Abstract
Low level lasers, cold or soft lasers:
These lasers do not produce thermal effects on tissues and induce photoreactions in cells through light stimulation which is called photobiostimulation. Power of these lasers is usually under 250mW.
The main point differentiating low level lasers and high power ones is the activation of photochemical reactions without heat formation. The most important factor to achieve this light characteristic in lasers is not their power, but their power density for each surfa ceunit (i.e cm2). Density lower than 670mW/cm2, can induce the stimulatory effects of low level lasers without thermal effects.
Low level lasers (therapeutic) used today as treatment adjunctive devices in medicine and dentistry. Numerous studies have been performed on the applications of low level lasers in patient pain reduction. Mechanisms of pain reduction with therapeutic lasers and their application are expressed, and the studies realized in this field are presented.
Keywords: LLLT, endodontic, laser
Laser Definition
Laser is a kind of electromagnetic irradiation source, having particular and exclusive properties. The word LASER is an abbreviation formed by joining the first letter of the words: Light Amplification by Emission of Radiation.
L refers to Light.
A refers to Amplification.
S refers to Stimulation.
E refers to Emission.
R refers to Radiation.
Lasers Classification
Different parameters influence lasers classification and the most important of them are power, wavelength and laser source material.
Classification of lasers based on Power
Power is one of the important parameters in treatments with lasers. Any physician using lasers should be able to recognize them and to know their characteristics. Based on the power, lasers are classified in three groups, as bellow1:
A-High power, warm or hard lasers:
These lasers instill their therapeutic effects by causing heat and enhancing the moving energy in tissues.These effects includes necrosis, carbonization, evaporation, coagulation and protein denaturation. As it’s been mentioned in table 1, it is possible to benefit from one or more of these effects, based on controlling the resulted temperature. Power of these lasers is usually more than 0/5W. These types of lasers have applications in surgery.
Table 1. Tissue reactions under heat .
| Type of Reaction | Temperature (C°) |
| Hyperthermia | 37-43 |
| Decline of Enzyme Activity | 43-50 |
| Protein Coagulation- Protein Damage | 50-60 |
| Collagen Damage and effect on Cell Membrane | 70-80 |
| Molecular Destruction | 80-100 |
| Carbonization | 100-140 |
| Evaporation and Desquamation | 140-400 |
| Cutting | 500-800 |
B-Lasers with Moderate Powers:
These lasers have their therapeutic effect without inducing a lot of heat. Their light has a stimulating effect in tissues. Powers of these lasers are between 250 to 500mW.
C-Low Level or Cold Lasers:
These lasers have no thermal effect on tissues. Inducing a light stimulation, they result in light and gradual reactions in tissues which are called Photobiostimulation. Power of these lasers is usually less than 250mW.
The principal point in differentiating low level lasers from high power ones is induction of photochemical reactions without heat. The most important factor to achieve this light feature in these lasers is not their power, but their power density per each surface unit (i.e. cm2). A density less than 670mW/ cm2 without heat can induce the stimulating effect of low level lasers.
Classification of lasers based on wavelength
Lasers are classified in 4 categories based on their wavelengths, as follows2:
Ultraviolet range 300-400 nm
Visible light range 400-700 nm
Near Infrared (NIR) range 700-1200nm
Far Infrared (FIR) range more than 1200nm
Classification of lasers based on source material2
Gas lasers such as CO2,Ne and He
Liquid lasers such as Dye lasers
Solid lasers such as Ruby lasers
Semi-conductor lasers such as GaAllnP, GaALAs and GaAs
History of Laser Therapy
The first studies on the application of lasers in medical treatments were focused on its use in the surgical field with the high power lasers. But gradually, in late sixties laser therapy and use of low level lasers in medicine started. At that time, scientists used laser irradiation on cell to exert an effect on disease.
Professor Andrew Mester, is known as the pioneer in the science of laser biologic stimulation. He reached the conclusion that lasers with low powers can have biologic effects in their beam trajectory. And have non thermal effects when irradiated on skin3.
In 1968, Mester performed studies on cells using Ruby, Argon and He-Ne with low output powers3. He also studied the histologic, immunologic and electromicroscopic effects of laser on open wounds under irradiation. Results of these experiments indicated that improvement of collagen synthesis, induction of neovascularization and increased enzyme synthesis occurred in areas under laser irradiation.
At the end of 1969, Mester released an article in the field of the effects of low level laser on the improvement of unhealed or delayed healing wounds, and published his results with the title of application of low level lasers3.One of the most important applications of lasers in medicine is the usage of Low Level Laser Therapy (LLLT) or laser biostimulation in order to treat patients. This treatment modality has attracted a lot of attention from clinicians and specialists in recent years.
