Abstract
Background
Colorectal cancer (CRC) screening rates are increasing, but they are still low, particularly in ethnic minority groups. In many resource-poor settings, fecal occult blood test (FOBT) is the main screening option.
Intervention
Culturally tailored telephone counseling by community health advisors employed by a community-based organization, culturally tailored brochures, and customized FOBT kits.
Design
RCT. Participants were randomized to (1) basic intervention: culturally tailored brochure plus FOBT kit (n=765); (2) enhanced intervention: brochure, FOBT plus telephone counseling (n=768); or (3) usual care (n=256).
Setting/participants
Latino and Vietnamese primary care patients at a large public hospital.
Main outcome measures
Self-reported receipt of FOBT or any CRC screening at 1-year follow-up.
Results
1358 individuals (718 Latinos and 640 Vietnamese) completed the follow-up survey. Self-reported FOBT screening rates increased by 7.8 % in the control group, by 15.1 % in the brochure group, and by 25.1 % in the brochure/telephone counseling group (p<0.01 for differences between each intervention and usual care and for the difference between brochure/telephone counseling and brochure alone). For any CRC screening, rates increased by 4.1 % in the usual care group, by 11.9 % in the FOBT/brochure group, and by 21.4 % in the brochure/telephone counseling group (p<0.01 for differences between each intervention and usual care and for the difference between the basic and the enhanced intervention).
Conclusions
An intervention that included culturally tailored brochures and tailored telephone counseling increased CRC screening in Latinos and the Vietnamese. Brochure and telephone counseling together had the greatest impact. Future research should address replication and dissemination of this model for Latinos and Vietnamese in other communities, and adaptation of the model for other groups.
Background
Colorectal cancer (CRC) is the second-leading cause of cancer mortality in the U.S. Among Latinos, CRC is the second-leading cause of cancer death in men and the third-leading cause of cancer death in women.1 CRC is the third most common cancer in Vietnamese Americans in the U.S.2 CRC screening is recommended for all individuals aged ≥50 years. There are many and increasing screening options.3–5 Although leading organizations differ in their recommendations, there is general agreement that CRC screening should include fecal occult blood testing, sigmoidoscopy, or colonoscopy. However, colonoscopy (and even sigmoidoscopy) may not be readily available, especially in resource-poor settings.
Although rates of CRC screening are increasing, they are still low and tend to be lowest among ethnic minority groups, including Latinos and Vietnamese, compared with non-Latino whites.6,7 Data from the 2007 California Health Interview Survey show that 33 % of Vietnamese adults and 39 % of Latino adults aged ≥50 years had never had any CRC screening test. This compares with 28 % and 25 % for African-American and Anglo adults, respectively.8 Latinos and Vietnamese are two rapidly growing ethnic groups in the U.S., with Latinos currently comprising 12.5 % of the U.S. population, and projected to become the nation’s largest ethnic/racial population by 2010.4 Vietnamese Americans are one of the fastest-growing Asian/Pacific ethnic groups.9 Thus, development of interventions that efficiently reach these subgroups with effective screening promotion strategies represents an important public health challenge.
Made possible by the diversity of the San Francisco Bay Area and an ethnically diverse research team, our study was designed to ascertain whether two culturally distinct ethnic subgroups could be reached through a common intervention delivered through a single partnering community-based organization for the purpose of raising rates of colorectal screening. The benefits of this approach are multiple. First, U.S. communities are increasingly diverse in the sense that multiple ethnic and language groups reside in the same or nearby neighborhoods, go to the same schools, and use the same clinics. For interventions targeting disparities, the greatest external validity might be achieved from strategies that are broad enough to target multiple culturally varied groups and at the same time retain an ability to tailor by culture.10 Second, the demonstration of effectiveness in two such diverse groups would signal considerable potential for applicability even more broadly. Third, limited English speakers have consistently shown the highest rates of late stage for detection of cancers amenable to routine screening.11,12 To demonstrate that a single intervention can be effective in more than one of these high-risk groups would have clear public health significance.
Interventions to increase rates of CRC screening have targeted both physicians and patients with strategies such as reminders,13–15 provision of fecal occult blood test (FOBT) cards,13,16 provision of patient education material,16,17 and academic detailing to physicians.18 To date, the most effective interventions have generated modest (6 %–12 %) increases in uptake of CRC screening,17,19,20 and others16,21 have shown no effect.
Our CRC promotion intervention had four features designed to achieve maximum effect. The first is cultural tailoring, that is, the development of interventions, strategies, messages, and materials to conform to specific cultural characteristics.22,23 In our intervention, this included language adaptation of all messages and materials, the development of unique brochures with images and messages found to be appealing and acceptable to each ethnic group, and perhaps most importantly, the use of ethnically concordant telephone counselors who possessed an innate understanding of the social context (the sociocultural forces that shape people’s day-to-day experiences and that directly and indirectly affect health and behavior) of our target audiences.24 Culturally tailored messages have been used in successful cancer screening programs targeting diverse ethnic groups,25–31 demonstrating a positive impact on cancer screening rates.
Second, the CRC screening messages were tailored by adoption stage according to the transtheoretical model of behavior change (TTM) which assesses an individual’s readiness to engage in a behavior.32,33 Rakowski adapted the TTM to successfully increase use of mammography.34 Third, in order to deliver tailored messages in a personal but still efficient manner, the choice was made to use telephone counseling by a team of Latino and Vietnamese lay health advisors. Telephone counseling can reach those who rarely access medical care, and it has been used to address several cancer disparities in clinic and community settings.35–38 Fourth, the telephone counseling intervention was located in and operated by a partnering community-based organization (CBO), Catholic Charities, located in San Jose CA, which helped enhance the credibility of the program as well as build the capacity of this trusted entity to promote the health of community members.
In this context, this study addressed the following question: Can an intervention that includes culturally tailored brochures with or without tailored telephone counseling increase rates of CRC screening among Latinos and Vietnamese seen in primary care clinics? To our knowledge, no prior studies have assessed the effect of a culturally and individually tailored intervention to increase CRC screening in diverse underserved populations.
Methods
Intervention
The intervention consisted of three components: telephone counseling, culturally tailored brochures, and a customized FOBT kit. Telephone counseling was delivered according to a protocol and scripts modeled on the Pathfinders study to increase breast and cervical cancer screening rates in five ethnic groups.39 Three Latino and five Vietnamese community health advisors (CHAs) were recruited by our CBO partner and trained for >20 hours using didactic course work, role-plays, and practice counseling sessions with study investigators as well as on-site visits to participating clinics and a gastroenterology suite. CHAs delivered messages specific to each individual’s adoption stage and perceived barriers to screening. Scripts for barriers were based on our study7 of barriers to CRC screening in Latinos and Vietnamese. There were separate scripts for each adoption phase as well as for each barrier. Thus individual participants were provided personalized information based on their defined stage of change as well as their defined barriers to cancer screening. To ensure quality control, study investigators met frequently with the CHAs, and they regularly reviewed the CHAs’ records.
