Abstract
Introduction: Knee osteoarthritis (KO) is the most common joint disease for which there is no optimal treatment. Monochromatic infrared photo energy (MIPE) is a relatively new light modality used to reduce pain and increase circulation. Low Level Laser Therapy (LLLT) is another light modality used to reduce pain in KO.
Methods: The aim of this study was to compare the effects of the MIPE and LLLT in improving pain and function in KO. Sixty participants with KO completed the program and were randomly assigned into two groups. Group 1 (experimental, n=30) received MIPE and exercises. Group 2 (control, n=30) received LLLT and exercises. Both groups received two visits per week for six weeks. Outcome included pain intensity measured on a visual analogue scale and physical function measured with the lower extremity functional scale, before and after the 12 therapy sessions (6 weeks after the start of the intervention).
Results: There were statistically significant improvements in pain intensity and lower extremity functional scale scores (p<0.05) in each group. However, no significant differences were recorded between the groups (p>0.05).
Conclusion: Therefore, MIPE and LLLT reduce pain and improve function in KO; however, there are no differences between the two modalities in reducing pain and increasing physical function in KO.
Keywords: light, osteoarthritis, knee, monochromatic, LLLT, pain
Introduction
Osteoarthritis is a common musculoskeletal disorder that is highly prevalent in the general population for which there is no optimal treatment1 . Osteoarthritis is the most frequent cause of disability2 .It is characterized by pain and functional limitations2 . Treatment of knee osteoarthritis (KO) focuses on reducing pain and improving physical function2 . Treatment approaches include nonsteroidal anti-inflammatory drugs, hyaluronic acid injection, glucosamine and chondroitin sulphate, aerobic, muscle strengthening and water-based exercises, weight reduction, orthosis, thermal modalities, low level laser therapy (LLLT), acupuncture, biomagentic therapy, transcutaneous electrical nerve stimulation, and ultrasound and acupuncture3-9 . Despite the wide variety of intervention options, the management of KO may be still far from optimal.
The Monochromatic infrared photo energy (MIPE) represents a relatively new approach for treating KO. It has been recently cleared by the United States Food and Drug Administration in 1994 to increase circulation and reduce pain10 . The monochromatic infrared photo energy device is a non-invasive drug-free that delivers MIPE with a wavelength of 890nm10 . The light is emitted by an array of 60 superluminous Gallium Aluminum Arsinide diodes located on flexible pads10 . The diode array must be placed in direct contact with the target skin, as the monochromatic infrared photo energy energizes cells in the epidermis and the most superficial portion of the dermis, thereby warming the skin10 . The 890-nm photo energy penetrates the skin enough to be absorbed by hemoglobin in the rete capillary loops in the papillary dermis, rather than just water in the more superficial layers10 .
The benefits of the MIPE rely on skin contact, pulsation, wavelength, radiant power, and energy density11 . The monochromatic infrared photo energy delivers pulsed adjustable radiant power of up to 10 milliwatts per diode, a power density per diode array of up to 10 milliwatts per cm2, and an energy density of up to 1.6 joules/cm2/minute11 . Therefore, treatment duration of 30 minutes of MIPE can deliver up to 48 joules/cm2 when the diodes are in direct contact with the epidermis11 . The mechanism of action is a combination of topical heat and a transient increase of local release of nitric oxide for pain relief12 .
MIPE has been shown to significantly decrease pain, improve sensation and/or balance in diabetic peripheral neuropathy13-14 . Researchers did not investigate intensively on the MIPE in patients with knee OA.
LLLT is another form of light energy used in managing osteoarthritis. It is a noninvasive, monochromatic electromagnetic high concentrated light beam and has a power output of less than 1W/cm2 15 . LLLT has been used in various neuromusculoskeletal disorders; however, its effectiveness is controversial16 . Some authors suggested that it may be effective in relieving pain in temporomandibular disorders, neck pain with radiculopathy, and shoulder myofascial pain syndrome17-19 . On the other hand, a few authors demonstrated that LLT have no significant effects in low back pain and carpal tunnel syndrome20-21. A few investigators postulated that LLLT may relieve pain and disability in KO22-23 , reduce periarticular swelling when compared to placebo24 .
