Abstract
Purpose:
The efficiency of an anchor plate placed during orthognathic surgery via minimal presurgical orthodontic treatment was evaluated by analyzing the mandibular relapse rate and dental changes.
Methods:
The subjects included nine patients with Class III malocclusion who had bilateral sagittal split osteotomy at the Division of Oral and Maxillofacial Surgery, Department of Dentistry in Ajou University Hospital, after minimal presurgical orthodontic treatment. During orthognathic surgery, anchor plates were placed at both maxillary buttresses. The anchor plates were used to move maxillary teeth backward and for maximum anchorage of Class III elastics to minimize mandibular relapse during the postoperative orthodontic treatment. The lateral cephalometric X-ray was taken preoperatively (T0), postoperatively (T1), and one year after the surgery (T2). Seven measurements (distance from Pogonion to line Nasion-Nasion perpendicular [Pog-N Per.], angle of line B point-Nasion and Nasion-Sella [SNB], angle of line maxilla 1 root-maxilla 1 crown and Nasion-Sella [U1 to SN], distance from maxilla 1 crown to line A point-Nasion [U1 to NA], overbite, overjet, and interincisal angle) were taken. Measurements at T0 to T1 and T1 to T2 were compared and differences tested by standard statistical methods.
Results:
The mean skeletal change was posterior movement by 13.87±4.95 mm based on pogonion from T0 to T1, and anterior movement by 1.54±2.18 mm from T1 to T2, showing relapse of about 10.2%. There were significant changes from T0 to T1 for both Pog-N Per. and SNB (P <0.05). However, there were no statistically significant changes from T1 to T2 for both Pog-N Per. and SNB. U1 to NA that represents the anterior-posterior changes of maxillary incisor did not differ from T0 to T1, yet there was a significant change from T1 to T2 (P <0.05).
Conclusion:
This study found that the anchor plate minimizes mandibular relapse and moves the maxillary teeth backward during the postoperative orthodontic treatment. Thus, we conclude that the anchor plate is clinically very useful.
Keywords: Orthodontic anchorage, Bone plate, Efficiency, Orthodontic treatment, Orthognathic surgery
Introduction
Conventionally, orthognathic surgery is performed after decompensation of teeth by presurgical orthodontic treatment, followed by postoperative orthodontic treatment. However, facial status may worsen owing to decompensation of teeth during the presurgical orthodontic treatment, increasing patient dissatisfaction. Also, such treatment places force in a direction countering the musculoskeletal system, making treatment very difficult for dentists. Thus, there are ongoing efforts to reduce the duration of presurgical orthodontic treatment. Surgery First Approach [1–4] or minimal presurgical orthodontic treatment [5,6] is capable of reducing the treatment period and improving patient satisfaction. Minimal presurgical orthodontic treatment refers to performing the surgery when the minimum conditions set prior to orthognathic surgery are achieved. The minimum conditions include removing uncertainty of the amount and direction of teeth movement after the surgery, of 3-dimensional changes of the mandible, of the location of the presurgical condyle, and removing occlusal interference that hinders skeletal improvement. However, it is impossible to fully satisfy these conditions, and the uncertainty of skeletal and dental status after the surgery is inevitable to a certain degree. If the surgery is scheduled in advance without sufficient preparation, the mandible may change in an unexpected direction after the surgery due to unstable occlusion, and the postoperative orthodontic treatment will last longer than planned, or the functional occlusion or aesthetic treatment goals cannot be fulfilled as expected [5,7]. Considering these problems, this study is focused on placing the anchor plate (Fig. 1), one of the skeletal anchorage systems (SAS), during the orthognathic surgery for postoperative orthodontic treatment, to shorten the treatment time via minimal presurgical orthodontic treatment and stabilize unstable occlusion as fast as possible after the surgery to minimize mandibular relapse. According to several studies, when orthognathic surgery is directly impacting bone, a quick reaction of skeletal parts is caused by a phenomenon called regional acceleratory phenomenon (RAP) [1,8]. When such phenomena are used actively, teeth movement can be fulfilled easily, reducing the time required for postoperative orthodontic treatment. The anchor plate [9], as a SAS, is an innovative material for orthodontic treatment of a severe malocclusion. Nagasaka et al. [3] and Villegas et al. [4] proved that the result of surgery using the anchor plate for postoperative orthodontic treatment was outstanding.