Bilingual culturally tailored brochures were developed separately in Spanish and Vietnamese languages. Initial messages were crafted using results from our prior survey7 of barriers to CRC screening in Latinos, Vietnamese, and whites. Focus groups were conducted at various developmental phases to refine message content and to ascertain appropriate brochure design formats. The brochures addressed the need for CRC screening, a description of the tests, and commonly asked questions about CRC screening. Examples of barriers addressed included embarrassment, concern about the stool collection being dirty or messy, the need for testing if one feels healthy or eats a healthy diet and concern about the cost of the test. The brochures included pictures of physicians and community members and all included an English translation. Some of the tailoring components included brochure size and color, types of pictures were included and where they were placed, and where the English translation was placed in the brochure.
The ColoScreen® FOBT kit contained three cards for collecting stool, three wooden applicator sticks, a stamped return envelope, a lab slip, and a letter from the individual’s primary care physician emphasizing the importance of CRC screening. Also included were simplified written instructions in English and Spanish or Vietnamese for collecting the stool and information on dietary restrictions particular to the Latino and Vietnamese cultures.
Setting
Santa Clara Valley Medical Center (SCVMC) is a public hospital owned and operated by the county of Santa Clara. SCVMC operates a network of community-based clinics that provide primary care to residents of Santa Clara County, many of whom are Latino or Vietnamese. There is limited endoscopy capacity at SCVMC and so the primary CRC screening option is the FOBT. Screening colonoscopy is not routinely available and is reserved for those who have a family history of CRC; otherwise diagnostic colonoscopy is used in patients who have a positive FOBT or CRC symptoms.
Participants
Participants were Vietnamese and Latino male and female patients at one of the five SCVMC primary care satellite sites. Primary care physician panel lists were generated via an electronic medical record and included patient name, age, and ethnicity. At SCVMC, some parts of the medical record are on paper and some are electronic, so identifying in advance only those patients due for CRC screening was not possible.
All primary care physicians seeing patients at the medical center were invited to participate and asked for permission to contact their eligible Vietnamese or Latino patients aged 50 –79 years with no history of cancer. Exclusion criteria included dementia or any condition (e.g., terminal illness) for which the primary care physician deemed the patient ineligible for CRC screening. After the physician gave permission, eligible patients received a mailed letter describing the study, enclosing a refusal postcard. Individuals who did not return the refusal postcard received a telephone call asking them to participate in a telephone survey and the intervention trial. Those who participated in the telephone interview received $15 cash after completion of both baseline and follow-up surveys.
Study Design
An RCT compared two variations of the intervention with usual care. Participants completed a baseline survey by phone and were then randomized to receive (1) usual care (controls), (2) mailed FOBT kit plus culturally tailored brochures, or (3) mailed FOBT kit plus culturally tailored brochures and tailored telephone counseling. Randomization was done using a computer-generated random number list, and a randomization scheme stratified by gender and ethnicity. A telephone follow-up survey was administered 9–12 months after baseline.
Baseline and Follow-Up Survey Instruments
The survey instrument was developed based on our prior survey7 of barriers to CRC screening in Vietnamese, Latinos, and whites. The survey was developed in English, translated into Spanish and Vietnamese, and then back-translated into English to ensure lexical equivalency; it was pilot tested and revised. This methodology ensured that the source language did not become the dominant language.22 The surveys were administered using computer-assisted telephone interviewing by trained bilingual telephone interviewers and conducted in Vietnamese, Spanish, or English, according to the participant’s choice. The follow-up survey, similar to the baseline survey although shorter, was administered 9 –12 months after the baseline survey. IRB approval was obtained from University of California, San Francisco, and SCVMC in May, 2005.
Survey items included demographics, acculturation, perceived health status, perceived risk of developing cancer, previous CRC screening behaviors, intention to be screened, beliefs, knowledge items, and perceived barriers and facilitators to CRC screening. Acculturation was measured using a five-item scale developed by Marin et al.40 and previously used and validated in the Latino population. These items included questions about language read and spoken at home, spoken with friends, used as a child, and language in which an individual thinks. The scale is graded such that a high value denotes high acculturation.
Provider factors were derived from available SCVMC physician data and included gender, ethnicity, and gender and language concordance with the patient.
Outcomes
Because the primary screening option available at SCVMC is FOBT, the main study outcomes were self-reported receipt of FOBT or any CRC screening (FOBT, sigmoidoscopy and/or colonoscopy) during the 1-year follow-up. All questions measuring CRC screening tests had been recommended for use as standardized self-report measures for CRC.41 Questions included whether or not respondents had ever completed a home stool blood test (FOBT); (2) recency of latest FOBT; (3) if they ever had a sigmoidoscopy or colonoscopy; and (4) recency of that endoscopy.
Sample Size
Sample size was calculated based on a test of differences between experimental groups on follow-up FOBT rates separately for Vietnamese and Latino participants. An effect size of 10 % was assumed to be clinically significant. For each ethnic group, each intervention group required 344 participants and the usual care group required 111 participants. Using a 90 % power and assuming 20 % attrition, it was calculated that 900 participants would be needed per ethnic group for a total of 1800 participants.
Analyses
The baseline survey was conducted in 2005–2006, the follow-up survey was conducted in 2006–2007, and the data analyses were completed during 2007–2009. Data were analyzed using SAS, version 1.3. The primary analyses were designed to examine the impact of the intervention on receipt of FOBT and on any CRC screening. Descriptive statistics were computed for all demographic and dependent variables, including means and SDs for continuous data and frequency distributions for each of the categoric variables. Descriptive statistics were also calculated for the telephone counseling variables.
For the univariate comparisons, t-tests were used for continuous variables and chi-square of independence for the categoric variables. The percentage of individuals up-to-date for screening at baseline and follow-up were measured as the percentage of individuals who had had the recommended screening test within the recommended time interval, specifically, the percentage of individuals who had had FOBT within the past year, sigmoidoscopy within the past 5 years, and colonoscopy within the past 10 years. The percentage of individuals up-to-date with any CRC screening was calculated as the percentage of individuals who had FOBT within the past year, sigmoidoscopy within the past 5 years, or colonoscopy within the past 10 years.
The difference between baseline and follow-up rates was calculated for each condition. To compare the differences in the change in screening rates between study groups, t-tests were used. The primary analysis assessed whether the difference with either Group-2 or Group-3 interventions was significantly greater than that with Group 1, the usual care (control) group. The secondary analysis evaluated whether the difference with the Group-3 intervention (FOBT kit plus brochure plus tailored telephone counseling) was significantly greater than that with the Group-2 intervention (FOBT kit plus brochure).
Multivariate analyses were performed to determine the independent impact of the interventions on rates of CRC screening and included both patient and provider factors. Patient factors included in the multivariate model were age, gender, marital status, education, employment, acculturation, self-rated health, perceived cancer risk, and cancer knowledge. Because all Vietnamese participants described a low acculturation level, acculturation was not included in the model for Vietnamese. Provider factors included gender, patient–physician gender, ethnicity, and language concordance. The estimates of these parameters of multivariate logistic regression models were computed in a stepwise manner by entering or removing variables, one variable at a time, from the list of potential predictors. The entry criterion of p=0.30 and the removal criteria of p=0.35 was set for entering and removing variables in the stepwise models. All predictors were presented in the final parsimonious model; variables showing a significant effect (p<0.05) are marked with an asterisk.
Results
Provider Characteristics
Of 49 SCVMC physicians asked to participate, 44 agreed (90 %). Among participating physicians, 23 (56 %) were women; half (51 %) were Caucasian; 10 % were Latino; 17 % were Vietnamese; and the remainder, of other ethnicities. About half (51 %) of participating physicians spoke Spanish. All of the Vietnamese physicians spoke Vietnamese. On average, physicians were in clinical practice about 6.5 half-day sessions per week and 42 (95 %) were U.S. graduates.
