Increasing obesity rates in Swiss HIV+ persons may partially be due to aging, demographic changes and earlier ART start. Most BMI increase occurred in year 1 of ART. The effect of individual ART regimens was limited.
Keywords: antiretroviral therapy, body mass index, HIV infection, immunosuppression, longitudinal study, obesity
Abstract
Background
The factors that contribute to increasing obesity rates in human immunodeficiency virus (HIV)-positive persons and to body mass index (BMI) increase that typically occurs after starting antiretroviral therapy (ART) are incompletely characterized.
Methods
We describe BMI trends in the entire Swiss HIV Cohort Study (SHCS) population and investigate the effects of demographics, HIV-related factors, and ART on BMI change in participants with data available before and 4 years after first starting ART.
Results
In the SHCS, overweight/obesity prevalence increased from 13% in 1990 (n = 1641) to 38% in 2012 (n = 8150). In the participants starting ART (n = 1601), mean BMI increase was 0.92 kg/m2 per year (95% confidence interval, .83–1.0) during year 0–1 and 0.31 kg/m2 per year (0.29–0.34) during years 1–4. In multivariable analyses, annualized BMI change during year 0–1 was associated with older age (0.15 [0.06–0.24] kg/m2) and CD4 nadir <199 cells/µL compared to nadir >350 (P < .001). Annualized BMI change during years 1–4 was associated with CD4 nadir <100 cells/µL compared to nadir >350 (P = .001) and black compared to white ethnicity (0.28 [0.16–0.37] kg/m2). Individual ART combinations differed little in their contribution to BMI change.
Conclusions
Increasing obesity rates in the SHCS over time occurred at the same time as aging of the SHCS population, demographic changes, earlier ART start, and increasingly widespread ART coverage. Body mass index increase after ART start was typically biphasic, the BMI increase in year 0–1 being as large as the increase in years 1–4 combined. The effect of ART regimen on BMI change was limited.
Obesity is a major long-term concern in human immunodeficiency virus (HIV)-positive (HIV+) persons given their increased cardiovascular risk [1], and the pathogenic link of obesity to diabetes mellitus, cardiovascular disease [2, 3], and all-cause mortality [4]. Soon after the introduction of antiretroviral treatment (ART), regional body fat distribution abnormalities became important metabolic concerns [5, 6]. With the use of the thymidine-analogs zidovudine and stavudine essentially disappearing in Western countries, lipoatrophy [7] has been receiving less attention and concern has shifted towards lipohypertrophy and obesity. Obesity is now increasingly recognized as a problem in HIV+ persons, and it has been attributed to improved health due to effective ART, normal aging, and obesity trends similar to those seen in the general population [8–17]. However, large-scale, longitudinal analyses are not available.
In this study, we describe obesity trends and concurrent demographic changes from 1990 to 2012 in the nationally representative Swiss HIV Cohort Study (SHCS), which currently follows more than 8000 active patients [18]. We also investigate the contribution of demographics, HIV-related factors, and the most commonly used ART combinations to body mass index (BMI) change after 1 and 4 years of ART in 1601 participants who started a first ART regimen after January 1, 1998. This study represents the most comprehensive longitudinal BMI analysis undertaken in HIV+ persons.
METHODS
Study Participants
Participants included HIV+ persons, aged ≥16 years who were followed in the SHCS (www.shcs.ch) [18]. The study was approved by local ethics committees. All participants provided written informed consent.
We present 2 main types of analyses: first, a population-based descriptive analysis of all SHCS patients with at least 1 available BMI from 1990 to 2012 (Figure 1; Supplementary Figure 1; Supplementary Table 1); second, detailed analyses of BMI changes from 0–1 and 1–4 years after starting ART in participants initiating a first ART regimen after January 1, 1998 (Tables 1 and 2; Supplementary Tables 2 and 3; Supplementary Figure 2). To limit confounding, pregnant females and patients with incident cancer or acquired immune deficiency syndrome (AIDS)-defining events after ART start were excluded. We also excluded participants with missing CD4 (+120/−30 days at ART start) or BMI information (+120/−120 days at ART start and at 1 and 4 years thereafter), those with ≥62 days of ART interruption, and injection drug users (IDUs), due to low numbers, increased rates of dropout, and missing data. A common reason for missing BMI information was ART initiation before SHCS enrollment.
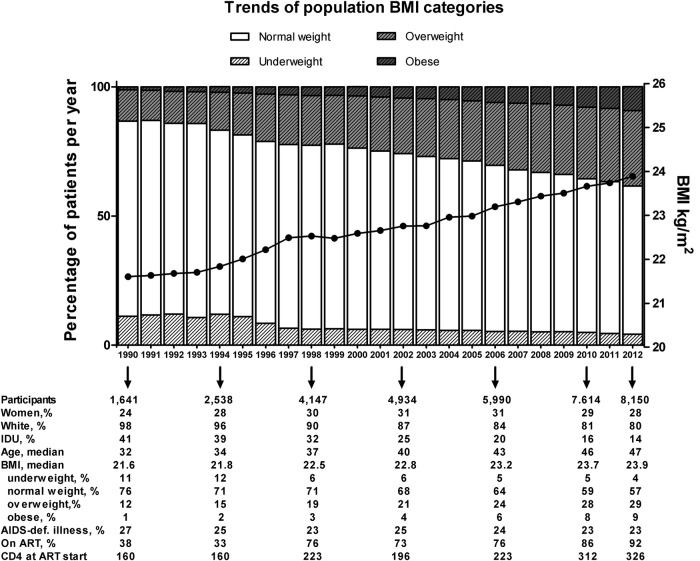
Fig. 1.
