Abstract
Objectives
The purpose of the DEFINITIVE Ca++ study was to evaluate the safety and effectiveness of directional atherectomy and distal embolic protection, used together to treat moderate to severely calcified femoropopliteal lesions.
Background
Despite advances in endovascular treatment modalities, treatment of calcified lesions remains a challenge.
Methods
A total of 133 subjects with 168 moderate to severely calcified lesions were enrolled. Lesions were treated with directional atherectomy devices, coupled with distal embolic protection.
Results
The 30-day freedom from MAE rate was 93.1%. Per angiographic core laboratory assessment, the primary effectiveness endpoint (≤50% residual diameter stenosis) was achieved in 92.0% (lower confidence bound of 87.6%) of lesions. By core lab analysis, these results did not achieve the success criteria (90%) for the primary effectiveness objective. Per site assessment, the objective was met with the endpoint being achieved in 97.0% (lower confidence bound 93.8%). A mean residual diameter stenosis of 33.3% was achieved with the directional atherectomy device. This was further decreased to 24.1% with the use of adjunctive therapy. The proportion of asymptomatic subjects [Rutherford Clinical Category (RCC) = 0] increased from 0% at baseline to 52.3% at the 30-day follow-up visit. In total, 88.5% of subjects experienced an improvement of one or more Rutherford categories.
Conclusions
The results of the DEFINITIVE Ca++ study demonstrate that the SilverHawk™ and TurboHawk™ atherectomy devices are safe and effective in the endovascular treatment of moderate to severely calcified lesions in the superficial femoral and/or popliteal arteries when used with the SpiderFX™ distal embolic protection device. © 2014 Wiley Periodicals, Inc.
Keywords: peripheral arterial disease, plaque excision, filter protection, atherosclerosis, peripheral vascular disease, revascularization
INTRODUCTION
The use of endovascular therapies as primary treatment for peripheral arterial disease (PAD) is increasing. Endovascular therapies include percutaneous transluminal angioplasty (PTA), stenting and more recently directional atherectomy, which removes plaque from the vessel to increase lumen size. Recent studies have documented that directional atherectomy is safe for the treatment of peripheral arterial disease and has low reintervention rates, acceptable complication rates 1–8, and less need for bail out stenting 9.
The second TransAtlantic Inter-Society Consensus (TASC II) document on management of PAD recommends endovascular treatment as the first choice for revascularization of a variety of lesions types, including heavily calcified occlusions ≤5 cm in length 10. However, treatment of calcified lesions is a challenge and calcium content in plaque was shown to increase as one progresses distally in the arterial tree of patients with PAD 11. Treatment of calcified lesions with PTA is often suboptimal with high rates of dissection and need for bail out stenting 12. Adding to the complexity of treating calcified lesions is the increased risk of distal embolization 13. Distal embolization requiring subsequent retrieval is correlated with longer fluoroscopy times, more contrast use and longer procedure times 14. Moreover, distal embolization has been shown to significantly lower limb salvage rates and freedom from recurrent symptoms 13.
This study utilized the SilverHawk LS-C and the TurboHawk LS-C and LX-C plaque excision atherectomy devices (SilverHawk™ and TurboHawk ™ plaque excision systems, Covidien, Plymouth, MN). Previously, these devices have been used in a surgical setting to facilitate the breakdown of complex, hard, calcified tissue that may be resistant to conventional treatment. In this study, the directional atherectomy devices were used in an endovascular fashion with a filter (SpiderFX™ embolic protection device, Covidien, Plymouth, MN) deployed distally to mitigate the risk of embolic complications in downstream arteries. The SpiderFX filter has been effectively and safely used in several prior studies but in less calcified lesions and with a high rate of embolic debris capture 9,15,16. The purpose of the DEFINITIVE Ca++ study was to evaluate the safety and effectiveness of this technique, use of the directional atherectomy and embolic protection together, to treat moderate to severely calcified lesions. Data obtained in this study was used to gain extended indications for the SpiderFX filter and plaque excision devices.
METHODS
Study Design
The DEFINITIVE Ca++ study was a prospective, multi-center, single-arm study. Patients with symptomatic peripheral arterial disease [Rutherford clinical categories (RCC) 2–4] who met the general inclusion/exclusion criteria were required to provide written informed consent prior to any study-related activities. Inclusion and exclusion criteria are listed in Table1.
Table 1.