Participant Characteristics
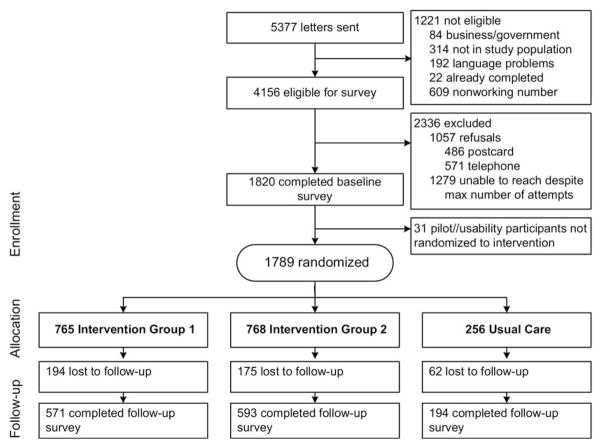
The participant flow diagram is shown in Figure 1. Letters were mailed to 5377 potential participants. After excluding those who were not eligible or for whom phone numbers were incorrect, 4156 were eligible for the survey. Call attempts were made to a total of 3670 eligible individuals who did not return refusal postcards. A total of 1789 individuals completed the baseline survey for a response rate of 51 %. Because 1279 individuals could not be reached by phone, the percentage of those reached who actually responded was 62 %. A total of 1358 individuals completed the follow-up survey for a retention rate of 76 %. Four percent of baseline survey participants refused the follow-up survey, 11 % were not available, and 10 % of total respondents were not found either because of a wrong number, phone number disconnected, or being deceased.
Figure 1.
Participant flow diagram
Participant characteristics (Table 1)
Table 1.
Characteristics of study participants who were primary care patients and completed the baseline survey
| Characteristics | Study arm | p-valuea | ||
|---|---|---|---|---|
| Group 1: usual care | Group 2: FOBT plus brochure | Group 3: FOBT plus brochure plus counseling | ||
| ALL PARTICIPANTS (N=1789) | ||||
| Sociodemographics | 0.59 | |||
| Age (years; M [SD]) | 60.37 (6.5) | 60.63 (6.7) | 60.73 (6.8) | |
| Gender | 0.96 | |||
| Male | 79 (30.9) | 237 (31.0) | 233 (30.3) | |
| Female | 177 (69.1) | 528 (69.0) | 535 (69.7) | |
| Marital status | 0.35 | |||
| Married or living with partner | 144 (56.3) | 452 (59.01) | 470 (61.2) | |
| Other | 112 (43.8) | 313 (40.9) | 298 (38.8) | |
| Country of birth | 0.80 | |||
| Mexico | 89 (34.9) | 284 (37.4) | 284 (37.2) | |
| U.S. | 32 (12.6) | 82 (10.8) | 89 (11.7) | |
| Vietnam | 113 (44.3) | 337 (44.3) | 337 (44.1) | |
| Other | 21 (8.2) | 57 (7.5) | 54 (7.1) | |
| Years in U.S. (M [SD]) | 19.17 (10.9) | 19.2 (10.9) | 19.0 (11.1) | 0.87 |
| Employment status | 0.13 | |||
| Employed | 62 (24.2) | 168 (22.0) | 157 (20.4) | |
| Unemployed | 77 (30.1) | 238 (21.1) | 245 (31.9) | |
| Homemaker | 79 (30.89) | 216 (28.2) | 229 (29.8) | |
| Retired | 38 (14.8) | 143 (18.7) | 137 (17.8) | |
| Annual household income ($) | 0.14 | |||
| <20,000 | 140 (54.7) | 443 (57.9) | 451 (58.7) | |
| >20,000 | 40 (15.6) | 81 (10.6) | 75 (9.8) | |
| Did not respond | 76 (29.7) | 241 (31.5) | 242 (31.5) | |
| Education (years) | 0.50 | |||
| ≤6 | 136 (53.1) | 433 (56.6) | 430 (56.0) | |
| 7–12 | 59 (23.1) | 186 (24.3) | 191 (24.9) | |
| ≥13 | 61 (23.8) | 146 (19.1) | 147(19.1) | |
| Language of interview | 0.83 | |||
| English | 29 (11.3) | 68 (8.9) | 76 (9.9) | |
| Spanish | 114 (44.5) | 358 (46.8) | 351 (45.7) | |
| Vietnamese | 113 (44.1) | 339 (44.3) | 341 (44.4) | |
| Acculturation scoreb | 0.32 | |||
| High (>3.0) | 34 (13.3) | 76 (9.9) | 81 (10.56) | |
| Low (<3.0) | 222 (86.7) | 689 (90.1) | 687 (89.5) | |
| Self-rated health | 0.87 | |||
| Excellent/very good | 11 (4.4) | 31 (4.2) | 42 (5.6) | |
| Good | 45 (18.1) | 148 (19.9) | 137 (18.4) | |
| Fair | 137 (55.0) | 399 (53.7) | 402 (53.9) | |
| Poor | 56 (22.5) | 165 (22.2) | 165 (22.1) | |
| Perceived risk of developing colon cancer | 0.39 | |||
| More likely than others | 27 (10.6) | 95 (12.4) | 108 (14.1) | |
| About the same as others | 179 (69.9) | 530 (69.3) | 502 (65.4) | |
| Less likely than others | 50 (19.5) | 140 (18.3) | 158 (20.6) | |
| LATINOS (n=993) | ||||
| Sociodemographics | 0.38 | |||
| Age (years; M [SD]) | 59 (6.8) | 60 (7.4) | 60 (7.6) | |
| Gender | 0.99 | |||
| Male | 39 (27.3) | 114 (26.8) | 115 (26.9) | |
| Female | 104 (72.7) | 312 (73.2) | 312 (73.1) | |
| Marital status | 0.23 | |||
| Married or living with partner | 66 (46.2) | 192 (45.1) | 217 (50.8) | |
| Other | 77 (53.9) | 234 (54.9) | 210 (49.2) | |
| Country of birth | 0.81 | |||
| Mexico | 32 (22.5) | 82 (19.4) | 89 (21.0) | |
| U.S. | 89 (62.7) | 284 (67.3) | 284 (67.0) | |
| Vietnam | — | — | — | |
| Other | 21 (14.8) | 56 (13.3) | 51 (12.0) | |
| Years in U.S. (M [SD]) | 23.33 (12.8) | 23.01 (12.7) | 22.92 (13.2) | 0.17 |
| Employment status | 0.53 | |||
| Employed | 32 (22.4) | 101 (23.7) | 92 (21.6) | |
| Unemployed | 40 (28.0) | 118 (27.7) | 114 (26.7) | |
| Homemaker | 49 (34.3) | 121 (28.4) | 138 (32.3) | |
| Retired | 22 (15.4) | 86 (20.2) | 83 (19.4) | |