Longitudinal trends of population body mass index (BMI) categories and median BMI trajectory, entire Swiss HIV Cohort Study population, 1990–2012. Note: Confidence intervals are omitted for visual clarity. Abbreviations: AIDS, acquired immune deficiency syndrome; IDU, injection drug user; ART, antiretroviral therapy.
Table 1.
Baseline Characteristics of 1601 SHCS Participants Who Started a First ART Regimen After January 1, 1998
| All | MSM* | Heterosexual male | Heterosexual female | P-value* | |
|---|---|---|---|---|---|
| Participants, n (%) | 1601 (100) | 892 (56) | 390 (24) | 319 (10) | |
| Age, median years (IQR) | 40 (34–47) | 40 (34–45) | 44 (36–53) | 37 (32–45) | <0.001 |
| Ethnicity | |||||
| White, n (%) | 1280 (80) | 808 (91) | 315 (81) | 157 (49) | <0.001 |
| Black, n (%) | 181 (11) | 10 (1) | 65 (17) | 106 (33) | |
| Asian, n (%) | 83 (5) | 38 (4) | 4 (1) | 41 (13) | |
| Other, n (%) | 57 (4) | 36 (4) | 6 (2) | 15 (5) | |
| Smoking ever, n (%) | 613 (38) | 377 (42) | 149 (38) | 87 (27) | <0.001 |
| HCV coinfection, n (%) | 21 (1) | 7 (1) | 9 (2) | 5 (2) | 0.08 |
| CD4 nadir, cells/µL, median (IQR) | 217 (131–289) | 235 (161–305) | 199 (103–271) | 194 (93–265) | <0.001 |
| HIV-RNA at start of ART, log10 copies/mL | 4.8 (4.2–5.4) | 4.9 (4.3–5.3) | 4.9 (4.2–5.5) | 4.7 (4.0–5.3) | 0.04 |
Abbreviations: ART, antiretroviral therapy; HIV, human immunodeficiency virus; IQR, interquartile range; MSM, men who have sex with men; SD; standard deviation; SHCS, Swiss HIV Cohort Study.
* MSM are compared with heterosexual males and females.
Table 2.
Bi- and Multivariable Linear Regression of BMI Changes During Year 0–1 and Years 1–4 of ART Among 1601 SHCS Participants Who Started a First ART Regimen After January 1, 1998
| Covariables | Year 0-1 of ART |
Years 1–4 of ART |
||||||
|---|---|---|---|---|---|---|---|---|
| Coefficient Bivariable models (95% CI)a | P Value | Coefficient Multivariable Models (95% CI)b | P Value | Coefficient Bivariable Models (95% CI)c | P Value | Coefficient Multivariable Models (95% CI)b | P Value | |
| Baseline BMId | −0.09 (−.11 to .07) | <.001 | −0.09 (−.11 to −.06) | <.001 | −0.02 (−.03 to −0.01) | <.001 | −0.01 (−.02 to −.00) | .002 |
| Delta BMI change, first year of ART | – | – | – | – | −0.05 (−.07 to −.03) | <.001 | −0.06 (−.07 to −.04) | <.001 |
| HIV transmission group | ||||||||
| MSM | 1 | – | 1 | – | 1 | – | 1 | – |
| Het male | 0.46 (.24 to .68) | <.001 | 0.20 (−.02 to .42) | .07 | 0.06 (−.02 to 0.13) | .14 | 0.02 (−.05 to .10) | .53 |
| Het female | 0.18 (−.06 to .41) | .14 | 0.07 (−.18 to .32) | .58 | 0.05 (−.03 to .13) | .24 | −0.03 (−.11 to .06) | .52 |
| Age per 10 yearse | 0.25 (.16 to .34) | <.001 | 0.15 (.06 to .24) | .002 | 0.01 (−.02 to .04) | .35 | 0.02 (−.01 to .05) | .14 |
| Ethnicity | ||||||||
| White | 1 | – | 1 | – | 1 | – | 1 | – |
| Black | 0.04 (−.25 to .33) | .80 | −0.05 (−.36 to .26) | .74 | 0.26 (.16 to .35) | <.001 | 0.28 (.16 to .37) | <.001 |
| Asian | −0.60 (−1.0 to −.18) | .005 | −0.79 (−1.2 to −.39) | <.001 | −0.01 (−.15 to .13) | .87 | 0.01 (−.13 to .15) | .88 |
| Other | −0.44 (−.93 to .05) | .08 | −0.25 (−.71 to .21) | .29 | −0.01 (−.17 to .15) | .90 | −0.03 (−.19 to .13) | .71 |
| CD4 nadir | ||||||||
| 0–99 cells/µL | 1.73 (1.45 to 2.02) | <.001 | 1.64 (1.4 to 1.9) | <.001 | 0.40 (.14 to .66) | .002 | 0.44 (.19 to .70) | .001 |
| 100–199 cells/µL | 0.50 (.24 to .76) | <.001 | 0.46 (.19 to .72) | .001 | −0.04 (−.16 to .07) | .44 | 0.05 (−.07 to .17) | .40 |
| 200–349 cells/µL | −0.00 (−.21 to .21) | .99 | −0.02 (−.23 to .19) | .82 | 0.04 (−.03 to .11) | .28 | 0.07 (−.00 to .14) | .05 |
| ≥350 cells/µL | 1 | – | 1 | – | 1 | – | 1 | – |
| Smoking, ever | −0.46 (−.65 to −.27) | <.001 | −0.29 (−.47 to −.11) | .002 | −0.04 (−.10 to .02) | .20 | – | – |
| Smoking cessation | −0.11 (−.78 to .56) | .75 | – | – | 0.15 (.03 to .26) | .01 | 0.16 (.04 to .27) | .006 |
| HCV coinfection | −0.73 (−1.5 to .06) | .07 | – | – | −0.26 (−.46 to −0.06) | .01 | – | – |
| Peginf | 0.56 (−3.1 to 4.2) | .76 | – | – | −0.72 (−1.1 to −.37) | <.001 | –0.71 (−1.0 to −.37) | <.001 |
| Most frequent ART regimens | ||||||||
| TDF, xTC, EFV | 1 | − | 1 | − | 1 | − | 1 | − |
| ABC, xTC, EFV | 0.27 (−.20 to .75) | .26 | 0.21 (−.23 to .64) | .35 | −0.01 (−.16 to .15) | .95 | −0.01 (−.16 to .14) | .89 |
| ABC, xTC, LPV | 0.51 (−0.05 to 1.1) | .08 | 0.22 (−.30 to .74) | .41 | 0.14 (−.07 to .35) | .21 | 0.15 (−.06 to .36) | .16 |
