Abstract
Background and Purpose
We examine whether the proportion of the US population with ≤ 60 minute access to PSCs varies based on geographic and demographic factors.
Methods
Population level access to PSCs within 60 minutes was estimated using validated models of prehospital time accounting for critical prehospital time intervals and existing road networks. We examined the association between geographic factors, demographic factors, and access to care. Multivariable models quantified the association between demographics and PSC access for the entire US and then stratified by urbanicity.
Results
Of the 309 million people in the US, 65.8% had ≤ 60 minute PSC access by ground ambulance (87% major cities, 59% minor cities, 9% suburbs, and 1% rural). PSC access was lower in stroke belt states (44% vs. 69%). Non-Whites were more likely to have access than Whites (77% vs. 62%) and Hispanics were more likely to have access than non-Hispanics (78% vs. 64%). Demographics were not meaningfully associated with access in major cities or suburbs. In smaller cities there was less access in areas with lower income, less education, more uninsured, more Medicare and/or Medicaid eligibles, lower healthcare utilization and healthcare resources...
Conclusions
There are significant geographic disparities in access to PSCs. Access is limited in non-urban areas. Despite the higher burden of cerebrovascular disease in stroke belt states, access to care is lower in these areas. Select demographic and healthcare factors are strongly associated with access to care in smaller cities, but not in other areas, including major cities.
INTRODUCTION
Stroke is a leading cause of death and adult disability in the United States.1 There are well described disparities in the burden of stroke, across both types of people and the places where people live. Black Americans have a higher risk of stroke and higher stroke mortality rates.2, 3 Cerebrovascular disease is more common in rural areas than in urban areas.4 There is a also 20–40% increase in stroke mortality in the Southeastern US compared to other regions, often referred to as the US “stroke belt.”5, 6
The factors underlying disparities in stroke are only partially understood. Hypothesized etiologies include differences in vascular risk factors, socioeconomic status, differential quality of care, and differential access to care.7, 8 Organized inpatient stroke care markedly reduces mortality after stroke, with a number needed to treat as low as 5.9–11 It is possible that geographic variability in the type and intensity of inpatient stroke care available across the US may be contributing to disparities in stroke outcomes.
In an effort to improve the care of stroke patients nationally there has been a strong push to develop systems of care based upon an organized hierarchy of stroke hospitals, similar to the US system of trauma center hospitals.12–14 The Joint Commission (TJC) began certifying Primary Stroke Centers (PSCs) in December of 2003. The certification process is based on criteria recommended by the Brain Attack Coalition. PSCs have been shown to utilize more recombinant tissue plasminogen activator (rt-PA) than non-PSCs.15, 16 TJC certified PSCs also have lower mortality rates than non-certified hospitals.17, 18 Since 2003 more than 900 hospitals throughout the US have become certified PSCs.19 To date however, the organized hierarchy of US stroke hospitals has not incorporated geographic and locational factors of patients and hospitals into its planning process, unlike the US system of trauma centers.20
Stroke, like trauma, is a time critical disease. It is estimated that 1.9 million neurons die every minute during an acute stroke and over time the efficacy of acute stroke therapies decrease.21, 22 In order to maximize the population impact of PSCs, they must be rapidly accessible to the US population. Accessibility, or geographic access, refers to the “relationship between the location of supply and the location of clients, taking into account transportation resources, travel time, distance, and cost.”23
It is known that a large proportion of the US population are not able to access a PSC within 60 minutes.24 However, more nuanced disparities in access to PSCs may exist. Because PSCs are expected to improve the health of the community they serve, disparities in access to PSCs may widen existing disparities in stroke mortality. We sought to determine if there were disparities in the accessibility of and to quantify the relationship between geographic factors and population level demographic variables and accessibility of PSCs.
METHODS
Study Design
A cross-sectional population level geographic analysis quantifying the accessibility of Primary Stroke Centers in the United States was conducted.
Access Calculations
PSCs were defined as hospitals certified by The Joint Commission as Primary Stroke Centers on or before 12/31/2010. A list of all currently certified PSCs was obtained directly from TJC on May 17th, 2011 (personal communication, Jean Range, Executive Director of Disease Specific Care, TJC). Geographic accessibility of PSCs was calculated at the block group level as described below. Block groups are small geographic units, with a population of ~800–1700 people. There are 208,667 block groups in the United States. Block groups are nested within census tracts, which are in turn nested within counties and states, respecting county and state boundaries.
