Abstract
Introduction: Pyogenic granuloma (PG) is a common tumor-like growth of the oral cavity, considered to be of non-neoplastic nature, often caused by constant low-grade trauma as well as poor oral hygiene and maybe due to hormonal disturbances. Surgical excision, and removal of underlying cause in some cases, is the preferred method of treatment as it is only a benign lesion.In order to remove this lesion, scalpel, cryosurgery and laser are used. Currently different lasers, with adequate parameters, are used for the surgery of PG, which include CO2 (Carbon Dioxide Laser), Nd:YAG (Neodymium-Doped Yttrium Aluminium Garnet), Diode and Er Family amongst others. In this present case, due to the proximity of the lesion with dental hard tissue, Er:YAG (Erbium-Doped Yttrium Aluminum Garnet) laser appears to be the more appropriate laser. The application of Laser is also a newly recommended technique. The aim of this study is to assess the stages of treatment, recovery and recurrence of PG when the Er:YAG laser is used. Furthermore this study aims to also evaluate the friendliness of this method with regards to the surgeon (therapist).
Case report: A 24-year-old female was referred to the Laser Research Center of Dentistry of Tehran University of Medical Sciences with a complaint of gingival overgrowth and bleeding. This lesion was in the buccal and palatal side of the 5 and 6 maxillary teeth. Treatment plan included an excisional biopsy of the lesion using Er:YAG laser (3W, 300mJ, 10Hz, Short pulse, with contact headpiece). The bones were then cleaned of soft tissue before being smoothed using a curette. The excised specimen was preserved and sent for histopathological examination.
Results: The patient reported no pain after surgery and did not use any systemic antibiotics. The patient was satisfied after the surgery. Chlorhexidine mouthwash was given to the patient. Pathology results confirmed Pyogenic granuloma.After 2 weeks, complete healing was observed. The 9-month follow-up was also carried out in order to check the process of healing as well as the recurrence.
Conclusion: Excisional surgery is the preferred treatment method for PG. The application of laser can be considered as an effective and safe technique for excision of this lesion with minimal invasion and many clinical advantages such as less intra-operative bleeding, hemostasis and reduced pain and times of healing.
Keywords: pyogenic granuloma, Er YAG Lasers, laser surgery
Introduction
In 1897 Pyogenic Granuloma (PG) was described for the first time by two French surgeons Poncet and Dor 1,2 . As the lesion is not a true granuloma, the term PG can be misleading 3 .
Pyogenic granuloma of the skin and oral cavity can form as a result of various etiologic factors that have been put forward by different researchers 4 . Chronic low grade trauma 5 , physical trauma 6 , hormonal factors 7 , bacteria, viruses 8 and certain drugs 9 have been considered as contributory factors in the development of pyogenic granulomas. Poor oral hygiene, foreign material in the gingiva, calculus, and local irritants generally are the advancing causes 4 .
These lesions possess certain clinical features such as being painless, sessile or pedunculated exophytic masses with a base beginning from the gingival margin or, in most cases, from the interproximal tissues in the maxillary anterior.
The size can vary from case to case but it hardly ever exceeds 2cm and it will return unless completely removed. In 70-75% of the cases, oral pyogenic granuloma is observed in gingiva, followed by the tongue, lips, and buccal mucosa 4,10 .
Pyogenic granuloma can develop at any age but in the majority of cases, 60%, PG is observed in the 10-40 years old age group, with the incidence peak between the ages of 20 to 30. Moreover, the possibility of PG is twice as likely with regards to females 1,11 .
The treatment of this lesion can be carried out using different approaches.
To remove PG, scalpel, cryosurgery and laser might be used.
Laser excision is the recommended method, which is well accepted by patients with no unfavorable consequences 1 .
Diode laser 1 , Nd:YAG (Neodymium-Doped Yttrium Aluminium Garnet)12 , CO2 (Carbon Dioxide Laser)13 , and Er:YAG (Erbium-Doped Yttrium Aluminum Garnet)14 have reportedly been successful in treating mucosal pyogenic granulomas.