| ABC, xTC, ATV, RTV | 0.15 (−0.50 to .80) | .66 | 0.19 (−.41 to .79) | .53 | 0.16 (−.04 to .36) | .11 | 0.14 (−.05 to .33) | .16 |
| AZT, xTC, EFV | 0.04 (−.30 to .39) | .81 | −0.13 (−.45 to .20) | .44 | −0.16 (−.28 to −.04) | .01 | −0.17 (−.29 to −.05) | .006 |
| AZT, xTC, LPV | 0.54 (.19 to .89) | .003 | 0.29 (−.04 to .62) | .08 | −0.16 (−.30 to −.02) | .03 | −0.12 (−.25 to .02) | .09 |
| AZT, xTC, NFV | 0.27 (−.27 to .80) | .33 | −0.09 (−.59 to .41) | .73 | −0.25 (−.46 to −.03) | .02 | −0.22 (−.43 to −.01) | .04 |
| TDF, xTC, LPV | 0.45 (.10 to .80) | .01 | 0.30 (−.03 to .62) | .08 | 0.08 (−.07 to .23) | .30 | 0.06 (−.08 to .21) | .38 |
| TDF, xTC, NVP | −0.09 (−.60 to .42) | .73 | 0.06 (−.42 to .54) | .81 | 0.00 (−.14 to .14) | .97 | 0.03 (−.10 to .16) | .65 |
| TDF, xTC, ATV, RTV | 0.04 (−.30 to .39) | .80 | 0.12 (−.20 to .44) | .45 | 0.01 (−.11 to .13) | .89 | 0.06 (−.05 to .17) | .30 |
| Otherf | 0.27 (−.01 to .55) | .06 | 0.14 (−.12 to .40) | .29 | −0.06 (−.14 to .03) | .17 | −0.04 (−.12 to .04) | .36 |
Abbreviations: ABC, abacavir; ART, antiretroviral therapy; ATV, atazanavir; AZT, zidovudine; BMI, body mass index; CI, confidence interval; EFV, efavirenz; HCV, hepatitis C virus; Het, heterosexual; LPV, lopinavir; NFV, nelfinavir; NRTI, nucleoside reverse-transcriptase inhibitor; NVP, nevirapine; Other, patients with no backbone or no third drug for 50% of the time or patients with 3 class regimens; Peginf, pegylated interferon; RAL, raltegravir; RTV, ritonavir; SHCS, Swiss HIV Cohort Study; TDF, tenofovir; xTC, lamivudine or emtricitabine.
a All covariables of the bivariable model were adjusted for baseline BMI.
b Multivariable models were adjusted for all variables listed.
c All covariables of the bivariable model were adjusted for BMI after 1 year of ART.
d Baseline BMI at start of ART and BMI after 1 year of ART, respectively.
e Age at baseline (January 1, 1998 or at registration in the SHCS, whichever is the later) and after 1 year of ART.
f Contains all ART regimens with <50 person-years of exposure.
Definitions and Measures
Body mass index (kg/m2) was stratified into <18.5 (underweight), 18.5–24.9 (normal), 25–29.9 (overweight), and 30 (obese), without modification for Asians [19]. Hepatitis C coinfection was defined as detectable hepatitis C virus (HCV) RNA. Smoking was stratified into ever, never, and smoking cessation during follow-up. xTC refers to ART containing either 3TC (lamivudine) or FTC (emtricitabine).
Statistical Analysis
Categorical variables were compared with χ2 tests, and continuous variables were assessed with non-parametric methods (Kruskal-Wallis equality-of-populations rank test or tests for trend over calendar year, whichever was applicable). We performed bi- and multivariable linear regression analyses to investigate the effects of HIV transmission groups, age, CD4 nadir, smoking, HCV coinfection, and ART agents on BMI after ART initiation, presented as mean BMI changes (95% confidence intervals [CIs]). Antiretroviral agents are recorded with start and stop dates in the SHCS, and ART exposure was assessed at every follow-up visit.
Assumptions underlying these analyses were verified in scatter diagrams. In exploratory analyses, BMI trajectories after ART start were typically biphasic, with an initial rapid BMI gain corresponding approximately to the first year, and a smaller BMI gain during years 1–4 of ART. Therefore, subsequent detailed analyses were performed separately for years 0–1 and 1–4 of ART. Multivariable linear regression models for BMI change during year 1 were adjusted for BMI at ART start, HIV transmission group, age per 10 years, ethnicity (white, black, Asian, other), CD4 nadir (0–99, 10–199, 200–349, >350 cells/µL), smoking (never, ever, smoking cessation), and ART regimen. During year 1–4 of ART, additional adjustments were for BMI after 1 year of ART and pegylated interferon treatment. Antiretroviral treatment exposure was considered in 3 ways: most frequent ART regimens (Table 2; Supplementary Table 2), nucleoside reverse-transcriptase inhibitor (NRTI) backbones (Supplementary Table 3), and third agents (Supplementary Table 3), each defined as being administered during ≥50% of the respective time periods (years 0–1 and 1–4). Antiretroviral treatment regimens with <50 person-years of exposure were summarized in an “other” category.