For each block group in the US we estimated prehospital time from the centroid, or population weighted center, to the nearest PSC. Prehospital time is the time required from calling 911 to arriving at a hospital. It is a composite of transport time and other key prehospital time intervals. Detailed methods for these calculations have been previously reported.24 Briefly, the Network Analyst Function in ESRI ArcMap 10.1 was used to calculate the shortest road distance between each centroid and the closest PSC. Posted speed limits were used to calculate transport times with 10 miles per hour added. The 911 activation to ambulance dispatch interval was estimated as 1.4, 1.4, and 2.9 minutes for urban, suburban, and rural areas.25 Ambulance dispatch to arrival at the scene was estimated by multiplying the drive time from the scene to the hospital by 1.6, 1.5, and 1.4 for urban, suburban, and rural drives, respectively.25 Finally, 13.5, 13.5, and 15.1 minutes were added to urban, suburban, and rural areas to account for time spent on scene by Emergency Medical Services (EMS) personnel.25, 26 Models were built assuming that patients and EMS providers would not cross state lines.
Population Level Demographic Data
Race, sex, ethnicity and employment data were obtained at the block group level from the 2010 Nielsen-Claritas census estimates. These are commercially available data based on the 2000 Census, but updated annually to account for projected changes to the population. Data on income, poverty, and education were obtained from the American Community Survey (ACS) 2005–2009 five year estimates. The ACS is released by the US Census Bureau and uses survey data to create national estimates. The 5 year data is available at the smallest geographic units, including block groups and census tracts. The 2005–2009 estimates were the most recent available dataset that maintained the geographic boundaries of the 2000 Census, upon which access calculations are based. Detailed data documentation are available online (http://www.census.gov/acs/www/data_documentation/documentation_main/). Data on insurance status, healthcare resources, and healthcare utilization were obtained from the Area Resource File 2011–2012 data release. The Area Resource File pulls together information from a variety of sources, including the American Hospital Association, American Medical Association, Centers for Medicare and Medicaid Services, and the US Census. ARF data are available only at the county level. Detailed data documentation are available online (http://datawarehouse.hrsa.gov/data/datadownload/ahrfdownload.aspx) We defined urbanicity using a modified version of the US Department of Agriculture Rural-Urban Continuum code (mRUC). The mRUC classifies counties based on the size of each metropolitan area and/or proximity to metropolitan areas.27 The mRUC is defined in Supplemental Table I. We categorized areas as major cities if mRUC was 0–1, minor cities if mRUC was 2–3, suburbs if mRUC was 4–7, and rural if mRUC was 8–9. For variables not available at the block group level, all block groups in the census tract or county were assigned the same value. Variables used in the analysis, including their source and level of geography are summarized in Supplemental Table II.
Statistical Analysis
We calculated the total prehospital time required to access a PSC via ground transport for each block group in the US. Block groups were considered to have geographic access to PSCs if the total prehospital time from the centroid to the nearest PSC was ≤ 60 minutes. It was assumed that the PSC was equally accessible to all inhabitants in the block group. Results were summed to determine the proportion of the US population able to access a PSC within 60 minute by ground transport. We then calculated the proportion of the population with PSC access stratified by mRUC categories. Access was further stratified by race (White vs. non-White), ethnicity (Hispanic vs. non-Hispanic), sex, Census region, and location within a stroke belt state (AL, AR, GA, LA, MS, NC, SC, TN).
We then performed a descriptive analysis comparing demographic variables between block groups with PSC access to those without PSC access. Variables included information on race, ethnicity, education, socioeconomic status, insurance status, healthcare resources, and healthcare utilization (Supplemental Table II). Data reduction techniques were used to convert correlated individual variables into a smaller number of summary variables to improve interpretability of the results. Cronbach’s alpha was used to evaluate the internal consistency of each set of variables, and factor analysis was conducted to create a single summary variable from a collection of strongly related individual variables.28 Each factor variable is measured as a z-score (mean=0, and standard deviation=1). A generalized linear mixed model was constructed using a logit link and robust standard error estimates. Models used a random intercept to account for clustering of block groups into counties. Because mRUC category was very strongly associated with access to PSCs in the univariate analysis, models were stratified by mRUC category for major cities, minor cities, and suburbs. Models were not constructed for rural areas because almost no rural block groups had access to PSCs (0.9%). After constructing models, the predicted probability of access to PSCs was estimated for each block group and the median predicted probability of PSC access was compared across block groups that were low (below the median) and high (above the median) for each factor variable.