This may be the first study comparing the effectiveness of MIPE and LLLT on KO. The aim of the present study was to evaluate the short-term effectiveness of two modalities in the treatment of KO: MIPE and LLLT.
Methods
Design
This was a randomized controlled trial with participants randomly assigned to one of two treatment groups: (1) group 1 that received the MIPE and therapeutic exercises or (2) group 2 that received LLLT and therapeutic exercises. The tester made group comparisons at the initial visit (before initiation of treatment) and 6 weeks. The duration of intervention was 6 weeks per participant, and each participant was scheduled to undergo 2 sessions per week.
Participants
Participants who met the inclusion criteria were recruited from an outpatient physical therapy clinic. The inclusion criteria were diagnosis of unilateral KO based on fulfillment of some of the following clinical criteria: persistent knee pain, limited morning stiffness for more than 30 minutes, crepitus, reduced function, or bony enlargement25 .
Reasons for exclusion included considerable deformity of the varus or valgus, ankylosis, malignancy, intense synovitis, arterial circulatory blockage in lower limbs, erosive or destructive alterations detected by radiograph (Kellgren-Lawrence stage 4). Those who received intra-articular glucocorticoid injection within one month of study entry were also excluded. All subjects signed a consent form permitting the use of their data for research purposes, and confidentiality was assured by the use of an anonymous coding system. Participants were asked to refrain from other forms of physical therapy during the study.
Instrumentation
The MIPE intervention was administered using the Anodyne® Therapy System, model 480 (Anodyne Therapy, LLC, Tampa, FL). The device consists of a base power unit and 8 therapy pads, each containing 60 gallium aluminum arsenide diodes. The area of Anodyne LEDs per therapy pads is 22.5 cm2, yielding a total treatment area of 180 cm2 . The device delivers monochromatic infrared photo energy pulsed at 292 Hz with a wavelength of 890 nm through the diodes9 . The active unit provides 62.4 Joules/cm2 of energy density10 .
The Gallium‐Aluminum‐Arsenide (GaAlAs, infrared laser) diode laser device (Chattanooga group, USA) was used with a power output of 100mW and a wavelength of 850 nm. The diameter of the laser beam at the treatment point was 1 mm. The laser was set to deliver a continuous form of energy.
The 10-cm visual analog pain scale (VAS) was used to measure pain because it is reliable, valid and responsive tool for pain intensity26-27 . Physical function was measured by the lower extremity functional scale (LEFS). The LEFS is a valid, reliable and responsive measure in patients with lower extremity dysfunction28 . Moreover, it is an appropriate alternative to the Western Ontario and McMaster Universities Osteoarthritis Index physical function subscale. It is also valid and reliable in assessing group and individual change among orthopedic inpatients 29 . These outcome measurements were obtained at baseline, prior to intervention, and again at 6 weeks following the intervention.
Procedure
Participants who met the inclusion criteria were randomly assigned to one of two groups. Randomization was done by a computer generated random table. Then each patient was tested using the VAS and LEFS. Only one independent investigator, blinded to group allocation, conducted the testing procedures at both the initial and final sessions. After initial testing, participants began the treatment on the same day. Another licensed physical therapist performed all interventions with participants in both groups. All participants received two sessions per week for 6 weeks.
Group 1 received the MIPE for 30 minutes and therapeutic exercises for 20 minutes. Each subject sat comfortably in a quiet room at 21ºC. The skin of the treatment area was covered with plastic wrap as a barrier between the skin and the diodes to ensure compliance with infection control procedures. The therapy pads were put on either side of the knee. The energy setting on the device was preset at 10 bars for every patient, in accordance with the manufacturer's recommendations. The diodes and plastic wrap were removed at the end of the treatment session.
Intervention with the MIPE was followed by therapeutic exercises for 20 minutes. The exercises included active range of motion exercises of the knee (knee mid-flexion to end-range extension in the long sitting position, knee mid-flexion to end-range flexion in the long sitting position and a stationary bicycle). The exercises also included stretching exercises for the hamstring in supine and calf muscles in standing position. Furthermore, participants also received strengthening exercises for the quadriceps, hip extensors, hip abductors, and ankle dorsiflexors in sitting and standing positions.