Based on multivariable linear regression analyses, we made standardized predictions of mean BMI changes [kg/m2 per year] for different HIV transmission categories (men who have sex with men [MSM], male heterosexual, female heterosexual), for different ethnicities (white, black, Asian), and different age groups (30–40, 41–50, 50+ years). For predictions, we fixed the remaining variables CD4 at 200–350 cells/µL, smoking status at never smoking, and baseline BMI at 22 kg/m2. Interactions between BMI changes and ART, transmission groups, and ethnicity were analyzed with a likelihood ratio test. We performed sensitivity analyses adjusting for calendar periods (2003–2005, 2006–2008, and 2009 and after). All analyses were done using Stata (version 13.1; StataCorp, College Station, TX).
RESULTS
Population BMI Trends, 1990–2012
The BMI distribution in the entire SHCS population stratified by calendar year is shown in Figure 1 and Supplementary Figure 1, respectively. From 1990 to 2012, the percentage of normal weight and underweight participants decreased. Median BMI and the percentage of obese and overweight participants increased (Figure 1; Supplementary Table 1). In 2012, the median BMI was 24 kg/m2 (interquartile range, 22–27), and 57% (95% CI, 56%–58%) of the population were normal weight, 4.3% (3.9–4.7) were underweight, 29% (28–30) were overweight, and 9.3% (8.6–9.9) were obese. From 1990 to 2012, the percentage of white participants (P < .001), IDUs (P < .001), and participants with AIDS-defining illnesses decreased (P < .001). The percentage of women (P = .03), participants on ART (P < .001), the median CD4 cell count at ART initiation (P < .001), and the median age of participants increased (P < .001).
BMI Change After ART Initiation
From January 1, 1998 to December 31, 2012, 5415 SHCS participants with MSM or heterosexual HIV transmission started a first ART regimen. Stringent inclusion criteria resulted in a substantial reduction of participants (Supplementary Figure 2). Subsequent analyses are based on 1601 participants (Table 1; Supplementary Table 2), 6250 person-years of follow-up, and 4803 BMI measurements. Median age at ART start was 40 years, 80% were white, and 19% were female. Body mass index change after ART initiation was biphasic; the mean BMI change during year 0–1 of ART was 0.92 kg/m2 per year (95% CI, .83–1.0), and during years 1–4 was 0.31 (0.29–0.34) kg/m2 per year. The mean interval between BMI determinations was 0.99 years (range, 0.43–1.5 years) between baseline and year 1 after ART start, and 2.9 years (1.7–4.2) between years 1 and 4.
Body Mass Index Change, Year 0–1 After ART Start
In the final, multivariable adjusted model, there was a trend towards larger BMI gain in heterosexual males compared with MSM. Compared with whites, annualized BMI change was not different in black and other ethnicities, but smaller in Asians (−0.79 [95% CI, −1.2 to −.39] kg/m2; P = .001). Body mass index change was associated with older age (0.15 [0.06–0.24] kg/m2 per 10 years older; P = .002). Compared to CD4 nadir >350 cells/µL, a CD4 nadir of 0–99 and 100–199 cells/µL had the largest effect on BMI change (1.64 [1.4–1.9] kg/m2 per year; P < .001 and 0.46 [0.19–0.71] kg/m2 per year; P = .001, respectively). Smoking was associated with a BMI decrease (−0.29 [−0.47 to 0.11] kg/m2 per year; P = .002). Body mass index change was similar with the ten most commonly prescribed ART regimens. Body mass index change was also similar for different NRTI backbones and third drugs, except for raltegravir, which was associated with a BMI change of 1.0 ([0.17–1.8] kg/m2 per year; P = .018), compared with efavirenz (Supplementary Table 3). These multivariable associations remained unchanged after adjustment for calendar period. No significant interactions were detected between BMI changes and ART, transmission groups, and ethnicity.
Body Mass Index Changes, Years 1–4 After ART Start
In the final, multivariable adjusted model, BMI change was similar in heterosexual males (0.02 [95% CI, −.05 to 0.10] kg/m2 per year; P = .53) and females (−0.03 [−0.11 to 0.06] kg/m2 per year; P = .52) compared with MSM. No age effect on BMI change was identified during years 1–4 (0.02 [−0.01 to 0.05] kg/m2 per year; P = .14). Body mass index gain was larger in black compared with white participants (0.28 [0.16–0.37] kg/m2 per year; P < .001). Body mass index change was also associated with CD4 nadir 0–99 cells/µL (0.44 [0.19–0.70] kg/m2 per year; P = .001) compared to CD4 nadir >350 cells/µL, with smoking cessation (0.16 [0.04–0.27] kg/m2 per year; P = .006) and with pegylated interferon (−0.71 [−1.0 to −0.37] kg/m2 per year; P < .001). Compared to calendar period 1998–2002, BMI change was similar in 2003–2005 (P = .57), but it increased in 2006–2008 (0.12 [0.03–0.21] kg/m2; P = .008) and in 2009 and after (0.19 [0.09–0.28] kg/m2 per year; P < .001). No significant interactions were detected between BMI changes and ART, transmission groups, and ethnicity. Body mass index change was similar for the 10 most commonly prescribed ART regimens (Table 2). As regards NRTIs and third agents (Supplementary Table 3), compared with tenofovir/xTC and efavirenz, zidovudine was associated with a smaller BMI increase, in combination with either efavirenz/xTC (−0.17 [−0.29 to −0.05] kg/m2 per year; P = .006) or with nelfinavir/xTC (−0.22 [−0.43 to −0.01] kg/m2 per year; P = .04). The NRTI backbones zidovudine/abacavir/xTC, zidovudine/xTC, and d4T/xTC were associated with a BMI decrease when comparing them with tenofovir/xTC (−0.20 [−0.32 to −0.08], 0−.20 [−0.28 to −0.13], and −0.35 [−0.67 to −0.04] kg/m2 per year, respectively). There was a larger BMI increase with atazanavir/ritonavir compared with efavirenz (P = .03) (Supplementary Table 3).
