Abstract
Introduction: Diode laser with wavelengths ranging from 810 to 980 nm in a continuous or pulsed mode was used as a possible instrument for soft tissue surgery in the oral cavity.
Discussion: Diode laser is one of laser systems in which photons are produced by electric current with wavelengths of 810, 940 and 980nm. The application of diode laser in soft tissue oral surgery has been evaluated from a safety point of view, for facial pigmentation and vascular lesions and in oral surgery excision; for example frenectomy, epulis fissuratum and fibroma. The advantages of laser application are that it provides relatively bloodless surgical and post surgical courses with minimal swelling and scarring. We used diode laser for excisional biopsy of pyogenic granuloma and gingival pigmentation.
Conclusion: The diode laser can be used as a modality for oral soft tissue surgery
Keywords: laser, soft tissue, oral surgery
Introduction
Laser systems and their application in dentistry and especially oral surgery are rapidly improving today. The specific advantages of lasers are incision of tissues, coagulation during operation and postoperative benefits. Semiconductor diode lasers (Gallium arsenide (GaAs), gallium-aluminum-arsenide (GaAlAs)) are portable compact surgical units with efficient and reliable benefits. They are assigned according to economic and ergonomic consideration and offer reduced costs in comparison to other modern hard laser devices1. This laser can be used in a continuous or pulsed mode of operation through contact or noncontact application on tissues according to the clinical approach and treatment method. The noncontact delivery is utilized to focus the emitted photons on tissue in order to create larger spot diameter, lower fluency, lower energy and gain for coagulation of superficial lesions, for example in removing the vascular tissues.
Diode laser with wavelengths ranging from 810 to 980 nm in a continuous or pulsed mode was used as a possible modality for soft tissue surgery in the oral cavity. Based on the photothermal effect of the diode laser, the lesions of the oral mucosa are removed with an excision technique, or by ablation/vaporization procedures 2 , 3, 4.
This report was done on the use of diode laser to surgically remove exophytic tissue and pigmented tissue in two cases.
Case number 1: Pyogenic granuloma
A 53 year old woman referred to the dental faculty of guilan medical university, she had exophytic lesion in the buccal mandibular gingiva that aroused eight months before referral time. In her medical history, the patient had been suffering from diabetes mellitus type 2 and for treatment of her disease, she was taking: Glybenglamide tablet 50mg per day, Metformin tablet 100mg per day. The laboratory test (FBS) was made and the result was in normal range.
In the clinical examination the exophytic lesion was seen as a nodule with a size of 1x0.8x1.2cm. The surface of the lesion was smooth, had a fibrotic consistency and had the normal color. The location of lesion was set near the teeth nr 42, the mentioned tooth was vital but had mobility grade III. In panoramic view a vertical bone loss around this tooth was seen. After study on the findings of the characteristic of the lesion (clinical-radiographic), the clinical diagnosis of lesion was made, three lesions were discussed, Figures 1 and 2:
Figure 1.

The clinical feature of the lesion
Figure 2.