In this treatment technique of using low level lasers, because of the low output power of the laser, wavelength between 630-1300nm and the deep penetration ability, it easily penetrates up to several centimeters in tissues and reaches the cell chromophores such as mitochondria and effects on them.
In laser therapy, energy absorbed by tissues does not provoke heat or damage to the vital tissues. In laser therapy method, the energy of laser photons is absorbed by the cell and leads to stimulation which is referred as Photobiostimulation4.
The beauty of laser therapy lies in the fact that how much of the amount of photons are directed towards which cells.
Considering the wide spectrum of applications of photon medicine, many clinicians haven’t realized the real grandeur and power of photons, so they don’t believe in this treatment modality. Butresults of numerous studies show that this treatment method is somehow considered as an evolution in the treatment of the patients. Photo biotherapy is not a new and emerging method. It has been many years since sun light radiations are being used for treatment; however, normal light because of its natural properties, which is released and distributed in all directions, does not have the ability to penetrate enough in living tissues. Thus it is only used for biologic stimulation in limited dermal treatments. While laser therapy, easily and without consumption of any drug, can heal most wounds or accelerate tissue growth and development via cellular stimulation.
It is also suggested that it can stimulate and activate the body immune system with LLLT, as well as considerably reducing harmful inflammatory responses.
It is mentioned that laser treatment maintains the process of the body tissue growth in a normal state via enzymatic activation. Since enzymes accelerate chemical reactions, laser photon action is seen in its potential to decuple enzymatic chain process capability5.
In human body, photons are absorbed via the eye, skin and mucosa. Absorptive molecules are categorized in photo acceptors and photo receptors.
Photo acceptors are part of key cell structures and do not react directly to light. But they play a role in the turning on or off of a reaction after its activation by light.The main location of these substances is the cell respiratory chain and mitochondria. Examples of these photo acceptors are cytochrome C oxidase, flavoproteins, riboflavins and porphyrin rings. Photo acceptors have a light regulatory role when cells are in redox state. The site of action of Red and Infrared ranges’ wavelengths is the mitochondria, and these wavelengths affect molecules responsible for oxidation or reduction of the respiratory chain such as cytochromes. The cell membrane and matrix ara other sites of action for Red and Infrared wavelengths. Flavoproteins, riboproteins are the photo acceptors of the ultraviolet range6.
Electrons are transferred to oxygen by cytochrome. Change and transfer of the electron charge in the mitochondrial membrane results in electrochemical potential which activates the ATP synthesis pathway potential up to 300%. Increase of ATP leads to RNA and DNA synthesis and finally protein synthesis7,8 (Figure 1).
Figure 1 .
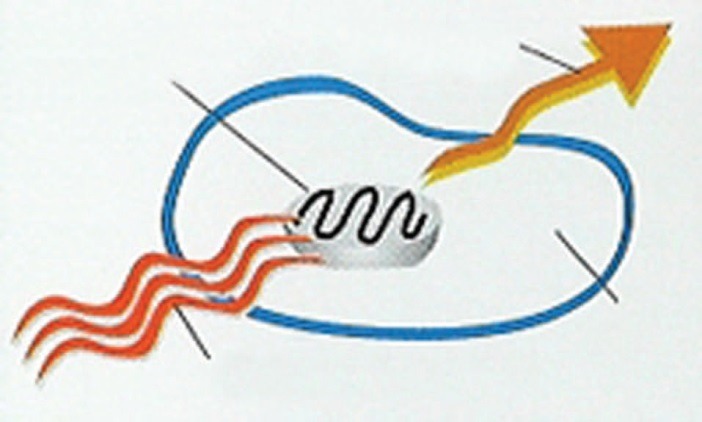
Photons’ energy is absorbed by mitochondria and lead to activation of primary reactions and increase in ATP synthesis. Then reactions of the dark region or secondary reactions start.
The effect of laser on a cell does not only depend on its wavelength, but also on the chromophores concerned oxidation state. In a way that in a normal or close to normal state, response to laser is weak but it is stronger in the reduction state, which is the reason for various responses in cell biology9.
Irradiation of certain wavelengths results in activation of photo acceptors of other wavelengths. It means that change in the oxidation and reduction of the target photo acceptors influences the absorption of other wavelengths. cytochrome oxidase C are the Photo acceptors of the Red and Infrared spectrums and the Photo acceptors of Ultra violet spectrum are flavoprotein molecules. The absorption of oxidases in activated state is partial, which is the basis for combination treatments with different wavelengths for certain diseases10.
Mechanism of Low Level Laser effect on Cell
The effect of laser irradiation on cell is divided in two stages of: primary reactions or reactions of the bright region and secondary reactions of dark region.
Primary Reactions
Reactions occurred in the cell during laser irradiation, resulting in the change of cell Redox state leading to oxidation or reduction.