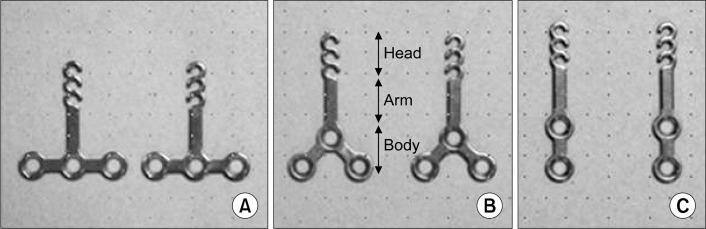
Fig. 1.
Skeletal anchorage system titanium anchor plates. (A) T-plate, (B) Y-plate, (C) I-plate. The head component has three continuous hooks for attachment of orthodontic forces. The arm component is transmucosal and is available in three different lengths to accommodate individual morphological differences. The body component is positioned subperiosteally and is available in three different configurations.
The clinical efficiency of anchor plate placed simultaneously in orthognathic surgery via minimal presurgical orthodontic treatment was evaluated by analyzing the mandibular relapse rate and dental changes.
Materials and Methods
The subjects are nine patients with Class III malocclusion who had bilateral sagittal split osteotomy at the Division of Oral and Maxillofacial Surgery, Department of Dentistry in Ajou University Hospital, after minimal presurgical orthodontic treatment. One surgeon for the Oral and Maxillofacial Surgery Department performed orthognathic surgery and a single orthodontist conducted orthodontic treatment for all patients. The anchor plate was placed at both maxillary buttresses during the orthognathic surgery (Fig. 2). The anchor plate was used to move maxillary teeth backward and for maximum anchorage of Class III elastics to the mandible, to minimize mandibular relapse during the postoperative orthodonic treatment. An anchor plate is divided into a head, arm, and body, and can be classified into T-plate, Y-plate and I-plate depending on the body shape. For the study, our hospital used the Y-plate (Fig. 1). The head is composed of three consecutive hooks, and elastic is placed on the hook to move teeth. The hook should be placed at the same height as the bracket, and it is important that it is spaced from the teeth, so that it does not interfere with the teeth movement. Since the measuring point used for analyses of mandibular relapse changes, 10 patients with genioplasty were excluded from the study and nine patients were finalized as the subjects. Maxillary first premolars on both sides were extracted for presurgical orthodontic treatment of eight out of nine patients, all of whom were female patients. The remaining patient was a male whose teeth were not extracted. After maxillomandibular fixation of patients for two weeks, postoperative orthodontic treatment began three weeks after surgery.
Fig. 2.

Clinical picture of the anchor plates placed at both maxillary parts. Hook is at the same height as that of bracket, and it has a space between the teeth.
A cephalometer was used to take the lateral cephalometric x-ray of preoperatively (T0), postoperatively (T1), and one year after the surgery (T2) (Fig. 3). When taking the x-ray, Frankfort horizontal line was in parallel to the floor and the patients were at the centric occlusion status. One investigator set the measuring points using V-ceph 6.0 (Cybermed, Seoul, Korea) and seven variables were measured (Fig. 4). ‘Distance from Pogonion to line Nasion-Nasion perpendicular (Pog-N Per.)’ and ‘angle of line B point-Nasion and Nasion-Sella (SNB)’ as the skeletal anterior-posterior values were measured for each period (T0, T1, and T2), to identify the postoperative mandibular changes and relapse rate. ‘Angle of line maxilla 1 root-maxilla 1 crown and Nasion-Sella (U1 to SN) (degree)’ and ‘distance from maxilla 1 crown to line A point-Nasion (U1 to NA) (mm)’ for each period of T0, T1, and T2 were measured to identify the angle changes of maxillary incisors and anterior-posterior changes. Finally, ‘overbite’, ‘overjet’, and ‘interincisal angle’ were measured at the period of T0, T1, and T2 to examine overbite, overjet, and interincisal angle changes. Differences between T0 to T1 and T1 to T2 for all measured parameters were assessed using paired t-tests, calculated with the PASW Statistics 18.0 statistical package (IBM Co., Armonk, NY, USA). Null hypotheses of no difference were rejected if P -values were less than 0.05.
