Abstract
Introduction: The aim of this study was to investigate the morphological changes of human dentin after Erbium-Doped Yttrium Aluminum Garnet (Er:YAG), Carbon Dioxide(CO2) laser-irradiation and acid-etching by means of scanning electron microscopic (SEM)
Methods: 9 extracted human third molars were used in this study. The teeth were divided in three groups: first group, CO2 laser with power of 1.5 w and frequency of 80 Hz; second group, Er:YAG laser with output power of 1.5 W frequency of 10 Hz, very short pulse with water and air spray was applied; and third group, samples were prepared by acid-etching 37% for 15 sec and rinsed with air-water spray for 20 sec. Then, the samples were prepared for SEM examination.
Results: Melting and cracks can be observed in CO2 laser but in Er:YAG laser cleanedablated surfaces and exposed dentinal tubules, without smear layer was seen.
Conclusion: It can be concluded that Er:YAG laser can be an alternative technique for surface treatment and can be considered as safe as the conventional methods. But CO2 laser has some thermal side effects which make this device unsuitable for this purpose.
Keywords: CO2 laser, Er:YAG lasers, morphological changes, SEM
Introduction
The development of new caries removal, cavity preparation methods and new restorative materials has been the goal of modern restorative dentistry, aiming for conservative and esthetic restorations that are acceptable by patients (1,2,3). Among modern technologies for cavity preparation and surface modification, use of hard tissue lasers have gained special attention. The conventional mechanical methods for caries removal like using a high-speed drill have some disadvantages such as the nonselective removal of hard tissue, discomfort for patients because of metallic sound and bone conducted vibration and the need for anesthesia. On the other hand, bactericidal effect of lasers makes them more useful than conventional high speed handpiece (4,5,6).
Erbium family lasers with two different wavelengths (2940 nm, 2780 nm) have a high absorption in water and hydroxyapatite that make these lasers suitable for removal of carious enamel and dentin without any damage to surrounding tissue (7,8). When other lasers like Carbon Dioxide (CO2) andNeodymium- Doped Yttrium Aluminium Garnet (Nd:YAG) lasers were used for surface conditioning, thermal side effects such as melting, carbonization, fissures and cracks occured in the surrounding tissue and also increase in pulpal temperature was observed (9,10).
The aim of etching is to remove the external layer and cause microscopic irregularities which lead to penetration of adhesives in order to obtain retention. So, assessing the surface structure after applying different techniques is important (11).
The aim of this study was to investigate the morphological changes of Er:YAG, CO2 laser-irradiated and acid-etching by means of SEM (scanning electron microscopy).
Methods
9 extracted human third molars were used in this study. Crowns with caries, restorations and fractured were excluded. The remaining soft tissue was removed from the teeth surface with a dental scalar (Sonic flex 2000, kavo, Biberach, Germany). All teeth were then stored in 4°C distilled water containing 0.2% thymol to inhibit microbial growth until use. The surface of the crown was cut fully hydrated, perpendicular to the long axis of the teeth to remove the enamel and expose the dentin surface. Then, surfaces of the samples were wet-polished to 600 grits (silicon carbide).
Following that the teeth were divided in three groups:
In the first group, CO2 laser (US-20D, DEKA, Italy) with an emission wavelength of 10600 nm was used. The laser was used with power of 1.5 w and frequency of 80 Hz by sweeping motion until the whole surface was irradiated.
In the second group, Erbium-Doped Yttrium Aluminum Garnet (Er:YAG) laser (2940D plus, Deka, Italy) with output power of 1.5 W and frequency of 10 Hz(energy of 150 mJ), very short pulse (230 μs) with water and air spray was applied.
In the third group, samples were prepared by acidetching 37% (Etch Royale, Pulpdent,USA) for 15 sec and rinsed with air-water spray for 20 sec.
The samples were prepared for scanning electron microscopic (SEM) examination.
For SEM analysis, samples were fixed in 2.5% Glutaraldeheyde for 12 hours (4°C), then dehydrated in ascending grades of ethanol (25-100%). After that, the samples were dried and sputter-coated with gold. The surfaces were analyzed with a scanning electron microscope (DSM 960A).