DEFINITIVE Ca++ Inclusion and Exclusion Criteria
| Inclusion criteria | Exclusion criteria |
|---|---|
| • Has a RCC Score of 2, 3 or 4. | • •Has known hypersensitivity to nitinol. |
| • Is willing to comply with all follow-up evaluations at the specified times. | • Has known hypercoagulable condition, or refuses blood transfusion. |
| • Is ≥ 18 years old. | • Is female with childbearing potential not taking adequate contraceptives or is currently breastfeeding. |
| • Provides written informed consent prior to any study-related procedures and enrollment in the study. | • Has life expectancy of <12 months. |
| • Has target lesion(s) located within the native femoropopliteal artery with target vessel diameter ≥3.5 mm and ≤7.0 mm, with the proximal point of the target lesion at least one cm below the origin of the profunda femoralis. | • Has any planned surgical intervention or endovascular procedure 30 days after the index procedure. |
| • Target lesion(s) has moderate to severe calcification visualized on angiogram. | • Has surgical or endovascular procedure of the target vessel within 30 days prior to the index procedure. |
| • Has evidence of ≥75% stenosis in the target lesion(s) confirmed by angiography. | • Is currently participating in an investigational drug or another device study that has not completed the primary endpoint or that clinically interferes with the current study endpoints. |
| • The target lesion(s) total length is ≤15 cm and any individual target lesion is ≤10 cm as determined by a spatially calibrated measurement using a device with known distance between radiopaque markers | • The guidewire cannot cross the target lesion and/or a subintimal approach is required. |
| • There is at least one target lesion identified to be treated. | • Has significant stenosis or occlusion of inflow tract not successfully treated before the treatment of the target lesion. |
| • There is evidence of at least single vessel runoff to the ankle/foot of the limb to be treated that does not also require treatment for significant (>50% stenosis or occlusion) stenosis during the index procedure. Treatment of infrapopliteal lesions must be staged at least 30 days before or after the index procedure. | • There is presence of an aneurysm in a target vessel. |
| • There is evidence that a SpiderFX can be placed in a vessel 3–6 mm in diameter and at least eight cm beyond the distal edge of the target lesion. | • There is presence of an acute intraluminal thrombus at the proposed lesion site. |
| • One or more of the following occurred prior to enrollment: clinical perforation, dissection (grade C or greater), pseudo-aneurysm, thrombosis, distal embolism, or other injury requiring additional stenting or surgical intervention prior to crossing the first target lesion. | |
| • The target lesion is an in-stent restenosis. | |
| • There is known or suspected active systemic infection. | |
| • The subject has other comorbid condition(s) that, in the judgment of the physician preclude(s) safe percutaneous intervention. | |
| • A lesion in the nontarget limb is treated on the same day as the target limb. |
The protocol was approved by the US food and drug administration (FDA) under an investigational device exemption and by each investigational site's Institutional Review Board. The study was conducted in accordance with Good Clinical Practice and was overseen by a steering committee. An angiographic core laboratory (Beth Israel Deaconess Medical Center, Boston, MA) provided independent analyses of radiographic images and a Clinical Events Committee (CEC) adjudicated all adverse events.
Devices
The SilverHawk LS-C and TurboHawk LS-C and LX-C devices, shown in Fig. 1, are catheters with a blade that rotates at the distal end of a flexible catheter shaft. The “LS-C” suffix signifies the model if for a large vessel (3.5–7 mm) with a standard tip length (6 cm) and a cutter designed for calcified plaque. The “LX-C” indicates the model has a long (or “xtended,” 9 cm) nosecone. When activated, the catheter is slowly advanced across the lesion, “shaving” occlusive material from the artery. The excised tissue is captured in the tip of the device. This cutting sequence can be repeated as many times as necessary to achieve the desired degree of plaque excision.
Fig 1.

TurboHawk plaque excision system. [Color figure can be viewed in the online issue, which is available at wileyonlinelibrary.com.]
Revisions to the SilverHawk device were made during the study to allow improved excision of more complex plaque, thereby creating a device designed specifically for calcific plaque. The TurboHawk device incorporated subsequent design changes which deliver a more consistent spin rate to the cutting blade and consistent apposition to the vessel wall. Additionally, the blade was redesigned to enable improved cutting in hard, calcified tissue.
The SpiderFX filter, shown in Fig. 2, is a nitinol mesh filter mounted on a PTFE-coated 0.014-in stainless steel wire. The delivery system can be advanced over any 0.014-in. guidewire. The wire on which the filter is mounted was utilized as the guidewire for the directional atherectomy catheters, and filter position was determined by the investigator.
Fig 2.