The possibility of recurrence of the lesion has reported to be 16%, however it seems that the use of laser will reduce this recurrence rate.
The purpose of this study is to assess the stages of treatment, recovery and recurrence of PG when the Er:YAG laser is used. Furthermore this study aims to also evaluate the friendliness of this method with regards to the surgeon (therapist).
Case Report
A 24-year-old female was referred to the Laser Research Center of Dentistry of Tehran University of Medical Sciences with a complaint of gingival overgrowth and bleeding. This lesion was in the right side of the maxilla. Macroscopic appearance of this lesion was a pedunculated mass in the interproximal region of 15 and 16 extended to buccal and palatal, which appeared almost round in shape. It was reddish pink covered by cream-colored mucosa. The surface was uneven with shallow grooves with ulcerations and bleeding in some areas. The lesion was approximately 14 mm × 8 mm in diameters and 6 mm in thickness with relatively soft consistency (Figure 1 and 2).
Figure 1 .

Microscopic appearance of the lesion between the teeth 15 and 16
Figure 2 .

Preoperative panoramic view
Excisional biopsy with an Er:YAG laser (2940D plus, Deka, Italy) (Output power=3W, E=300mJ, Frequency=10Hz, Short pulse, with contact headpiece, contact tip, with 50% water & 50% air, Diameter of tip=1 mm) was the main step of treatment (Figure 3). An elliptical incision was made around the peduncle, and then the lesion was lifted along with the underlying periosteum from the bone surface and removed until debris and soft tissue were eliminated (Figure 4 and 5).
Figure 3 .

The view of surgery using contact handpiece of Er:YAG laser
Figure 4 .

Complete removal of the lesion with elimination of debris and soft tissue from the surface of bone and teeth
Figure 5 .

Palatal view after removal of the lesion
In order to prevent recurrence, up to the surrounding PDLs were cleaned by laser and also up to 2mm of the safe margin of the lesion was removed.
Hemostasis was achieved with the same laser and healing was obtained for second intention.
In order to achieve an acceptable hemostasis, Er:YAG laser was used without water, which scanned the area of wound. After the surgery, coe-pak (GC America, USA) was placed on the area. Chlorhexidine mouthwash (0.2 %) was also prescribed for the patient.
Excised specimen was preserved and the sample was placed in 10% formalin and then sent for histopathological examination.
Histopathologic Findings
For histopathological evaluation, H &E staining was carried out.
Microscopic examination (Zeiss.KF2. Germany) of sections prepared from the sample shows acanthotic and atrophic parakeratinized stratified squamous epithelium of oral mucosa and in some areas ulceration was seen with fibrino-leukocytic membrane where in the surface, epithelium had Plasma pooling areas. Supportive fibrovascuular connective tissue with numerous blood vessels in various sizes with plump endothelial cells. Mild to moderate infiltration of acute and chronic inflammatory cells was evident in the whole sample. The remaining host bone was observed in some sample areas. (Figures 6 and 7)
Figure 6 .
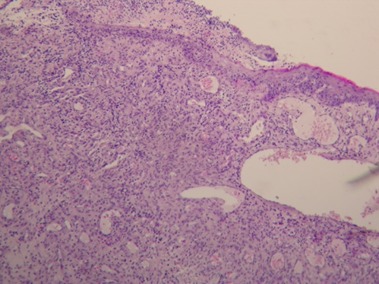
Microscopic view of the lesion with 100 × magnification
Figure 7 .
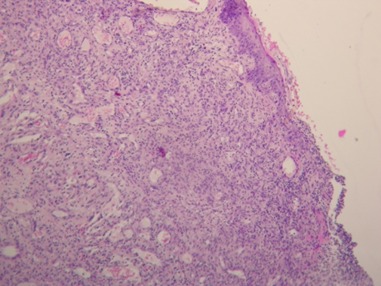
Microscopic view of the lesion with 100× magnification
This Histopathologic view confirmed the diagnosis of pyogenic granuloma.
The gingival tissues were revisited after seven days and were observed as healthy with successful healing (Figure 8). Furthermore full recovery was achieved within two weeks (Figure 9).
Figure 8 .

