Abstract
Introduction: Solar lentigines are among commonest cosmetic problems. There are many topical therapies suggested to treat these lesions including cryotherapy, chemical peeling with tri chloro acetic acid (TCA) and laser therapy with q-switched lasers as well as long pulsed lasers. Considering possible treatment side effects (PIH, scar) with cryotherapy and peeling in Iranian patients (darker skin types) it seems necessary to try to find alternative measures. The aim of the present study was to evaluate effect of long pulsed dye laser (LPDL) on lentigines via an objective method (computerized dermoscopy).
Methods: Patients with pathologically confirmed lentigines were selected if they agreed to participate in the study,were not treated before, hadn’t history of psoriasis, vitiligo, scar formation and were not pregnant. Letigines were dermoscopied before and after treatment with PDL (V-beam, 595nm, Candela Corp. Wayland, USA) using fluence of 10 joules,without DCD (dynamic cooling device) via extra compress lens provided with laser system.The resulting figures were compared by two academic unrelated dermatologists as well as by computerized analysis. Post laser side effects were treated with topical antibiotics and mild topical steroids. Patients were followed for six months after the end of the study to determine the rate of recurrence via dermoscopy of sites of previous lesions and also delayed side effects.
Results: A total of 21 patients with the same number of lesions, were included in the study.Mean age of patients was 54.2 years (±23.3) ranging from 39 to 71 years. Included patient swere 18 females and three males. From 21 treated lesions, 11 were located on the hands and 10 on the face. Comparing before and after photographs taken through dermoscopy system,revealed that approximately 57% of patients had more than 75% improvement. Mean pigment analysis score (calculated by computerized dermoscope software) was respectively 8 and 2 before and after PDL therapy, showing noticeable decrease in pigment density of lesions.Side effects were mild erythema and local irritation responding to topical mild steroids.No hypo or persistent hyper pigmentation or other delayed side effects was seen after six months follow up. One patient experienced transient hyper pigmentation of treatment site after treatment. During six months follow up, no recurrences were seen.
Conclusion: In conclusion, PDL is a safe and effective option to treat lentigines if applied properly using compression method, especially in Iranian patients. However, further studies with larger sample size are required to confirm these results.
Keywords: PDL, lentigines, topical therapies
Introduction
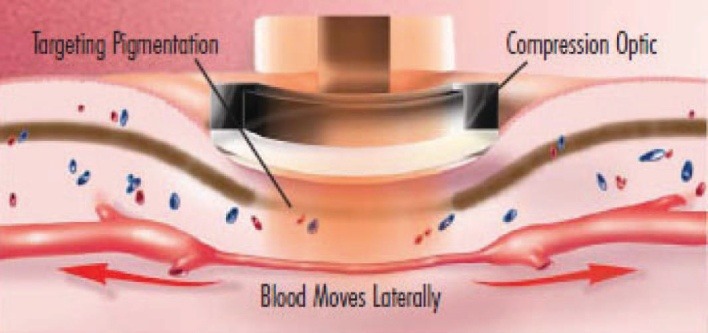
Among pigmented skin lesions, solar lentigines are common and perfect treatments with minimal side effects such as post inflammatory hyper pigmentation, erythema, and hypo pigmentation and in rare situation, scarring could be very interesting. Patients, especially women seeking for these treatments account for a large part of ambulatory dermatologic visits. Hence, development of new therapies with high safety profile to clear these lesions is demanded. Previous studies support this hypothesis that PDL is a good option in treating solar lentigines (1-5). PDL is known as best option for treating vascular lesions including portwine stains and hemangioma. Pressure ‘‘diascopy’’ eliminates blood from cutaneous vessels by coapting the vessel lumen. Removal of blood removes absorption by hemoglobin, making it possible to use the PDL for treating lentigines without purpura, which is indicative of vascular injury. “V-Beam perfecta” PDL apparatus used in the present study is equipped with two 5 and 7 mm “pigmented” distance gages, having convex glass lens to apply pressure and purge the tissue from blood. Approximately all of the studies used visual analogue scale (VAS) as an evaluating method to determine effectiveness of therapy with PDL in clearance of lentigines with naked eye. Q-switched lasers are known as effective treatment option for pigmented lesions (6-8). According to nature of these lasers and very short pulse duration, it is possible for these lasers to induce erythema, blistering and post inflammatory hypo or hyper pigmentation. Hence, we hypothesized that long pulsed dye laser (PDL) with 595 nm wavelength and 3ms pulse duration, could be an effective alternative to treat benign pigmented cutaneous lesions including solar lentigines, according to good absorption of this wavelength by melanin and suitable epidermal sparing in this pulse duration range. For better absorption of this laser by melanin, we used a compressive lens to purge tissue blood and reducing hemoglobin as a competitive chromophore (3,9). The aim of the present study was to determine the safety profile of PDL as an alternative for Q-switched lasers and evaluating of its effects using an objective method (dermoscopy).