In general, all cell metabolic reactions are controlled by the Redox state. Cells’ response to laser is different based on the quality of Redox .In a normal or close to normal stat, the response is weak and cases of transfer or tendency toward reduction have better response Healthy cells show less reactions under laser light which is an advantage of laser1,4.
Delayed Reactions
They are referred to the mechanisms that continue after laser irradiation. After mitochondrial stimulation a chain of biochemical reactions starts. And finally the amount of cell ATP increases, which subsequently leads to mRNA activation and DNA replication and in the end protein synthesis.
The amount of effect of laser with various wavelengths is assessed by measuring cell DNA and the quantity of the proteins. The synthesized protein is in many cases a neurotransmitter, a coenzyme, an enzyme or another substance regulating critical processes.
Following this process, laser effects spread from cell level to tissues and organ or macro vascular levels1,4.
Physiologic effects of laser at tissue level
Tissue response to laser can be divided in two categories:
Primary responses, comprising:
Vasodilation, blood circulation and lymphatic
drainage enhancement, increased activity of neutrophil
and fibroblast, improvement of cellular metabolism
and increased stimulus threshold of pain receptors.
Secondary responses, comprising:
- Increased concentration of certain prostaglandins such as PGL2 which has an anti-inflammatory effect.
- Increased immunoglobulins, lymphokins and their effect on the immune system.
- Increased beta endorphins and encephalins which are effective in analgesia.
Responses mentioned above result in physiologic responses which includes1:
- Stimulation of biologic system
- Effect on immune system
- Anti inflammatory and anti edema effect
- Effect on vessels and circulation
- Effect on wound healing
- Effect on nerves
- Analgesic effect
Anti inflammatory and anti edema effect of LLLT
Treatment by low level laser is effective in every 3 phases of inflammation (Exudation, alteration and proliferation). Laser decreases swelling, redness, heat, pain and inflammation by the following mechanisms11:
- Change in prostaglandins synthesis (PGE and PGF2α)
Increased synthesis of PCL2
- Inhibition of bradykinins synthesis
Increase of phagocytosis
Vasodilatation and more circulation
Increased lymphatic drainage
Increased secretion of MIF (Migration Inhibitory Factor)
- Reduction of histamine release
Biologic stimulation of LLLT
By moving the cell Redox system, laser orients the anaerobic metabolism toward aerobic. Anaerobic metabolism plays a major role in creation of pain and inflammation as well as slowing down healing process by formation of waste products and reduction of PH. Therefore, moving the metabolism toward aerobic and normal, laser has a positive impact12.
Effect on immune system
Red and Infrared wavelengths of laser activate the immune system by the following pathway13:
- Activation of T cells (T helper-T suppressor)
- Immune Modulation
- Increased macrophages and lymphocytes activity
- Increased phagocytosis
- Increased immunoglobulins and lymphokins
- Enhancement of complement system
Effect on wound healing
Are low level lasers carcinogenic?
One of the most thoroughly studied areas in laser therapy is wound healing. In fact, this was one of the first indications reported, with studies by Mester and by Carney14 as early as 1967. Electromagnetic radiation can injure living organisms if it has enough intensity to burn (many Watts) and/or contains highly energy photons (short wavelengths). Photons with the wavelength shorter than 320 nm are capable of ionizing molecules and atoms in tissue and can cause cancer. The risk factor depends on both, the dose (input energy, measured in joules per cm2 of skin) and the power density (intensity) of the radiation.
No effects have been observed resulting from light with wavelengths in the red or infrared range in doses used within laser therapy, but does it stimulate the cancer growth in someone who has cancer and is unaware of it?
There are many in vitro studies on this subject; however, with respect to the cancer in vivo, the situation is rather different.
Experiments on rats have shown that, small tomours treated with laser therapy may completely disappear, although it has no effect on tomours over a certain size15.
The electromagnetic spectrum comprises radiations with various wavelengths. Wavelengths of some of these radiations like Gamma rays are very short i.e. 10-6nm, when radio wavelengths reach 105 nm. Wavelength has an inverse proportion with frequency. Considering that energy of each atom is equal to its frequency multiplied by plank constant so the shorter the wavelength the more energy photons will have. High energy photons result in ionization of target cells. Photons with wavelengths shorter than 320nm like Gamma, X and ultraviolet rays cause atom and molecules’ chemical liaisons to fracture, and finally mutation happens, so they are carcinogenic. Ultra violet radiations with wavelengths between 320- 400nm provokes skin burns in prolonged irradiation, and are rarely carcinogenic. While radiations with long wavelengths such as radio frequency, microwave, infrared and visible light do not cause ionization, but only cause excitation and heat.