1 week after removal of the lesion using Er:YAG laser
Figure 9 .

2 weeks after removal of the lesion using Er:YAG laser
After the surgery the patient was asked about the level of pain and as there was no pain the patient was very pleased. The 9-month follow-up was also carried out in order to check the process of healing as well as the recurrence (Figure 10-12).
Figure 10 .

9 months after removal of the lesion using Er:YAG laser(Buccal)
Figure 12 .
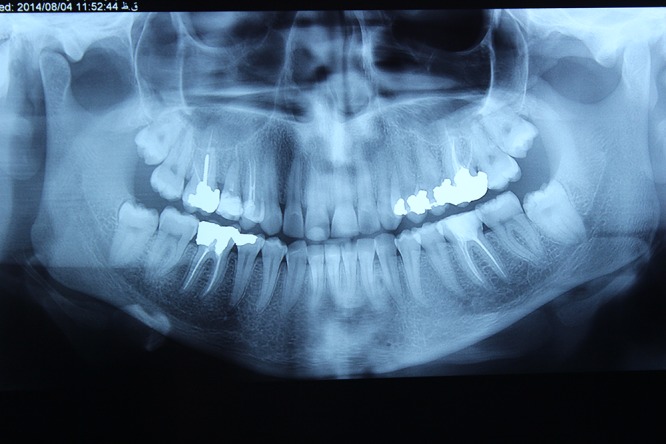
Panoramic view of 9 months after removal of the lesion using Er:YAG laser
Figure 11 .

9 months after removal of the lesion using Er:YAG laser(Palatal)
Discussion
Pyogenic Granuloma is an inflammatory hyperplastic lesion. The exact reason behind PG is not yet known.
Namazi et al. (2012) state that “trauma, hormonal influences, viral oncogenes, underlying microscopic arteriovenous malformation, the production of angiogenic growth factor and cytogenic abnormalities have all been postulated to play a role” 15,16 .
Literatures have suggested many factors such as trauma, viral oncogenes, infection, hormonal influences, poor oral hygiene, defective restorations, and residual roots 17,18 .
Differential diagnosis of pyogenic granuloma includes peripheral giant cell granuloma, peripheral ossifying fibroma, haemangioma, conventional granulation tissue, hyperplastic gingival inflammation, and in some cases even malignant lesions such as metastatic carcinoma, amelanotic melanoma and nonHodgkin’s lymphoma1,19-21 .
During histopathologic evaluation of the sample highly vascular proliferation resembling granulation tissue was the dominant feature of the tissue. Numerous small and large endothelium lined channels engorged with red blood cells under the ulcerated surface and the mixed inflammation led us to the diagnosis. On the other hand we did not observe any other significant element to make us take any of the other possible diagnosis into consideration.
Although the most commonly used technique for treatment of PG is surgical excision, many other methods including elimination with electric scalpel or cryosurgery 22 , cauterization with silver nitrate, sclerotherapy with sodium tetra decyl sulfate and monoethanolamine oleate 23 ligation, absolute ethanol injection dye24 , Nd:YAG and CO2 laser13 , shave excision, and laser photocoagulation25 have been reported to be used for this purpose. Surgical excision has been reported to have 16% rate of recurrence in treatment of PG.
Recently the application of different lasers for removal of PG has increased.
The advantages of laser surgery compared with conventional methods include maintenance of sterile conditions, reduction of bleeding, good possible estimation of cutting depth, precision of cutting, reduction in the number of instruments, often no need for suturing or bandages, pain reduction intra- and post-operatively, no inhibition of, and perhaps even promotion of wound healing, less scars, staff and time 26,27 .
Perhaps due to the high cost of laser devices it is not very cost-effective however, since Erbium laser is a kind of laser that is also used for restorative treatments, it may be used as an additional application in surgery too.
Laser surgery results in less pain, bleeding and the patient’s comfort. Also in areas where aesthetics are important, laser is a suitable means. This is a less invasive method compared to scalpel and cryosurgery with less risk of infection.
Since laser involves less bleeding it is considered to be very appropriate in the view of the surgeon, however as it is technically done using a handpiece it is more time consuming.