Methods
Patients having solar lentigines, confirmed through histopathology, seeking for treatment were selected to participate in this before-after clinical trial. Local ethics committee approved the study. All patients signed an informed consent after being briefed about the study and treatment procedure. Patients were excluded if they were pregnant, had history of PUVA therapy, scar formation, previous treatment for lentigines, vitiligo, psoriasis and unrealistic expectations from laser therapy. All selected lesions photographed before and after laser therapy through a computerized CCD camera dermatoscopy system. Stored figures were then evaluated to determine the effect of laser in reduction of pigmentation by two independent dermatologists as well as via computerized analysis by dermoscope firmware (VisioMed® H8). After initial dermoscopy, all lesions were treated with pulsed dye laser (V-Beam perfecta™ , Candela Corp. Wayland, CA, USA) using fluence 10 jouls, spot size 7mm, dynamic cooling device (DCD) off and a compression lens (Figure 1) equipped with laser apparatus without pulse stacking. During treatment, contact window were compressed on the lesions to purge skin blood vessels and prevent purpura to develop (Figure 2).
Figure 1 .

7mm contact lens used to treat pigmented lesions.
Figure 2 .
Compression effect used in treatment of pigmented lesions.
After laser therapy, a mild topical steroid (hydrocortisone cream) and antibiotic (mupirocin ointment) applied on the lesions for no more than seven consecutive days until any sign of epidermal injury, if occurred, completely healed. If there were any sign of deep injuries including persistent erythema, crust or bulla formation, patients referred for further treatment and excluded from the study. After four weeks, lesions were photographed again using dermoscopy system, and resulting figures evaluated to determine pigment reduction. We used computerized analysis of taken figures using dermoscope firmware that could analyze pigmented lesion to obtain an index value representing pigment density and irregularity. This index was documented for each lesion before and after therapy. We also, used visual analogue scale (VAS) system to determine rate of pigment reduction in dermoscopic images: less than 25% reduction in pigmentation was considered as poor response, between 25 to 50% considered as moderate response, between 50 to 75% considered as good response and more than 75% response considered as excellent response. Patients were questioned about their satisfaction rate and their answers documented in questionnaires. The same protocol was used to determine patients’ satisfaction from the clinical viewpoint. More than 75% clearance: very satisfied, between 75 and 50% clearance: satisfied and below 50% clearance: partial response. All data were collected in appropriate questionnaires and analyzed using chi-square and paired t-test when needed through SPSS ver 16.
Results
A total of 21 patients with 21 lentigo lesions, matching inclusion criteria, were included in the study. Mean age of patients was 54.2 years (±23.3) ranging from 39 to 71 years. Included patients were 18 females and three males. From 21 treated lesions, 11 were located on the hands and 10 on the face. We had four patients with type 2, 11 patients with type 3 and six with type 4 Fitzpatrick skin type.