Group 2 received LLLT (wavelength 850nm, continuous wave, power 100mW) in skin contact at a dose of 5 J/point. The treating therapist irradiated each point for two minutes (a total of 10 minutes). The diameter of the laser beam at the irradiated point was 1 mm. The therapist applied laser to five painful points on both sides of the knee. The points were the medial and lateral epicondyle of the tibia and femur, the medial and lateral knee joint gap, and the medial edge of the tendon of the biceps femoris muscle and semitendinosus muscle in the popliteal fossa.
Participants in group 2 underwent the therapeutic exercises which were the same regimens undertaken by the participants in group 1. The therapist educated all participants regarding the rationale for MIPE and LLLT. The therapist provided verbal and written instructions related to the proper method of exercise, and participants demonstrated their ability to properly perform the prescribed exercises to the treating physical therapist. All participants were instructed to exercise at home on the days that they did not go to the clinic for supervised intervention, and the home program was monitored by asking the participants to record exercise using weekly self-reported exercise logs.
Statistical Analysis
SPSS (Statistical Package for the Social Sciences Inc., Chicago, IL) was used for the statistical analysis, the mean values and standard deviations of the parameters were calculated. Differences between the groups were determined using the Mann‐Whitney U test. The difference within groups between baseline and end of treatment was tested with Wilcoxon test. A 5% level of probability was adopted as the level for statistical significance.
Results
Participants with KO were randomly assigned to two groups. Group 1 consisted of 36 participants and Group 2 consisted of 33 participants. Two patients in the first group and one patient in the second group withdrew for difficult transportation. One participant in the first group withdrew for lack of interest. One participant in the first group and two in the second group withdrew due to time constraints. One participant in the first group withdrew for insurance problems. Therefore, 30 participants completed the study in each group.
60 patients were able to complete the therapy program without any adverse effects. Group 1 (n=30; 18 men and 12 women). Group 2 (n= 30; 17 men and 13 women). Patient flow through the study is shown in the CONSORT flow chart shown in figure 1.
Figure 1 .
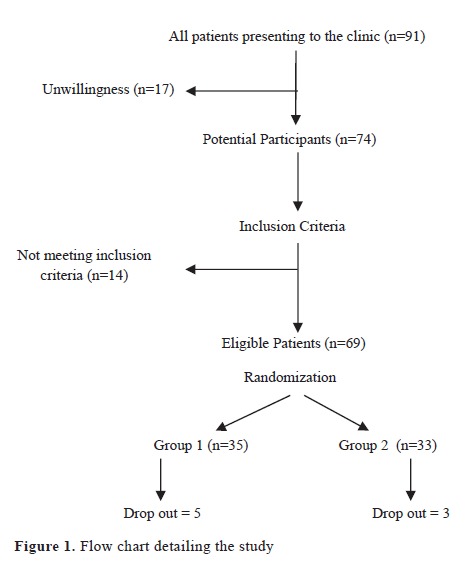
Flow chart detailing the study
Baseline characteristics of the 60 participants who completed the study are given in Table 1. There were no statistically significant differences between the treatment groups in regard to age, height, body weight, and body mass index (P > .05). Mean values and standard deviations of pain intensity and the lower extremity functional scale score at baseline and at 6 weeks are presented in Table 2. In group I, statistically significant improvements in pain intensity and lower extremity functional scale scores were observed compared to baseline scores (p<0.05). In Group 2, all parameters were improved (p<0.05). However, no significant differences were recorded between the groups (p>0.05).
Table 1 . Physical characteristics of the participants (mean ±SD).
| Group 1 (n=30) | Group 2 (n=30) | P value | |
| Age (years) | 37.23± 7.23 | 42.2±4.31 | 0.92 |
| Height (cm) | 168.50±2.01 | 158.63±6.84 | 0.53 |
| Body weight (kg) | 69.39±08.49 | 74.03±10.31 | 0.28 |
| Body mass index kg/m2 | 30.35±7.12 | 26.7±3.34 | 0.34 |
Table 2 . Comparison of mean values of pain severity, and lower extremity functional scores before and after the treatment between the groups .
| Group 1 | Group 2 | P | |
| Pain Intensity | |||
| Baseline (Mean± SD) | 7.21±1.31 | 7.68±1.43 | 0.37 |
| Post-treatment (Mean± SD) | 3.51±1.19 | 4.21±2.11 | 0.24 |
| P | 0.001* | 0.011* | |
| LEFS | |||
| Baseline (Mean± SD) | 38.7±8.13 | 45.21±7.5 | 0.28 |
| Post-treatment (Mean± SD) | 61.41±6.32 | 59.21±9.13 | 0.11 |
| P | 0.001* | 0.021* | |
LEFS: Lower extremity functional scale; SD: Standard deviation.