| Annual household income ($) | 0.22 | |||
| <20,000 | 72 (50.4) | 239 (56.1) | 231 (54.1) | |
| >20,000 | 27 (18.9) | 55 (12.9) | 50 (11.7) | |
| Did not respond | 44 (30.8) | 132 (31.0) | 146 (34.2) | |
| Education (years) | 0.57 | |||
| ≤6 | 93 (65.0) | 307 (72.1) | 295 (69.1) | |
| 7–12 | 34 (23.8) | 85 (20.0) | 94 (22.0) | |
| ≥13 | 16 (11.2) | 34 (8.0) | 38 (8.9) | |
| Language of interview | 0.48 | |||
| English | 29 (20.3) | 68 (16.0) | 76 (17.8) | |
| Spanish | 114 (79.7) | 358 (84.0) | 351 (82.2) | |
| Acculturation scoreb | 0.39 | |||
| High (>3.0) | 33 (23.1) | 76 (17.8) | 81 (19.0) | |
| Low (<3.0) | 110 (76.9) | 350 (82.2) | 346 (81.0) | |
| Self-rated health | 0.39 | |||
| Excellent/very good | 9 (6.3) | 23 (5.4) | 38 (8.9) | |
| Good | 25 (17.6) | 93 (22.0) | 80 (18.8) | |
| Fair | 80 (56.3) | 232 (54.9) | 232 (54.6) | |
| Poor | 28 (19.7) | 75 (17.7) | 75 (17.7) | |
| Perceived risk of developing colon cancer | 0.73 | |||
| More likely than others | 20 (14.0) | 70 (16.4) | 80 (18.7) | |
| About the same as others | 95 (66.4) | 277 (65.0) | 266 (62.3) | |
| Less likely than others | 28 (19.6) | 79 (18.5) | 81 (19.0) | |
| VIETNAMESE (n=793) | ||||
| Sociodemographics | 0.48 | |||
| Age (years; M [SD]) | 61 (6.1) | 61 (5.7) | 61 (5.7) | |
| Gender | 0.90 | |||
| Male | 40 (35.4) | 123 (36.3) | 118 (34.6) | |
| Female | 73 (64.6) | 216 (63.7) | 223 (65.4) | |
| Marital status | 0.26 | |||
| Married or living with partner | 78 (69.0) | 260 (76.7) | 253 (74.2) | |
| Other | 35 (31.0) | 79 (23.3) | 88 (25.8) | |
| Country of birth | 0.40 | |||
| Vietnam | 113 (100.0) | 337 (99.7) | 337 (99.1) | |
| Other | 0 (0.0) | 1 (0.3) | 3 (0.7) | |
| Years in U.S. (M [SD]) | 15.05 (6.5) | 15.15 (6.4) | 15.25 (6.7) | 0.68 |
| Employment status | 0.27 | |||
| Employed | 30 (26.6) | 67 (19.8) | 65 (19.1) | |
| Unemployed | 37 (32.7) | 120 (35.4) | 131 (38.4) | |
| Homemaker | 30 (26.6) | 95 (28.0) | 91 (26.7) | |
| Retired | 16 (14.2) | 57 (16.8) | 54 (15.8) | |
| Annual household income ($) | 0.36 | |||
| <20,000 | 68 (60.2) | 204 (60.2) | 220 (64.5) | |
| >20,00 | 13 (11.5) | 26 (7.7) | 25 (7.3) | |
| Did not respond | 32 (28.3) | 109 (32.2) | 96 (28.2) | |
| Education (years) | 0.45 | |||
| ≤6 | 43 (38.1) | 126 (37.2) | 135 (39.6) | |
| 7–12 | 25 (22.1) | 101 (29.8) | 97 (28.5) | |
| ≥13 | 45 (39.8) | 112 (33.0) | 109 (32.0) | |
| Language of interview | N/A | |||
| English | ||||
| Vietnamese | 113 (100.0) | 339 (100.0) | 341 (100.0) | |
| Acculturation scoreb | 0.64 | |||
| High (>3.0) | 1 (0.9) | 0 (0.0) | 0 (0.0) | |
| Low (<3.0) | 112 (99.12) | 339 (100.00) | 341 (100) | |
| Self-rated health | 0.85 | |||
| Excellent/very good | 2 (1.9) | 8 (2.5) | 4 (1.3) | |
| Good | 20 (18.7) | 55 (17.2) | 57 (17.8) | |
| Fair | 57 (53.3) | 167 (52.2) | 170 (53.0) | |
| Poor | 28 (26.2) | 90 (28.1) | 90 (28.0) | |
| Perceived risk of developing colon cancer | 0.55 | |||
| More likely than others | 7 (6.2) | 25 (7.4) | 28 (8.2) | |
| About the same as others | 84 (74.3) | 253 (74.6) | 236 (69.2) | |
| Less likely than others | 22 (19.5) | 61 (18.0) | 77 (22.6) | |
Note: All participants: Group 1, n=256; Group 2, n=765; Group 3, n=768. Latinos: Group 1, n=143; Group 2, n=426; Group 3, n=427. Vietnamese: Group 1, n=113; Group 2, n=339; Group 3, n=341.
Differences between the groups calculated by χ2 or t-tests
Acculturation score was measured by a previously validated five-item scale.38 Low acculturation was defined as ≤2.99 and high acculturation was defined as ≥3.0. Scale items include language(s) read and speak, spoken at home, spoken with friends, language(s) used as a child (up to age 12 years), and language(s) in which a person thinks.
FOBT, fecal occult blood test
Participants’ mean age was 61 years; the majority of both ethnicities were female and married or living with a partner. The majority of Latinos was born outside of the U.S. and completed the interview in Spanish; all of the Vietnamese were foreign-born and virtually all completed the interview in Vietnamese. The majority of both groups had less than a 12th-grade education and measured low on the acculturation scale. Most rated their health as fair to poor. Few perceived themselves to be at high risk for CRC. There were no significant differences among the three study arms.
Baseline cancer screening behavior (Table 2)
Table 2.