From patients viewpoints, nine patients (43%) were very satisfied, seven (33%) were satisfied and the rest of patients (4 patients, 20%) explained partial response and requested further treatment.
Comparing before and after photographs taken through dermoscopy system, revealed that 12 patients (57%) had more than 75% improvement (excellent response), 5 patients (23.8%) had partial response (50- 75% resolution) and four patients (19%) had less than 50% response.
Mean pigment analysis score (calculated by computerized dermoscope software) was respectively 8 and 2 for before and after PDL therapy, showing noticeable decrease in pigment density of lesions. It was interesting that there was good positive correlation between this machine producing index and clinical evaluation of pre and post treatment figures by judging dermatologists. The most common side effect of treatment was mild post laser erythema that resolved spontaneously or using mild topical steroid, through 4 weeks after treatment. There was no hypopigmentation or scarring after treatment. One patient had mild burn and transient post inflammatory hyperpigmentation which resolved spontaneously after 12 weeks. There were no significant relationship between patient’s skin types and response to treatment or treatment side effects. This was the same for lesion’s sites. Patients were followed for 6 months. No evidence of recurrence or delayed side effects was seen in follow up period. Figure 3-6 show some lesions before and after the treatment.
Figure 3.
Excellent response (expert opinion : more than 80% resolution, Computerized index : from 7 to 1). (A) Before treatment. (B) After treatment.
A.

B.
Figure 6.
Partial response (expert opinion : 20-30% resolution, computerized index : from 7 reduced to 5). (A) Before treatment. (B) After treatment
A.

B.
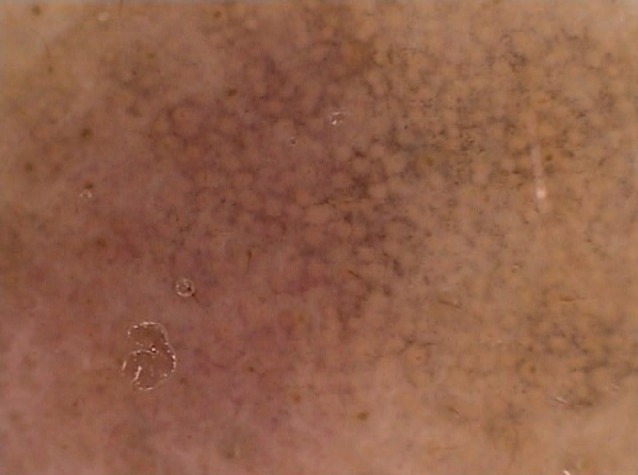
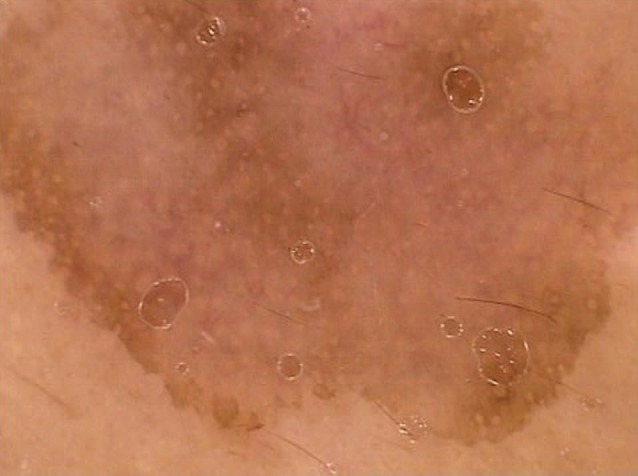
Figure 4.
Excellent response (expert opinion : more than 80% resolution, Computerized index : from 8 to 1). (A) Before treatment. (B) After treatment
A.

B.

Figure 5.
Good response (expert opinion : more than 50% resolution, Computerized index : from 8 to 3.5). (A) Before treatment. (B) After treatment
A.

B.