* P<0.05
Discussion
The present study compared the results obtained after 12 treatment sessions over a period of six consecutive weeks using two different physical modalities in KO. There were no significant differences between the effects of these modalities in KO. However, there were statistically significant differences in decreasing pain and improving physical function in each group. The observed improvements in each group were most likely attributable to the intervention modality. Given the design of the study (which included random assignment to study groups, relatively homogenous groups at the outset, and a blinded tester to group assignment); it might be unlikely that the desirable outcomes were caused by the passage of time or by tester bias.
The author measured pain perception and physical function to get a thorough picture of the outcome of the interventions. The author did not employ other validated tools for measurement of pain and disability such as the Western Ontario and McMaster Universities Osteoarthritis Index physical function subscale or the Lequesne index. However, there is a high correlation between LEFS and these tools29 , and it seems unlikely that incorporation of these tools would have altered the findings of the study.
In group 1, participants experienced improvements in pain and function in response to MIPE treatment. MIPE may reduce pain by promoting release of nitric oxide in the endothelium30 . Nitric oxide relaxes smooth muscle cells in the arteries, veins, capillaries and lymph vessels and results in vasodilatation of the blood vessels and thus increasing circulation31-32 .MIPE treatment increases local blood flow by 400% after a 20-30 minute treatment. Phototherapy elicits changes in cell membrane permeability, resulting in enhanced synthesis of endorphins, increases nerve cell potential and the resulting pain relief31-32 . Thus, release of nitric oxide reduces pain and increases functional ability of the knee joint.
Researchers focused on diabetic peripheral neuropathy13-14 ; however, they did not work intensively on musculoskeletal disorders. There was one study investigating MIPE in 73 patients with KO33 . Hsieh et al conducted a randomized placebo-controlled study33 . Participants received six 40-min sessions of active or placebo MIPE treatment over the knee joints for four weeks. Energy had a wavelength of 890 nm, power of 6.24W, energy density of 2.08J/cm2 /min and total energy received was 83.2 J/cm2 . Patients were assessed according to the International Classification of Functioning, Disability, and Health structure. They failed to find any effect of MIPE on pain, daily living activities, and function.
The improvements of the dependent variables in participants of group 2 which received LLLT agree with the findings of Gur et al.34 , Fukuda et al.35 , Alfredo et al.36 and Alghadir et al.37 . Gur et al.34 compared two different low levels Gallium-Arsenide laser therapy in patients with KO. They divided 90 patients into three groups. Group A received laser (3 J total dose) and exercises. Group B received 3 minutes of laser (2 J total dose) and exercises. Group C received placebo laser and exercises. The authors reported statistically significant improvements in pain, function, and quality of life in both laser groups when compared with placebo laser group (P < 0.05).
Fukuda et al evaluated the use of LLLT for reducing pain and increasing physical function in patients with KO35 . They randomly divided 47 patients into laser and placebo groups. They used a Gallium Arsenide (940 nm laser with mean power of 60 mW and beam area of 0.5 cm2 ). They irradiated nine points on the knee, with energy of 3.0 J/point. Patients in the laser group showed significant differences in pain reduction and improved function compared with the placebo group.
Alfredo et al evaluated the effects of LLLT and exercises on improving pain, strength, function, and range of motion in patients with KO36 . They divided the 40 participants into laser and placebo groups. They showed that LLLT associated with exercises improved pain (P = 0.001), function (P = 0.001) and activity (P<0.001).
Alghadir et al utilized a Gallium-Arsenide diode laser with a power output of 50 mW, a wavelength of 850 nm in 40 patients with chronic KO37 . They randomly divided patients into a laser group and placebo group. They reported decrease of pain, as measured by the visual analog scale and increased knee function using Western Ontario McMaster Universities Osteoarthritis Index scale in comparison with the placebo group.