Baseline CRC screening behavior of 1789 Latino and Vietnamese primary care patients
| Screening status | Study arm | p-valuea | ||
|---|---|---|---|---|
| Group 1: usual care | Group 2: FOBT plus brochure | Group 3: FOBT plus brochure plus counseling | ||
| ALL PARTICIPANTS (N=1789) | ||||
| Ever heard of screening | ||||
| Heard of colon cancer | 213 (83.2) | 644 (84.2) | 632 (82.3) | 0.43 |
| Heard of polyp | 79 (30.7) | 281 (36.7) | 296 (38.5) | 0.09 |
| Heard of FOBT | 170 (66.4) | 498 (65.1) | 465 (60.6) | 0.09 |
| Heard of SIG | 129 (50.4) | 343 (44.8) | 343 (44.7) | 0.10 |
| Heard of COL | 106 (41.4) | 323 (42.2) | 327 (42.6) | 0.82 |
| Heard of SIG/COL | 147 (57.4) | 421 (55.0) | 408 (53.1) | 0.23 |
| Ever had CRC screening | ||||
| Ever FOBT | 178 (69.5) | 544 (71.1) | 529 (68.9) | 0.63 |
| Ever SIG | 56 (21.9) | 174 (22.8) | 148 (19.3) | 0.37 |
| Ever COL | 53 (20.7) | 185 (24.2) | 178 (23.2) | 0.25 |
| Ever SIG or COL | 93 (36.3) | 303 (39.6) | 281 (36.6) | 0.36 |
| Up-to-date with CRC screening | ||||
| FOBT in past year | 110 (43.0) | 348 (45.5) | 338 (44.0) | 0.58 |
| SIG in past 5 years/COL in past 10 years | 77 (30.1) | 253 (33.1) | 246 (32.0) | 0.37 |
| Any CRC screening | 152 (59.4) | 483 (63.1) | 458 (59.6) | 0.25 |
| LATINOS (n=996) | ||||
| Ever heard of screening | ||||
| Heard of colon cancer | 113 (79.0) | 341 (80.1) | 330 (77.3) | 0.62 |
| Heard of polyp | 41 (28.7) | 130 (30.5) | 131 (30.7) | 0.37 |
| Heard of FOBT | 78 (54.5) | 218 (51.2) | 189 (44.3) | 0.04 |
| Heard of SIG | 59 (41.3) | 156 (36.7) | 146 (34.2) | 0.13 |
| Heard of COL | 50 (35.0) | 157 (36.9) | 146 (34.2) | 0.52 |
| Heard of SIG/COL | 71 (49.7) | 208 (48.8) | 183 (42.9) | 0.14 |
| Ever had CRC screening | ||||
| Ever FOBT | 84 (58.7) | 257 (60.3) | 239 (56.0) | 0.68 |
| Ever SIG | 28 (19.6) | 82 (19.3) | 63 (14.8) | 0.26 |
| Ever COL | 28 (19.6) | 87 (20.4) | 67 (15.7) | 0.10 |
| Ever SIG or COL | 47 (32.9) | 139 (32.6) | 109 (25.5) | 0.15 |
| Up-to-date with CRC screening | ||||
| FOBT in past year | 57 (39.9) | 163 (38.3) | 156 (36.5) | 0.52 |
| SIG in past 5 years/COL in past 10 years | 36 (25.2) | 115 (27.0) | 94 (22.0) | 0.22 |
| Any CRC screening | 77(53.9) | 225 (52.8) | 205 (48.0) | 0.30 |
| VIETNAMESE (n=793) | ||||
| Ever heard of screening | ||||
| Heard of colon cancer | 100 (88.5) | 303 (89.4) | 302 (88.6) | 0.77 |
| Heard of polyp | 38 (33.6) | 151 (44.6) | 165 (48.4) | 0.03 |
| Heard of FOBT | 92 (81.4) | 280 (82.6) | 276 (80.9) | 0.92 |
| Heard of SIG | 70 (62.0) | 187 (55.2) | 197 (57.8) | 0.19 |
| Heard of COL | 56 (49.6) | 166 (49.0) | 181 (53.1) | 0.46 |
| Heard of SIG/COL | 76 (67.0) | 213 (62.8) | 225 (66.0) | 0.34 |
| Ever had CRC screening | ||||
| Ever FOBT | 94 (83.2) | 287 (84.7) | 290 (85.0) | 0.80 |
| Ever SIG | 28 (24.8) | 92 (27.1) | 85 (84.9) | 0.53 |
| Ever COL | 25 (22.1) | 98 (28.9) | 111 (32.6) | 0.15 |
| Ever SIG or COL | 46 (40.7) | 164 (48.4) | 172 (50.4) | 0.14 |
| Up-to-date with CRC screening | ||||
| FOBT in past year | 53 (47.0) | 185 (54.6) | 182 (53.4) | 0.20 |
| SIG in past 5 years/COL in past 10 years | 41 (36.3) | 138 (40.7) | 152 (44.6) | 0.35 |
| Any CRC screening | 75 (66.4) | 258 (76.1) | 253 (74.2) | 0.42 |
Note: All participants: Group 1, n=256; Group 2, n=765; Group 3, n=768. Latinos: Group 1, n=143; Group 2, n=426; Group 3, n=427. Vietnamese: Group 1, n=113; Group 2, n=339; Group 3, n=341.
Differences between the groups calculated by χ2 or t-tests
COL, colonoscopy; CRC, colorectal cancer; FOBT, fecal occult blood test; SIG, sigmoidoscopy
he majority of both ethnicities had heard of CRC, although fewer had heard of a polyp or the endoscopic screening tests. About two thirds had ever had CRC screening at baseline. There were no significant differences between intervention groups.
Impact of intervention on colorectal cancer screening (Table 3)
Table 3.
Colorectal cancer screening rates before and after the intervention in 1358 primary care clinic patients
| Screening status | Baseline (n [%]) | Follow-up (n [%]) | Change (%) | p-valuea | p-valueb |
|---|---|---|---|---|---|
| ALL PARTICIPANTS | |||||
| Up-to-date on FOBT | <0.001 | ||||
| 1: Usual care | 92 (47.4) | 107 (55.2) | 7.8 | — | |
| 2: FOBT + brochure | 257 (45.0) | 343 (60.1) | 15.1 | 0.010 | |
| 3: FOBT + brochure + counseling | 265 (44.7) | 414 (69.8) | 25.1 | <0.001 | |
| Up-to-date on any CRC screening | <0.001 | ||||
| 1: Usual care | 124 (63.9) | 132 (68.0) | 4.1 | — | |
| 2: FOBT + brochure | 369 (64.6) | 437 (76.5) | 11.9 | 0.002 | |
| 3: FOBT + brochure + counseling | 358 (60.4) | 485 (81.8) | 21.4 | <0.001 | |
| LATINOS | |||||
| Up-to-date on FOBT | 0.137 | ||||
| 1: Usual care | 49 (48.5) | 53 (52.5) | 4.0 | — | |
| 2: FOBT + brochure | 108 (35.6) | 168 (55.4) | 19.8 | <0.001 | |
| 3: FOBT + brochure + counseling | 117 (37.3) | 195 (62.1) | 24.8 | <0.001 | |
| Up-to-date on any CRC screening | 0.003 | ||||
| 1: Usual care | 62 (61.4) | 61 (60.4) | –1.0 | — | |
| 2: FOBT + brochure | 161 (53.1) | 206 (68.0) | 14.9 | <0.001 | |
| 3: FOBT + brochure + counseling | 153 (48.7) | 230 (73.2) | 24.5 | <0.001 | |
| VIETNAMESE | |||||
| Up-to-date on FOBT | <0.001 | ||||
| 1: Usual care | 43 (46.2) | 54 (58.1) | 11.9 | — | |
| 2: FOBT + brochure | 149 (55.6) | 175 (65.3) | 9.7 | 0.547 | |
| 3: FOBT + brochure + counseling | 148 (53.0) | 219 (78.5) | 25.5 | 0.006 | |
| Up-to-date on any CRC screening | 0.001 | ||||
| 1: Usual care | 62 (61.4) | 71 (76.3) | 14.9 | — | |
| 2: FOBT + brochure | 208 (77.6) | 231 (86.2) | 8.6 | 0.770 | |
| 3: FOBT + brochure + counseling | 205 (73.5) | 255 (91.4) | 17.9 | 0.058 |
Difference between usual care and interventions
Difference between two interventions
CRC, colorectal cancer; FOBT, fecal occult blood test
The changes in screening rates (follow-up rate versus baseline rate) are compared in Table 3. The Group-2 intervention (FOBT kit plus brochure) and Group-3 intervention (FOBT kit plus brochure plus telephone counseling) are each compared to the Group-1 intervention (usual care). In addition, Group 3 is then compared to Group 2. For the primary outcome (receipt of FOBT), screening rates increased 7.8 % in Group 1; 15.1 % in Group 2; and 25.1 % in Group 3. Group-2 and Group-3 pre–post differences were both significantly greater than that in Group 1. The difference in Group 3 was significantly greater than that in Group 2. Similar trends were seen for the secondary outcome of being up-to-date with any CRC screening.
