i.e., leaving impoverished areas) or if depression is exacerbated by the social and financial strains presented by living in areas with high levels of ethnic density. Social support may not be the primary mediator of ethnic density to depression, and we did not assess other psychosocial variables including discrimination, acculturative stress or neighborhood cohesion that may mediate the density-depression association.
We chose as a stressor the presence of ACS. We do not know if the same effects will emerge among samples facing other medical or non-medical stressors. However, ACS individuals are at risk for depression and depression outcomes are associated with increased risk of subsequent morbidity and/or mortality among individuals with ACS (Barth et al., 2004; Carney & Freedland, 2003; Kronish et al., 2009; van Melle et al., 2004). Therefore, given the importance of depression for ACS outcomes, we consider it important for public health planning to understand the degree to which neighborhood contextual factors serve to increase the public health burden.
Despite the limitations, this study is the first to examine effects of ethnic density considering its role as a potential buffer of effects of a medical stressor (ACS) on depression. The results suggest that Hispanic ethnic density does not operate in a vacuum, independent of other social processes. The findings suggest that there are complex interrelations between ethnic density and socioeconomic and social resources that have implications for mental health. A substantial stress burden or restricted local economic and social resources may undermine the psychosocial benefits of ethnic density.
Acknowledgments
Source of Funding: This work was supported by grants HL088117-02S1 from the National Heart, Lung, and Blood Institute (NHLBI) of the National Institutes of Health (NIH), Bethesda, MD., USA; and by an unrestricted research grant from the Hinduja Foundation, New York, NY. Dr. Shaffer is supported by grants 12CRP8870004 from the American Heart Association and K23-HL112850 from NHLBI/NIH. Dr. Alcantara is supported by grant 3R01HL115941-01S1 from NHLBI/NIH.
Footnotes
Conflicts of Interest: None reported.
References
- Acevedo-Garcia D. Residential segregation and the epidemiology of infectious diseases. Social Science & Medicine. 2000;51:1143–1161. doi: 10.1016/s0277-9536(00)00016-2. [DOI] [PubMed] [Google Scholar]
- Alegria M, Mulvaney-Day N, Torres M, Polo A, Cao Z, Canino G. Prevalence of psychiatric disorders across Latino subgroups in the United States. American Journal of Public Health. 2007;97:68–75. doi: 10.2105/AJPH.2006.087205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barth J, Schumacher M, Herrmann-Lingen C. Depression as a risk factor for mortality in patients with coronary heart disease: a meta-analysis. Psychosomatic Medicine. 2004;66:802–813. doi: 10.1097/01.psy.0000146332.53619.b2. [DOI] [PubMed] [Google Scholar]
- Bécares L, Cormack D, Harris R. Ethnic density and area deprivation: neighbourhood effects on Māori health and racial discrimination in Aotearoa/New Zealand. Social Science & Medicine. 2013 Apr 13; doi: 10.1016/j.socscimed.2013.04.007. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Brondolo E, Gallo LC, Myers HF. Race, racism and health: disparities, mechanisms, and interventions. Journal of Behavioral Medicine. 2009;32:1–8. doi: 10.1007/s10865-008-9190-3. [DOI] [PubMed] [Google Scholar]
- Brondolo E, Libretti M, Rivera L, Walsemann KM. Racism and social capital: The implications for social and physical well-being. Journal of Social Issues. 2012;68:358–384. [Google Scholar]
- Broudy R, Brondolo E, Coakley V, Brady N, Cassells A, Tobin JN, et al. Perceived ethnic discrimination in relation to daily moods and negative social interactions. Journal of Behavioral Medicine. 2007;30:31–43. doi: 10.1007/s10865-006-9081-4. [DOI] [PubMed] [Google Scholar]
- Carney RM, Freedland KE. Depression, mortality, and medical morbidity in patients with coronary heart disease. Biological Psychiatry. 2003;54:241–247. doi: 10.1016/s0006-3223(03)00111-2. [DOI] [PubMed] [Google Scholar]
- Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. Journal of Chronic Diseases. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- Das-Munshi J, Becares L, Dewey ME, Stansfeld SA, Prince MJ. Understanding the effect of ethnic density on mental health: multi-level investigation of survey data from England. British Medical Journal. 2010;341:c5367. doi: 10.1136/bmj.c5367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson KW, Bigger JT, Burg MM, Carney RM, Chaplin WF, Czajkowski S, et al. Centralized, Stepped, Patient Preference-Based Treatment for Patients With Post-Acute Coronary Syndrome Depression: CODIACS Vanguard Randomized Controlled Trial. JAMA Internal Medicine. 2013 Mar 7;:1–8. doi: 10.1001/jamainternmed.2013.915. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diez Roux AV, Mair C. Neighborhoods and health. Annals of the New York Academy of Sciences. 2010;1186:125–145. doi: 10.1111/j.1749-6632.2009.05333.x. [DOI] [PubMed] [Google Scholar]