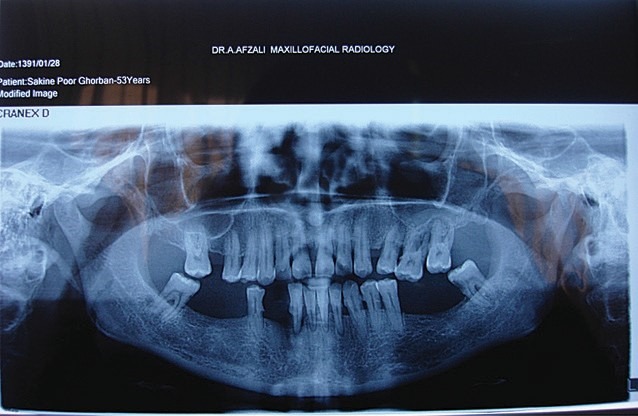
The radiographic (panoramic view) of the lesion
1- Pyogenic granuloma
2- Peripheral ossifying fibroma
3- Peripheral giant cell granuloma
Treatment plan was designed as excisional biopsy of the lesion and histologic evaluation of this abnormality. For this aim we used diode laser class IV (CHEESE ™ type made by GIGGA laser CO, UK) with wavelength 810nm, output power 3.5 W CW, 200 um fiber and cut the lesion from the base, because the of the laser beams wer not seen by eyes,the guiding light was prepared by manufacture company and was looked as red light during operation, Figure 3.the lesion was cut at the base,but we observed massive hemorrhage from the surgery area and for its control we moved the laser fiber tip in a sweeping way on the surgical site in order to achieve coagulation, after many seconds hemostasis occurred and somehow the surface of the lesion was carbonized, thus, there was no need to suture the surgical site and the wound would be healed with secondary intention, Figure 4. After finishing this process, the biopsy sample was put in a fixative agent (formalin 10% solution) and sent for microscopic evaluation, Figure 5. The result of microscopic evaluation was:” pyogenic granuloma”. Follow up of the treatment process occurred after ten days from removal of lesion, somehow, healing of the surgery site occurred and repair of the epithelium was performed completely; Figure 6.
Figure 3.

The application the diode laser(Gigga) and view of guiding light during operation
Figure 4.

The coagulation of the location after removing the lesion
Figure 5.
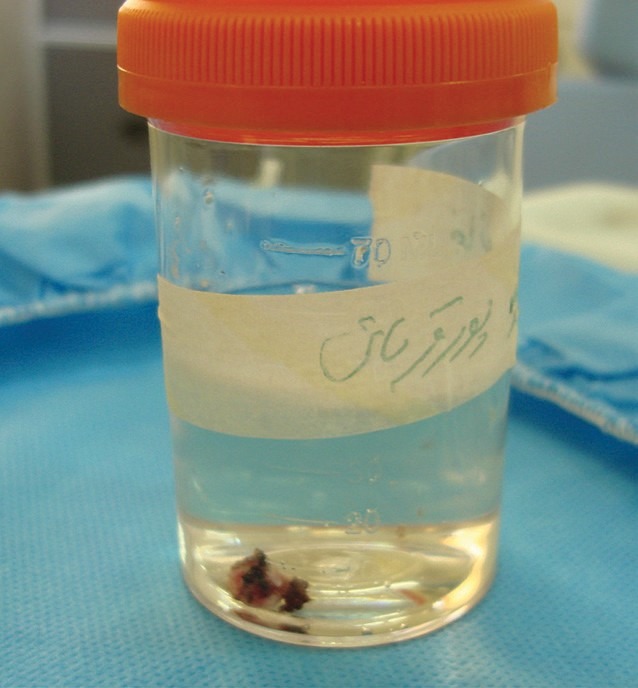
The biopsy sample in a fixative formalin solution10%
Figure 6.

Follow up the patient after ten days
Case number 2
A 26 year old woman referred to practice because she had complaints regarding darkening of gingival color during smiling. Gingival pigmentation is created by production and accumulation of melanin in basal layer and lamina propria. Oral pigmentation is a process that occurs from many etiologic causes, for example: physiologic pigmentation, smoking, endocrine disturbances, drug adverse reactions, HIV infection. In oral examination, in the buccal aspect of the attached gingiva of lower and upper jaws, a diffuse pigmentation as “patch” was seen.
- No history of the consumption of drugs induced pigmentation.
- No history of systemic disease (Addison and Cushing disease,…).
- No consumption of smoking
We ruled out other causes of pigmentation in lamina propria of gingiva through clinical process (Figure 7). There are many procedures for the treatment of this lesion such as periodontal surgery, use of caustic material and laser therapy. Laser therapy has many beneficial effects that are mentioned such as; removal of gingival pigmentation for esthetic, faster action and no need for sutures and flaps, also diode laser has the best absorption for melanin and hemoglobin in comparison to other laser types. Therefore, we decided to use this type of laser in order to treat the lesion.
Figure 7.