RESULTS
There were 811 PSCs in the US on 12/31/2010. Of the 309 million people in the US, 65.8% had ≤ 60 minute PSC access by ground ambulance. Geographic accessibility of PSCs is mapped in Figure 1. The proportion of the population with PSC access ≤ 60 minutes was: 87% in major cities, 59% in minor cities, 9% in suburbs, and 1% in rural areas (Table 1). By Census region, PSC access was lower in the South (61%) than in the Midwest (66%), Northeast (67%), and West (72%). PSCs were less accessible in the stroke belt than the rest of the US (44% vs. 69%, p<0.001). Although this was partially attributable to more people living in non-urban areas within the stroke belt, PSC access was also worse in stroke belt cities (Table 2). A greater proportion of non-Whites had access to PSCs than Whites (77% vs. 62%, p<0.001), and a greater proportion of Hispanics had access to PSCs than non-Hispanics (78% vs. 64%, p<0.001). These differences were greatest in Major Cities (Table 2). There was no meaningful difference in access to PSCs by sex (65.6% vs. 66.0%, p<0.001).
Figure 1. Areas of the US with ≤60 Minute PSC Access as of 12/31/2010.
Adapted with permission from www.strokemaps.org
Gray shaded areas represent areas of the US with ≤ 60 minute access to hospitals certified as PSCs by The Joint Commission as of 12/31/2010.
Table 1.
Proportion of the US Population with ≤60 Minute PSC Access
| # Block Groups |
Total Population |
% of US Population |
≤ 60 Min PSC Access | >60 min PSC Access | |||
|---|---|---|---|---|---|---|---|
| N | % | N | % | ||||
| Major Cities | 105,028 | 166,133,404 | 54% | 144,760,736 | 87% | 21,372,668 | 13% |
| Minor Cities | 60,944 | 92,336,028 | 30% | 54,523,084 | 59% | 37,812,944 | 41% |
| Suburbs | 37,490 | 45,389,833 | 15% | 3,933,477 | 9% | 41,456,356 | 91% |
| Rural | 5,205 | 5,179,715 | 2% | 66,025 | 1% | 5,113,690 | 99% |
Table 2.
Access to PSCs by Stroke Belt Location, Race, and Ethnicity
| Entire US | Major Cities | Minor Cities | Suburbs | Rural | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | 60 Min Access |
N | 60 Min Access |
N | 60 Min Access |
N | 60 Min Access |
N | 60 Min Access |
|
| StrokeBelt | 45,374,794 | 44.5% | 12,593,422 | 75.6% | 20,160,323 | 47.1% | 11,249,333 | 10.2% | 1,371,716 | 1.3% |
| Non-StrokeBelt | 263,664,186 | 69.4% | 153,539,978 | 88.1% | 72,175,710 | 62.4% | 34,140,499 | 8.2% | 3,807,999 | 1.3% |
| White | 223,493,068 | 61.7% | 109,736,596 | 84.3% | 71,478,980 | 58.5% | 37,810,368 | 9.1% | 4,467,124 | 1.4% |
| non-White | 85,545,907 | 76.6% | 56,396,799 | 92.7% | 20,857,051 | 61.0% | 7,579,466 | 6.7% | 712,591 | 0.6% |
| Hispanic | 48,892,409 | 77.9% | 32,859,227 | 93.2% | 12,469,131 | 58.3% | 3,373,560 | 5.7% | 190,491 | 0.8% |
| non-Hispanic | 260,146,565 | 63.5% | 133,274,168 | 85.6% | 79,866,900 | 59.2% | 42,016,273 | 8.9% | 4,989,224 | 1.3% |
Demographic variables are summarized in Table 3. The 35 individual variables were reduced to 11 composite factor variables representing: income, poverty, proportion uninsured, proportion eligible for Medicare and/or Medicaid, proportion who dropped out of high school or college, proportion with an advanced degree, race, ethnicity, healthcare utilization, physician supply, and hospital supply. The employment variable did not fit into any factors and was maintained as an individual variable.
Table 3.