Wavelengths used in laser are comprised between visible light and infrared i.e. 600-1200nm. Photons of the visible and infrared range when they collide to tissues are either reflected, pass through them or are absorbed. So the energy they lose is transformed to other forms of energy. Till now no scientific report claiming mutation effect in these wavelengths range has been presented4,16. On the other hand doses used in laser therapy between 0.01 up to a maximum of 50 joules/cm2 are sometimes in inhibitory doses, while small changes in DNA result from 250 joules/ cm2 irradiation, which has a very large distance to therapeutic doses5.
Nevertheless, till the time when our science and knowledge hasn’t be turned to certitudes, it is reasonable in special cases where there is possibility of cancer or procreative organs concerned to avoid the use of low level lasers.
Lasers used in laser therapy from the beginning up to now include He-Ne, Ruby, Argon, CO2, Nd:YAG lasers and types of semi solid lasers (like GaAs, GaAlAs, GaAllnP). But today semi solid lasers constitute the base and foundation of more laser therapy devices. These lasers, in addition to positive biologic effects, are considered the lighter, smaller, cheaper and in the same time more durable lasers (Tuner)4.(Table 2)
Table 2. Most important therapeutic lasers with their wavelengths .
| HeNe laser | 633nm | Gas laser |
| InGaAIP lasers | 633-700nm | Semiconductor laser |
| GaAIAs lasers | 780-890nm | Semiconductor laser |
| GaAs laser | 904nm | Semiconductor laser |
| Defocused CO2 laser | 10600nm | Gas laser |
| Defocused Ruby laser | 694nm | Solid state laser |
| Defocused Nd:YAG laser | 1064 | Solid state laser |
Application of Low Level Lasers in Dentistry
The oral cavity is one of the best regions for laser therapy, because of convenient accessibility, comfortability for patients and particular biologic conditions. Low level lasers are used in the oral cavity and surrounding tissues including soft tissues, hard tissues and temporomandibular joint (TMJ). Soft tissues comprise mucosa, muscles and skin; hard tissues comprise bones, teeth and TMJ. Existence of such complex biologic structures in a small and limited space is seen nowhere else in the body.
Laser is used to treat various conditions in dentistry. Use of laser needs minimum anesthesia and is time saving for patients. Sometimes it is used as an adjunctive beside other treatments (drugs, surgery and physiotherapy) and sometimes as the principal treatment. It is the anti-inflammatory, analgesic and biostimulative regeneration effects of laser which causes the reestablishment of tissue normal physiologic state.
Low level lasers are used in different fields of dentistry. Treatment method, convenient wavelength and efficient doses are items to be determined by the clinician. Also response to different treatments and drugs varies from an individual to another. Response to laser therapy also depends on patient tissues and immune system condition.
Taking into account the mechanisms for biologic effect of lasers, it is possible to modify laser physical parameters in order to obtain treatment effect concordant with the targeted lesions. As well, time between treatment sessions which can be daily or every two days are determined depending on the type of disease in an acute or chronic point of view with consideratin of the body resistance.
Since laser therapy is a young science, methods and conditions of treatment are continuously under evaluation and improvement by researchers. Treatment failure is mostly due to choice of incorrect method or insufficient dosage and is not a reason for inefficiency of laser. In general it is necessary that the treatment course and the amount of effect of laser on the person, to be regularly under control5.
Application of Low Level Laser in Endodontic Treatments
1- Laser therapy in decreasing dentin hypersensitivity
Dentin hypersensitivity happens as a short and sharp pain from naked dentin in response to various stimuli. To treat dentin hypersensitivity, different anti sensitivity substances are used. In more complicated cases like reversible pulpitis, it is possible to use laser energy to help. Low level laser irradiation of cervix and apex region of sensitive teeth can be an appropriate treatment to eliminate sensitivity (Figure 2).
Figure 2.

Laser therapy can be use for decreasing dentin hypersensitivity
Effect of this laser is more based on changes created on pulp nerve transmission17. It is possible to relate laser effect at the cell level to the prevention of the signal transmission of pain from peripheral to central parts as well as blocking of the depolarization of sensory C fibers18,19. In a study Gerschman et al20 used low level laser with 830nm to decrease sensitivity in the dentinal region of teeth and repeated treatment in three time intervals. The most reduction of sensitivity was observed after the first treatment session. Also evidence has been presented on decrease of dental hypersensitivity immediately after beginning of treatment with He-Ne laser and lasted till 3 months after treatment and all teeth remained vital as well. GaAs and GaAlAs have more penetration. Irradiation is done in the apex region but by the use of Ne-He laser, irradiation would be only possible in the teeth anterior cervical region. Sometimes irradiation on cervix, pulp and apex is recommended. A tooth that would not respond to 4 to 6 joules of irradiation on its root for 2 to 3 sessions probably needs root canal herapy21,22.
2- Laser therapy in treatment of wounds and periapical lesions
In a study, low level laser was used to wound healing and the result showed that:
Less inflammation was observed on days 3 and 7 in the treatment group (p < 0.01). The inflammation rate on both sides was the same on day 14 (p > 0.05).