The difusse physiologic hyperpigmentation of gingiva of the patient before laser therapy
The treatment plan was performed; first, the area was anesthetized by lidocaine 2% with epinephrine 1/100000 cartridge by infiltration technique. After this, retraction of upper lip was made by Minoseta retractor. We used diode laser Ezlase 940 nm wavelength, made by Biolase Co (Germany) with 1.5W CW, 400μm fiber, in sweeping motion. The diode laser was set and safety protection such as use of specific room, wearing specific eye glass was applied. Then we used the laser tip on the surface of the lesion in contact mode. In this process almost three minutes after laser therapy, the de-epithelialization of gingiva occurred, then we scratched a piece of wet sterile gauze on the de- epithelialized surface and detached the epithelium, after what the laser was irradiated on the denuded area for coagulation of this area, in spite of this some carbonization of the affected area happened (Figures 8,9). During the process despite ventilation the little amount of fume and burning smell had caused some discomfort to the patient. The follow up occurred after one month and repair of epithelium was completely achieved, Figure 10.
Figure 8 .

The laser therapy of the lesion with use of Ezlase and contact mode of operation
Figure 9.

The denuded area after laser therapy, the remants of epithelium was removed by pulling wet sterilized dental gaz on the area
Figure 10.

The follow up the patient after one month,the healing was occurred compleletly,and the pink color of the upper gingiva in comparison to lower gingiva was seen
Discussion
One of the applications of lasers in dentistry is soft tissue surgery and ablation of lesions. The excision of exophytic lesions is one of this utilization. The advantages of laser application are relatively bloodless surgery, minimal swelling, scarring and coagulation, no need for suturing, reduction in surgical time and less or no post surgical pain. Also, the laser instantly disinfects the surgical wound as well as allowing a noncontact type of operative procedure and therefore no mechanical trauma to the tissue 5 , 6, 7.
Laser transmits energy to the cells causing warming,welding, coagulation, protein denaturation, drying, vaporization and carbonization. The diode laser was introduced in dentistry and oral surgery in the mid-90s 6 , 8. The diode laser devices have specifications such as relatively small size, portable and lower cost that attract the dental practitioners and oral surgeons for use in various surgical indications in comparison to other laser equipment1, 9, 10. The pump source is an electrical current, the photons are produced by electric current and laser active medium is semiconductor. The diode lasers have been used in three wavelengths 810,940 and 980nm in surgical treatments. Provided correct selection and application of diode lasers in soft tissue oral surgery, for example frenectomy, epulis fissuratum, fibroma, facial pigmentation and vascular lesions, they are safety and useful4. The side effects and harmful consequences of diode lasers were studied in many researches for example in Janda et al research, they evaluated the thermal tissue effects of two diode lasers Holmium Yttrium Aluminium Garnet(Ho:YAG), Neodymium-Doped Yttrium Aluminium Garnet(Nd:YAG) with wavelengths of 830 and 940 nm in contact application. They observed that diode laser had low thermal effect on depth of carbonized zones at the surface of the tissue in histological examination11. In another experimental study, performed by Goharkhay et al, they compared the histological effects of treatment with laser on the oral mucosa of fresh pig mandibles using a diode laser with a wavelength of 810 nm and surgical blade. They surveyed the vertical and horizontal tissue damage as well as incision depth and width of the oral mucosa. They showed that the epithelial damage occurred and the depth of damage depended on penetration, and correlated strongly with average powers used, but not with other laser parameters or the tip diameter12. In almost all researches the scientists declared the unique specialties of lasers and particularly diode lasers such as; sharp and definite cutting edge, hemostasis and coagulation after surgery in addition to small size and better maneuver during application, which makes this laser very effective and a useful alternative device in soft tissue surgery in the oral cavity in comparison to other lasers types such as Carbon Dioxide Laser (CO2) and erbium lasers. The disadvantages reported in researches on diode laser application were somehow similar to other lasers, like, delayed repair which is prominent in larger lesions and charring tissue in smaller lesions compared to the application of