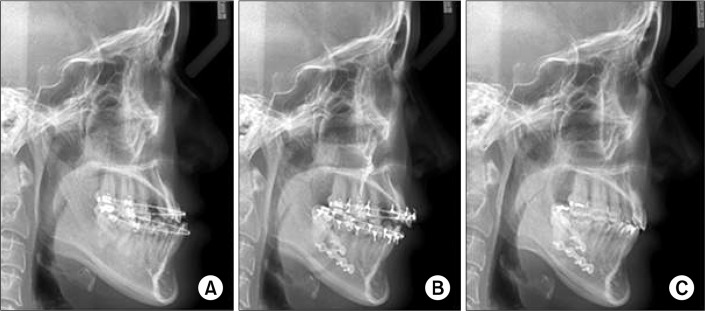
Fig. 3.
(A) Lateral cephalometric x-ray after the completion of the minimal presurgical orthodontic treatment. (B) Lateral cephalometric x-ray right after orthognathic surgery. The anchor plate placed in the maxillary buttress area can be observed. (C) Lateral cephalometric x-ray after one year of orthognathic surgery.
Fig. 4.
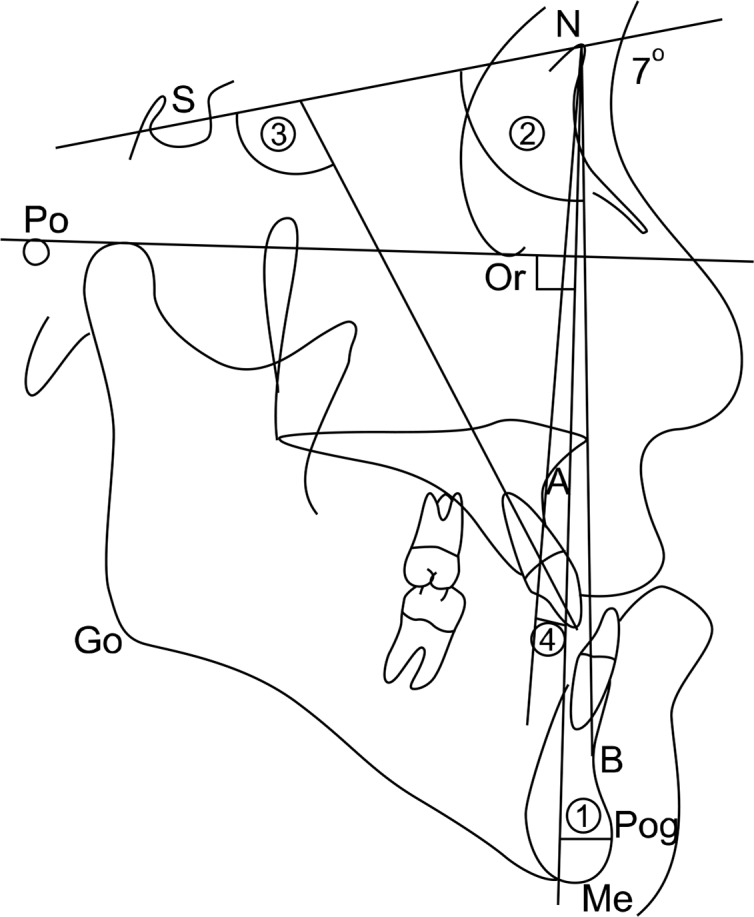
Measurement items. Anterior/posterior skeletal relationship: ① Pog-N perpendicular (mm), ② SNB (degree). Dental relationship: ③ U1 to SN (degree), ④ U1 to NA (mm), ⑤ overbite (mm), ⑥ overjet (mm), ⑦ interincisal angle (degree). S, Sella (center of sella trucica); N, Nasion (anterior point on the frontonasal suture); Po, Porion (the midpoint of th upper contour of the external auditory canal); Or, Orbitale (a point midway between the lowest point on the inferior margin of the two orbits); A, A point (deepest point on the concave outline of the upper labial alveolar process); B, B point (the deepest point on the bony curvature between the crest of the alveolus and the pogonion); Go, Gonion (the midpoint at the angle of the mandible); Pog, Pogonion (the most anterior point on the madibular symphysis); Me, Menton (the lowest point on the lower border of the mandibular symphysis).