LLLT using optimal parameters can accelerate full thickness wound healing23.
Laser therapy result in better wound healing by the following mechanisms on the 3 phases of primary inflammation, proliferative and remodeling phases.
- Increased synthesis of RNA, DNA and proteins
- Angiogenesis and neovascularization
- Accelerated epithelialization
Anti inflammatory effect by affecting leukocytes and macrophages
Moving metabolism toward aerobic
Reduction of pain and decreased secretion of pain mediators
Activation of the immune system via effect on immunoglobulins IgM-IgG and complements (Figure 3)
Figure 3.
Laser therapy result in better wound healing. (A)Patient X-ray (B)Patient treatment by LLLT
A.
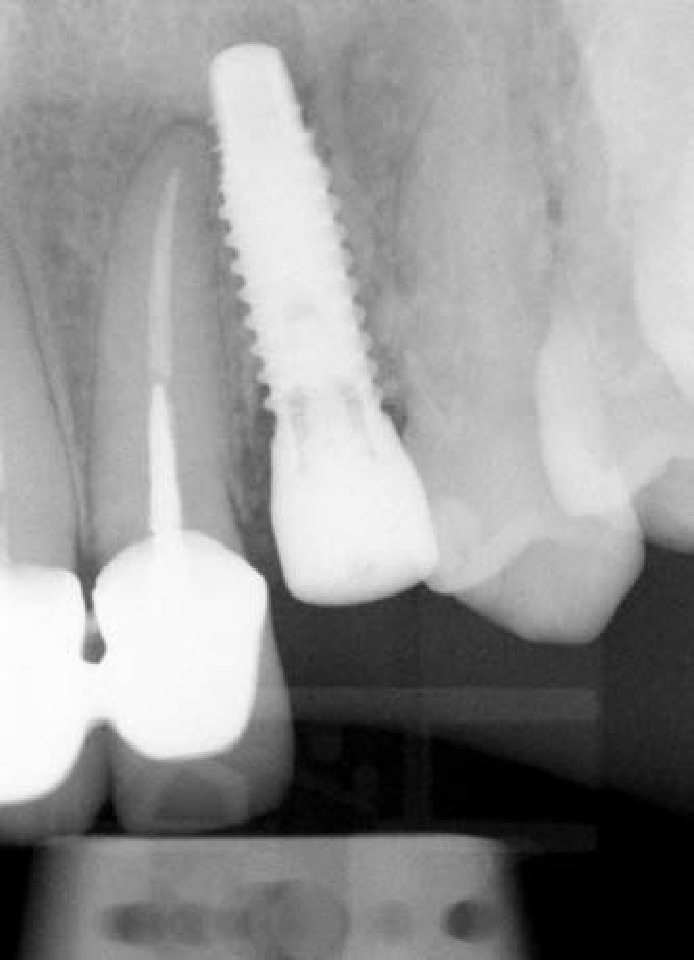
B.

Also daily use of low level laser in a treatment course resulted in stimulation of synthesis of type I collagen fibers and strengthens the scar tissue.
The anti-oedematous effect of laser energy is based on a dilation of lymphatic vessels and a reduction in the permeability of blood vessels. Laser energy has a regenerative effect on lymphatic vessels, as it has on veins4,24.
Pain reduction
Patient may sometimes experience pain the day after endodontic treatment. This is particularly common after the treatment of chronic complaints. It occurs because an injury is made acute when the process of healing starts4.
In a study, low level laser was used to decrease the pain after one session treatment and the result showed that:
Regarding the significant pain reduction in LLLT group at 4, 8, 12, and 48 hours after endodontic treatment, LLLT seems to be an effective and nonpharmacological approach for the reduction of post-en dodontic treatment pain25.
One of the most thoroughly studied areas in laser therapy is the wound healing. In fact, this was
one of the first indications which has been studied by Mester13.In the case study using 810nm diode laser and low Level Laser and sixteen months follow-up to improve healling of the edema26 (Figure 4,5).
Figure 4.
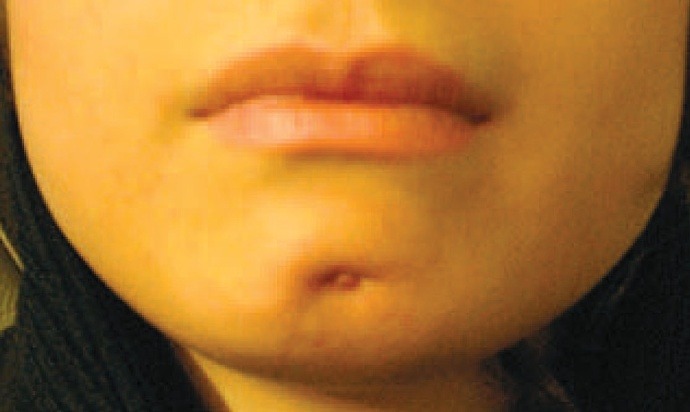
Chief complain: A fistula on the chin skin with a large swelling around it.