Results
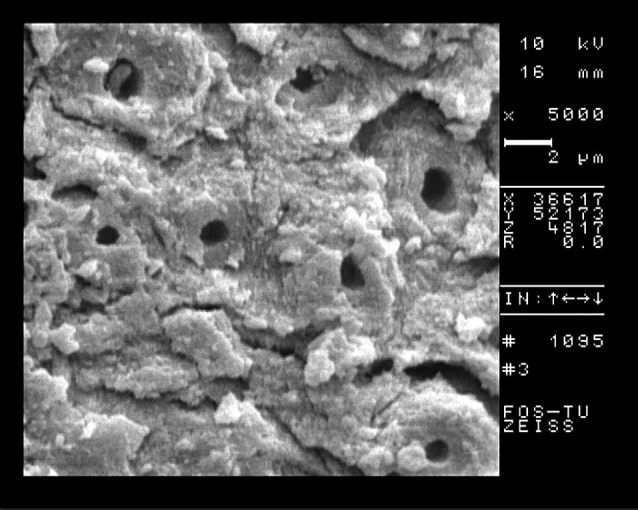
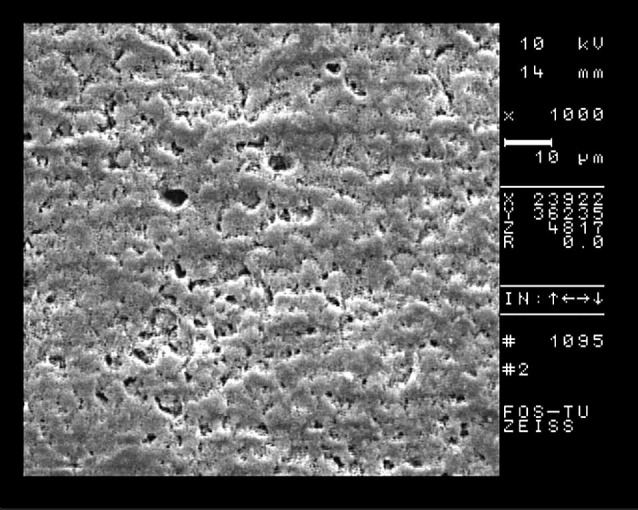
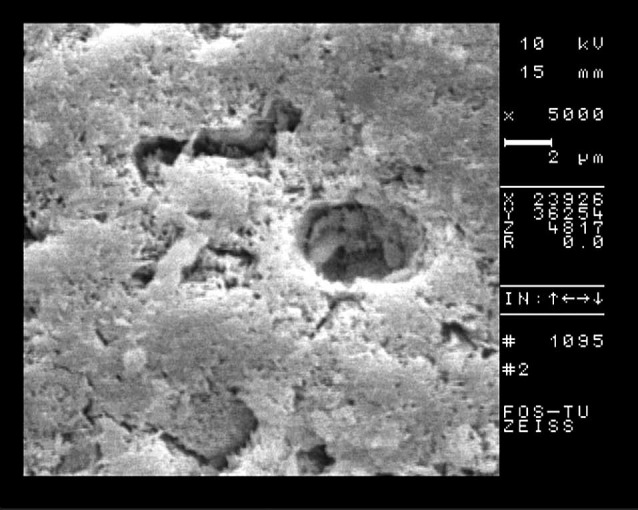
The SEM results of CO2 laser-irradiated human dentin showed some exposed dentinal tubules because of being smear layer on them, having some cracks evidence of thermal damage. (Figure 1) Under SEM evaluation, second group showed cleaned ablated surfaces and exposed dentinal tubules, without smear layer. No burning and melting were seen. (Figure 2)
Figure 1.
(A) Photomicrograph of dentin surface after CO2 laser irradiation. (original magnification ×5000, bar=2μm) (B) Photomicrograph of dentin surface after CO2 laser irradiation. Melting and cracks can be observed. (original magnification ×1000, bar=10μm)
A.
B.