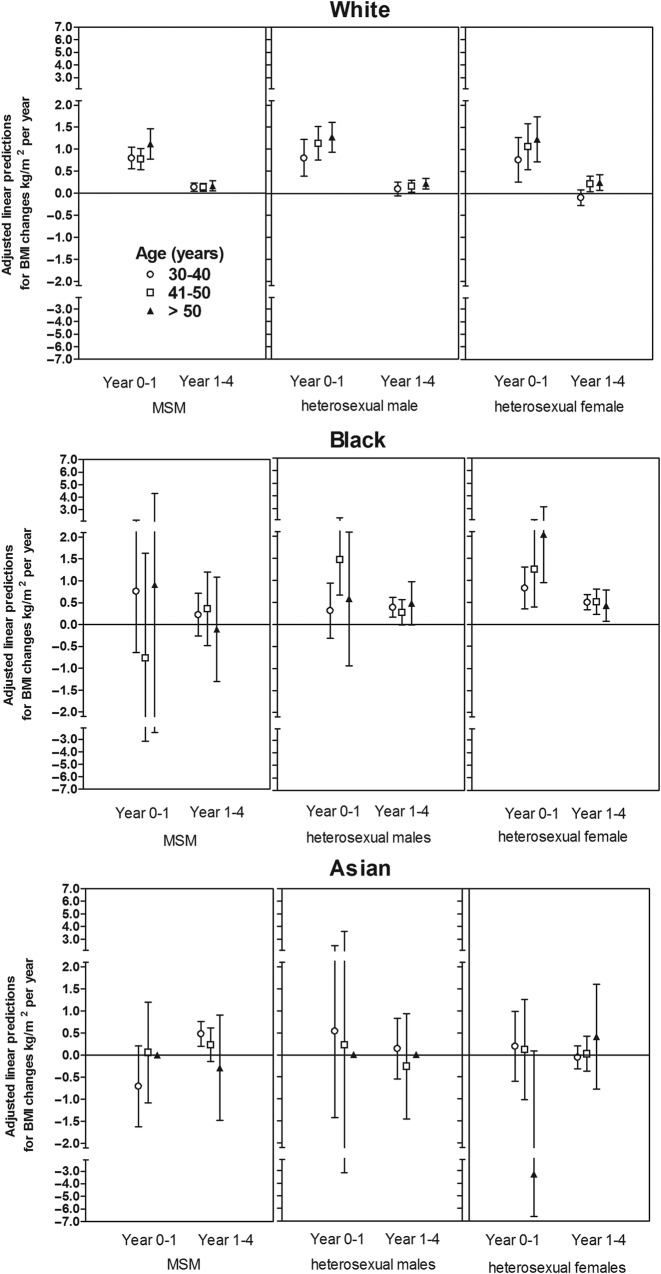
The effects of transmission category, ethnicity, and age groups are further illustrated in Figure 2, which shows predicted BMI changes during years 0–1 and 1–4 of ART. The BMI increase was biphasic in white patients and black women, and the age effect was restricted to year 0–1 of ART.
Fig. 2.
Adjusted predicted annualized body mass index (BMI) changes during years 0–1 and years 1–4 of ART start. Separate predictions of BMI changes/year are presented for human immunodeficiency virus transmission category, gender, ethnicity, and age groups. Results are based on multivariable regression models adjusted for transmission category, ethnicity, age group, CD4 categories, and smoking status. For predictions, we fixed the remaining variables CD4 at 200–350, never smoking, and baseline BMI of 22 kg/m2. Abbreviations: hetero, heterosexual; MSM, men who have sex with men.
DISCUSSION
This study has 3 major findings; first, obesity rates in the SHCS have been increasing since 1995 in the setting of demographic changes, earlier ART start, and more widespread population ART coverage; second, BMI increase after ART initiation typically was biphasic, and the BMI increase in year 0–1 was as large as the increase in years 1–4 combined and was related most notably to the CD4 nadir; and third, we found little evidence that the individual ART regimen selected is a major driver of the extent of BMI change after ART start.
We describe a number of changes in demographics and in HIV management that may be partially responsible for the increasing obesity prevalence in the entire SHCS population over time, including an aging population, fewer IDU, initiation of ART at higher CD4 counts, and increasingly complete ART coverage. Injection drug use has been associated with lower BMI, more weight loss, and less weight gain after ART start, compared with other HIV+ persons [20], but not in all studies [11]. Before ART start, BMI typically declines with advanced HIV infection [21] and may predict survival and progression to AIDS [22]. In contrast, earlier ART start in recent years may prevent opportunistic complications, wasting, and the associated weight loss. Successful ART has produced an aging HIV+ population that is in much better health [23]. Advancing age is an important contributor to BMI in the general population [14, 15, 17, 24–26]. Increasing obesity rates have previously been recorded in HIV+ populations [11, 13, 23, 27], and the percentages of normal weight, underweight and overweight persons in the SHCS in 2012 was very similar to the percentages reported in the Swiss general population in 2012 [28].