Figure 5.

Follow up after 16 month low level laser therapy
3- Laser therapy in repairing damaged nerves
Generally, damages on nerve repair slowly. Surgeries in dentistry and endodontics can result in nerve damages. Also, Extrusion of sealers containing formaldehyde from the end of the canals can affect the adjacent nerve tissue. Use of low level laser can be a good idea for the regeneration of damaged nerve tissue in animal models use of low level laser resulted in stimulation of damaged fibers’ axon growth. Protocol of laser therapy includes the use of 4/5J irradiation for 10 days.
In a double blind clinical study by Khullar et al, effects of LLLT on 13 patients with antecedent of injury of inferior alveolar nerves were evaluated. In the experimental group, after treatment with low level laser, significant improvement in touch sense was observed compared to control group. For sense of heat there was no difference between the two groups27.
4- Effects of laser on analgesia
One of the most important effects of low level lasers is its analgesic effect. Laser act on acute and chronic pains via the following mechanisms:
- Decrease of histamine, acetylcholine, serotonin, bradykinin and prostaglandin E2
- Augmentation of acetylcholine esterase
- Increase of lymphatic drainage
- Increase ATP and aerobic metabolism
- Augmentation of pain threshold
- Increase of beta adrenaline and encephalins
- Equilibrium in adrenalin and noradrenalin activity
- Reducing the production of P substance in spinal posterior horn
In vivo studies of analgesic effect of low level lasers on nerves of the oral cavity showed that these lasers reduced the frequency of stimuli of pain in nerve fibers and also increased the nerve stimulation threshold. In controlling pain by laser, it is possible to irradiate the points introduced by acupuncture medicine instead of stimulation by needles and obtain similar results28.
5- Laser therapy in accelerated anesthesia
In patients experiencing problems during anesthesia, with irradiation of 2 to 3 J of laser on apex of teeth, blood circulation of the area improves and anesthesia with lidocaine is obtained sooner. In addition, the start time of anesthesia is reduced because of improvement of local blood circulation. Irradiation of 2J of laser on injection area is effective in reducing patient’s pain and increasing stimulation threshold. Injection in periodontal ligament is very painful, and irradiation of 3 to 4J under papilla, well decreases pain during injection4 (Figure 6).
Figure 6.

Laser therapy can accelerated anesthesia
6- Laser therapy to reduce nausea during stages of root canal therapy and radiography
Nausea is one of the most common problems during dental treatments. Some clinicians use acupuncture to reduce nausea. It is possible to use laser instead of special needles. For this purpose at least 2J of energy is used in the hand wrist area and P6 Meridian point. Application of this method was accompanied with success in more patients4 (Figure 7).
Figure 7.