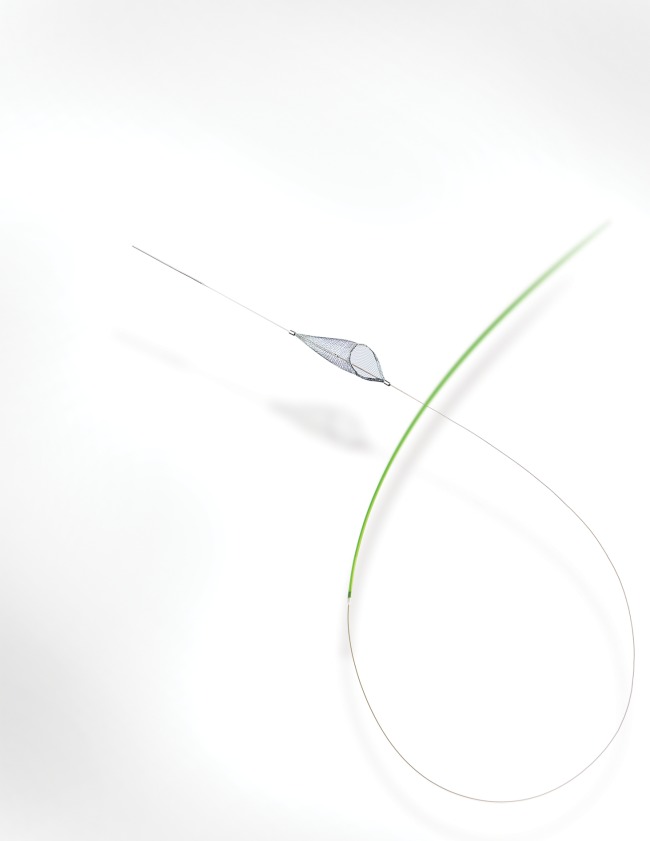
SpiderFX embolic protection device. [Color figure can be viewed in the online issue, which is available at wileyonlinelibrary.com.]
Procedure
Patients were enrolled after angiographic evaluation confirmed the lesion characteristics met study requirements (Table1) per operator assessment, and the target lesion was successfully crossed. All moderate to severely calcified lesions that met the inclusion/exclusion criteria were to be considered target lesions.
Patients were medically managed for PAD per AHA/ACC guidelines and received anticoagulation as determined by the operator to maintain appropriate clotting times. Operators were instructed to select a filter size slightly larger than the vessel diameter. For example, a size 7 mm for a peripheral vessel 4.5–6 mm in diameter. They were also instructed to place the filter at least 2 cm distal to the point at which the tip of the atherectomy catheter would reach. This 2 cm “stand-off” distance ensured the tip of the catheter didn't pull the mouth of the filter away from the vessel wall, compromising complete apposition.
Following filter placement, directional atherectomy was completed per standard practice. Stand-alone directional atherectomy was encouraged, but adjunctive therapy, including PTA, stent, and any FDA-approved devices, was permitted for any of the following: dissections (grade C or greater), perforations, occlusive complications, and residual stenosis ≥30% following atherectomy. Angiographic images demonstrating the target lesion(s) stenosis in views that minimized the degree of vessel overlap and demonstrated the stenosis in its most severe view were obtained. Angiographic images were acquired before and after treatment with SilverHawk/TurboHawk and after any adjunctive therapy. The angiographic core laboratory assessed percent residual diameter stenosis, number of distal run-off vessels (to the ankle/foot), lesion morphology and provided qualitative morphological data.
Post-procedural follow-up through 30 days consisted of a physical examination, assessment of RCC and adverse event evaluation.
Endpoints and Definitions
The primary safety endpoint was defined as the absence of major adverse events (MAE) to 30 days post-procedure. MAE was defined as any serious adverse event leading to death, myocardial infarction (MI), vessel dissection classified as ≥ Type C (as classified by the National Heart, Lung and Blood Institute), clinical perforation, pseudoaneurysm, thrombosis, clinically relevant distal embolization (defined as requiring surgical or medical intervention and/or the presence of symptoms, unplanned amputation, or clinically driven target vessel revascularization (TVR)).
The primary effectiveness endpoint was successful revascularization of the target vessel defined as ≤50% residual diameter stenosis following directional atherectomy. Both investigator and core laboratory assessments of this endpoint were recorded.
Predefined secondary endpoints included (1) technical procedural success defined as meeting the following requirements: no procedure-related MAE, ≤50% residual stenosis at the target lesion, no device malfunction causing the procedure to be aborted, and successful delivery and placement of the filter; (2) <30% residual stenosis following directional atherectomy and any additional adjunctive therapy; (3) presence of debris in the directional atherectomy device nosecone and the filter by visual inspection; and (4) preservation of runoff distal to the filter. All endpoints were determined by core laboratory assessment and/or CEC adjudication.
Severe calcification was defined as the presence of radiopacities noted on both sides of the arterial wall and extending more than one cm of length prior to contrast injection or digital subtraction angiography. Moderate calcification was defined as the presence of radiopacities on one side of the arterial wall or less than one cm of length prior to contrast injection or digital subtraction angiography. Because there is no standard definition, this definition was agreed upon by the study's national principal investigators and the Food and Drug Administration.
Statistical Analysis
The study was designed to compare to performance goals (PGs) derived from the TALON registry 4, the largest study on the use of SilverHawk devices at the time of protocol development. Registry data provided estimates for a PG of 90.0% for effectiveness and a PG for MAE-free rate of 85.5% at 30 days, although the data evaluated in the TALON registry were site-reported without independent evaluation.