Our study represents the most comprehensive assessment of longitudinal BMI change after ART start to date. In detailed analyses, we found BMI change after ART initiation to be a biphasic process that included a mean increase during the first year of ART that was as large as the mean increase during the 3 subsequent years combined. A biphasic BMI behavior has not previously been described; it likely represents a rapid re-gain of weight lost during untreated HIV infection [6, 10], perhaps similar to the return of plasma lipid levels to preinfection levels after ART start [29]. The biphasic BMI increase resembles the biphasic CD4+ lymphocyte increase after starting ART, which is initially rapid and followed by a second phase of slower CD4 increase [30]. We observed a biphasic BMI increase after ART start in white participants and in black women; there were limited numbers of patients of other ethnicities in our study and CIs were wide.
The largest contributor to BMI increase was the CD4 nadir. A larger degree of weight loss before ART that may occur with profound immunosuppression presumably correlates with a larger degree of weight re-gain after ART start. The BMI effect of a CD4 nadir < 100 cells/µL persisted into years 1–4 of ART. An effect of the CD4 nadir on weight gain during the first [31] and the first 2 years [20] of ART has been previously reported. Contrary to our expectations, smoking and advancing age had no effect on BMI behavior during years 1–4 of ART, whereas smoking cessation was associated with larger BMI gain, consistent with data from the general population [32].
We found a limited contribution of the selected ART regimen to BMI change. Potential differences between individual drugs were not apparent when the BMI effect of commonly used ART combinations was examined during prolonged exposure (years 1–4). Our findings extend previous reports including a randomized study (422 participants; median follow-up, 5 years) in which median BMI increase did not differ with protease inhibitor (PI) vs non-NRTI (NNRTI) treatment, even though individual PIs and NNRTIs were not compared [33]. In AIDS Clinical Trials Group (ACTG) Study A5142 (753 participants), the median BMI increase did not differ between treatment arms at 96 weeks [34]. A5142 compared lopinavir/ritonavir vs efavirenz vs both, and stavudine vs tenofovir vs zidovudine. In ACTG A5224s, a larger mean BMI gain was noted at 96 weeks in patients randomized to atazanavir/ritonavir (n = 109) compared with efavirenz (n = 94) [35]. In an observational study of 681 patients, PI treatment was associated with greater weight gain than NNRTI treatment after 2 years of ART, but individual PIs and NNRTIs were not assessed [20].
Zidovudine-containing regimens were associated with smaller BMI increases in the SHCS compared with other regimens. This result is consistent with the well recorded, sustained effect of thymidine analogs on peripheral fat loss [7, 36, 37] and suggests that lipoatrophy may result in an attenuated BMI gain, as previously reported [10]. The increased BMI gain in our study in more recent calendar periods may partially be related to little use of thymidine analogs [9]. We note that 2 studies conducted during 1999–2002 and 1999–2003, respectively, reported no longitudinal BMI increase in HIV+ persons [38, 39]. Possible explanations for this include much less widespread ART use during the early ART era and, if ART was given, it typically included thymidine analogs.
Strengths of this study include longitudinal data collection in an established, large observational study. Due to the prospective design of the SHCS, we were able to control for important cofactors. Limitations include that information on diet and certain psychiatric comedications potentially associated with weight gain are not yet systematically captured; alcohol use and physical activity has been recorded since 2009 and was not considered in the present study. Moreover, the SHCS does not collect information on poverty, an important social determinant of BMI change.
In conclusion, increasing obesity rates in the SHCS population have occurred at the same time as trends towards restoration of health and normal aging in the setting of increasingly widespread population ART coverage. Ethnicity and immune suppression (CD4 nadir) had important effects on BMI behavior after ART start, but there was no clear evidence that frequently used ART regimens differ in their influence on BMI change during 4 years of follow-up. Similar to the general population, HIV+ patients should be motivated to consider a healthy lifestyle including diet, exercise, and behavioral modifications.
Author Contributions
P. E. T. and M. I. designed the study. B. L. analyzed the data. B. H. and M. I. wrote the first draft, and B. H., M. I., B. L., and P. E. T. wrote the final version of the manuscript. All investigators contributed to data collection and interpretation of the data, reviewed drafts of the manuscript, and approved the final manuscript.
Supplementary Data
Supplementary material is available online at Open Forum Infectious Diseases (http://OpenForumInfectiousDiseases.oxfordjournals.org/).
Acknowledgments
We thank all involved physicians, study nurses, and, most importantly, participants of the SHCS. The members of the Swiss HIV Cohort Study are as follows: Aubert V, Barth J, Battegay M, Bernasconi E, Böni J, Bucher HC, Burton-Jeangros C, Calmy A, Cavassini M, Egger M, Elzi L, Fehr J, Fellay J, Furrer H (Chairman of the Clinical and Laboratory Committee), Fux CA, Gorgievski M, Günthard H (President of the SHCS), Haerry D (deputy of "Positive Council"), Hasse B, Hirsch HH, Hösli I, Kahlert C, Kaiser L, Keiser O, Klimkait T, Kouyos R, Kovari H, Ledergerber B, Martinetti G, Martinez de Tejada B, Metzner K, Müller N, Nadal D, Pantaleo G, Rauch A (Chairman of the Scientific Board), Regenass S, Rickenbach M (Head of Data Center), Rudin C (Chairman of the Mother & Child Substudy), Schöni-Affolter F, Schmid P, Schultze D, Schüpbach J, Speck R, Staehelin C, Tarr P, Telenti A, Trkola A, Vernazza P, Weber R, Yerly S.
Financial support. This study was financed within the framework of the Swiss HIV Cohort Study (Study no. 627), supported by the Swiss National Science Foundation (grant no. 134277).