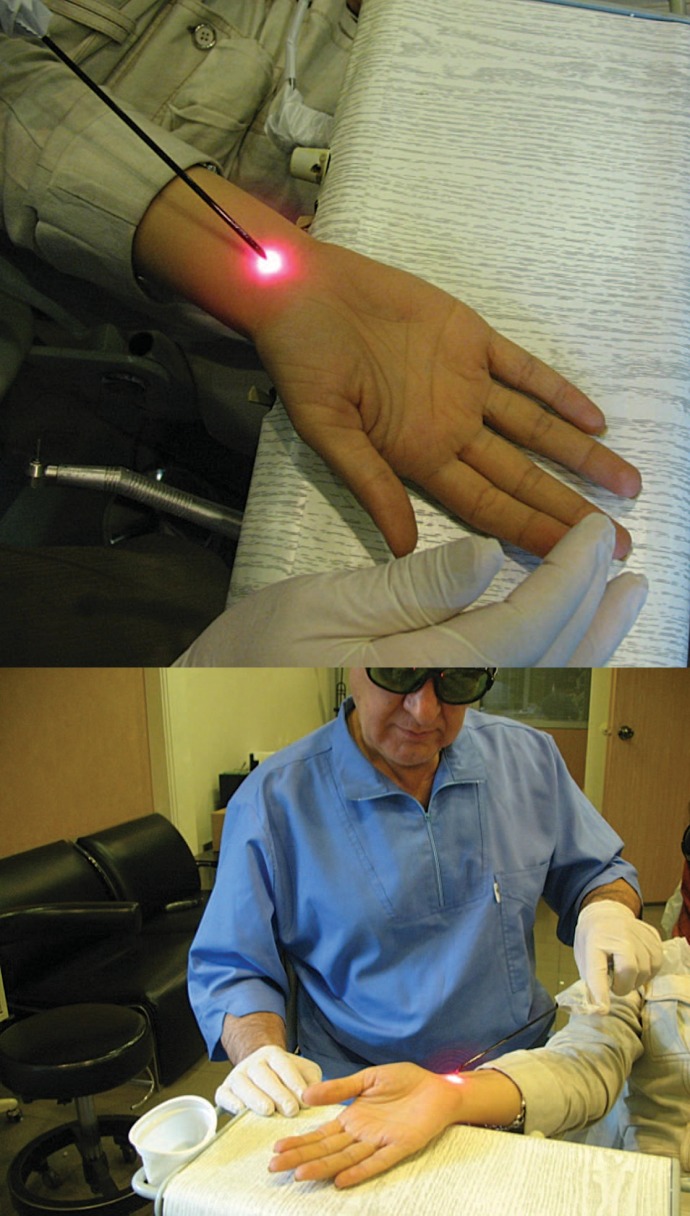
Use laser therapy to reduce nausea during stages of root canal therapy. (A) Finding the point. (B)Using low level laser
Risks and side effect related to laser irradiation on the body
Laser light depending on wavelength, power or output energy can be dangerous for body tissues, particularly eyes and skin. Laser light is not only dangerous when directly encountering tissues but also after reflection from reflective materials. Also, when using low level laser, its complications have to be kept in mind. The most important complications are:
1- Pain sensation in first sessions because of a chronic process becoming acute
2- False impression of improvement because of the analgesic effect of laser before apparition of repair effect
3- Sensation of fatigue is common after treatment with laser
4- Drop of blood pressure and vertigo if laser irradiation site is close to vessels or if laser is used intravenously and causes vessel dilation which results in drop of blood pressure, vertigo and darkening of the visual fields4.
Contraindication of laser therapy use
1- It is not prescribed in patients with pacemakers, or used with precaution
2- Laser should not be used in the uterus region in pregnant women
3- Shouldn’t be used in epileptic patients or with frequency less than 800Hz
4- Shouldn’t be used in patients with antecedent of arrhythmia or chest pain
5- Shouldn’t be used on glands, e.g. thyroid gland
6- Laser therapy should be avoid on tumorous tissues or benign tumors with malignant tendency
7- Prescription of laser therapy is forbidden in patients with lupus or patients treated with substances sensible to light
8- Low level lasers, under the title of cold-soft lasers, are used for years in different countries all over the world. The favorable effects of these lasers such as: decreasing inflammation and pain, increasing the quality and rapidity of repair, increasing the immunologic system, etc., are presented in different books and articles.
9- The aim of this article is to present a part of favorable effects of these lasers in dental, especially in endodontic treatments.
Please cite this article as follows:
Asnaashari M, Safavi N. Application of Low level Lasers in Dentistry (Endodontic). J Lasers Med Sci 2013; 4(2):57-66
References
- 1. Mokmeli S. Lasers classification, Eslami Faresani R. Rezvan F. The principals of low level laser therapy. Iran, Boshra 2004.;.
- 2. Eslami Faresani R. Ashtiani Araghi B. Kamrava K. Rezvan F. Laser Principles. Mokmeli S. Saghafi S. Laser therapy (handbook on basic and clinical practice of low level laser).Iran, Tehran, Boshra 2006.
- 3.Mester E, Mester AF, Mester A. The biomedical effects of laser application. Lasers Surg Med. 1985;5:31–9. doi: 10.1002/lsm.1900050105. [DOI] [PubMed] [Google Scholar]
- 4. Tuner J, Hode L.The laser therapy handbook, Sweden, Prima Book AB 2007.
- 5. Eghbali F. Low level or theraputic lasers, Fekrazad R. Applying low level laser therapy in dentistry. Tehran:Shayan nemoodar; 2009.