Data were analyzed for all patients enrolled and standard summaries provided. Confidence intervals for the primary effectiveness endpoint were computed using generalized estimating equations to account for intrapatient correlation in the case of multiple lesions; for the primary safety endpoint confidence intervals were computed using exact methods. The sample size of 133 was selected to provide at least 80% power against the predefined performance goals. All P values were two-sided with values <0.05 deemed statistically significant.
RESULTS
Between October 2008 and October 2010, 133 patients (168 lesions) were enrolled at 17 investigational sites in the United States. The mean age was 69.7 years, 71.4% were male and 47.4% of patients presented with diabetes. Roughly one-third (31.6%) of the population had moderate claudication, 52.6% had severe claudication and 15.8% had ischemic rest pain. Demographics and clinical risk factors are provided in Table2. The mean lesion length was 39.0 ± 27.0 mm, 17.9% of lesions were occluded and 81.0% were severely calcified. Lesion characteristics as assessed by the investigators and the angiographic core laboratory are provided in Table3. A third (31.6%) of patients had single-vessel run-off, 44.4% had two-vessel run-off and 24.1% had three-vessel run off.
Table 2.
Baseline Characteristics
| Subject characteristics | N = 133 |
|---|---|
| Age (years) | |
| Mean ± SD (N) | 69.7 ± 9.8 (133) |
| Range (min, max) | (41.0, 95.0) |
| Male | 71.4% (95/133) |
| Race | |
| White | 78.9% (105/133) |
| Black | 15.8% (21/133) |
| Asian | 1.5% (2/133) |
| Unknown | 3.0% (4/133) |
| Other | 0.8% (1/133) |
| Hispanic or Latino | 6.0% (8/133) |
| Risk factors | |
| Diabetes | 47.4% (63/133) |
| History of hypertension requiring medication | 91.7% (122/133) |
| History of MI* | 30.8% (41/133) |
| Hyperlipidemia | 88.0% (117/133) |
| History of CABG or PCI* | 52.6% (70/133) |
| History of major amputation | 0.8% (1/133) |
| Family history of CAD* | 49.6% (66/133) |
| History of peripheral intervention | 57.1% (76/133) |
| History of smoking | 78.9% (105/133) |
| CVA/TIA* | 15.8% (21/133) |
| Renal insufficiency | 24.8% (33/133) |
| Rutherford clinical category | |
| 2 (moderate claudication) | 31.6% (42/133) |
| 3 (severe claudication) | 52.6% (70/133) |
| 4 (ischemic rest pain) | 15.8% (21/133) |
Table 3.
Baseline Target Lesion Characteristics
| Baseline target lesion characteristics | Site-reported (N = 169) | Core laboratory-reported (N = 168a) |
|---|---|---|
| Lesion length (mm) | 43.4 ± 30.5 (169) | 39.0 ± 27.0 (168) |
| Preprocedure reference vessel diameter (mm) | 5.5 ± 0.7 (169) | 4.9 ± 0.9 (168) |
| Preprocedure minimum lumen diameter (mm) | Not reported | 1.1 ± 0.8 (168) |
| Preprocedure diameter stenosis (%) | 88.3 ± 8.5 (169) | 76.5 ± 15.4 (168) |
| Occlusion | 9.5% (16/169) | 17.9% (30/168) |
| Arterial Segment Treated | ||
| Proximal superficial femoral artery | 11.8% (20/169) | 14.3% (24/168) |
| Mid superficial femoral artery | 38.5% (65/169) | 31.5% (53/168) |
| Distal superficial femoral artery | 36.1% (61/169) | 43.5% (73/168) |
| Proximal popliteal | 8.3% (14/169) | 9.5% (16/168) |
| Mid/distal popliteal | 5.3% (9/169) | 1.2% (2/168) |
| Type of lesion | ||
| Restenotic | 12.4% (21/169) | Not reported |
| De Novo | 87.6% (148/169) | Not reported |
| Lesion Eccentricity | ||
| Concentric/none | 18.3% (31/169) | 41.7% (70/168) |
| Eccentric | 81.7% (138/169) | 58.3% (98/168) |
| Calcification | ||
| None/Mild | 0% (0/169) | 6.0% (10/168) |
| Moderate | 47.9% (81/169) | 13.1% (22/168) |
| Severe | 52.1% (88/169) | 81.0% (136/168) |
Per angiographic core laboratory assessment there were 168 lesions; in one subject, the site reported two discrete lesions while the angiographic core laboratory reported a single diffuse lesion.
Procedures
The SpiderFX filter was successfully deployed at the intended site in 97.2% of patients. Predilatation was performed for 41 lesions in 34 subjects. Lesions that were predilated had a higher degree of stenosis (81.5% vs. 74.9%, P = 0.016) and were more likely to be severely calcified (92.7% vs. 77.0%, P = 0.038) than those that were not predilated. Accordingly, residual stenosis was significantly higher in predilated lesions postdirectional atherectomy (37.8% vs. 31.9%, P = 0.016), although not postprocedure (26.8% vs. 25.1%, P = 0.40). Excised plaque was present in 97.0% (129/133) of directional atherectomy devices' tips and 88.4% (122/138) of deployed filters. Capture of debris in sufficient quantities to require filter retrieval and use of a second filter device occurred in two patients (1.5%). A full basket was identified in one case by slow blood flow beyond the filter by angiographic assessment. In the second case, the operator retrieved the filter, found it was full, and then deployed a new filter after deciding to make additional passes with the atherectomy device.