This study was reviewed and approved by the Institutional Review Board at the Ajou University Hospital (AJIRB-MED-MDB-14-089).
Results
The mean skeletal change after orthognathic surgery from T0 to T1 was posterior movement of 13.87±4.95 mm from the mandible based on Pog, and from T1 to T2 was anterior movement of 1.54±2.18 mm from the mandible based on Pog. The mean skeletal change after one year of orthognathic surgery (T0∼T2) was posterior movement of 12.32±4.60 mm from the mandible based on Pog (Table 1).
Table 1.
Means and comparisons preoperatively (T0), postoperatively (T1), 1 year after surgery (T2)
| Measurement | T0∼T1 | P-value | T1∼T2 | P-value | ||
|---|---|---|---|---|---|---|
|
|
|
|||||
| T0 | T1 | T1 | T2 | |||
| AP skeletal relationship | ||||||
| Pog-N Per. (mm) | 7.42±2.70 | −6.45±3.16 | 0.000* | −6.45±3.16 | −4.90±2.82 | 0.066 |
| SNB (degree) | 82.40±3.85 | 78.09±4.01 | 0.001* | 78.09±4.01 | 77.90±4.14 | 0.758 |
| Dental relationship | ||||||
| U1 to SN (degree) | 110.72±9.47 | 108.80±10.24 | 0.316 | 108.80±10.24 | 105.33±8.73 | 0.138 |
| U1 to NA (mm) | 8.25±4.58 | 8.04±5.11 | 0.747 | 8.04±5.11 | 4.98±5.02 | 0.036* |
| Overbite (mm) | −0.09±1.82 | −0.25±2.04 | 0.847 | −0.25±2.04 | 1.28±1.50 | 0.158 |
| Overjet (mm) | −3.40±3.71 | 8.74±2.42 | 0.000* | 8.74±2.42 | 4.39±1.29 | 0.001* |
| Interincisal angle (degree) | 118.93±10.19 | 123.30±8.64 | 0.021* | 123.30±8.64 | 125.60±8.27 | 0.405 |
Values are presented as mean±standard deviation.
AP, anteroposterior; Pog, Pogonion; N, Nasion; Per, perpendicular; S, Sella; B, basion; U1, upper central incisior; A, A point.
Statistically significant (P<0.05).
There were significant anterior-posterior mandibular changes from T0 to T1 for both Pog-N Per. and SNB (P <0.05; Table 1), but none from T1 to T2 for Pog-N Per. and SNB.
There was no dental change (U1 to SN, the angle changes of maxillary incisor, and overbite) T0, T1, and T2. U1 to NA (anterior-posterior changes of maxillary incisor) did not change from T0 to T1, yet there was a significant change from T1 to T2 (P <0.05; Table 1). There was a significant change in overjet from T0 to T1, and T2 and in interincisal angle from T0 to T1 (P <0.05; Table 1). However, there was no difference in interincisal angle from T1 to T2.
Discussion
Conventional presurgical orthodontic treatment is capable of producing stable occlusion after surgery, increasing skeletal stability after surgery and improving patient cooperation during the presurgical orthodontic treatment. However, most patients claim the orthodontic device is inconvenient, report discomfort during mastication, and dislike the worsened facial appearance and lengthy treatment.