Demographic Variables, Stratified by ≤60 Min PSC Access
| All Block Groups in the USA | Block Groups with Access to a Primary Stroke Center* |
Block Groups without Access to a Primary Stroke Center* |
|||
|---|---|---|---|---|---|
| Median | Interquartile Range | Median | Median | p-value | |
| Income | |||||
| Per Capita Income1 | $23,139 | $17,551 – $31,060 | $24,870 | $21,493 | <.0001 |
| Per Capita Income2 | $23,208 | $17,312 – $31,369 | $24,999 | $21,342 | <.0001 |
| Median Household Income2 | $48,125 | $34,632 – $66,904 | $52,436 | $43,250 | <.0001 |
| Median Family Income2 | $57,404 | $41,552 – $79,010 | $62,500 | $52,303 | <.0001 |
| Poverty | |||||
| % Population Under 18 Living in Poverty3 | 15.2% | 5.9% – 29.1% | 13.1% | 17.9% | <.0001 |
| % Population 18 to 64 Living in Poverty3 | 10.7% | 5.8% – 18.2% | 9.5% | 12.2% | <.0001 |
| % Population 65 and Over Living in Poverty3 | 8.2% | 3.8% – 14.8% | 7.2% | 9.5% | <.0001 |
| % Total Population Living in Poverty3 | 11.5% | 6.1% – 19.6% | 10.2% | 13.1% | <.0001 |
| % of Households Receiving Public Assistance Income2 | 0.5% | 0.0% – 3.6% | 0.0% | 0.9% | <.0001 |
| % of Families with Income Below the Poverty Level2 | 6.6% | 0.0% – 16.5% | 5.6% | 8.0% | <.0001 |
| Insurance Status | |||||
| % Under 19 without Health Insurance4 | 7.1% | 5.4 – 11.0% | 6.6% | 7.1% | <.0001 |
| % Under 65 without Health Insurance4 | 16.3% | 12.7% – 20.2% | 16.3% | 16.7% | 0.0013 |
| CMS Eligibles | |||||
| % Eligible for Medicare4 | 14.9% | 12.3% – 17.5% | 13.4% | 17.4% | <.0001 |
| % Eligible for Medicaid4 | 19.0% | 14.2% – 24.6% | 18.4% | 19.5% | <.0001 |
| Education - Dropouts | |||||
| % Population 25 or Over with Less than High School Degree2 | 13.0% | 6.2% – 23.4% | 11.8% | 14.6% | <.0001 |
| % Population 25 or Over with Some College Education2 | 27.2% | 20.3% – 34.0% | 26.9% | 27.6% | <.0001 |
| Education - Degrees | |||||
| % Population 25 or Over, High School Graduate2 | 30.8% | 21.2% – 39.9% | 27.5% | 35.5% | <.0001 |
| % Population 25 or Over, Bachelors Degree2 | 13.5% | 7.1% – 22.8% | 16.1% | 10.6% | <.0001 |
| % Population 25 or Over, Master’s Degree2 | 4.5% | 1.6% – 9.4% | 5.4% | 3.6% | <.0001 |
| % Population 25 or Over, Professional Degree2 | 0.3% | 0.0% – 2.3% | 0.7% | 0.0% | <.0001 |
| % Population 25 or Over, Doctoral Degree2 | 0.0% | 0.0% – 1.3% | 0.0% | 0.0% | <.0001 |
| Employment | |||||
| % in Labor Force who are Employed1 | 94.6% | 90.8% – 97.1% | 94.7% | 94.5% | <.0001 |
| Race | 2.7% | 0.6% – 12.9% | 4.0% | 1.2% | <.0001 |
| % Black1 | 16.0% | 5.6% – 43.6% | 22.7% | 8.3% | <.0001 |
| % Non-White1 | |||||
| Ethnicity & Origin | |||||
| % Hispanic1 | 4.4% | 1.6% – 15.4% | 6.5% | 2.3% | <.0001 |