Procedure characteristics are presented in Table4. Adjunctive therapy was performed for 91 (53.8%) lesions in 74 subjects. The primary mode of adjunctive therapy was PTA with a mean maximum pressure of 5.6 atm. Per site assessment, residual diameter stenosis after directional atherectomy was 25.8% ± 16.5%, and following adjunctive therapy 12.9% ± 9.8%. Per core laboratory evaluation, residual diameter stenosis after directional atherectomy and at the conclusion of the procedure was 33.3% ± 13.4% and 24.1% ± 10.9%, respectively.
Table 4.
Procedure Characteristics
| Procedure characteristic | Mean ± SD or % (n N−1) |
|---|---|
| Total procedure time (min) | 74.2 ± 28.4 (133) |
| Total fluoroscopy time (min) | 21.1 ± 9.7 (132) |
| Total contrast administered (cm3) | 182.3 ± 72.4 (132) |
| Visible debris in filter device | 88.4% (122/138) |
| Adjunctive therapy | 53.8% (91/169) |
| Adjunctive (bail-out) stenting | 4.1% (7/169) |
| Preservation of run-off (per angiographic core lab) | 98.3% (113/115) |
The bail-out stent rate was 4.1% (7/169). Reasons for stenting included residual stenosis >30% in three patients and a perforation in two patients. In one patient, the TurboHawk catheter could not cross the target lesion. This patient was treated with PTA and a stent. A stent was also placed in one patient despite a residual diameter stenosis of <30% and no other qualifying condition.
The outflow vasculature was preserved in 98.3% (113/115) of patients with angiograms sufficient to assess run-off status to the ankle at baseline and post procedure. The angiographic core laboratory noted a filling defect in the remaining two patients; per site assessment, run-off was maintained in both of these patients.
Safety
The 30-day freedom from MAE rate was 93.1% (122/131). The 95% lower confidence limit was 88.3%, exceeding the performance goal of 85.5% and meeting the primary safety endpoint. There were nine MAEs in nine subjects (Table5) including one acute MI, one dissection (grade D), three distal embolizations, three perforations and one thrombosis. There were no amputations and no clinically driven target vessel revascularization. The dissection was treated with successful vessel stenting. Two of the three perforations were treated with covered stents, and the other with extended balloon inflation. There were no lesion characteristics or procedural techniques unique to the cases that led to perforations. The distal embolizations were all treated with catheter aspiration. In two cases, this was successful with removal of what was interpreted as thrombotic debris. The third patient had unsuccessful removal of debris and the clinical decision was made to observe the patient who remained asymptomatic from this event and had relief of clinical claudication. Overall, the filter device successfully prevented an embolic event in 97.5% (119/122) cases in which material was captured in the basket. The single target vessel thrombosis was treated with covered stent deployment and balloon inflation. The MI was deemed procedure, but not device-related by the CEC; no treatment was instituted during this hospitalization.
Table 5.
Summary of Major Adverse Events
| Major adverse event | % of Subjects (no. of events) |
|---|---|
| Total | 6.9% (9/131) [9] |
| Death | 0.0% (0/131) [0] |
| Acute myocardial infarction | 0.8% (1/131) [1] |
| Dissection, target vessel (C) | 0.0% (0/131) [0] |
| Dissection, target vessel (grade D or greater) | 0.8% (1/131) [1] |
| Vessel clinical perforation, target vessel | 2.3% (3/131) [3] |
| Pseudoaneurysm, target vessel | 0.0% (0/131) [0] |
| Thrombosis, target vessel | 0.8% (1/131) [1] |
| Distal embolism | 2.3% (3/131) [3] |
| Amputation, above metatarsal line | 0.0% (0/131) [0] |
| Clinically driven TVR | 0.0% (0/131) [0] |
Effectiveness
Primary effectiveness with directional atherectomy was achieved in 92.0% of patients as recorded by core laboratory evaluation, with a lower confidence bound of 87.6%. Site assessment placed this value at 97.0% (lower confidence bound 93.8%). Per core laboratory assessment, these results did not achieve the success criteria for the primary effectiveness objective, which was a comparison to the PG of 90.0%. However, when comparing the site-reported residual diameter stenosis data to the performance goal, the performance goal was exceeded.
Clinical Outcomes and Secondary Endpoints
RCC improved in 88.5% of patients at 30 days, and 10.8% were stable. One patient (0.8%) was worse at the 30-day follow-up and underwent revascularization a month later. At 30 days 2% of patients still had rest pain (decreased from 16% preprocedure), and 6% had severe claudication (decreased from 53%). Over half (52.3%) of patients were asymptomatic at 30 days.