Potential conflicts of interest. B. H. has received travel grants from Essex Chemicals, Wyeth, Astra Zeneca, and Janssen. B. L. has received travel grants, grants, or honoraria from Abbott, Aventis, Bristol-Myers Squibb, Gilead, GlaxoSmithKline, Merck Sharp & Dohme, Roche, and Tibotec. E. B. has received travel grants, grants, and honoraria from Abbott, BMS, Boehringer Ingelheim, Gilead Sciences, Janssen, MSD, and ViiV. A. C. received travel grants from Boehringer Ingelheim and received unrestricted educational grants from Janssen Cilag, Gilead, MSD, ViiV, BMS, and AbbVie. P. E. T.′s institution has received advisory fees from MSD and honoraria from ViiV. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1.Freiberg MS, Chang CC, Kuller LH, et al. HIV infection and the risk of acute myocardial infarction. JAMA Intern Med. 2013;173:614–22. doi: 10.1001/jamainternmed.2013.3728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Reis JP, Loria CM, Lewis CE, et al. Association between duration of overall and abdominal obesity beginning in young adulthood and coronary artery calcification in middle age. JAMA. 2013;310:280–8. doi: 10.1001/jama.2013.7833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Global Burden of Metabolic Risk Factors for Chronic Diseases Collaboration (BMI Mediated Effects) Metabolic mediators of the effects of body-mass index, overweight, and obesity on coronary heart disease and stroke: a pooled analysis of 97 prospective cohorts with 1.8 million participants. Lancet. 2014;383:970–83. doi: 10.1016/S0140-6736(13)61836-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA. 2013;309:71–82. doi: 10.1001/jama.2012.113905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Carr A, Samaras K, Burton S, et al. A syndrome of peripheral lipodystrophy, hyperlipidaemia and insulin resistance in patients receiving HIV protease inhibitors. AIDS. 1998;12:F51–8. doi: 10.1097/00002030-199807000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Kotler DP, Rosenbaum K, Wang J, Pierson RN. Studies of body composition and fat distribution in HIV-infected and control subjects. J Acquir Immune Defic Syndr Hum Retrovirol. 1999;20:228–37. doi: 10.1097/00042560-199903010-00003. [DOI] [PubMed] [Google Scholar]
- 7.Bernasconi E, Boubaker K, Junghans C, et al. Abnormalities of body fat distribution in HIV-infected persons treated with antiretroviral drugs: The Swiss HIV Cohort Study. J Acquir Immune Defic Syndr. 2002;31:50–5. doi: 10.1097/00126334-200209010-00007. [DOI] [PubMed] [Google Scholar]
- 8.Bacchetti P, Gripshover B, Grunfeld C, et al. Fat distribution in men with HIV infection. J Acquir Immune Defic Syndr. 2005;40:121–31. doi: 10.1097/01.qai.0000182230.47819.aa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nguyen A, Calmy A, Schiffer V, et al. Lipodystrophy and weight changes: data from the Swiss HIV Cohort Study, 2000–2006. HIV Med. 2008;9:142–50. doi: 10.1111/j.1468-1293.2007.00537.x. [DOI] [PubMed] [Google Scholar]
- 10.Brown TT, Chu H, Wang Z, et al. Longitudinal increases in waist circumference are associated with HIV-serostatus, independent of antiretroviral therapy. AIDS. 2007;21:1731–8. doi: 10.1097/QAD.0b013e328270356a. [DOI] [PubMed] [Google Scholar]
- 11.Amorosa V, Synnestvedt M, Gross R, et al. A tale of 2 epidemics: the intersection between obesity and HIV infection in Philadelphia. J Acquir Immune Defic Syndr. 2005;39:557–61. [PubMed] [Google Scholar]
- 12.Shor-Posner G, Campa A, Zhang G, et al. When obesity is desirable: a longitudinal study of the Miami HIV-1-infected drug abusers (MIDAS) cohort. J Acquir Immune Defic Syndr. 2000;23:81–8. doi: 10.1097/00126334-200001010-00011. [DOI] [PubMed] [Google Scholar]
- 13.Crum-Cianflone N, Tejidor R, Medina S, et al. Obesity among patients with HIV: the latest epidemic. AIDS Patient Care STDS. 2008;22(12):925–30. doi: 10.1089/apc.2008.0082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lewis CE, Jacobs DR, Jr, McCreath H, et al. Weight gain continues in the 1990s: 10-year trends in weight and overweight from the CARDIA study. Coronary Artery Risk Development in Young Adults. Am J Epidemiol. 2000;151:1172–81. doi: 10.1093/oxfordjournals.aje.a010167. [DOI] [PubMed] [Google Scholar]
- 15.Clarke P, O'Malley PM, Johnston LD, Schulenberg JE. Social disparities in BMI trajectories across adulthood by gender, race/ethnicity and lifetime socio-economic position: 1986–2004. Int J Epidemiol. 2009;38:499–509. doi: 10.1093/ije/dyn214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Falutz J. HIV infection, body composition changes and related metabolic complications: contributing factors and evolving management strategies. Curr Opin Clin Nutr Metab Care. 2011;14:255–60. doi: 10.1097/MCO.0b013e3283457a8f. [DOI] [PubMed] [Google Scholar]
- 17.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA. 2012;307:491–7. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 18.Schoeni-Affolter F, Ledergerber B, Rickenbach M, et al. Cohort profile: the Swiss HIV Cohort study. Int J Epidemiol. 2010;39:1179–89. doi: 10.1093/ije/dyp321. [DOI] [PubMed] [Google Scholar]