In contrast, minimal presurgical orthodontic treatment [6] sets the minimum goals for orthognathic surgery and fulfills them during the presurgical orthodontic treatment so that the overall treatment period is shortened and more stable occlusion can be realized, minimizing the skeletal relapse that may occur after surgery. Shortened treatment duration not only reduces the duration of presurgical orthodontic treatment, but also for improving the bone metabolism after surgery. Several studies have reported that when orthognathic surgery is directly impacting bone, a quick reaction of skeletal parts is caused by a phenomenon called RAP [1,8]. RAP increases bone metabolism and reduces local bone density through complicated physiological processes including change to the composition of osteoblast and osteoclast, formation of new blood vessels and calcification, although the biologic mechanism is not understood. Yaffe et al. [8] reported that RAP lasts for about four months right after the surgery. Therefore, it is important to utilize the period as much as possible for quick teeth movement.
The introduction of a SAS resulted in a tremendous paradigm change in the field of orthodontics. Since orthodontic force acts directly on the teeeth by the intraosseous anchorage, severe malocclusion that is complicated and difficult to resolve by existing orthodontic treatments can be treated and three dimensional teeth movement becomes possible [9]. When such material is used for postoperative orthodontic treatment, the result is effective movement of teeth and a good prognosis of orthognathic surgery.
Study results show that the mean posterior change of mandible was 13.87±4.95 mm based on pogonion, and the mean anterior change of mandible from T1 to T2, in other words, the relapse, was 1.54±2.18 mm, equivalent to around 10.2% of relapse rate. Examining published study results on relapse rates, this is significantly low. In addition, the changes of SNB angle based on B point was posterior mandibular movement of −4.31°±2.46° in average from T0 to T1, and around 0.19°±1.75° from T1 to T2, showing a very slight change. There was no significant difference in SNB angles from T1 to T2.
Many researchers have conducted studies on postoperative relapse rate for patients who had bilateral sagittal split osteotomy. Ingervall et al. [10] selected 29 patients in 1995 and examined the postoperative relapse rate. The amount of mandibular set back was 6.0 mm in average, the relapse was 1.1 to 1.3 mm, and relapse rate is around 18% 14 months after the surgery. Mobarak et al. [11] examined 80 prognathism patients in 2000 and found that the relapse rate six months following the surgery was 19% at B point and 26% at pogonion. Such relapse occurred within six months following the surgery (72%). Dolce et al. [12] reported that the relapse rate one year after surgery was 12.1% for prognathism patients. Kwon et al. [13] stated that the relapse rate one year following surgery was 16% at B point and 18% at pogonion when 30 prognathism patients were examined. Hwang et al. [14] examined 32 patients in 2011 who had two-jaw surgery without pre-operative orthodontic treatment, and reported that their relapse rate was 11.6% six months after surgery. According to a study on relapse degree following orthognathic surgery based on duration of the preoperative orthodontic treatment after extracting both maxillary first premolars of prognathism patients [5], a group with shorter preoperative orthodontic treatment showed more counterclockwise rotation and relapse of mandible. In another study [7] of the mandibular relapse degree between a group with the surgery first approach and a group with conventional surgery, operative stability was lower in the former group. In addition, the degree of mandibular relapse was higher. In contrast, a comparison of changes to the soft and hard tissue following the two-jaw surgery of prognathism patients between a group with the minimal presurgical orthodontic treatment and a group with the conventional presurgical orthodontic treatment [6], found no significant difference between groups. The authors concluded that minimal presurgical orthodontic treatment can be recommended as long as accurate diagnosis and treatment plans are established. In another study [15], the relapse rate of the surgery first approach was compared with that of preoperative orthodontic treatment following orthognathic surgery. The rate of the surgery first approach patients was 14.3% and that of the preoperative orthodontic treatment group was 15.7%, no statistically significant difference. The stability of jaw bone and occlusion after surgery whether by the conventional preoperative orthodontic treatment, minimal presurgical orthodontic treatment, and surgery first approach varies broadly across studies. Thus, it is necessary to ensure skeletal and dental stability during the postoperative orthodontic treatment to minimize potential instability and it is essential to have intraosseous anchorage sources such as anchor plates.
