Abstract
Transoral vertical ramus osteotomy (TOVRO) procedure can result in a variety of complications. Complications commonly reported include extensive bleeding due to major blood vessel injury, unpredictable fracture, postoperative infection, neurosensory deficit related Inferior alveolar nerve, insufficient osteosynthesis, and temporomandibular joint problem. The authors describe a case of partial necrosis of the mandibular proximal segment following TOVRO, a rarely reported complication. A 37-year-old otherwise healthy woman underwent Lefort l osteotomy and TOVRO to correct mandibular prognathism. Postoperatively, she developed pain and swelling in the right submandibular region and was found to have a partial necrosis of proximal segment.
Keywords: Transoral vertical ramus osteotomy, Osteonecrosis, Orthognathic surgery
Introduction
Transoral vertical ramus osteotomy (TOVRO) is an orthognathic surgical technique used to correct mandibular prognathism. Complications commonly reported include extensive bleeding due to major blood vessel injury, unpredictable fracture, postoperative infection, neurosensory deficit related to the inferior alveolar nerve, displacement of proximal segment, and mal-union or non-union of bony segments [1]. It is rare to have bony segment necrosis after TOVRO [1–3] given the bone healing pattern and revascularization of the mandible [4]. There have been no cases of necrosis of bony segments reported since the introduction of perioperative antibiotic use and improved surgical techniques. The authors present a case of an otherwise healthy 37-year-old female patient who underwent LeFort I osteotomy and TOVRO to correct a skeletal deformity, complicated by a partial necrosis of the proximal segment.
Case Report
A 37-year-old female patient who underwent orthognathic surgery was re-admitted with persistent pain, swelling and purulent discharge from her right submandibular region. The patient underwent LeFort I osteotomy and TOVRO by a private practice oral surgeon 10 weeks prior. The post-operative day 2 panoramic radiograph was un-remarkable (Fig. 1). The patient received peri-operative intravenous antibiotics and was discharged home with two weeks of oral antibiotics.
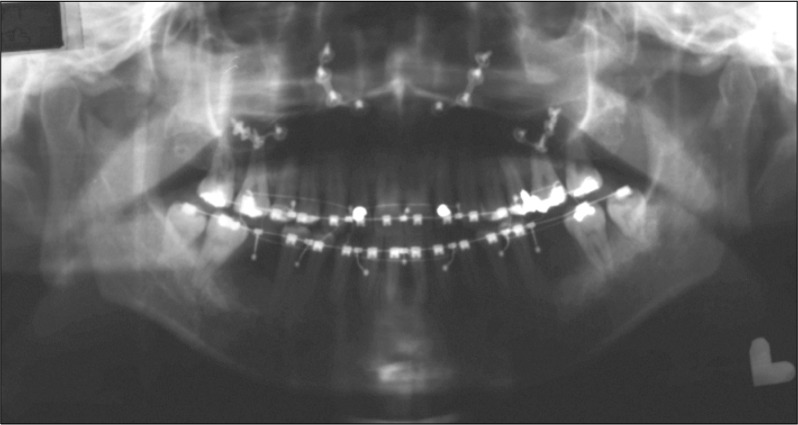
Fig. 1.
Post-operative panoramic radiograph (two days after orthognathic surgery).
The working diagnosis from the history and physical examination was osteomyelitis of right proximal segment of mandible. This was supported by the panoramic radiograph and computed tomography (Fig. 2, 3) that demonstrates radiolucency and destructive bony change at the angle of right mandible with an evidence of sequestering bony segment. The patient was started on intravenous antibiotics (combination of 3rd generation cephalosporin and Metronidazole) upon admission, and she was taken to the operating room for removal of the sequestered bony segment and a drain placement. Intra-operatively, an approximately 15 mm sequestrum at the inferior aspect of the proximal segment was noted and removed. A three month post-operative panoramic radiograph (Fig. 4) was un-remarkable, with resolution of symptoms.
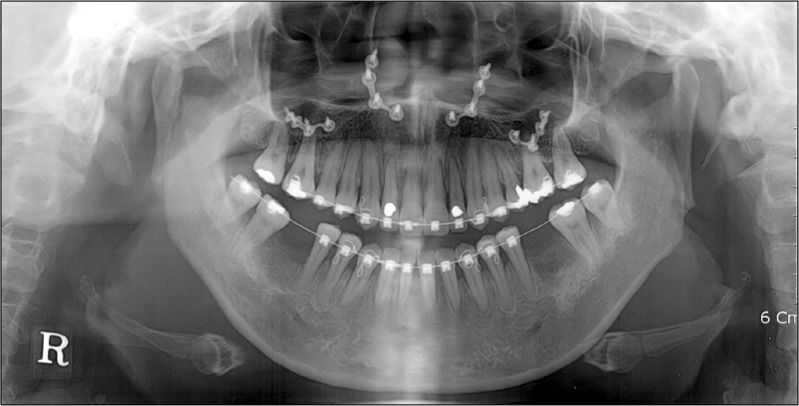
Fig. 2.
Ten weeks after the orthognathic surgery, panoramic radiograph, showing discontinuity of proximal segment by radiolucent lesion.
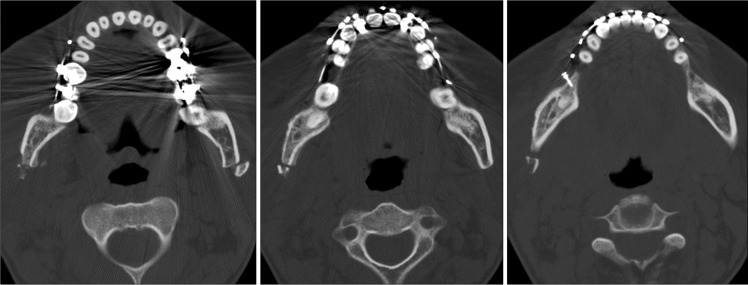
Fig. 3.