Despite all the advantages of laser, the skills of the dentist working with the laser are of great importance.
The type of laser used in the surgery is also very important. For example, CO2 and Er:YAG lasers, due to their high water absorption and less penetration compared to Nd:YAG and Diode lasers, are suitable means for cutting. The coagulation caused by these two lasers is also less. Moreover Nd:YAG and Diode cannot be used for bone resection.
When using Er:YAG laser, as the lesion is less damaged, the remaining tissue has more pathological value.
In some studies, because of the bleeding of PG Nd:YAG laser was used. But it seems that for the reasons stated above the cuts should be done using the Erbium Laser and if there was a problem of coagulation in some areas then those specific areas can be coagulated with Nd:YAG or Diode lasers.
CO2 is also difficult to work with and requires technical knowledge.
White et al. in 1998 have reported the success of CO2 and Nd:YAG laser irradiation in surgical treatment. They stated that laser excision is a well-accepted method by patients with no adverse effects 28 .
In a recent research in 2014 Kocaman et al. used Nd:YAG laser (power output 4W, energy 100 mJ, frequency 40 Hz, pulsed emission mode) in order to eliminate PG and concluded that the use of Nd:YAG laser in the treatment of pyogenic granuloma reduced bleeding during surgery, with a consequent reduction in operating time, promoted rapid postoperative hemostasis, and has better patient acceptance29 .
Meffert et al. used the flash lamp pulsed dye laser on a mass of granulation tissue and concluded that previously resolute tissue responded well to the series of treatments with pulsed dye laser 30 . Diode laser has shown excellent results in cutaneous pyogenic granulomas with only minimal pigmentary and textural complications. González et al. investigated the use of the 585 nm flashlamp-pumped pulsed dye laser (585 nm PDL) for the treatment of eighteen patients with symptomatic pyogenic granulomas and the results showed both symptomatic and clinical clearing of the lesions with excellent cosmetic results in 16 of 18 treated patients.31
In 2013 Licata et al. published a case report of PG which used Er,Cr:YSGG (Erbium, Chromium doped Yttrium Scandium Gallium Garnet) laser as the treatment method but no laser parameters were mentioned in this paper32 .
The advantages of application of laser include fast healing of the wound, less requirement for antibiotic therapy after the operation and less pain observed by the patient 26,27 . Taking into account the acceptable clinical results, Er:YAG laser can be taken as an effective technique for both soft and hard tissue treatment by reducing chair time and providing more convenience to the patient due to its simple procedure.
The Er:YAG laser can further be used for root curettage. Also that PG may arise from PDL, in which case Er:YAG is the best option. Furthermore, if PG occurs around the implant, Er:YAG has the advantage of removing the lesion with minimal damage to the implant.
Considering the recovery after the surgery, logically as Erbium has less penetration and results in less damage of the tissue, the recovery will be faster and better. This issue can be discussed in a comprehensive study in future.
Considering the recurrence of lesion, it appears that the type of laser used has no effect and furthermore recurrence does not depend on the laser wavelength and it is only affected by the surgical technique. However, a comprehensive study is also required in this regard.
Conclusion
Excisional surgery is the preferred treatment method for PG. The application of laser can be considered as an effective and safe technique for excision of this lesion with minimal invasion and many clinical advantages such as less intra-operative bleeding, hemostasis and reduced pain and time of healing.