Technical procedural success was achieved in 88.6% (117/132) of subjects. The 15 failures included one failure to achieve ≤50% residual diameter stenosis (stenosis = 50.34%), nine procedure-related MAEs, one device malfunction that caused the procedure to be aborted, and four instances of an inability to initially place the SpiderFX device successfully; a second filter was successfully deployed in all cases.
The additional step of predilatation did not result in safety concerns. Of the nine subjects experiencing an MAE, one had a predilated lesion for an MAE rate with predilation of 2.9% (1/34) vs. 8.1% (8/99) without.
DISCUSSION
Successful endovascular interventional therapies are hampered in the presence of calcific disease 17. Stent apposition and expansion is less complete and drug deposition in the vessel wall with the use of drug-eluting stents or drug-coated balloons is suspected to be reduced.
A single-center, prospective study was recently published on the use of the SilverHawk device to treat calcified femoropopliteal lesions 18. In 88% of cases, <30% residual diameter stenosis was achieved with SilverHawk alone; in every case, this was achieved with the use of adjunctive therapy including four stents (10.5%). The primary patency rate was reasonable at 69% at 1 year. Cioppa et al. combined treatment of the TurboHawk device with a SpiderFX filter placed distally and paclitaxel-coated balloons (PCB) to treat heavily calcified femoropopliteal lesions that resulted in freedom from target lesion revascularization of 90% at 1 year 19 in 30 patients with severe calcification. In addition to the high patency rate observed at 1 year, there were no embolizations or perforations, an encouraging outcome in a difficult patient population. A similar randomized trial, DEFINITIVE AR, recently completed enrolling patients who were randomized to treatment with PCB alone or TurboHawk followed by PCB.
The value of using of embolic protection with atherectomy is controversial and varies by lesion characteristics and disease severity (i.e., CLI or single vessel run-off). The presence of embolization has been shown across all endovascular modalities (PTA, stent, laser and atherectomy) using embolic filters 15,20 or by continuous monitoring of the downstream artery with duplex ultrasound 21. Furthermore, calcification was shown to increase the risk of clinically significant embolism 13. Consistent with these previous reports, debris was present in 88.4% of deployed SpiderFX filters upon recovery and preservation of run-off was verified by the angiographic core laboratory in 98.3% of subjects with available data. There were three embolic events (2.3%), none of which resulted in clinical sequelae. This embolization rate is comparable to stenting and PTA 22, in spite of the challenging calcified lesion population.
In this study, consistent with the instructions for use, operators were instructed to place the filter at least 2 cm distal to the point at which the tip of the atherectomy catheter would reach to ensure the tip of the catheter didn't pull the mouth of the filter away from the vessel wall. Such an occurrence would have compromised wall apposition. If space allows, the ideal filter position is in the popliteal artery just proximal to the anterior tibial take-off. The filter comes in three sizes appropriate for peripheral popliteal and SFA use: 5, 6, and 7 mm. The filter size was selected such that it was slightly larger than the vessel diameter. For example, a size 7 mm was used for a vessel 4.5–6 mm in diameter.
In this study, an independent core laboratory applied unbiased assessment to residual diameter stenosis; however, the primary effectiveness performance goal was based on site-reported residual diameter stenosis from the TALON Registry 4. Site-reported data typically report worse pre-treatment diameter stenosis and better post-treatment diameter stenosis. The differences between site-assessed stenosis data and core laboratory-assessed stenosis data seen in this study are consistent in direction and magnitude with other studies 23,24. The mean residual diameter stenosis following SilverHawk/TurboHawk atherectomy was 25.8% as reported by the sites and 33.3% by core laboratory assessment, a difference of 7.5%. The randomized FemPac study 23, which assessed PCBs in the femoropopliteal artery, showed similar site vs. core laboratory differences of 14.6% in the control group and 9.1% in the PCB group. It is not known why these differences exist, nor was this study designed to explore the accuracy of site-reported data.
These differences suggest that it is more germane to compare data from the same source (either the core laboratory or sites). The TALON registry did not have a core laboratory to assess angiographic data; therefore site-reported data was used to establish the 90% performance goal. When site-reported data are used for this endpoint analysis, the primary endpoint success criterion (≤50% residual diameter stenosis) was achieved in 97.0% (162/167) of lesions. The lower bound of the confidence interval is 93.8%, above the 90% performance goal that was derived from site-reported data.
In this study, bail out stenting was 4.1% despite the presence of moderately or severely calcific lesions. Moderate calcification is a strong predictor of bail out stenting 25. Recent data suggest that directional atherectomy improves vessel compliance and reduces dissection and bail out stenting 9. It should be noted, however, that shorter lesions length and the small number of total occlusions may have also accounted for the reduced need for stenting.