Discussion
Solar or senile lentigines are benign pigmented lesions causing cosmetic concerns in many patients visiting dermatology clinics. Topical treatments may induce resolution, but also are time consuming and could induce irritation. So, physical modalities of treatment had their own advocates. Among these modalities, lasers and cryo-therapy are more popular (10). Any treatment modality must be selected according to its safety profile and side effects. It was believed that cryotherapy is the golden standard treatment of lentigines (10). Although cryotherapy with liquid nitrogen has been the treatment of choice for lentigines since long time ago, its side effects especially in Iranian patients, including post inflammatory hyperpigmentation, incomplete removal of lesions, and rarely scarring, makes it necessary to find substitute treatments (9). The effectiveness and safety of PDL in treatment of skin pigmented lesions including lentigines has been shown previously (2,3,11,12). The present study may be the first one that used computerized CCD dermoscopic camera to evaluate clearance of lesions using firmware analysis as an objective method and VAS to judge response according to experts’ opinion. We found that PDL is an effective measure in treating solar lentigines and this was proved by comparing post treatment dermoscopic photographs, showing near to complete clearance of lentigines as well as reduction in machine produced index number. This is in agreement with other studies (1-5). Also, the present study revealed good safety profile of PDL. We had only one patient who experienced mild burn and transient post treatment hyperpigmentation resolving in the course of six months follow up with topical treatment. Other studies which used PDL to treat pigmented lesions also reported good safety profile (2,3,11,12). We found no significant relationship between sites of lesions or patients skin type and safety profile or response rate. This was the same for previous studies. The applications of the LPDL have been expanded in the past decade to include such applications as wrinkles, warts, hypertrophic scars, acne, and leg veins (13-18). According to our results, solar lentigines could be in the list.
In conclusion, PDL is a safe and effective option to treat lentigines if applied properly using compression method, especially in Iranian patients. However, further studies with larger sample size are required to confirm these results.
Please cite this article as follows:
Ghaninejhadi H, Ehsani A, Edrisi L, Gholamali F, Akbari Z, Noormohammadpour P. Solar Lentigines: Evaluating Pulsed Dye Laser (PDL) as an Effective Treatment Option . J Lasers Med Sci 2013; 4(1):33-8
References
- 1.Ashinoff R, Geronemus RG. Q-switched ruby laser treatment of labial lentigos. J Am Acad Dermatol. 1992;27(5 Pt 2):809–11. doi: 10.1016/0190-9622(92)70253-c. [DOI] [PubMed] [Google Scholar]
- 2.Day TW, Pardue CC. Preliminary experience with a flashlamp-pulsed tunable dye laser for treatment of benign pigmented lesions. Cutis. 1993;51(3):188–90. [PubMed] [Google Scholar]
- 3.Kono T, Chan HH, Groff WF, Sakurai H, Takeuchi M, Yamaki T. et al. Long-pulse pulsed dye laser delivered with compression for treatment of facial lentigines. Dermatol Surg. 2007;33(8):945–50. doi: 10.1111/j.1524-4725.2007.33196.x. [DOI] [PubMed] [Google Scholar]
- 4.Galeckas KJ, Ross EV, Uebelhoer NS. A pulsed dye laser with a 10-mm beam diameter and a pigmented lesion window for purpura-free photorejuvenation. Dermatol Surg. 2008;34(3):308–13. doi: 10.1111/j.1524-4725.2007.34063.x. [DOI] [PubMed] [Google Scholar]