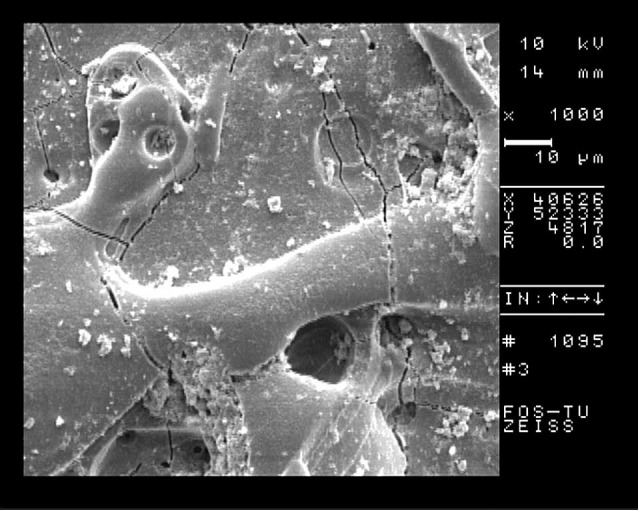
Figure 2.
(A) Surface treated by Er:YAG. Open dentinal tubules, no smear layer, scaly and flake surface was observed. (original magnification ×1000, bar=10μm) (B) Surface treated by Er:YAG (Higher magnification), Open tubules with remainig peritubular dentin (original magnification ×5000, bar=2μm)
A.
B.
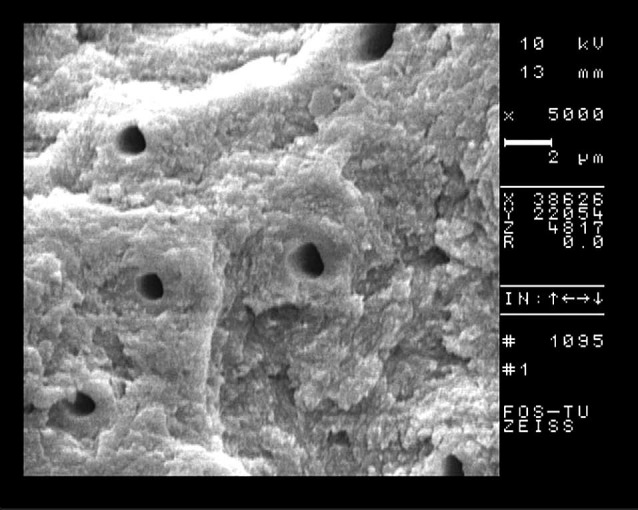
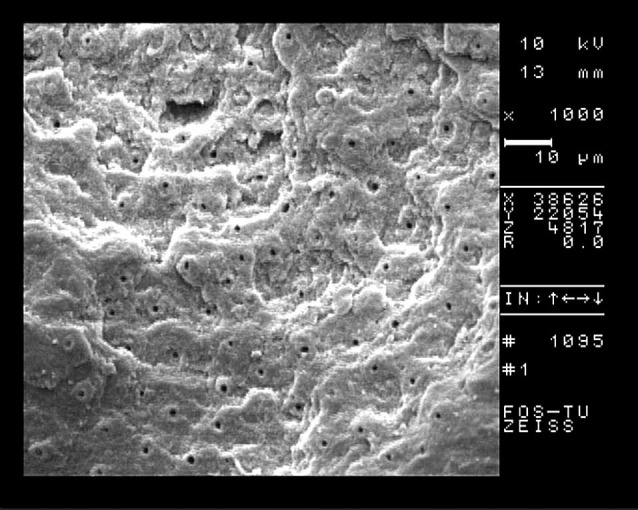
In the third group, there was much smear layer on tubules so they weren’t exposed enough. (Figure 3)
Figure 3.
(A) Acid-etch surface. The surface was covered by smear layer and debris. (original magnification ×1000, bar=10μm) (B) Acidetch surface. Smear layer and debris could be observed around dentinal tubules. (original magnification ×5000, bar=2μm)
A.
B.
Discussion
Preparation of dental hard surfaces for resin composite restorations is one of the main concerns (12).
In this study, we evaluated the dentin surfaces prepared by different methods through SEM. According to several studies, using Er:YAG laser for dental hard tissue seems to be safe without causing damage to surrounding areas (13). Using Er:YAG laser for surface modification showed irregular surface with no crack and smear layer. These characteristics make this device suitable for resin restorations (14).
The laser initially vaporizes water and other hydrated organic components of the tissue. During this process, the internal pressure increases in the tissue until the explosive destruction of inorganic substances occurs which subsequently forms hydrokinetic forces that can quickly ablate the dental hard tissues. This mechanism of ablation is called hydrokinetic system (4,15).
It was shown that when Er:YAG laser was used by air/water spray, there was no pulpal inflammation compared to conventional methods (16).