Limitations of this study include a lack of a control arm and long-term follow-up. This study was designed to study a specific cohort of patients; the selection criteria should be considered with generalizing the data. Additionally, the location of the filter was not assessed by the core lab, so the exact location cannot be reported. Because the target lesion location was limited to the femoropopliteal artery, it is likely that most filters were placed above the anterior-tibial artery take-off in order to protect all distal arteries.
CONCLUSION
Endovascular atherectomy with distal protection should be considered as a treatment option for complex calcified disease in the lower extremities. Significant improvement in clinical status was achieved in over 90% of patients and protection of distal vasculature was achieved in over 98% of patients utilizing the combination of these devices with the SpiderFX distal embolic protection system even in the setting of complex lesions.
Acknowledgments
The authors thank Sue Kim, DPM for data collection, Scott Brown, PhD for statistical analysis, and Meghan Schadow, MS for assistance in preparing the manuscript.
REFERENCES
- 1.Kandzari DE, Kiesz RS, Allie D, Walker C, Fail P, Ramaiah VG, et al. Procedural and clinical outcomes with catheter-based plaque excision in critical limb ischemia. J Endovasc Ther. 2006;13:12–22. doi: 10.1583/05-1634.1. [DOI] [PubMed] [Google Scholar]
- 2.Keeling WB, Shames ML, Stone PA, Armstrong PA, Johnson BL, Back MR, et al. Plaque excision with the Silverhawk catheter: early results in patients with claudication or critical limb ischemia. J Vasc Surg. 2007;45:25–31. doi: 10.1016/j.jvs.2006.08.080. [DOI] [PubMed] [Google Scholar]
- 3.McKinsey JF, Goldstein L, Khan HU, Graham A, Rezeyat C, Morrissey NJ, et al. Novel treatment of patients with lower extremity ischemia: Use of percutaneous atherectomy in 579 lesions. Ann Surg. 2008;248:519–528. doi: 10.1097/SLA.0b013e318188e1de. [DOI] [PubMed] [Google Scholar]
- 4.Ramaiah V, Gammon R, Kiesz S, Cardenas J, Runyon JP, Fail P, et al. Midterm outcomes from the TALON Registry: Treating peripherals with SilverHawk: Outcomes collection. J Endovasc Ther. 2006;13:592–602. doi: 10.1583/05-1780MR.1. [DOI] [PubMed] [Google Scholar]
- 5.Yancey AE, Minion DJ, Rodriguez C, Patterson DE, Endean ED. Peripheral atherectomy in TransAtlantic InterSociety Consensus type C femoropopliteal lesions for limb salvage. J Vasc Surg. 2006;44:503–509. doi: 10.1016/j.jvs.2006.05.038. [DOI] [PubMed] [Google Scholar]
- 6.Zeller T, Rastan A, Schwarzwalder U, Frank U, Burgelin K, Amantea P, et al. Percutaneous peripheral atherectomy of femoropopliteal stenoses using a new-generation device: Six-month results from a single-center experience. J Endovasc Ther. 2004;11:676–685. doi: 10.1583/04-1316R.1. [DOI] [PubMed] [Google Scholar]
- 7.Zeller T, Rastan A, Sixt S, Schwarzwalder U, Schwarz T, Frank U, et al. Long-term results after directional atherectomy of femoro-popliteal lesions. J Am Coll Cardiol. 2006;48:1573–1578. doi: 10.1016/j.jacc.2006.07.031. [DOI] [PubMed] [Google Scholar]
- 8.Zeller T, Sixt S, Schwarzwalder U, Schwarz T, Frank U, Burgelin K, et al. Two-year results after directional atherectomy of infrapopliteal arteries with the SilverHawk device. J Endovasc Ther. 2007;14:232–240. doi: 10.1177/152660280701400216. [DOI] [PubMed] [Google Scholar]
- 9.Shammas NW, Coiner D, Shammas GA, Dippel EJ, Christensen L, Jerin M. Percutaneous lower-extremity arterial interventions with primary balloon angioplasty versus Silverhawk atherectomy and adjunctive balloon angioplasty: Randomized trial. J Vasc Interv Radiol. 2011;22:1223–1228. doi: 10.1016/j.jvir.2011.05.013. [DOI] [PubMed] [Google Scholar]
- 10.Adam DJ, Bradbury AW. TASC II document on the management of peripheral arterial disease. Eur J Vasc Endovasc Surg. 2007;33:1–2. doi: 10.1016/j.ejvs.2006.11.008. [DOI] [PubMed] [Google Scholar]
