Abstract
Introduction: Several treatment options have been introduced for removal of gingival hyperplasic lesions, but using diode lasers have many advantages such as less bleeding, time saving, better shaping, improved healing and less complication for the patients.
Case: A 15-year-old girl with multiple fibroma-like lesions in the oral cavity, who had a medical history of tuberous sclerosis, was selected for gingivoplasty treatment with 810nm diode laser.
Result: A perfect shaping was obtained after removal of the whole lesion in one session and no recurrence was observed in 6 months.
Conclusion: Using laser in the treatment of oral lesions leads to excellent wound healing along with excellent functional results.
Keywords: tuberous sclerosis, diode laser, fibroma
Introduction
Several clinical signs have been reported for tuberous sclerosis. Common symptoms include seizures, mental retardation, dermatologic signs such as hypomelanotic macules and facial angiofibromas (pringle sebaceous adenomas). Oral lesions which usually appear in the form of fibromas occur in 11-56% of the patients and the common sites are the gingiva, mucosa, lips and the base of the tongue1. It has been reported that oral fibromas may not be truly tuberous sclerosis lesions, but rather caused by the drugs used to treat the neurological disorders. Hydantoins produce secondary gingival hypertrophy when significant amount of bacterial plaque is present2,3.
There are different kinds of treatment for these hyperplasic tissues such as scalpel excision, electrical surgery and laser surgery. Conventional surgery could be followed by several complications such as intraoperative bleeding, difficulties in wound healing and maintenance of sterility during surgery2,4,5.
Diode lasers have been used in a variety of soft tissue surgical procedures and have many advantages such as less pain, bleeding, scar formation and infection6. Examined histologically, laser wounds have been found to contain a significantly lower number of myofibroblasts.This results in less wound contracture or scarring, and ultimately improved healing6.
As a result of improved healing and hemostasis, intraoral laser wounds can often be left without sutures, healing by secondary intention except when cosmetic is a concern. Less postoperative swelling and pain is another advantage of lasers which most likely correlates with decreased tissue trauma and an alteration of neural transmission6.
Case
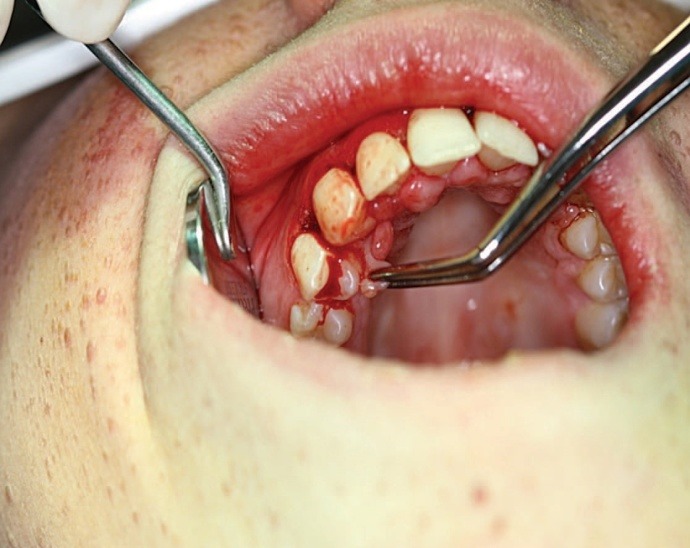
A 15-year-old girl with chief complaint of oral lesions was referred to laser department of Shahid Beheshti University. The clinical examination and the medical history of the patient revealed that she was diagnosed with tuberous sclerosis. She also mentioned use of hydantoins to control the condition. Multiple angiofibromas were also seen on her face (Figure1). Her intraoral examination revealed multiple diffuse fibroma like lesions on her gingiva on labial, palatal and lingual sides (Figure 2,3).
Figure 1 .

Extra oral view of the tuberous sclerosis patient
Figure 2 .
Intraoral view of the patient
Figure 3 .

Intraoral view of the patient
Previously, she had similar lesions which were excised with scalpel. Diode laser (Dr.smile) at the wavelength of 810nm was selected for excision and gingivoplasty with an average power of 2.5w, contact mode and a total time of 5 minutes. The irradiation mode was CW (continuous wave). After application of local anesthesia the lesion was excised by the laser with a sweeping motion accompanied by a high vacuum suction (Figure 4).
Figure 4 .