Ten weeks after the orthognathic surgery, computed tomography axial view, showing destructive bony changes and erosive cortical layers at the angle of right mandible.
Fig. 4.
Three months after removal of necrotic bone. Post-operative panoramic radiograph.
Discussion
Necrosis of the proximal segment after TOVRO is extremely rare. The case reported by Tuinzing and Greebe [1] does not represent the majority of patients undergoing orthognathic surgery, as their patient’s condition was compromised by systemic illness, including diabetes. In 1976, Bell and Kennedy [4] studied bone healing and revascularization after pedicled and nonpedicled vertical ramus osteotomy using 15 adult Rhesus monkeys. The microangiographic and histologic studies showed osseous union, minimal osteonecrosis, and minimal vascular ischemia when the proximal condylar segment is pedicled to the articular capsule and lateral pterygoid muscle. In contrast, when the proximal segment is not pedicled to soft tissue, there were complications including intraosseous necrosis, vascular ischemia, and delayed healing. Bell and Kennedy [4] believed that necrosis or non-union of the inferior portion of proximal segments can be prevented by creating the osteotomy more posterior and above the gonial angles. However, this study is based on intraosseous circulation and viability based on microangiographic and histologic evaluation. Therefore, it is difficult to predict the extent of proximal segment necrosis in clinical practice.
In 1980, Lownie et al. [5] performed L-osteotomy and C-osteotomy on 10 baboons and observed the effects of disrupting the blood supply of the baboon mandible. The contralateral (control) side was not osteomized. The lateral pterygoid muscles were left attached, the periosteum on the lateral surface was raised, and a silastic sheet was placed to prevent reattachment of the periosteum. Fourteen days post-operatively, the mandibles were removed and examined histologically. Surprisingly, avascular necrosis was evident even on the control side. This study contradicts Bell and Kennedy’s [4] conclusion that necrosis of proximal segments can be prevented as long as the lateral pterygoid attachment is maintained. Instead, Lownie et al. [5] demonstrated the importance of periosteum reattachment as well as temporomandibular joint capsule and lateral pterygoid muscle attachment to prevent avascular necrosis of the bony segments.
In addition, vertical ramus osteotomy for correcting mandibular prognathism involves the posteriorly positioned distal segments with bony segments overlap. It is a common technique to detach the muscles of mastication except the temporomandibular joint capsule and lateral pterygoid muscles to ease the reposition of the bony segments. Park [6] reported that detachment of those muscles does not affect the normal healing of the proximal segments and anticipated no complication associated with low blood supply. Considering all factors, the authors believe that the blood supply to the bony segments is re-established as long as the periosteum reattaches in the setting of surgical detachment of most muscles of mastication. Transient ischemia of the bony segments can occur in the initial healing phase, but the revascularization and normal healing process follows unless the transient ischemia is prolonged by damage to the periosteum inhibiting the reattachment, or systemic illness such as diabetes delaying wound healing.
The authors report a rare case of a partial osteonecrosis of mandibular proximal segment following a routine TOVRO procedure. The patient was a healthy individual without any systemic diseases or conditions that could delay wound healing. The operative note describes the surgical technique involving a preservation of temporomandibular joint capsule and lateral pterygoid muscle attachment. The surgeon said that the patient had severe swelling after surgery due to bleeding from the masseteric artery during surgery. There was a large cleft between the end of proximal segment and distal segment in the post-operative day 2 panoramic radiograph (Fig. 1), so that end of the proximal segment may have overstepped the bounds of mucoperiosteum, The etiology of a rare osteonecrosis of the bony segment on this healthy patient after the routine operation is unclear, but we may assume that osteonecrosis can be caused by ischemia due to detachment of periosteum and hematoma formation. Consequently surgeons must be aware and conscientious about a rare potential complication of osteonecrosis following orthognathic surgery.
Acknowledgments
This study was supported by a grant of the Korea Healthcare technology R&D Project, Ministry for Health, Welfare & Family Affairs, Republic of Korea (A084120).
References
- 1.Tuinzing DB, Greebe RB. Complications related to the intraoral vertical ramus osteotomy. Int J Oral Surg. 1985;14:319–24. doi: 10.1016/s0300-9785(85)80020-x. [DOI] [PubMed] [Google Scholar]
- 2.Lanigan DT, West RA. Aseptic necrosis of the mandible: report of two cases. J Oral Maxillofac Surg. 1990;48:296–300. doi: 10.1016/0278-2391(90)90397-k. [DOI] [PubMed] [Google Scholar]
- 3.Quinn PD, Wedell D. Complications from intraoral vertical subsigmoid osteotomy: review of literature and report of two cases. Int J Adult Orthodon Orthognath Surg. 1988;3:189–96. [PubMed] [Google Scholar]
- 4.Bell WH, Kennedy JW., 3rd Biological basis for vertical ramus osteotomies--a study of bone healing and revascularization in adult rhesus monkeys. J Oral Surg. 1976;34:215–24. [PubMed] [Google Scholar]
- 5.Lownie JF, Cleaton-Jones PE, Austin JC, Vieira EG, Reitzik M. Avascular necrosis of the mandibular ramus in the baboon (Papio ursinus) following orthognathic surgery. Int J Oral Surg. 1980;9:206–15. doi: 10.1016/s0300-9785(80)80020-2. [DOI] [PubMed] [Google Scholar]
- 6.Park HS. Transoral vertical ramus osteotomy. In: Fonseca RM, Turvey TA, Marciani RD, editors. Oral and maxillofacial surgery. 2nd ed. St Louis: Elsevier; 2009. pp. 119–36. [Google Scholar]