- 6.Derr VE, Fine S. Free radical occurrence in some laser-irradiated biologic materials. Fed Proc. 1965;24(Suppl14):99–103. [PubMed] [Google Scholar]
- 7.Ben-Dov N, Shefer G, Irintchev A, Wernig A, Oron U, Halevay O. Low energy laser irradiation affects cell proliferation and differentiation in vitro. Biochim Biophys Acta. 1999;1448(3):372–80. doi: 10.1016/s0167-4889(98)00147-5. [DOI] [PubMed] [Google Scholar]
- 8.Passarella S, Casamassima E, Molinari S, Pastore D, Quagliariello E, Catalano IM. et al. Increase of proton electrochemical potential and ATP synthesis in rat liver mitochondria irradiated in vitro by helium-neon laser. FEBS Letters. 1984;175(1):95–9. doi: 10.1016/0014-5793(84)80577-3. [DOI] [PubMed] [Google Scholar]
- 9.Bolton P, Young S, Dyson M. Macrophage responsiveness to light therapy with varying power and energy densities. Laser Therapy. 1991;3(3):105–12. [Google Scholar]
- 10.Karu T. Mechanisms of interaction of monochromatic visible light with cells. Proc SPIE. 1996;2630:2–9. [Google Scholar]
- 11.Tadakuma T. Possible application of the laser in immunobiology. Keio J Med. 1993;42(4):180–82. doi: 10.2302/kjm.42.180. [DOI] [PubMed] [Google Scholar]
- 12.Kovacs IB, Mester E, Gorog P. Laser-induced stimulation of the vascularization of the healing woundAn ear chamber experiment. experientia. 1974;30(4):341–3. doi: 10.1007/BF01921652. [DOI] [PubMed] [Google Scholar]
- 13.Mester E. Biostimulating Effect of Laser beams. Z Exp Chir. 1982;15(2):67–74. [PubMed] [Google Scholar]
- 14.Carney SA, Lawrence JC, Ricketts CR. The effect of light from a ruby laser on the metabolism of skin in tissue culture. Biochim Biophys Acta. 1967;148(2):525–30. doi: 10.1016/0304-4165(67)90151-1. [DOI] [PubMed] [Google Scholar]
- 15.Saldo I. et al. Effects of GaAs- laser on murine sarcoma depends on tomour size. Lasers in surgery and medicine. 1989;Suppl 1:40. [Google Scholar]
- 16.Nanami T, Shiba H, Ikeuchi S, Nagai T, Asanami S, Shibata T. Clinical applications and basic studies of laser in dentistry and oral surgery. Keio J Med. 1993;42(4):199–201. [PubMed] [Google Scholar]
- 17.Scherman A, Jacobsen PL. Managing dentin hypersensitivity: what treatment to recommend to patients. J Am Dent Assoc. 1992;123(4):57–61. doi: 10.14219/jada.archive.1992.0107. [DOI] [PubMed] [Google Scholar]
- 18.Sandford MA, Walsh LJ. Thermal effects during desensitization of teeth with gallium-aluminium-arsenide lasers. Periodontology. 1994;15:25–30. [Google Scholar]
- 19.Featherstone JD, Nelson DG. Laser effects on dental hard tissues. Adv Dent Res. 1987;1(1):21–6. doi: 10.1177/08959374870010010701. [DOI] [PubMed] [Google Scholar]
- 20.Gerschman JA, Ruben J, Gebart-Eaglemont J. Low level laser therapy for dentinal tooth hypersensitivity. Australian Dental Journal. 1994;39(6):353–7. doi: 10.1111/j.1834-7819.1994.tb03105.x. [DOI] [PubMed] [Google Scholar]
- 21.Tsuchiya K, Kawatani M, Takeshige C, Matsumoto I. Laser irradiation abates neuronal responses to nociceptive stimulation of rat-paw skin. Brain Res Bull. 1994;34(4):369–74. doi: 10.1016/0361-9230(94)90031-0. [DOI] [PubMed] [Google Scholar]
- 22.Matsui S, Tsujimoto Y, Matsushima K. Stimulatory effects of hydroxyl radical generation by Ga-Al-As laser irradiation on mineralization ability of human dental pulp cells. Biol Pharm Bull. 2007;30(1):27–31. doi: 10.1248/bpb.30.27. [DOI] [PubMed] [Google Scholar]
- 23.Alipanah Y, Asnaashari M, Anbari F. The effect of low level laser (GaAlAs) therapy on the post-surgical healing of full thickness wounds in rabbits. Med Laser Application. 2011;26(3):133–8. [Google Scholar]
- 24.Ando T, Noguchi I, Satoh Y, Fuse S, Hayama S, Takahashi M. et al. Use of soft lasers in dentistry. Shikai Tenbo. 1985;66(6):1265–8. (Japanese) [PubMed] [Google Scholar]
- 25.Asnaashari M, Mohebi S, Paymanpour P. Pain reduction using low level laser irradiation in single-visit endodontic treatment. J Lasers Med Sci. 2011;2(4):139–43. [Google Scholar]
- 26.Asnaashari M, Asnaashari N. Clinical application of 810nm diode laser and low level laser therapy for treating an endodontic problem. J Lasers Med Sci. 2011;2(2):82–6. [Google Scholar]
- 27.Khullar SM, Brodin P, Barkvoll P, Haanaes HR. Preliminary study of low-level laser for treatment of long-standing sensory aberrations in the inferior alveolar nerve. J Oral Maxillofac Surg. 1996;54(1):2–7. doi: 10.1016/s0278-2391(96)90290-6. [DOI] [PubMed] [Google Scholar]
- 28.Schlager A, Offer T, Baldissera I. Laser stimulation of acupuncture point P6 reduces postoperative vomiting in children undergoing strabismus surgery. Br J Anaesth. 1998;81(4):529–32. doi: 10.1093/bja/81.4.529. [DOI] [PubMed] [Google Scholar]