Final view after gingivectomy
Then a periodontal dressing was used to cover the area. The patient was instructed to maintain a good oral hygiene at the end of treatment. Also chlorhexidine mouthwash 0.12 % mouthwash was prescribed for the patient.
The patient was visited after 3 days and the periodontal dressing was removed. Her gingival tissue was in perfect condition. The patient was followed up after 3 months and 6 months and no recurrence was observed. Also the patient did not suffer from any post-operative complications like swelling or pain.
Discussion
In the present case we evaluated the advantages of diode laser for the treatment of gingival hyperplasia. Laser application for excising oral hyperplastic lesions shows some advantages such as less bleeding that is suitable for the surgical treatment of oral mucosal lesions which are rich in blood vessels6. The advantages of laser therapy are similar to electrical surgery concerning coagulation of the wound area combined with the precise cutting force of scalpels7. Only one instrument would be necessary for excision and coagulation. Completely different effects can be obtained by simple changes of pulse duration, average power and pulse repetition by the same laser, which means one tool acts as several instruments for the operator8. It has been documented in numerous studies that laser creates locally sterile conditions which would result in the reduction of bacteremia concomitant to the operation7.
Many international studies have shown further advantages of laser surgery compared to conventional surgery, such as lowering of the pain level, an almost bleeding-free operation field, as well as low incidence of postoperative hemorrhage, all of which reduce psychological load for both the patient and the surgeon9.
It is reported that the recurrence rate in laser surgery varies between 7.7% and 38.1% depending on differences in the variety and condition of the laser beams, the follow up period and the race5. Therefore the regular follow up is obligatory after excision of the lesion5.
Conclusion
Among different treatment modalities for gingival overgrowths, laser surgery has gained special attention according to its excellent shaping, perfect healing and functional results.
Please cite this article as follows:
Asnaashari M, Azari-Marhabi S, Alirezaei S, Asnaashari N. Clinical Application of 810nm Diode Laser to Remove Gingival Hyperplasic Lesion. J Lasers Med Sci 2013; 4(2):96-8
References
- 1.Cruz MP, López J, Küstner ED, Viñas M. Tuberous sclerosis: literature review and case report. Bull Group Int Rech Sci Stomatol Odontol. 2007;48:8–14. [Google Scholar]
- 2.Daniel B, Eisen MD, Fazel N. Treatment of gingival fibromas using CO2 laser and electrosurgery in a patient with tuberous sclerosis. Dermatol Online J. 2008;14:7–10. [PubMed] [Google Scholar]
- 3.Giunta J L. Gingival fibrous nodule. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;88:451–4. doi: 10.1016/s1079-2104(99)70060-0. [DOI] [PubMed] [Google Scholar]
- 4.Weston J. Carbon dioxide laser abrasion for treatment of adenoma sebaceous in tuberous sclerosis. Ann Plast Surg. 1985;15:18–25. doi: 10.1097/00000637-198508000-00007. [DOI] [PubMed] [Google Scholar]
- 5.Guelmann M, Britto LR, Katz J. Cyclosporin-induced gingival overgrowth in a child treated with CO2 laser surgery: a case report. J Clin Pediatr Dent. 2003;27:123–6. doi: 10.17796/jcpd.27.2.v70187716x08286q. [DOI] [PubMed] [Google Scholar]
- 6. Coluzzi DJ, Convissar RA. Laser application in dentistry. New York: Quintessence publishing co; 2007.
- 7. Moritz A. Oral laser application. Berlin: Quintessenz Verlags-GmbH; 2006.
- 8.Wilder-Smith P, Dang J, Neev J. The Influence Of Laser Parameter Configuration At 93 Microns On Incisional And Collateral Effects In Soft Tissue. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;84:22–7. doi: 10.1016/s1079-2104(97)90288-2. [DOI] [PubMed] [Google Scholar]
- 9.Slutzki S, Shafir R, Bornstein LA. Use of a carbon dioxide laser for laser excisions with minimal blood loss. Plast Reconstr Surg. 1997;60:250–5. doi: 10.1097/00006534-197708000-00012. [DOI] [PubMed] [Google Scholar]