| % Foreign-Born1 | 5.9% | 2.0% – 15.4% | 9.6% | 2.4% | <.0001 |
| Healthcare Utilization | |||||
| Total Hospital Admissions per 1,000 Population4 | 118.9 | 83.0 – 166.2 | 130.2 | 96.1 | <.0001 |
| Total Hospital Beds per 1,000 Population4 | 2.9 | 2.0 – 4.1 | 3.1 | 2.7 | <.0001 |
| Total Hospital Inpatient Days Per 1,000 Population4 | 739.2 | 439.2 – 1054.0 | 811.0 | 533.3 | <.0001 |
| Total Hospital ED Visits per 1,000 Population4 | 398.3 | 278.7 – 524.3 | 380.9 | 436 | <.0001 |
| Healthcare Resources - Doctors | |||||
| Non-Federal MDs in Neurology Devoted to Total Patient Care per 100,000 Population4 | 3.9 | 1.6 – 6.2 | 4.9 | 1.4 | <.0001 |
| Non-Federal MDs in Emergency Medicine Devoted to Total Patient Care per 100,000 Population4 | 9.7 | 5.0 – 13.9 | 10.9 | 5 | <.0001 |
| Healthcare Resources - Hospitals | |||||
| Total Number of Hospitals Per 100,000 population4 | 1.6 | 1.1-2.6 | 0.7 | 1.5 | <.0001 |
| Per Capita Total Number of Critical Access Hospitals4 | 0 | 0.0 - 0.0 | 0 | 0 | <.0001 |
| Per Capita STG Hospitals With ED4 | 0.8 | 0.6-1.5 | 0.7 | 1.5 | <.0001 |
Within 60 minutes via ground transport, not crossing state boundaries
Neilsen/Claritas (block group level data)
2005 – 2009 ACS (block group level data)
2005 – 2009 ACS (census tract level data)
2011 – 2012 ARF (county level data)
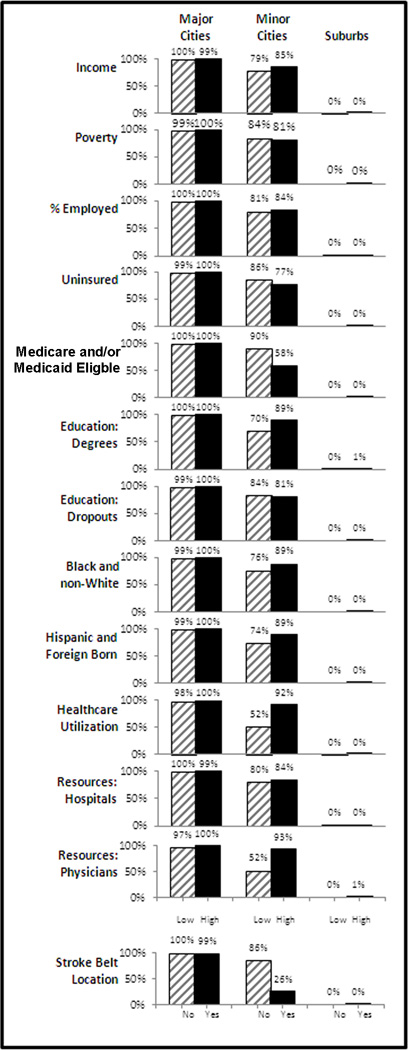
Multivariable modeling results are summarized in Supplemental Table III, IV, V. Figure 2 shows the median predicted probability of access to PSCs in areas that are low and high for each composite variable. In Major Cities, access to PSCs is high in all areas with very little variation. Conversely, in suburban areas access to PSCs was uniformly low in all areas.
Figure 2. Adjusted Probability of ≤60 Minute PSC Access.
Predicted probabilities of having ≤ 60 minute PSC access for block groups that are above the median (“High”) and below the median (“low”) for each factor, adjusted for all other factors.
There was significant variability in access within minor cities. In minor cities, areas with high rates of Medicare and/or Medicaid eligibility were less likely to have access (58% vs. 90%). In minor cities, areas with higher rates of uninsured individuals were also less likely to have access to PSCs (77% vs. 86%). Areas with high healthcare utilization were more likely to have access to PSCs (92% vs. 52%). Areas with higher physician resources were also more likely to have access (93% vs. 52%). Areas in the stroke belt were less likely to have access (26% vs. 86%). Hospital resources, education, income, black/non-white, and Hispanic/foreign born were also positively associated with access to PSCs in minor cities (Figure 2).