A preplanned subgroup analysis was performed comparing the effects of the intervention separately in Latinos and Vietnamese. In Latinos, the pre–post differences for the primary outcome for Group 2 and Group 3 were both significantly greater than that for Group 1; however, the Group-3 difference was not significantly greater than that in Group 2. For any CRC screening, both interventions were significantly better than usual care and the Group-3 difference was significantly greater than that seen in Group 2.
In contrast, among Vietnamese, the pre–post difference for Group 2 was not significantly greater than Group 1, although the difference for Group 3 was significantly greater than that for Group 1 and Group 2. For the secondary outcome, the only significant difference was between Groups 2 and 3.
Multivariate analyses (Tables 4 and 5)
Table 4.
Multivariate predictors of being up-to-date with FOBT (OR [95 % CI])
| Predictors | All participants | Latino participants | Vietnamese participants |
|---|---|---|---|
| Married: yes vs no | 0.86 (0.67, 1.11) | 0.72 (0.52, 0.99) | 0.90 (0.59, 1.38) |
| Acculturation: high vs low | 0.44 (0.29, 0.66) | 0.53 (0.34, 0.84) | — |
| Provider factors | |||
| Ethnicity concordance: yes vs no | 0.90 (0.70, 1.13) | 0.79 (0.53, 1.16) | 0.85 (0.56, 1.24) |
| Language concordance: yes vs no | 0.71 (0.55, 0.91) | 0.71 (0.49, 1.03) | 1.16 (0.71, 1.87) |
| Intervention group | |||
| FOBT + brochure vs usual care | 1.18 (0.84, 1.66) | 1.08 (0.68, 1.73) | 1.33 (0.80, 2.20) |
| FOBT + brochure + counseling vs usual care | 1.89 (1.34, 2.66) | 1.44 (0.90, 2.30) | 3.02 (1.77, 5.14) |
Note: Boldface indicates significance.
FOBT, fecal occult blood test
Table 5.
Multivariate predictors of being up-to-date with any CRC screeninga (OR [95 % CI])
| Predictors | All participants | Latino participants | Vietnamese participants |
|---|---|---|---|
| Acculturation: high vs low | 0.37 (0.23, 0.57) | 0.57 (0.35, 0.92) | Not in model |
| CRC knowledge: high (>3.0) vs low (<3.0) | 1.51 (1.13, 2.01) | 1.34 (0.93, 1.92) | 1.58 (0.95, 2.65) |
| Provider factors | |||
| Ethnicity concordance: yes vs no | 0.85 (0.64, 1.14) | 0.66 (0.44, 0.99) | 0.55 (0.30, 1.02) |
| Language concordance: yes vs no | 0.74 (0.55, 0.99) | 0.88 (0.58, 1.32) | 1.68 (0.82, 3.43) |
| Intervention group | |||
| FOBT + brochure vs usual care | 1.51 (1.03, 2.19) | 1.36 (0.84, 2.21) | 1.99 (1.05, 3.76) |
| FOBT + brochure + counseling vs usual care | 2.01 (1.37, 2.95) | 1.76 (1.08, 2.87) | 3.20 (1.62, 6.33) |
Note: Boldface indicates significance. Factors included in the models but that were not significant included age, gender, marital status, level of education, employment, self-rated health, perceived risk of developing cancer, ever having heard of a polyp, provider gender, provider–patient gender concordance, and provider language concordance.
Any CRC screening included FOBT in the past year or sigmoidoscopy in the past 5 years or colonoscopy in the past 10 years.
CRC, colorectal cancer; FOBT, fecal occult blood test
Multivariate analyses were performed for the entire study cohort and also separately for Latinos and Vietnamese. For the primary outcome of FOBT in the past year, the effect of the Group-3 intervention was significant compared to the Group-1 intervention, but the effect of the Group-2 intervention was not significant when compared to that of Group 1. Similar results were seen when Latinos and Vietnamese were analyzed separately. For the outcome of any CRC screening, both Group-2 and Group-3 interventions had significant effects compared to Group 1; however, when Latinos and Vietnamese were analyzed separately, only the Group-3 intervention was significant.
Features of tele phone counseling
There were eight CHAs: three were Latino and five were Vietnamese. All of the Latino counselors were women and three of the Vietnamese counselors were women. A total of 758 participants were randomized to receive telephone counseling, and 593 participants (78 %) actually received telephone counseling. The average number of times a participant was contacted was 1.74 (SD=1.62), and the average duration of counseling was 17 (SD=11) minutes. Latino participants were counseled an average of 20 (SD=10) minutes and Vietnamese participants were counseled an average of 14 (SD=8) minutes.
Discussion
This study targeted promotion of colorectal screening to two low-income and ethnically diverse populations. This highly successful intervention resulted in a large increase in self-reported rates of FOBT screening among Latinos and Vietnamese. Overall, direct provision of an FOBT kit and a culturally tailored brochure plus individually and culturally tailored counseling—all provided in the patient’s language of choice: English, Spanish, or Vietnamese—resulted in a 25 % pre–post increase in self-reported screening. The basic intervention, which included the FOBT kit and brochure without the telephone counseling, was not sufficient to increase rates of self-reported CRC screening, but the addition of the tailored telephone counseling seemed to be the key feature that made a difference.
It is thus far rare for studies to feature both cultural and individual tailoring across two or more ethnic groups in the context of a single intervention. Pasick and colleagues’ randomized trial39 of 1463 African-American, white, Latina, Filipina, and Chinese women used culturally and individually tailored print as well as telephone counseling in four languages, resulting in significant pre–post increases of 16 % for Pap (p=0.001) and 10 % for mammography (p=0.05).
Surprisingly, individuals who were less acculturated were more likely to be up-to-date at follow-up. In another study,42 low acculturation was associated with less endoscopic screening but it was not associated with FOBT screening. It is possible that those who are less acculturated are less likely to question their physicians and to have testing if it is recommended.
Few CRC screening interventions have targeted a disadvantaged group or those of diverse ethnicity or levels of acculturation. In a recent randomized trial in a community health center serving a low-income and ethnically diverse (predominantly Latino, African-American, and white) population where colonoscopy was the primary available screening test, patients were randomized to receive a culturally tailored letter with educational material and contact (either in person or by phone) with a language-concordant “navigator” or to usual care. The-navigators were community health workers trained to address barriers to CRC screening. Nine months later, participants in the intervention group were more likely to receive colonoscopy than those in the control group (21 % vs 10 %; p<0.001).27 In Healthy Colon, Healthy Life, there was an increase in CRC screening, but as in many low-income settings, the main available CRC screening test was FOBT. In addition, in Healthy Colon, Healthy Life, all of the CHA contact with the participants occurred by telephone, demonstrating that telephone counseling only (which is inherently more efficient than in-person contact) is both feasible and highly effective.
This study has several limitations. It was conducted in a single geographic setting and it is possible that Latinos and Vietnamese living in Santa Clara CA are different from Latinos and Vietnamese living elsewhere in the country. However, these are all patients in a public health care system, and it is likely that this system has many similarities with other public health-care systems nationwide. Second, only two ethnic groups, Latinos and Vietnamese, were included, although these are two very large and important groups in the U.S. However, because efficacy was shown in these two diverse groups, this suggests the potential for broad applicability.