conventional scalpel surgical procedures and laser plume in excision of exophytic lesions produced by human papilloma virus and may be creates similar lesions in upper respiratory tract of laser operator13. In our study the definite incision of lesion was accomplished and in spite of the broad ulcer created in the surface, hemostasis occurred on the surface of ulcer after laser irradiation and because of this, we didn’t need to suture the area. Also, the patients were acquiescent during and after laser therapy. And despite the burned border of the biopsy species, the majority of the biopsy sample was safe for histopathologic examination. But in studies accomplished on diode lasers in comparison to CO2 lasers, it was reported that the thermal damage zone and marginal damage of biopsy species were less in CO2 laser and thus because of damaged tissue they didn’t relieve definite diagnosis by histopathology examination and this is related to the smaller size lesions and technical method, this may be one of the main disadvantages of diode laser application, but this matter did not occur in our study. Small size of the equipment and easy application of diode laser for fibers conduction system was observed in comparison to arms conduction system in Co2 laser. The most common complication after laser surgery mentioned in the literature is pain and discomfort 6 , 7, 14, 15. Postoperative bleeding is only reported in a study for laser-assisted uvulopalatoplasty in Brandon & Strauss 2004 research and was not encountered after other treatments, for example the treatment of the pyogenic granuloma in the present study16. Otherwise, decreased postoperative swelling and improved tissue healing and scarring are reported. However, in the present study, we did not evaluate these parameters with objective methods including a proper control group (scalpel incision), and the number of participants was not high enough to do so. Therefore, the findings are inconclusive in that regard. Laser induced wounds because of definite and clean wound, generally heal with secondary intention and no scar formation compared to scalpel incisions. This is may be due to the minimal degree of wound contraction following laser irradiation which occurs through induction and formation of smaller number of myofibroblasts and collagen18 , 19. During the operation while performing the incision some fume were released from vaporization of epithelium with a burning smell, which can provoke stress and hurt in the patient, and for relief of this complication, it is necessary to operate with a powerful air evacuator, and to offer a block by temporary dam20.
Conclusion
Diode lasers can be used in oral soft tissue surgery and especially small prominent lesions because of easy application, better coagulation, no need for suturing, less swelling and pain, as well as for its capability for treatment of physiologic gingival pigmentation from an esthetic point of view. It can be considered as a first choice despite periodontal surgery due to; faster action, better de-epithelialization, no bleeding and better repair.
Please cite this article as follows:
Ehsan Azma, Nassimeh Safavi. Diode Laser Application in Soft Tissue Oral Surgery. J Lasers Med Sci 2013; 4(4):206-11
References
- 1.Deppe H, Horch HH. Laser applications in oral surgery and implant dentistry. Lasers Med Sci. 2007;22:217–21. doi: 10.1007/s10103-007-0440-3. [DOI] [PubMed] [Google Scholar]
- 2.Romanos G, Nentwig GH. Diode laser (980) in oral and maxillofacial surgical procedures: clinical observations based on clinical applications. J Clin Laser Med Surg. 1999;17(5):193–7. doi: 10.1089/clm.1999.17.193. [DOI] [PubMed] [Google Scholar]
- 3.Coluzzi D. Fundamental of lasers in dentistry: Basic science, tissue interaction, and instrumentation. J Laser Dent. 2008;16:4–10. [Google Scholar]
- 4.Desiate A, Cantore S, Tullo D, Profetta G, Grassi FR, Ballini A. 980 nm diode lasers in oral and facial practice: current state of the science and art. Int J Med Sci. 2009;6(6):358–64. doi: 10.7150/ijms.6.358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Eliades A, Stavrianos C, Kokkas A, Kafas P, Nazaroglou I. 808 nm diode laser in oral surgery: A case report of laser removal of fibroma. Res J Med Sci. 2010;4(3):175–8. [Google Scholar]
- 6.Pick RM, Pecaro BC. Use of the CO2 laser in soft tissue dental surgery. Lasers Surg Med. 1987;7:207–13. doi: 10.1002/lsm.1900070213. [DOI] [PubMed] [Google Scholar]
- 7.Pecaro BC, Garehime WJ. The CO2 laser in oral and maxillofacial surgery. J Oral Maxillofac Surg. 1983;41:725–8. doi: 10.1016/0278-2391(83)90189-1. [DOI] [PubMed] [Google Scholar]
- 8. Harris DM, Pick RM. Laser physics. In: Lasers in Dentistry. Miserendino LJ, Pick RM (editors); 1995. Quintessence, Chicago: pp 27–38.