Please cite this article as follows:
Fekrazad R, Nokhbatolfoghahaei H, Khoei F, Kalhori KA. Pyogenic Granuloma: Surgical Treatment with Er:YAG Laser. J Lasers Med Sci 2014;5(4):199-205
References
- 1.Rai S, Kaur M, Bhatnagar P. Laser: a powerful tool for treatment of pyogenic granuloma. J Cutan Aesthet Surg. 2011 May;4(2):144–7. doi: 10.4103/0974-2077.85044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jafarzadeh H, Sanatkhani M, Mohtasham N. Oral pyogenic granuloma: a review. J Oral Sci. 2006 Dec;48(4):167–75. doi: 10.2334/josnusd.48.167. [DOI] [PubMed] [Google Scholar]
- 3.Parrulli R, Franco S, Petruzzi M, Maiorano E, Favia G. Pyogenic Granuloma: surgical treatment with Diode Laser. Ann Stomatol (Roma) 2013;4(Suppl 2):35–6. [PMC free article] [PubMed] [Google Scholar]
- 4.Gomes SR, Shakir QJ, Thaker PV, Tavadia JK. Pyogenic granuloma of the gingiva: A misnomer? - A case report and review of literature. J Indian Soc Periodontol. 2013 Jul;17(4):514–9. doi: 10.4103/0972-124X.118327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Neville BW, Damm DD, Allen CM, JE. B. Oral and Maxillofacial Surgery. 2nd ed. Philadelphia: Saunders. 2002:447-9.
- 6. Regezi JA, Sciubba JJ, RC J. Oral Pathology: Clinical Pathological Considerations. 4th ed. Philadelphia: WB Saunders. 2003:115-6.
- 7.Mussalli NG, Hopps RM, Johnson NW. Oral pyogenic granuloma as a complication of pregnancy and the use of hormonal contraceptives. Int J Gynaecol Obstet. 1976;14(2):187–91. doi: 10.1002/j.1879-3479.1976.tb00592.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Janier M. [Infection and angiomatous cutaneous lesions] J Mal Vasc. 1999 May;24(2):135–8. [PubMed] [Google Scholar]
- 9.Bachmeyer C, Devergie A, Mansouri S, Dubertret L, Aractingi S. Pyogenic granuloma of the tongue in chronic graft versus host disease. Ann Dermatol Venereol. 1996;123(9):552–4. [PubMed] [Google Scholar]
- 10.Angelopoulos AP. Pyogenic granuloma of the oral cavity: statistical analysis of its clinical features. J Oral Surg. 1971 Dec;29(12):840–7. [PubMed] [Google Scholar]
- 11.Nthumba PM. Giant pyogenic granuloma of the thigh: a case report. J Med Case Rep. 2008;2:95. doi: 10.1186/1752-1947-2-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kocaman G, Belduz N, Erdogan C, Ozbek E, Sadik E, Kara C. The use of surgical Nd:YAG laser in an oral pyogenic granuloma: A case report. J Cosmet Laser Ther . 2014 Apr 1 doi: 10.3109/14764172.2014.910078. [DOI] [PubMed] [Google Scholar]
- 13.Raulin C, Greve B, Hammes S. The combined continuous-wave/pulsed carbon dioxide laser for treatment of pyogenic granuloma. Arch Dermatol. 2002 Jan;138(1):33–7. doi: 10.1001/archderm.138.1.33. [DOI] [PubMed] [Google Scholar]
- 14.Kaya A, Ugurlu F, Basel B, Sener CB. Oral Pyogenic Granuloma associated with a Dental Implant treated with an Er:YAG Laser: A Case Report. J Oral Implantol . 2013 Dec 18 doi: 10.1563/AAID-JOI-D-13-00251. [DOI] [PubMed] [Google Scholar]
- 15.Namazi Esmaeil, Baliga Sharmila, Muglikar Sangeeta, Rahul K. A case report of pregnancy tumor and its management using the diode laser. Journal of Dental Lasers. 2012;6(2):68–71. [Google Scholar]
- 16. Regezi JA, Sciubba JJ, RC J. Oral pathology: Clinical pathologic considerations. 4th ed. Philadelphia: WB Saunders; 2003. pp. 115–6.