Our hospital conducts minimal presurgical orthodontic treatment following orthognathic surgery. Anchor plates are placed at both maxillary buttresses during the surgery to quickly stabilize unstable occlusion relations. There are many benefits to placing anchor plates during orthognathic surgery. First, an operating field is sufficient for a surgeon to place anchor plates at a desired location: the thick, firm part of maxillary bone. Second, about three weeks are required until loading after placement of anchor plates, and since it compensates for the duration required for recovery after orthognathic surgery, the time for postoperative orthodontic treatment can be set earlier. Third, teeth movement by orthodontic force for around four months following orthognathic surgery can be rapid [8]. If that period is used efficiently, the duration for postoperative orthodontic treatment can be shortened. Fourth, it is possible to achieve stable occlusion status quickly after orthognathic surgery with the first surgery approach or the minimal presurgical orthodontic treatment. Fifth, no additional surgical treatment is required for placement of anchor plates. Sixth, it is easy to change the location of anchor plates if they are not properly placed.
While the low relapse rate in this study may have several causes, anchor plates greatly contributed to inhibiting anterior mandibular movement after surgery, providing maximum anchorage of Class III elastics. Furthermore, in most study patients, the maxillary premolars were extracted and the mandibular teeth were not extracted, so considerable posterior movement of maxillary incisors could be observed as postoperative orthodontic treatment was under progress. Overjet was −3.40±3.71 mm under crossbite status T0 and 8.74±2.42 mm T1, greatly different from the occlusion of orthognathic surgery through conventional preoperative orthodontic treatment. This was reduced to 4.39±1.29 mm T2, possibly resulting from posterior movement of maxillary incisors and decompensation of mandibular incisors. Moreover, overbite and interincisal angle of T2 were balanced, showing that stable occlusion status was fulfilled. This is because the anchor plates are firmly placed at both maxillary buttresses as the intraosseous anchorage and the hook of anchor plates is placed at the same height as that of the maxillary teeth’s bracket, allowing natural movement not restricting the physiological movement of teeth and making easier teeth movement. A study of SAS placed for posterior movement of maxillary teeth [16] noted the success rate was about 97%, and surgical success resulted from minimal invasiveness and placement of plates at a firm area. When anchor plates are placed upon orthognathic surgery, surgical and treatment success rates are higher.
Anchor plates greatly contribute to the stability of mandible and occlusion after surgery. In particular, it is essential for orthognathic surgery conducted after the minimal presurgical orthodontic treatment or for surgery first approach. The conclusion is that anchor plates are clinically useful in minimizing mandibular relapse, allowing efficient teeth movement as RAP stage occurring after orthognathic surgery is used properly and actively.
Conclusion
When anchor plates were placed at the maxillary buttress area of Class III malocclusion patients upon bilateral sagittal split osteotomy after minimal presurgical orthodontic treatment following the postoperative orthodontic treatment, the mandible relapse rate was significantly lower than that of published studies and the maxillary incisors were effectively moved within a short time. Minimal presurgical orthodontic treatment reduced instability of mandible and teeth and anchor plates acted as the maximum anchorage of Class III elastic, decreasing anterior movement of mandible after the surgery. Furthermore, the hook of anchor plates was located at the same height as that of the maxillary teeth’s bracket and teeth movement were quick and stable owing to RAP, greatly contributing to forming a stable occlusion after surgery. However, there are some limitations to this study. It is difficult to place anchor plates at maxillary buttresses during two-jaw surgery and there is no measurement of vertical skeletal changes. Also, there are no cases of patients with Class II malocclusion. Thus, further studies are necessary.