- 11.Bishop PD, Feiten LE, Ouriel K, Nassoiy SP, Pavkov ML, Clair DG, et al. Arterial calcification increases in distal arteries in patients with peripheral arterial disease. Ann Vasc Surg. 2008;22:799–805. doi: 10.1016/j.avsg.2008.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shammas NW, Lam R, Mustapha J, Ellichman J, Aggarwala G, Rivera E, et al. Comparison of orbital atherectomy plus balloon angioplasty vs. balloon angioplasty alone in patients with critical limb ischemia: Results of the CALCIUM 360 randomized pilot trial. J Endovasc Ther. 2012;19:480–488. doi: 10.1583/JEVT-12-3815MR.1. [DOI] [PubMed] [Google Scholar]
- 13.Davies MG, Bismuth J, Saad WE, Naoum JJ, Mohiuddin IT, Peden EK, et al. Implications of in situ thrombosis and distal embolization during superficial femoral artery endoluminal intervention. Ann Vasc Surg. 2010;24:14–22. doi: 10.1016/j.avsg.2009.06.020. [DOI] [PubMed] [Google Scholar]
- 14.Shammas NW. Intraprocedural outcomes following distal lower extremity embolization in patients undergoing peripheral percutaneous interventions. Vasc Dis Manage. 2009;3 [Google Scholar]
- 15.Shammas NW, Dippel EJ, Coiner D, Shammas GA, Jerin M, Kumar A. Preventing lower extremity distal embolization using embolic filter protection: Results of the PROTECT registry. J Endovasc Ther. 2008;15:270–276. doi: 10.1583/08-2397.1. [DOI] [PubMed] [Google Scholar]
- 16.Suri R, Wholey MH, Postoak D, Hagino RT, Toursarkissian B. Distal embolic protection during femoropopliteal atherectomy. Catheter Cardiovasc Interv. 2006;67:417–422. doi: 10.1002/ccd.20634. [DOI] [PubMed] [Google Scholar]
- 17.Spaargaren GJ, Lee MJ, Reekers JA, van Overhagen H, Schultze Kool LJ, Hoogeveen YL. Evaluation of a new balloon catheter for difficult calcified lesions in infrainguinal arterial disease: Outcome of a multicenter registry. Cardiovasc Intervent Radiol. 2009;32:132–135. doi: 10.1007/s00270-008-9398-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Minko P, Katoh M, Jaeger S, Buecker A. Atherectomy of heavily calcified femoropopliteal stenotic lesions. J Vasc Interv Radiol. 2011;22:995–1000. doi: 10.1016/j.jvir.2011.03.017. [DOI] [PubMed] [Google Scholar]
- 19.Cioppa A, Stabile E, Popusoi G, Salemme L, Cota L, Pucciarelli A, et al. Combined treatment of heavy calcified femoro-popliteal lesions using directional atherectomy and a paclitaxel coated balloon: One-year single centre clinical results. Cardiovasc Revascular Med. 2012 doi: 10.1016/j.carrev.2012.04.007. [DOI] [PubMed] [Google Scholar]
- 20.Shammas NW, Coiner D, Shammas GA, Christensen L, Dippel EJ, Jerin M. Distal embolic event protection using excimer laser ablation in peripheral vascular interventions: Results of the DEEP EMBOLI registry. J Endovasc Ther. 2009;16:197–202. doi: 10.1583/08-2642.1. [DOI] [PubMed] [Google Scholar]
- 21.Lam RC, Shah S, Faries PL, McKinsey JF, Kent KC, Morrissey NJ. Incidence and clinical significance of distal embolization during percutaneous interventions involving the superficial femoral artery. J Vasc Surg. 2007;46:1155–1159. doi: 10.1016/j.jvs.2007.07.058. [DOI] [PubMed] [Google Scholar]
- 22.Schillinger M, Sabeti S, Loewe C, Dick P, Amighi J, Mlekusch W, et al. Balloon angioplasty versus implantation of nitinol stents in the superficial femoral artery. N Engl J Med. 2006;354:1879–1888. doi: 10.1056/NEJMoa051303. [DOI] [PubMed] [Google Scholar]
- 23.Werk M, Langner S, Reinkensmeier B, Boettcher HF, Tepe G, Dietz U, et al. Inhibition of restenosis in femoropopliteal arteries: Paclitaxel-coated versus uncoated balloon: Femoral paclitaxel randomized pilot trial. Circulation. 2008;118:1358–1365. doi: 10.1161/CIRCULATIONAHA.107.735985. [DOI] [PubMed] [Google Scholar]
- 24.Popma JJ, Lansky AJ, Yeh W, Kennard ED, Keller MB, Merritt AJ, et al. Reliability of the quantitative angiographic measurements in the new approaches to coronary intervention (NACI) registry: A comparison of clinical site and repeated angiographic core laboratory readings. Am J Cardiol. 1997;80:19K–25K. doi: 10.1016/s0002-9149(97)00761-3. [DOI] [PubMed] [Google Scholar]
- 25.Shammas NW, Coiner D, Shammas G, Jerin M. Predictors of provisional stenting in patients undergoing lower extremity arterial interventions. Int J Angiol. 2011;20:95–100. doi: 10.1055/s-0031-1279683. [DOI] [PMC free article] [PubMed] [Google Scholar]