- Dohrenwend BP. Socioeconomic status and psychiatric disorders: an update on the social causation - social selection issue. Epidemiology & Psychiatric Sciences. 1993;2:71–74. [Google Scholar]
- Frasure-Smith N, Lesperance F, Gravel G, Masson A, Juneau M, Talajic M, et al. Social support, depression, and mortality during the first year after myocardial infarction. Circulation. 2000;101:1919–1924. doi: 10.1161/01.cir.101.16.1919. [DOI] [PubMed] [Google Scholar]
- Gerst K, Miranda PY, Eschbach K, Sheffield KM, Peek MK, Markides KS. Protective neighborhoods: neighborhood proportion of Mexican Americans and depressive symptoms in very old Mexican Americans. Journal of the American Geriatrics Society. 2011;59:353–358. doi: 10.1111/j.1532-5415.2010.03244.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Hasin DS, Dawson DA, Chou SP, Anderson K. Immigration and lifetime prevalence of DSM-IV psychiatric disorders among Mexican Americans and non-Hispanic whites in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry. 2004;61:1226–1233. doi: 10.1001/archpsyc.61.12.1226. [DOI] [PubMed] [Google Scholar]
- Halpern D, Nazroo J. The ethnic density effect: results from a national community survey of England and Wales. International Journal of Social Psychiatry. 2000;46:34–46. doi: 10.1177/002076400004600105. [DOI] [PubMed] [Google Scholar]
- Henderson C, Diez Roux AV, Jacobs DR, Jr., Kiefe CI, West D, Williams DR. Neighbourhood characteristics, individual level socioeconomic factors, and depressive symptoms in young adults: the CARDIA study. Journal of Epidemiology & Community Health. 2005;59:322–328. doi: 10.1136/jech.2003.018846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hwang WC, Myers HF, Takeuchi DT. Psychosocial predictors of first-onset depression in Chinese Americans. Social Psychiatry & Psychiatric Epidemiology. 2000;35:133–145. doi: 10.1007/s001270050196. [DOI] [PubMed] [Google Scholar]
- Juang LP, Nguyen HH, Lin Y. The Ethnic Identity, Other-Group Attitudes, and Psychosocial Functioning of Asian American Emerging Adults From Two Contexts. Journal of Adolescent Research. 2006;21:542–568. [Google Scholar]
- Karpati A, Kerker B, Mostashari F, Singh T, Hajat A, Thorpe L, et al. Health Disparities in New York City. New York, NY.: 2004. p. 32. [Google Scholar]
- Kramer MR, Hogue CR. Is segregation bad for your health? Epidemiology Review. 2009;31:178–194. doi: 10.1093/epirev/mxp001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kronish IM, Rieckmann N, Schwartz JE, Schwartz DR, Davidson KW. Is depression after an acute coronary syndrome simply a marker of known prognostic factors for mortality? Psychosomatic Medicine. 2009;71:697–703. doi: 10.1097/PSY.0b013e3181ad2abd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee MA. Neighborhood residential segregation and mental health: a multilevel analysis on Hispanic Americans in Chicago. Social Science & Medicine. 2009;68:1975–1984. doi: 10.1016/j.socscimed.2009.02.040. [DOI] [PubMed] [Google Scholar]
- Lester D. Does residential segregation in cities predict African-American suicide rates? Perceptual & Motor Skills. 2000;91:870. doi: 10.2466/pms.2000.91.3.870. [DOI] [PubMed] [Google Scholar]
- Leu J, Walton E, Takeuchi D. Contextualizing acculturation: gender, family, and community reception influences on Asian immigrant mental health. American Journal of Community Psychology. 2011;48:168–180. doi: 10.1007/s10464-010-9360-7. [DOI] [PubMed] [Google Scholar]
- Ludwig J, Duncan GJ, Gennetian LA, Katz LF, Kessler RC, Kling JR, et al. Neighborhood effects on the long-term well-being of low-income adults. Science. 2012;337:1505–1510. doi: 10.1126/science.1224648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mair C, Diez Roux AV, Osypuk TL, Rapp SR, Seeman T, Watson KE. Is neighborhood racial/ethnic composition associated with depressive symptoms? The multi-ethnic study of atherosclerosis. Social Science & Medicine. 2010;71:541–550. doi: 10.1016/j.socscimed.2010.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mintz NL, Schuartz DT. Urban Ecology and Psychosis: Community Factors in the Incidence of Schizophrenia and Manic-Depression among Italians in Greater Boston. International Journal of Social Psychiatry. 1964;10:101–117. doi: 10.1177/002076406401000202. [DOI] [PubMed] [Google Scholar]