- 5.Pootongkam S, Asawanonda P. Purpura-free treatment of lentigines using a long-pulsed 595 nm pulsed dye laser with compression handpiece: a randomized, controlled study. J Drugs Dermatol. 2009;8(11 Suppl):s18–s24. [PubMed] [Google Scholar]
- 6.Goldberg DJ. Goldberg DJBenign pigmented lesions of the skinTreatment with the Q-switched ruby laser. J Dermatol Surg Oncol. 1993;19(4):376–9. doi: 10.1111/j.1524-4725.1993.tb00360.x. [DOI] [PubMed] [Google Scholar]
- 7.Kilmer SL, Wheeland RG, Goldberg DJ, Anderson RR. Treatment of epidermal pigmented lesions with the frequency-doubled Q-switched Nd:YAG laser. A controlled, single-impact, dose-response, multicenter trial. Arch Dermatol. 1994;130(12):1515–9. [PubMed] [Google Scholar]
- 8.Taylor CR, Anderson RR. Treatment of benign pigmented epidermal lesions by Q-switched ruby laser. Int J Dermatol. 1993;32(12):908–12. doi: 10.1111/j.1365-4362.1993.tb01417.x. [DOI] [PubMed] [Google Scholar]
- 9.Seirafi H, Fateh S, Farnaghi F, Ehsani AH, Noormohammadpour P. Efficacy and safety of longpulse pulsed dye laser delivered with compression versus cryotherapy for treatment of solar lentigines. Indian J Dermatol. 2011;56(1):48–51. doi: 10.4103/0019-5154.77552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ortonne JP, Pandya AG, Lui H, Hexsel D. Treatment of solar lentigines. J Am Acad Dermatol. 2006;54(5 Suppl 2):S262–S271. doi: 10.1016/j.jaad.2005.12.043. [DOI] [PubMed] [Google Scholar]
- 11.Tan OT, Morelli JG, Kurban AK. Pulsed dye laser treatment of benign cutaneous pigmented lesions. Lasers Surg Med. 1992;12(5):538–42. doi: 10.1002/lsm.1900120513. [DOI] [PubMed] [Google Scholar]
- 12.Kono T, Manstein D, Chan HH, Nozaki M, Anderson RR. Q-switched ruby versus long-pulsed dye laser delivered with compression for treatment of facial lentigines in Asians. Lasers Surg Med. 2006;38(2):94–7. doi: 10.1002/lsm.20246. [DOI] [PubMed] [Google Scholar]
- 13.Komericki P, Akkilic M, Kopera D. Pulsed dye laser treatment of genital warts. Lasers Surg Med. 2006;38(4):273–6. doi: 10.1002/lsm.20293. [DOI] [PubMed] [Google Scholar]
- 14.Smucler R, Jatsova E. Comparative study of aminolevulic acid photodynamic therapy plus pulsed dye laser versus pulsed dye laser alone in treatment of viral warts. Photomed Laser Surg. 2005;23(2):202–5. doi: 10.1089/pho.2005.23.202. [DOI] [PubMed] [Google Scholar]
- 15.Seaton ED, Charakida A, Mouser PE, Grace I, Clement RM, Chu AC. Pulsed-dye laser treatment for inflammatory acne vulgaris: randomised controlled trial. Lancet 2003. 25;362(9393):1347–52. doi: 10.1016/s0140-6736(03)14629-6. [DOI] [PubMed] [Google Scholar]
- 16.Sawcer D, Lee HR, Lowe NJ. Lasers and adjunctive treatments for facial scars: a review. J Cutan Laser Ther. 1999;1(2):77–85. doi: 10.1080/14628839950516904. [DOI] [PubMed] [Google Scholar]
- 17.Bowes LE, Nouri K, Berman B, Jimenez G, Pardo R, Rodriguez L. et al. Treatment of pigmented hypertrophic scars with the 585 nm pulsed dye laser and the 532 nm frequency-doubled Nd:YAG laser in the Q-switched and variable pulse modes: a comparative study. Dermatol Surg. 2002;28(8):714–9. doi: 10.1046/j.1524-4725.2002.01058.x. [DOI] [PubMed] [Google Scholar]
- 18.Kono T, Yamaki T, Ercocen AR, Fujiwara O, Nozaki M. Treatment of leg veins with the long pulse dye laser using variable pulse durations and energy fluences. Lasers Surg Med. 2004;35(1):62–7. doi: 10.1002/lsm.20035. [DOI] [PubMed] [Google Scholar]