In agreement with our results, Ceballos et al. in analyzing the Er:YAG laser treated surfaces showed open dentinal tubules which allowed the development of resin tags (17). Also, Freitas et al. in evaluation of SEM of cavity prepared by Er:YAG laser with different parameters concluded that Er:YAG laser was effective for ablation of hard tissue and could create surfaces irregular with open dentinal tubules without smear layer (18).
Several studies showed that temperature rise during Er:YAG laser irradiation with different powers does not exceed 3°C which is below the threshold safe temperature (5°C) reported by Zach and Cohen (19).
SEM of surface irradiated by Er:YAG laser showed irregular and retentive pattern with scaly surface which is in agreement with previous results (5). But in surfaces treated by acid etch the presence of smear layer could be observed. In CO2 group, thermal side effects such as melting, cracks and fissures could be seen.
The mechanism of CO2 laser on target tissue is the conversion of laser energy in to heat. Different studies showed that CO2 laser with various parameters causes vaporization of water and dental organic components resulted in irregularities, fissures and melting areas (20). Actually, cracks were the result of contraction of the tissue after the loss of water and collagen matrix. So, it seems that the application of CO2 laser is not a good option for surface treatment because of presence of melted area that can influence the adhesion of filling materials (21,22).
Overall, it’s important to use the optimum laser parameters for safe and effective ablation of hard tissue by an expert operator (23).
Conclusion
It can be concluded that Er:YAG laser can be an alternative technique for surface treatment and can be considered as safe as the conventional methods. But CO2 laser has some thermal side effects which make this device unsuitable for this purpose. More studies are needed to evaluate the characteristic of lasertreated surfaces to find the appropriate parameters for restorative procedures and obtain enough information for using materials which can interact properly with irradiated surfaces.
Please cite this article as follows:
Shahabi S, Chiniforush N, Juybanpoor N. Morphological Changes of Human Dentin after Erbium-Doped Yttrium Aluminum Garnet (Er:YAG) and Carbon Dioxide (CO2) Laser Irradiation and Acid-etch Technique: An scanning electron microscopic (SEM) Evaluation. J Lasers Med Sci 2013; 4(1):48-52
References
- 1.Walsh LJ. The current status of laser applications in dentistry. Aust Dent J. 2003;48:146–55. doi: 10.1111/j.1834-7819.2003.tb00025.x. [DOI] [PubMed] [Google Scholar]
- 2.Goldman L, Gray JA, Goldman J, Goldman B, Meyer R. Effect of laser beam impacts on teeth Dentistry. J Am Dent Assoc. 1965;70:601–6. doi: 10.14219/jada.archive.1965.0260. [DOI] [PubMed] [Google Scholar]
- 3.Dederich DN, Bushick RD. Lasers in dentistry. J Am Dent Assoc. 2004;135:204–12. doi: 10.14219/jada.archive.2004.0153. [DOI] [PubMed] [Google Scholar]
- 4.Parker S. Surgical lasers and hard dental tissues. Br Dent J. 2007;202:445–54. doi: 10.1038/bdj.2007.294. [DOI] [PubMed] [Google Scholar]
- 5.Nokhbatolfoghahaie H, Chiniforush N, Shahabi S, Monzavi A. SEM evaluation of tooth surface irradiated by different parameters of Er:YAG laser. J Lasers Med Sci. 2012;3(2):51–5. [Google Scholar]
- 6. Shahabi S, Chiniforush N, Bahramian H, Monzavi A, Baghalian A, Kharazifard MJ. The effect of erbium family laser on tensile bond strength of composite to dentin in comparison with conventional method. Lasers in medical science; 2012 Apr 11. [Epub ahead of print]. [DOI] [PubMed]