References
- 1.Liou EJ, Chen PH, Wang YC, Yu CC, Huang CS, Chen YR. Surgery-first accelerated orthognathic surgery: postoperative rapid orthodontic tooth movement. J Oral Maxillofac Surg. 2011;69:781–5. doi: 10.1016/j.joms.2010.10.035. [DOI] [PubMed] [Google Scholar]
- 2.Yu CC, Chen PH, Liou EJ, Huang CS, Chen YR. A Surgery-first approach in surgical-orthodontic treatment of mandibular prognathism--a case report. Chang Gung Med J. 2010;33:699–705. [PubMed] [Google Scholar]
- 3.Nagasaka H, Sugawara J, Kawamura H, Nanda R. “Surgery first” skeletal Class III correction using the Skeletal Anchorage System. J Clin Orthod. 2009;43:97–105. [PubMed] [Google Scholar]
- 4.Villegas C, Uribe F, Sugawara J, Nanda R. Expedited correction of significant dentofacial asymmetry using a “surgery first” approach. J Clin Orthod. 2010;44:97–103. [PubMed] [Google Scholar]
- 5.Kim JW, Lee NK, Yun PY, Moon SW, Kim YK. Postsurgical stability after mandibular setback surgery with minimal orthodontic preparation following upper premolar extraction. J Oral Maxillofac Surg. 2013;71:1968.e1–1968.e11. doi: 10.1016/j.joms.2013.07.004. [DOI] [PubMed] [Google Scholar]
- 6.Joh B, Bayome M, Park JH, Park JU, Kim Y, Kook YA. Evaluation of minimal versus conventional presurgical orthodontics in skeletal class III patients treated with two-jaw surgery. J Oral Maxillofac Surg. 2013;71:1733–41. doi: 10.1016/j.joms.2013.06.191. [DOI] [PubMed] [Google Scholar]
- 7.Kim CS, Lee SC, Kyung HM, Park HS, Kwon TG. Stability of mandibular setback surgery with and without presurgical orthodontics. J Oral Maxillofac Surg. 2014;72:779–87. doi: 10.1016/j.joms.2013.09.033. [DOI] [PubMed] [Google Scholar]
- 8.Yaffe A, Fine N, Binderman I. Regional accelerated phenomenon in the mandible following mucoperiosteal flap surgery. J Periodontol. 1994;65:79–83. doi: 10.1902/jop.1994.65.1.79. [DOI] [PubMed] [Google Scholar]
- 9.Sugawara J, Nishimura M. Minibone plates: the skeletal anchorage system. Semin Orthod. 2005;11:47–56. [Google Scholar]
- 10.Ingervall B, Thüer U, Vuillemin T. Stability and effect on the soft tissue profile of mandibular setback with sagittal split osteotomy and rigid internal fixation. Int J Adult Orthodon Orthognath Surg. 1995;10:15–25. [PubMed] [Google Scholar]
- 11.Mobarak KA, Krogstad O, Espeland L, Lyberg T. Long-term stability of mandibular setback surgery: a follow-up of 80 bilateral sagittal split osteotomy patients. Int J Adult Orthodon Orthognath Surg. 2000;15:83–95. [PubMed] [Google Scholar]
- 12.Dolce C, Hatch JP, Van Sickels JE, Rugh JD. Rigid versus wire fixation for mandibular advancement: skeletal and dental changes after 5 years. Am J Orthod Dentofacial Orthop. 2002;121:610–9. doi: 10.1067/mod.2002.123341. [DOI] [PubMed] [Google Scholar]
- 13.Kwon TK, Kim YD, Shin SH, Kim UK, Kim JR, Chung IK. Stability after surgical correction of mandibular prognathism using bilateral saggital split ramus osteotomy and fixation with Poly-L/DL-Lactide copolymer screws (biosorbTMFX) J Korean Assoc Maxillofac Plast Reconstr Surg. 2005;27:160–3. [Google Scholar]
- 14.Hwang DS, Kim YI, Lee JY, et al. Evaluation of skeletal stability following two-jaw surgery via surgery first orthodontic treatment in class III malocclusion. J Korean Assoc Maxillofac Plast Reconstr Surg. 2011;33:407–12. [Google Scholar]
- 15.Ko EW, Hsu SS, Hsieh HY, Wang YC, Huang CS, Chen YR. Comparison of progressive cephalometric changes and post-surgical stability of skeletal Class III correction with and without presurgical orthodontic treatment. J Oral Maxillofac Surg. 2011;69:1469–77. doi: 10.1016/j.joms.2010.07.022. [DOI] [PubMed] [Google Scholar]
- 16.De Clerck EE, Swennen GR. Success rate of miniplate anchorage for bone anchored maxillary protraction. Angle Orthod. 2011;81:1010–3. doi: 10.2319/012311-47.1. [DOI] [PMC free article] [PubMed] [Google Scholar]