- 9.Coleton S. Lasers in surgical periodontics and oral medicine. Dent Clin North Am. 2004;48:937–62. doi: 10.1016/j.cden.2004.05.008. [DOI] [PubMed] [Google Scholar]
- 10.Andreana S. Andreana SThe use of diode lasers in periodontal therapyLiterature review and suggested technique. Dent Today. 2005;24:130–5. [PubMed] [Google Scholar]
- 11.Janda P, Sroka R, Mundweil B, Betz CS, Baumgartner R, Leunig A. Comparison of thermal tissue effects induced by contact application of fiber guided laser systems . Lasers Surg Med. 2003;33:93–101. doi: 10.1002/lsm.10199. [DOI] [PubMed] [Google Scholar]
- 12.Goharkhay K, Moritz A, Wilder-Smith P, Schoop U, Kluger W, Jakolitsch S. et al. Effects on oral soft tissue produced by a diode laser in vitro. Lasers Surg Med. 1999;25:401–6. doi: 10.1002/(sici)1096-9101(1999)25:5<401::aid-lsm6>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 13.D’Arcangelo C, Di Nardo Di Maio F, Prosperi G D, Conte E, Baldi M, Caputi S. A preliminary study of healing of diode laser versus scalpel incisions in rat oral tissue: a comparison of clinical, histological, and immunohistochemical results. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:764–73. doi: 10.1016/j.tripleo.2006.08.002. [DOI] [PubMed] [Google Scholar]
- 14.Frame JW. Removal of oral soft tissue pathology with the CO2 laser. J Oral Maxillofac Surg. 1985;43(11):850–5. doi: 10.1016/0278-2391(85)90221-6. [DOI] [PubMed] [Google Scholar]
- 15.Bornstein MM, Suter VGA, Stauffer E, Buser D. [The CO2 laser in stomatology: Part 1.] Schweiz Monatsschr Zahnmed. 2003a;113:559–70. German. [PubMed] [Google Scholar]
- 16.Brandon MS, Strauss RA. Complications of CO2 laser procedures in oral and maxillofacial surgery. Oral Maxillofac Surg Clin North Am. 2004;16:289–99. doi: 10.1016/j.coms.2004.01.005. [DOI] [PubMed] [Google Scholar]
- 17.Fisher SE, Frame JW, Browne RM, Tranter RMD. A comparative histological study of wound healing following CO2 laser and conventional surgical excision of canine buccal mucosa. Arch Oral Biol. 1983;28:287–91. doi: 10.1016/0003-9969(83)90069-9. [DOI] [PubMed] [Google Scholar]
- 18.Chomette G, Auriol M, Labrousse F, Vaillant JM. [The effect of CO2 laser radiation on the morphological changes of mucocutaneous wound healing in oral surgery A histoenzymologic and ultrastructural study] Rev Stomatol Chir Maxillofac. 1991;92:1–7. French. [PubMed] [Google Scholar]
- 19.Zeinoun T, Nammour S, Dourov N, Aftimos G, Luomanen M. Myofibroblasts in healing laser excision wounds. Lasers Surg Med. 2001;28(1):74–9. doi: 10.1002/1096-9101(2001)28:1<74::AID-LSM1019>3.0.CO;2-B. [DOI] [PubMed] [Google Scholar]
- 20.Suter VG, Altermat HJ, Sendi P, Mettraux G, Bornstein MM. Co2 and diode laser for excisional biopsies of oral mucosal lesions. Schweis Monatsshr Zahnmed. 2010;120(8):664–71. [PubMed] [Google Scholar]