- Neeleman J, Wilson-Jones C, Wessely S. Ethnic density and deliberate self harm; a small area study in south east London. Journal of Epidemiology & Community Health. 2001;55:85–90. doi: 10.1136/jech.55.2.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ostir GV, Eschbach K, Markides KS, Goodwin JS. Neighbourhood composition and depressive symptoms among older Mexican Americans. Journal of Epidemiology & Community Health. 2003;57:987–992. doi: 10.1136/jech.57.12.987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker GB, Hilton TM, Walsh WF, Owen CA, Heruc GA, Olley A, et al. Timing Is Everything: The Onset of Depression and Acute Coronary Syndrome Outcome. Biological Psychiatry. 2008;64:660–666. doi: 10.1016/j.biopsych.2008.05.021. [DOI] [PubMed] [Google Scholar]
- Peterson RD, Krivo LJ. Racial Segregation, the Concentration of Disadvantage, and Black and White Homicide Victimization. Sociological Forum. 1999;14:465–493. [Google Scholar]
- Pickett KE, Shaw RJ, Atkin K, Kiernan KE, Wilkinson RG. Ethnic density effects on maternal and infant health in the Millennium Cohort Study. Social Science & Medicine. 2009;69:1476–1483. doi: 10.1016/j.socscimed.2009.08.031. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavioral Research Methods. 2008;40:879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Roh S, Jang Y, Chiriboga DA, Kwag KH, Cho S, Bernstein K. Perceived neighborhood environment affecting physical and mental health: a study with Korean American older adults in New York City. Journal of Immigrant & Minority Health. 2011;13:1005–1012. doi: 10.1007/s10903-011-9492-3. [DOI] [PubMed] [Google Scholar]
- Schulz AJ, Gravlee CC, Williams DR, Israel BA, Mentz G, Rowe Z. Discrimination, symptoms of depression, and self-rated health among african american women in detroit: results from a longitudinal analysis. American Journal of Public Health. 2006;96:1265–1270. doi: 10.2105/AJPH.2005.064543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz AJ, Zenk SN, Israel BA, Mentz G, Stokes C, Galea S. Do neighborhood economic characteristics, racial composition, and residential stability predict perceptions of stress associated with the physical and social environment? Findings from a multilevel analysis in Detroit. Journal of Urban Health. 2008;85:642–661. doi: 10.1007/s11524-008-9288-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stafford M, Newbold BK, Ross NA. Psychological distress among immigrants and visible minorities in Canada: a contextual analysis. International Journal of Social Psychiatry. 2011;57:428–441. doi: 10.1177/0020764010365407. [DOI] [PubMed] [Google Scholar]
- Syed M, Juan MJD. Discrimination and psychological distress: Examining the moderating role of social context in a nationally representative sample of Asian American adults. Asian American Journal of Psychology. 2012;3:104–120. [Google Scholar]
- van Melle JP, de Jonge P, Spijkerman TA, Tijssen JG, Ormel J, van Veldhuisen DJ, et al. Prognostic association of depression following myocardial infarction with mortality and cardiovascular events: a meta-analysis. Psychosomatic Medicine. 2004;66:814–822. doi: 10.1097/01.psy.0000146294.82810.9c. [DOI] [PubMed] [Google Scholar]
- Vega WA, Kolody B, Aguilar-Gaxiola S, Alderete E, Catalano R, Caraveo-Anduaga J. Lifetime prevalence of DSM-III-R psychiatric disorders among urban and rural Mexican Americans in California. Archives of General Psychiatry. 1998;55:771–778. doi: 10.1001/archpsyc.55.9.771. [DOI] [PubMed] [Google Scholar]
- Vogt Yuan AS. Racial Composition of Neighborhood and Emotional Well-being. Sociological Spectrum. 2007;28:105–129. [Google Scholar]
- Walters P, Ashworth M, Tylee A. Ethnic density, physical illness, social deprivation and antidepressant prescribing in primary care: ecological study. British Journal of Psychiatry. 2008;193:235–239. doi: 10.1192/bjp.bp.107.038299. [DOI] [PubMed] [Google Scholar]
- Warheit GJ, Holzer CE, 3rd, Robbins L. Social indicators and mental health planning: an empirical case study. Community Mental Health Journal. 1979;15:94–103. doi: 10.1007/BF00757331. [DOI] [PubMed] [Google Scholar]
- Williams DR, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Reports. 2001;116:404–416. doi: 10.1093/phr/116.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie J, Wu EQ, Zheng ZJ, Sullivan PW, Zhan L, Labarthe DR. Patient-reported health status in coronary heart disease in the United States: age, sex, racial, and ethnic differences. Circulation. 2008;118:491–497. doi: 10.1161/CIRCULATIONAHA.107.752006. [DOI] [PubMed] [Google Scholar]
- Yuan S, Kerr G, Salmon K, Speedy P, Freeman R. Evaluating a community-based dental registration program for preschool children living in areas of high social deprivation. European Archives of Paediatric Dentistry. 2007;8:55–61. doi: 10.1007/BF03262571. [DOI] [PubMed] [Google Scholar]