- 17.Vasconcelos MG, Vasconcelos RG, Mafra RP, LMG Q. Pyogenic granuloma on the lower lip: An unusual location. Stomatos. 2012;18(35):34–8. [Google Scholar]
- 18.Akyol MU, Yalciner EG, Dogan AI. Pyogenic granuloma (lobular capillary hemangioma) of the tongue. Int J Pediatr Otorhinolaryngol. 2001 May 11;58(3):239–41. doi: 10.1016/s0165-5876(01)00425-6. [DOI] [PubMed] [Google Scholar]
- 19.Kamal R, Dahiya P, Puri A. Oral pyogenic granuloma: Various concepts of etiopathogenesis. J Oral Maxillofac Pathol. 2012 Jan;16(1):79–82. doi: 10.4103/0973-029X.92978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Patussi C, Sassi LM, Da Silva WP, Zavarez LB, JL S. Oral Pyogenic Granuloma after Tongue Piercing Use: Case Report. Dentistry. 2014;4(5):229–30. [Google Scholar]
- 21. Greenberg MS, Glick M, JA S. In: Burkett's textbook of oral medicine. 11th ed. USA: BC Becker Inc; 2008. pp. 131–2.
- 22.Gupta R, Gupta S. Cryo-therapy in granuloma pyogenicum. Indian J Dermatol Venereol Leprol. 2007 Mar-Apr;73(2):141. doi: 10.4103/0378-6323.31912. [DOI] [PubMed] [Google Scholar]
- 23.Matsumoto K, Nakanishi H, Seike T, Koizumi Y, Mihara K, Kubo Y. Treatment of pyogenic granuloma with a sclerosing agent. Dermatol Surg. 2001 Jun;27(6):521–3. doi: 10.1046/j.1524-4725.2001.01039.x. [DOI] [PubMed] [Google Scholar]
- 24.Ichimiya M, Yoshikawa Y, Hamamoto Y, Muto M. Successful treatment of pyogenic granuloma with injection of absolute ethanol. J Dermatol. 2004 Apr;31(4):342–4. doi: 10.1111/j.1346-8138.2004.tb00682.x. [DOI] [PubMed] [Google Scholar]
- 25.Kirschner RE, Low DW. Treatment of pyogenic granuloma by shave excision and laser photocoagulation. Plast Reconstr Surg. 1999 Oct;104(5):1346–9. doi: 10.1097/00006534-199910000-00016. [DOI] [PubMed] [Google Scholar]
- 26.Chiniforush N, Kamali A, Shahabi S, Bassir SH. Leukoplakia removal by co2 laser. J Lasers Med Sci. 2012;3(1):33–5. [Google Scholar]
- 27.Fekrazad R, Chiniforoush N. One Visit Providing Desirable Smile by Laser Application. J Lasers Med Sci. 2014;5(1):47–50. [PMC free article] [PubMed] [Google Scholar]
- 28.White JM, Chaudhry SI, Kudler JJ, Sekandari N, Schoelch ML, Silverman S, Jr Jr. Nd:YAG and CO2 laser therapy of oral mucosal lesions. J Clin Laser Med Surg. 1998 Dec;16(6):299–304. doi: 10.1089/clm.1998.16.299. [DOI] [PubMed] [Google Scholar]
- 29.Kocaman G, Belduz N, Erdogan C, Ozbek E, Sadik E, Kara C. The use of surgical Nd:YAG laser in an oral pyogenic granuloma: A case report. J Cosmet Laser Ther. 2014 Aug;16(4):197–200. doi: 10.3109/14764172.2014.910078. [DOI] [PubMed] [Google Scholar]
- 30.Meffert JJ, Cagna DR, Meffert RM. Treatment of oral granulation tissue with the flashlamp pulsed dye laser. Dermatol Surg. 1998 Aug;24(8):845–8. doi: 10.1111/j.1524-4725.1998.tb04261.x. [DOI] [PubMed] [Google Scholar]
- 31.Gonzalez S, Vibhagool C, Falo LD, Jr Jr, Momtaz KT, Grevelink J, Gonzalez E. Treatment of pyogenic granulomas with the 585 nm pulsed dye laser . J Am Acad Dermatol . 1996 Sep;35(3 Pt 1):428–31. doi: 10.1016/s0190-9622(96)90610-6. [DOI] [PubMed] [Google Scholar]
- 32.Licata ME, Albanese A, Giannatempo G, Dioguardi M, Campisi G. Minimally invasive approach to eliminate pyogenic granuloma using Er, Cr: YSGG laser. Ann Stomatol (Roma) 2013;4(Suppl 2):25. [PMC free article] [PubMed] [Google Scholar]