Third, the outcome of CRC screening was by self-report. Nevertheless, standardized questions about CRC screening that have been used and validated in many surveys where individuals are asked about CRC screening were used.41,43,44 In addition, self-report of FOBT screening has previously been shown to be very accurate, with no difference in accuracy related to ethnicity.45 Fourth, CRC screening outcomes are available for only those participants who completed both the baseline and follow-up surveys. Finally, FOBT was the primary available screening test and this may not be the case in other settings. However, self-reported receipt of sigmoidoscopy and colonoscopy was also measured. Also, these results are probably generalizable to many resource-poor settings where there is limited endoscopy capacity and stool tests are likely to be the primary screening option available.
The results of Healthy Colon, Healthy Life, expand on the recommendations of the Task Force on Community Preventive Services46 about client-oriented screening interventions and CRC screening. The Task Force recommends the use of small media, such as brochures, to encourage FOBT screening based on strong evidence of efficacy. However, when the Task Force evaluated the use of one-on-one education either in person or by telephone to increase rates of FOBT screening, it concluded that the evidence was insufficient. The results of Healthy Colon, Healthy Life provide important new evidence to suggest that one-on-one education combined with small media is indeed effective in increasing rates of CRC screening.
Conclusion
This individually and culturally tailored intervention was highly successful in increasing rates of CRC screening in two ethnically diverse populations, Latino and Vietnamese. Key features of the intervention included a single overall approach in which messages were linguistically and culturally appropriate, and telephone counseling was tailored to individual stage of change and delivered by community members through a trusted community-based organization. Future directions include assessment of the cost effectiveness of this intervention and its dissemination for other Vietnamese and Latino communities in addition to research to adapt and test our approach among other ethnic groups in both urban and rural locations.
Acknowledgments
We acknowledge Drs. Longhang Nguyen, Angela Suarez, Ginger Roerhig, Kevin Nguyen, and Leslie Schmidt—all primary care physicians at the participating clinic sites—without whose involvement this study could not have been done. We thank Jacqueline Bishop for assistance in manuscript preparation.
This study was funded by a Research Scholars Grant from the American Cancer Society (JMEW).
This study was partly supported by Grant U01CA114640 from the Center to Reduce Cancer Health Disparities/National Cancer Institute, and its contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Cancer Institute.
Dr. Lamkieu Nguyen, coinvestigator at Santa Clara Valley Medical Center and coauthor, was extremely dedicated to the cause of improving the health of ethnic minorities. She was untiring in her efforts on this project and she was the one who named the project “Healthy Colon, Healthy Life.” Dr. Nguyen died in June 2009.
Footnotes
No financial disclosures were reported by the authors of this paper.
References
- 1.Cancer Facts & Figures for Hispanics/Latinos. 2009 http://www.cancer.org/downloads/STT/FF_Hispanics_Latinos_2009_2011.pdf.
- 2.Cockburn M, Deapen M. Los Angeles Surveillance Program. Los Angeles: University of California; 2004. Cancer incidence and mortality in California: trends by race/ethnicity, 1988–2001. [Google Scholar]
- 3.Levin B, Lieberman DA, McFarland B, et al. Screening and surveillance for the early detection of colorectal cancer and adenomatous polyps, 2008: a joint guideline from the American Cancer Society, the U.S. Multi-Society Task Force on Colorectal Cancer, and the American College of Radiology. Gastroenterology. 2008;134(5):1570–95. doi: 10.1053/j.gastro.2008.02.002. [DOI] [PubMed] [Google Scholar]
- 4.USPSTF. Screening for colorectal cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2008;149(9):627–37. doi: 10.7326/0003-4819-149-9-200811040-00243. [DOI] [PubMed] [Google Scholar]
- 5.Pignone M, Sox HC. Screening guidelines for colorectal cancer: a twice-told tale. Ann Intern Med. 2008;149(9):680–2. doi: 10.7326/0003-4819-149-9-200811040-00247. [DOI] [PubMed] [Google Scholar]
- 6.Wong ST, Gildengorin G, Nguyen T, Mock J. Disparities in colorectal cancer screening rates among Asian Americans and non-Latino whites. Cancer. 2005;104(12S):2940–7. doi: 10.1002/cncr.21521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Walsh J, Kaplan C, Nguyen B, Gildengorin G, McPhee S, Perez-Stable E. Barriers to colorectal cancer screening in Latino and Vietnamese Americans. J Gen Intern Med. 2004;19:156–66. doi: 10.1111/j.1525-1497.2004.30263.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.California Health Interview Survey. 2007 chis.ucla.edu/main/DQ3/output.asp?_rn=0.2959406.
- 9.Barnes JS, Bennett CE. The Asian population: 2000. www.census.gov/prod/2002pubs/c2kbr01-16.pdf.
- 10.Pasick RJ, Hiatt RA, Paskett ED. Lessons learned from community-based cancer screening intervention research. Cancer. 2004;101(5S):1146–64. doi: 10.1002/cncr.20508. [DOI] [PubMed] [Google Scholar]
- 11.Johnson-Kozlow M, Roussos S, Rovniak L, Hovell M. Colorectal cancer test use among Californians of Mexican origin: influence of language barriers. Ethn Dis. 2009;19(3):315–22. [PMC free article] [PubMed] [Google Scholar]
- 12.Watts L, Joseph N, Velazquez A, et al. Understanding barriers to cervical cancer screening among Hispanic women. Am J Obstet Gynecol. 2009;201(2):199.e1–8. doi: 10.1016/j.ajog.2009.05.014. [DOI] [PubMed] [Google Scholar]
- 13.Sequist TD, Zaslavsky AM, Marshall R, Fletcher RH, Ayanian JZ. Patient and physician reminders to promote colorectal cancer screening: a randomized controlled trial. Arch Intern Med. 2009;169(4):364–71. doi: 10.1001/archinternmed.2008.564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McPhee SJ, Bird JA, Jenkins CNH, Fordham D. Promoting cancer screening: a randomized, controlled trial of three interventions. Arch Intern Med. 1989;149:1866–72. doi: 10.1001/archinte.149.8.1866. [DOI] [PubMed] [Google Scholar]
- 15.Turner B, Day S, Borenstein B. A controlled trial to improve delivery of preventive care: physician or patient reminders? J Gen Intern Med. 1989;4(5):403–9. doi: 10.1007/BF02599691. [DOI] [PubMed] [Google Scholar]
- 16.Walsh J, Salazar R, Terdiman J, Gildengorin G, Perez-Stable E. Promoting use of colorectal cancer screening tests. Can we change physician behavior? J Gen Intern Med. 2005;20(12):1097–101. doi: 10.1111/j.1525-1497.2005.0245.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zubarik R, Eisen G, Zubarik J, et al. Education improves colorectal cancer screening by flexible sigmoidoscopy in an inner city population. Am J Gastroenterol. 2000;95(2):509–12. doi: 10.1111/j.1572-0241.2000.t01-1-01776.x. [DOI] [PubMed] [Google Scholar]