- 19.WHO Expert Consultation, et al. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–63. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 20.Tate T, Willig AL, Willig JH, et al. HIV infection and obesity: where did all the wasting go? Antivir Ther. 2012;17:1281–9. doi: 10.3851/IMP2348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Maas JJ, Dukers N, Krol A, et al. Body mass index course in asymptomatic HIV-infected homosexual men and the predictive value of a decrease of body mass index for progression to AIDS. J Acquir Immune Defic Syndr Hum Retrovirol. 1998;19:254–9. doi: 10.1097/00042560-199811010-00007. [DOI] [PubMed] [Google Scholar]
- 22.Palenicek JP, Graham NM, He YD, et al. Weight loss prior to clinical AIDS as a predictor of survival. Multicenter AIDS Cohort Study Investigators. J Acquir Immune Defic Syndr Hum Retrovirol. 1995;10:366–73. [PubMed] [Google Scholar]
- 23.Crum-Cianflone N, Roediger MP, Eberly L, et al. Increasing rates of obesity among HIV-infected persons during the HIV epidemic. PLoS One. 2010;5:e10106. doi: 10.1371/journal.pone.0010106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hankinson AL, Daviglus ML, Bouchard C, et al. Maintaining a high physical activity level over 20 years and weight gain. JAMA. 2010;304:2603–10. doi: 10.1001/jama.2010.1843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rissanen A, Heliovaara M, Aromaa A. Overweight and anthropometric changes in adulthood: a prospective study of 17,000 Finns. Int J Obes. 1988;12:391–401. [PubMed] [Google Scholar]
- 26.Williamson DF, Kahn HS, Remington PL, Anda RF. The 10-year incidence of overweight and major weight gain in US adults. Arch Intern Med. 1990;150:665–72. [PubMed] [Google Scholar]
- 27.Boodram B, Plankey MW, Cox C, et al. Prevalence and correlates of elevated body mass index among HIV-positive and HIV-negative women in the Women's Interagency HIV Study. AIDS Patient Care STDS. 2009;23:1009–16. doi: 10.1089/apc.2009.0175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Swiss Health Survey 2012 of the Swiss Federal Office of Statistics. Available at: http://www.bfs.admin.ch/bfs/portal/de/index/themen/14/01/new/nip_detail.html?gnpID=2013-523 . Accessed 10 February 2014. [Google Scholar]
- 29.Riddler SA, Smit E, Cole SR, et al. Impact of HIV infection and HAART on serum lipids in men. JAMA. 2003;289:2978–82. doi: 10.1001/jama.289.22.2978. [DOI] [PubMed] [Google Scholar]
- 30.Kaufmann GR, Perrin L, Pantaleo G, et al. CD4 T-lymphocyte recovery in individuals with advanced HIV-1 infection receiving potent antiretroviral therapy for 4 years: the Swiss HIV Cohort Study. Arch Intern Med. 2003;163:2187–95. doi: 10.1001/archinte.163.18.2187. [DOI] [PubMed] [Google Scholar]
- 31.Lakey W, Yang LY, Yancy W, et al. Short communication: from wasting to obesity: initial antiretroviral therapy and weight gain in HIV-infected persons. AIDS Res Hum Retroviruses. 2013;29:435–40. doi: 10.1089/aid.2012.0234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Flegal KM, Troiano RP, Pamuk ER, et al. The influence of smoking cessation on the prevalence of overweight in the United States. New Engl J Med. 1995;333:1165–70. doi: 10.1056/NEJM199511023331801. [DOI] [PubMed] [Google Scholar]
- 33.Shlay JC, Bartsch G, Peng G, et al. Long-term body composition and metabolic changes in antiretroviral naive persons randomized to protease inhibitor-, nonnucleoside reverse transcriptase inhibitor-, or protease inhibitor plus nonnucleoside reverse transcriptase inhibitor-based strategy. J Acquir Immune Defic Syndr. 2007;44:506–17. doi: 10.1097/QAI.0b013e31804216cf. [DOI] [PubMed] [Google Scholar]
- 34.Haubrich RH, Riddler SA, DiRienzo AG, et al. Metabolic outcomes in a randomized trial of nucleoside, nonnucleoside and protease inhibitor-sparing regimens for initial HIV treatment. AIDS. 2009;23:1109–18. doi: 10.1097/QAD.0b013e32832b4377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.McComsey GA, Kitch D, Sax PE, et al. Peripheral and central fat changes in subjects randomized to abacavir-lamivudine or tenofovir-emtricitabine with atazanavir-ritonavir or efavirenz: ACTG Study A5224s. Clin Infect Dis. 2011;53:185–96. doi: 10.1093/cid/cir324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Brinkman K, Smeitink JA, Romijn JA, Reiss P. Mitochondrial toxicity induced by nucleoside-analogue reverse-transcriptase inhibitors is a key factor in the pathogenesis of antiretroviral-therapy-related lipodystrophy. Lancet. 1999;354:1112–5. doi: 10.1016/S0140-6736(99)06102-4. [DOI] [PubMed] [Google Scholar]
- 37.Grunfeld C, Saag M, Cofrancesco J, Jr, et al. Regional adipose tissue measured by MRI over 5 years in HIV-infected and control participants indicates persistence of HIV-associated lipoatrophy. AIDS. 2010;24:1717–26. doi: 10.1097/QAD.0b013e32833ac7a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tien PC, Cole SR, Williams CM, et al. Incidence of lipoatrophy and lipohypertrophy in the women's interagency HIV study. J Acquir Immune Defic Syndr. 2003;34:461–6. doi: 10.1097/00126334-200312150-00003. [DOI] [PubMed] [Google Scholar]
- 39.Brown T, Wang Z, Chu H, et al. Longitudinal anthropometric changes in HIV-infected and HIV-uninfected men. J Acquir Immune Defic Syndr. 2006;43:356–62. doi: 10.1097/01.qai.0000243052.73321.8e. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.