There are a number of potential biases that could threaten the validity or the conclusions and for these reasons future investigation remains necessary in order to better understand the clinical value of the MIPE in the management of KO. Perhaps the biggest limitation of this study relates to the fact that the sample size was too small to detect differences between groups. Another limitation is the lack of a control group that received no treatment. Therefore, there is a small possibility that both groups may have improved due to the passage of time and avoiding vigorous activity throughout the treatment time. There was a lack of follow-up to demonstrate whether the improvements in each group are sustained in long-term. Based on the results of this randomized, controlled clinical trial, the MIPE and LLLT may be equally effective in decreasing pain and increasing physical function in patients with KO.
Please cite this article as follows:
Tarek AbdelRahman Ali Ammar. Monochromatic Infrared Photo Energy versus Low Level Laser Therapy in patients with Knee Osteoarthritis.J Lasers Med Sci 2014;5(4):176-82
References
- 1.Gross KD, Hillstrom H. Knee osteoarthritis: primary care using noninvasive devices and biomechanical principles. Med Clin North Am. 2009;93(1):179–200. doi: 10.1016/j.mcna.2008.09.007. [DOI] [PubMed] [Google Scholar]
- 2. Murphy L , Helmick CG . The impact of osteoarthritis in the United States: a population-health perspective. Am J Nurs. 2012;112(3 Suppl 1):S13–S19. doi: 10.1097/01.NAJ.0000412646.80054.21. [DOI] [PubMed] [Google Scholar]
- 3.Hale LA, Waters D, Herbison P. A randomized controlled trial to investigate the effects of water-based exercise to improve falls risk and physical function in older adults with lower-extremity osteoarthritis. Arch Phys Med Rehabil. 2012;93(1):27–34. doi: 10.1016/j.apmr.2011.08.004. [DOI] [PubMed] [Google Scholar]
- 4. Wallis JA, Webster KE, Levinger P, Fong C, Taylor NF. A pre-operative group rehabilitation program provided limited benefit for people with severe hip and knee osteoarthritis. Disabil Rehabil 2014; March 16: PubMed PMID: 24597936. [DOI] [PubMed]
- 5.Atamaz FC, Durmaz B, Baydar M, Demircioglu OY, Iyiyapici A. et al. Comparison of the efficacy of transcutaneous electrical nerve stimulation, interferential currents, and shortwave diathermy in knee osteoarthritis: a double-blind, randomized, controlled, multicenter study. Arch Phys Med Rehabil. 2012;93(5):748–56. doi: 10.1016/j.apmr.2011.11.037. [DOI] [PubMed] [Google Scholar]
- 6.Zhang W, Moskowitz RW, Nuki G, Abramson S, Altman RD , Arden N . OARSI recommendations for the management of hip and knee osteoarthritis, Part II: OARSI evidence-based, expert consensus guidelines. Osteoarthr Cartil. 2008;16(2):137–62. doi: 10.1016/j.joca.2007.12.013. [DOI] [PubMed] [Google Scholar]
- 7.Bennell KL, Hunt MA, Wrigley TV, Lim BW , Hinman RS . Muscle and exercise in the prevention and management of knee osteoarthritis: an internal medicine specialist's guide. Med Clin North Am. 2009;93(1):161–77. doi: 10.1016/j.mcna.2008.08.006. [DOI] [PubMed] [Google Scholar]
- 8.Gremion G, Gaillard D, Leyvraz PF , Jolles BM . Effect of biomagnetic therapy versus physiotherapy for treatment of knee osteoarthritis: a randomized controlled trial. J Rehabil Med. 2009;41(13):1090–95. doi: 10.2340/16501977-0467. [DOI] [PubMed] [Google Scholar]
- 9.Cakir S, Hepguler S, Ozturk C, Korkmaz M, Isleten B, Atamaz FC. Efficacy of Therapeutic Ultrasound for the Management of Knee Osteoarthritis: A Randomized, Controlled, and Double-Blind Study. Am J Phys Med Rehabil. 2013;Dec 6 PMID:24322433. doi: 10.1097/PHM.0000000000000033. [DOI] [PubMed] [Google Scholar]
- 10.Burke T. Questions and answers about the MIRE treatment. Adv Skin Wound Care. 2003;12:369–71. doi: 10.1097/00129334-200312000-00016. [DOI] [PubMed] [Google Scholar]
- 11. Belanger AY. Evidence-Based Guide to Therapeutic Physical Agents. Philadelphia, PA: Lippincott Williams & Wilkins; 2002. 191-221.