- 18.Lane DS, Messina CR, Cavanagh MF, Chen JJ. A provider intervention to improve colorectal cancer screening in county health centers. Med Care. 2008;46(9S1):S109–16. doi: 10.1097/MLR.0b013e31817d3fcf. [DOI] [PubMed] [Google Scholar]
- 19.King J, Fairbrother G, Thompson C, Morris D. Colorectal cancer screening: optimal compliance with postal faecal occult blood test. Aust N Z J Surg. 1992;62(9):714–9. doi: 10.1111/j.1445-2197.1992.tb07068.x. [DOI] [PubMed] [Google Scholar]
- 20.Pye G, Christie M, Chamberlain JO, Moss SM, Hardcastle JD. A comparison of methods for increasing compliance within a general practitioner–based screening project for colorectal cancer and the effect on practitioner workload. J Epidemiol Community Health. 1988;42:66–71. doi: 10.1136/jech.42.1.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zapka J, Lemon S, Puleo E, Estabrook B, Luckmann R, Erban S. Patient education for colon cancer screening: a randomized trial of a video mailed before a physical examination. Ann Inter Med. 2004;141(9):683–92. doi: 10.7326/0003-4819-141-9-200411020-00009. [DOI] [PubMed] [Google Scholar]
- 22.Pasick R, D’Onofrio C, Otero-Sabogal R. Similarities and differences across cultures: questions to inform a third generation for health promotion research. Health Educ Q. 1996;23(S):s142–61. [Google Scholar]
- 23.Pasick RJ, Kagawa-Singer M. Cultural norms. In: Breslow L, editor. Encyclopedia of public health. New York: Macmillan Press; 2001. [Google Scholar]
- 24.Pasick R, Burke NJ, Barker J. Behavioral theory in a diverse society: like a compass on mars. Health Educ Behav. 2009;36:11S–35S. doi: 10.1177/1090198109338917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sabogal F, Otero-Sabogal R, Pasick RJ, Jenkins CNH, Perez-Stable EJ. Printed health education materials for diverse communities: suggestions learned from the field. Health Educ Q. 1996;23(S):S123–41. [Google Scholar]
- 26.Taylor V, Hislop G, Jackson J, et al. A randomized controlled trial of interventions to promote cervical cancer screening among Chinese women in North America. J Natl Cancer Inst. 2002;94(9):670–7. doi: 10.1093/jnci/94.9.670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Percac-Lima S, Grant RW, Green AR, et al. A culturally tailored navigator program for colorectal cancer screening in a community health center: a randomized, controlled trial. J Gen Intern Med. 2009;24(2):211–7. doi: 10.1007/s11606-008-0864-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nguyen TU, Kagawa-Singer M. Overcoming barriers to cancer care through health navigation programs. Semin Oncol Nurs. 2008;24(4):270–8. doi: 10.1016/j.soncn.2008.08.007. [DOI] [PubMed] [Google Scholar]
- 29.Han HR, Lee H, Kim MT, Kim KB. Tailored lay health worker intervention improves breast cancer screening outcomes in non-adherent Korean-American women. Health Educ Res. 2009;24(2):318–29. doi: 10.1093/her/cyn021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sauaia A, Min SJ, Lack D, et al. Church-based breast cancer screening education: impact of two approaches on Latinas enrolled in public and private health insurance plans. Prev Chronic Dis. 2007;4(4):A99. [PMC free article] [PubMed] [Google Scholar]
- 31.Wang JH, Liang W, Schwartz MD, Lee MM, Kreling B, Mandelblatt JS. Development and evaluation of a culturally tailored educational video: changing breast cancer-related behaviors in Chinese women. Health Educ Behav. 2008;35(6):806–20. doi: 10.1177/1090198106296768. [DOI] [PubMed] [Google Scholar]
- 32.Prochaska JO, Redding CA, Evers KE. The transtheoretical model and stages of change. In: Glanz K, Rimer BK, Viswanath K, editors. Health behavior and health education. 4. San Francisco: Jossey-Bass; 2008. p. 105. [Google Scholar]
- 33.Prochaska JO, DiClemente CC. In search of how people change: applications to the addictive behaviors. Am Psychol. 1992;47(9):1102–14. doi: 10.1037//0003-066x.47.9.1102. [DOI] [PubMed] [Google Scholar]
- 34.Rakowski W, Ehrich B, Dube CE, et al. Screening mammography and constructs from the transtheoretical model: associations using two definitions of the stages-of-adoption. Ann Behav Med. 1996;18(2):91–100. doi: 10.1007/BF02909581. [DOI] [PubMed] [Google Scholar]
- 35.Rimer BK, Halabi S, Sugg Skinner C, et al. The short-term impact of tailored mammography decision-making interventions. Patient Educ Couns. 2001;43(3):269–85. doi: 10.1016/s0738-3991(00)00172-5. [DOI] [PubMed] [Google Scholar]
- 36.Lando H, Hellerstedt W, Pirie P, McGovern P. Brief supportive telephone outreach as a recruitment and intervention strategy for smoking cessation. Am J Public Health. 1992;82(1):41–6. doi: 10.2105/ajph.82.1.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Stead L. Telephone counselling for smoking cessation. Cochrane Database Syst Rev. 2002;(3) doi: 10.1002/14651858.CD002850.pub2. [DOI] [PubMed] [Google Scholar]
- 38.Miller SM, Siejak KK, Schroeder CM, Lerman C, Hernandez C, Helm CW. Enhancing adherence following abnormal Pap smears among low-income minority women: a preventive telephone counseling strategy. J Natl Cancer Inst. 1997;89(10):703–8. doi: 10.1093/jnci/89.10.703. [DOI] [PubMed] [Google Scholar]
- 39.Pasick R, Stewart S, Otero-Sabogal R, et al. Outcome of a tailored print and phone counseling trial to increase cancer screening in five ethnic groups. Paper presented at the 27th annual meeting of the American Society of Preventive Oncology; 2003; Philadelphia PA.. [Google Scholar]
- 40.Marin G, Sabogal F, Marin BV, Otero-Sabogal R, Perez-Stable EJ. Development of a short acculturation scale for Hispanics. Hisp J Behav Sci. 1987;9:183–205. [Google Scholar]
- 41.Vernon SW, Meissner H, Klabunde C, et al. Measures for ascertaining use of colorectal cancer screening in behavioral, health services, and epidemiologic research. Cancer Epidemiol Biomarkers Prev. 2004;13(6):898–905. [PubMed] [Google Scholar]
- 42.Shah M, Zhu K, Potter J. Hispanic acculturation and utilization of colorectal cancer screening in the U. S. Cancer Detect Prev. 2006;30(3):306–12. doi: 10.1016/j.cdp.2006.04.003. [DOI] [PubMed] [Google Scholar]
- 43.Etzioni DA, Ponce NA, Babey SH, et al. A population-based study of colorectal cancer test use: results from the 2001 California Health Interview Survey. Cancer. 2004;101(11):2523–32. doi: 10.1002/cncr.20692. [DOI] [PubMed] [Google Scholar]
- 44.CDC. Screening for colorectal cancer—U.S. 1992–1993, and new guidelines. MMWR Morb Mortal Wkly Rep. 1996;45(5):107–10. [PubMed] [Google Scholar]
- 45.Baier M, Calonge N, Cutter G, et al. Validity of self-reported colorectal cancer screening behavior. Cancer Epidemiol Biomarkers Prev. 2000;9(2):229–32. [PubMed] [Google Scholar]
- 46.Task Force on Community Preventive Services. http://www.thecommunityguide.org/cancer/screening/client-oriented.