- 7.Hibst R. Laser for Caries Removal and Cavity Preparation: State of the Art and Future Directions. J Oral Laser Applications. 2002:203–12. [Google Scholar]
- 8.Lin S, Caputo AA, Eversole LR, Rizoiu L. Topographical characteristics and shear bond strength of tooth surfaces cut with a laser-powered hydrokinetic system. J of Prosthet Dent. 1999;82:451–5. doi: 10.1016/s0022-3913(99)70033-8. [DOI] [PubMed] [Google Scholar]
- 9.Ekworapoj P, Sidhu SK, McCabe JF. Effect of different power parameters of Er,Cr:YSGG laser on human dentine. Laser Med Sci. 2007;22:175–82. doi: 10.1007/s10103-006-0426-6. [DOI] [PubMed] [Google Scholar]
- 10.Shahabi S, Chiniforoush N, Fekrazad R, Fatemi SM. Comparison of tensile bond strength of composite to dentine in conventional or laser prepared-cavities (Er;Cr:YSGG) J Oral Laser Applications. 2010;10:107–10. [Google Scholar]
- 11.Schien MT, Bocangel JS, Nogueira GE, Schien PA. SEM evaluation of the interaction pattern between dentin and resin after cavity preparation using Er:YAG laser. J Dent. 2003;31:127–35. doi: 10.1016/s0300-5712(03)00003-4. [DOI] [PubMed] [Google Scholar]
- 12.Pick RM. Using lasers in clinical dental practice. J Am Dent Assoc. 1993;124:37–47. doi: 10.14219/jada.archive.1993.0027. [DOI] [PubMed] [Google Scholar]
- 13.Ramos ACB, Esteves-Oliveira M, Arana-Chavez VE, de Paula Eduardo C. Adhesives bonded to erbium:yttriumaluminum- garnet laser-irradiated dentin: transmission electron microscopy, scanning electron microscopy and tensile bond strength analysis. Lasers Med Sci. 2008;25:181–9. doi: 10.1007/s10103-008-0600-0. DOI 10.1007/s10103-008-0600-0. [DOI] [PubMed] [Google Scholar]
- 14.Botta SB, da Ana PA, Zezell DM, Powers JM, Matos AB. Adhesion after erbium, chromium: yttrium-scandiumgallium- garnet laser application at three different irradiation conditions. Laser Med Sci. 2009;24(1):67–73. doi: 10.1007/s10103-007-0521-3. [DOI] [PubMed] [Google Scholar]
- 15.Freiberg RJ, Cozean CD. Pulsed erbium laser ablation of hard dental tissue: the effects of atomized water spray versus water surface film. Proc SPIE. 2002;4610:74–84. [Google Scholar]
- 16.Oelgiesser D, Blasbalg J, Ben-Amar A. Cavity preparation by Er:YAG laser on pulpal temperature rise. Am J Dent. 2003;16:96–8. [PubMed] [Google Scholar]
- 17.Ceballos L, Toledano M, Osorio R, Tay FR, Marshal GW. Bonding to Er:YAG laser-treated dentin. J Dent Res. 2002;81:119–22. [PubMed] [Google Scholar]
- 18.Freitas PM, Navarro RS, Barros JA, Eduardo CP. The use of Er:YAG laser for cavity preparation: An SEM evaluation. Microsc Res Tech. 2007;70:803–8. doi: 10.1002/jemt.20470. [DOI] [PubMed] [Google Scholar]
- 19.Zach L, Cohen C. Pulp response to externally applied heat. Oral Surg Oral Med Oral Pathol. 1965;19:515–30. doi: 10.1016/0030-4220(65)90015-0. [DOI] [PubMed] [Google Scholar]
- 20.Marracini TM, Bachmann L, Widgor HA, Walsh JT, Stabholtz Stabholtz, Zezell DM. Morphological evaluation of enamel and dentin irradiated with 96 μm and 294 μm Er:YAG lasers. Laser Phys. 2005;11:551–5. [Google Scholar]
- 21.Steiner-Oliveira C, Rodrigues LKA, Soares LES, Martin AA, Zezell DM, Nobre-dos-Santos M. Chemical, morphological and thermal effects of 106 μm CO2 laser on the inhibition of enamel demineralization. Dent Mater J. 2006;25(3):455–62. doi: 10.4012/dmj.25.455. [DOI] [PubMed] [Google Scholar]
- 22.Nomelini SMB, Gabriel AES, Marchesan MA, Sousa- Neto MD, Silva-Sousa YTC. Ultrastructural analysis of radicular dentine surface submitted to CO2 laser at different parameters. Microsc Research Tech. 2009;72:737–43. doi: 10.1002/jemt.20723. [DOI] [PubMed] [Google Scholar]
- 23.Piccione PJ. Piccione PJDental laser safety. Dent Clin North Am. 2004;48:795–807. doi: 10.1016/j.cden.2004.05.009. [DOI] [PubMed] [Google Scholar]