- 12.Burke TJ. Infrared photo energy may reduce neuropathic pain. Pract pain mang. 2007;7(6):57–63. [Google Scholar]
- 13.Powell MW, Carnegie DH , Burke TJ . Reversal of diabetic peripheral neuropathy with phototherapy (MIRE) decreases falls and the fear of falling and improves activities of daily living in seniors. Age and Ageing. 2006;35(1):11–6. doi: 10.1093/ageing/afi215. [DOI] [PubMed] [Google Scholar]
- 14.Ammar TA. Monochromatic Infrared Photo Energy in Diabetic Peripheral Neuropathy. International Scholarly Research Network ISRN Rehabilitation. 2012:1–8. [Google Scholar]
- 15.Dogan SK, Ay S, and Evcik D. The effectiveness of low laser therapy in subacromial impingement syndrome: a randomized placebo controlled double-blind prospective study. Clinics. 2010;65(10):1019–22. doi: 10.1590/S1807-59322010001000016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Jang H , Lee H . Meta-Analysis of Pain Relief Effects by Laser Irradiation on Joint Areas. Photomed Laser Surg. 2012;30(8):405–17. doi: 10.1089/pho.2012.3240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Salmos-Brito JA, de Menezes RF, Teixeira CE, Gonzaga RK, Rodrigues BH, Braz R. et al. Evaluation of low-level laser therapy in patients with acute and chronic temporomandibular disorders. Lasers Med Sci. 2013;28(1):57–64. doi: 10.1007/s10103-012-1065-8. [DOI] [PubMed] [Google Scholar]
- 18.Rayegani S, Bahrami M, Samadi B, Sedighipour L, Mokhtarirad M, Eliaspoor D. Comparison of the effects of low energy laser and ultrasound in treatment of shoulder myofascial pain syndrome: a randomized single-blinded clinical trial. Eur J Phys Rehabil Med. 2011;4793:381–9. [PubMed] [Google Scholar]
- 19.Konstantinovic LM, Cutovic MR, Milovanovic AN, Jovic SJ, Dragin AS, Letic MD , Miler VM . Low-level laser therapy for acute neck pain with radiculopathy: a double-blind placebo-controlled randomized study. Pain Med. 2010;11(8):1169–78. doi: 10.1111/j.1526-4637.2010.00907.x. [DOI] [PubMed] [Google Scholar]
- 20.Ay S, Doğan SK, and Evcik D. Is low-level laser therapy effective in acute or chronic low back pain? Clin Rheumatol. Clin Rheumatol. 2010;29(8):905–10. doi: 10.1007/s10067-010-1460-0. [DOI] [PubMed] [Google Scholar]
- 21.Evcik D, Kavuncu V, Cakir T, Subasi V, Yaman M. Laser therapy in the treatment of carpal tunnel syndrom,: a randomized controlled trial. Photomed Laser Surg. 2007;25(1):34–9. doi: 10.1089/pho.2006.2032. [DOI] [PubMed] [Google Scholar]
- 22.Kheshie AR, Alayat MS, Ali MM. High-intensity versus low-level laser therapy in the treatment of patients with knee osteoarthritis: a randomized controlled trial. Lasers Med Sci. 2014;Feb 1 doi: 10.1007/s10103-014-1529-0. [DOI] [PubMed] [Google Scholar]
- 23.Gworys K, Gasztych J, Puzder A, Gworys P, Kujawa J. Influence of various laser therapy methods on knee joint pain and function in patients with knee osteoarthritis. Ortop Traumatol Rehabil. 2012;14(3):269–77. doi: 10.5604/15093492.1002257. [DOI] [PubMed] [Google Scholar]
- 24.Yurtkuran M, Alp A, Konur S, Ozcakir S, Bingol U. Laser Acupuncture in Knee Osteoarthritis: A double-blind, randomized controlled study. Photomedicine and Laser Surgery. 2007;25:14–20. doi: 10.1089/pho.2006.1093. [DOI] [PubMed] [Google Scholar]
- 25.Zhang W, Doherty M, Peat G, Bierma-Zeinstra M, Arden N, Bresnihan B, Herrero-Beaumont G. EULAR evidence-based recommendations for the diagnosis of knee osteoarthritis. Ann Rheum Dis. 2010;69:483–9. doi: 10.1136/ard.2009.113100. [DOI] [PubMed] [Google Scholar]
- 26.Boonstra AM, Schiphorst Preuper HR, Reneman MF, Posthumus JB , Stewart RE . Reliability and validity of the visual analogue scale for disability in participants with chronic musculoskeletal pain. Int J Rehabil Res. 2008;31(2):165–9. doi: 10.1097/MRR.0b013e3282fc0f93. [DOI] [PubMed] [Google Scholar]
- 27.Zampelis V, Ornstein E, Franzén H, Atroshi I. A simple visual analog scale for pain is as responsive as the WOMAC, the SF-36, and the EQ-5D in measuring outcomes of revision hip arthroplasty. Acta Orthop. 2014;85(2):128–32. doi: 10.3109/17453674.2014.887951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Binkley JM, Stratford PW, Lott SA, Riddle DL. The lower extremity functional scale: scale development, measurement properties, and clinical applicationNorth American Orthopaedic Rehabilitation Research Network. Phys Ther. 1999;79(4):371–83. [PubMed] [Google Scholar]
- 29.Pua YH, Cowan SM, Wrigley TV , Bennell K . The Lower Extremity Functional Scale could be an alternative to the Western Ontario and McMaster Universities Osteoarthritis Index physical function scale. J Clin Epidemiol. 2009;62(10):1103–11. doi: 10.1016/j.jclinepi.2008.11.011. [DOI] [PubMed] [Google Scholar]
- 30. Matsunaga K , Furchgott RF . Interactions of light and sodium nitrite in producing relaxation of rabbit aorta. J Pharmacol Exp Ther. 1989;248(2):687–95. [PubMed] [Google Scholar]
- 31.Abramson S. Osteoarthritis and nitric oxide. Osteoarthr Cartil. 2008;16(Suppl 2):S15–20. doi: 10.1016/S1063-4584(08)60008-4. [DOI] [PubMed] [Google Scholar]
- 32.Hancock CM, Riegger-Krugh C. Modulation of pain in osteoarthritis: the role of nitric oxide. Clin J Pain. 2008;24(4):353–65. doi: 10.1097/AJP.0b013e31815e5418. [DOI] [PubMed] [Google Scholar]
- 33.Hsieh R, Lo MT, Lee W, Liao W. Therapeutic effects of short-term monochromatic infrared energy therapy on patients with knee osteoarthritis: a double-blind, randomized, placebo-controlled study. J Orthop Sports Phys ther. 2012;42(11):947–56. doi: 10.2519/jospt.2012.3881. [DOI] [PubMed] [Google Scholar]
- 34.Gur A, Cosut A, Sarac AJ, Cevik R, Nas K, Uyar A. Efficacy of different therapy regimes of low-power laser in painful osteoarthritis of the knee: a double-blind and randomized-controlled trial. Lasers Surg Med. 2003;33:330–8. doi: 10.1002/lsm.10236. [DOI] [PubMed] [Google Scholar]
- 35.Fukuda VO, Fukuda TY, Guimarães M, Shiwa S , Martins RA . Short term efficacy of low level laser therapy in patients with knee osteoarthritis: A randomized placebo controlled double blind clinical trial. Revista Brasileira de Ortopedia. 2011;46(5):526–33. doi: 10.1016/S2255-4971(15)30407-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Alfredo PP, Bjordal JM, Dreyer SH, Meneses SR, Zaguetti G, Ovanessian V. et al. Efficacy of low level laser therapy associated with exercises in knee osteoarthritis: a randomized double-blind study. Clin Rehabil. 2012;26(6):523–33. doi: 10.1177/0269215511425962. [DOI] [PubMed] [Google Scholar]
- 37.Alghadir A, Omar MT, Al-Askar AB, Al-Muteri NK. Effect of low-level laser therapy in patients with chronic knee osteoarthritis: a single-blinded randomized clinical study. Lasers Med Sci. 2014;29(2):749–55. doi: 10.1007/s10103-013-1393-3. [DOI] [PubMed] [Google Scholar]