DISCUSSION
As of December 31st 2010, 105 million Americans were unable to access a PSC by ground ambulance within 60 minutes of calling 911. Geography was the major determinate of access to PSCs, with worse access in the stroke belt and in non-urban areas. In major cities 87% of the population had ≤60 minute access. This fell to 59% in minor cities, 9% in suburbs, and 1% in rural areas. Reduced access in the stroke belt is likely due, in part, to a higher proportion of people living in suburban/rural areas compared to the rest of the US (29.0% vs. 16.4%). This is not the only explanation, as stroke belt access was also worse in major cities (75.6% vs. 88.1%) and in minor cities (47% vs. 62.4%). Geographic disparities in the burden of cerebrovascular disease are well known, with a greater burden of disease in the stroke-belt and in non-urban areas.29, 30,4, 31 It is possible that reduced access to care in stroke belt states and in non-urban areas has contributed to the development of these disparities.29
If stroke care systems improve the health of the communities that they serve, disparities in access to specialized stroke care may widen existing disparities in stroke outcomes. In an effort to improve population health, the Institute of Medicine recommended the development of regionalized systems of care which direct patients to specialized hospitals that are best equipped to care for them.3233 In accordance with these recommendations, many states have enacted prehospital routing policies shunting patients to certified PSCs and bypassing closer hospitals.34 Although data quantifying the impact of regionalization are limited, it is known that PSCs utilize more acute stroke therapies and have lower mortality rates than non-PSCs.15–18 Prehospital delays in arrival at a PSC reduce the chances of receiving acute stroke therapies and reduce the effectiveness of those therapies in treated patients.35–37 Living further from a stroke center is also associated with higher mortality after stroke.3839 It therefore seems plausible that, as regionalized systems of care develop, areas with limited PSC access may have worse outcomes than other areas.
Our finding that areas with higher burdens of cerebrovascular disease are less likely to have access to PSCs underscores the need for population planning to ensure that stroke care is rapidly accessible in areas with the greatest need. Although the adjusted probability of PSC access is uniformly high in major cities, there is considerable variability within minor cities and almost no access in non-Urban areas. Policy makers and health planners can incentivize the development of PSCs in order to improve access to care. This is likely to be particularly important in areas of minor cities with lower socioeconomic status and poor payer mix, as these areas are densely populated but less likely to gain access. Importantly, data from the US and Canada suggest that socioeconomic status does not have a significant effect on hospital choice, so increased geographic accessibility should benefit all people.40, 41 Improving access in suburban and rural areas may pose challenging. Although there are more than 50 million Americans living in non-urban areas, low population density and/or limited physician/hospital resources may make it difficult to provide PSC access to all of these people. It is likely that targeted interventions - which identify areas with great need and provide access to the maximum number of people – will be necessary. For other areas, which are unable to support a PSC, alternative solutions such as telemedicine and/or pre-defined transfer agreements may be preferable.
The development of flexible tools that can be used by policy makers to plan systems of care, incorporating the local burden of disease, hospital/physician resources, and costs have the potential to significantly impact population health. These tools will become even more important as stroke care systems become increasingly complex, incorporating Comprehensive Stroke Centers and Acute Stroke Ready Hospitals. Such tools could also be used to help guide the development of systems of care for other time sensitive conditions like myocardial infarction, cardiac arrest, and sepsis. For regionalization to be optimized there is also a need for public policies which incentivize cooperation across hospitals and between hospitals and EMS providers. Furthermore, population level health outcome measures must be developed in order to quantify the impact of regionalization.
This ecologic study has important limitations. Our access calculations estimate the geographic accessibility of PSCs. Because geographic accessibility is only one component of access to care, we may be over-estimating PSC access. Our results however are consistent with a prior study which looked at disparities in realized access to PSCs. That study, which identified the treating hospital for 1000 subjects with suspected stroke in a large prospective cohort study (REGARDS) found that non-urban residence (OR=0.39, 95% CI 0.22–0.67) and stroke belt residence (OR=0.54, 95% CI 0.38–0.77) were independent, negative predictors of evaluation at a PSC.40 PSC access calculations require assumptions about key EMS time intervals. We used estimates that were empirically derived from the trauma literature using data from over 150,000 patients in 20 states. Prior studies have suggested that stroke prehospital intervals may be up to 11 minutes longer, although these studies were geographically limited to 2 large urban centers and may not be generalizable.42, 43 Additionally, both studies were conducted before the American Heart Association released a policy statement recommending that stroke patients be treated at the highest possible priority. As a result, they may not be representative of current practice.44 If differences in prehospital time intervals between stroke and trauma exist this could introduce measurement bias; although, this is expected to be non-differential and comparisons across geographic areas should still be valid. The analysis was limited to hospitals certified by TJC and did not account for hospitals certified by other agencies, including state health departments. There are 10 states with state-based PSCs (CT, FL, MD, MA, NJ, NY, OK, TX, VA, and WA). We likely underestimate access in these states. Since none of these states are located in the stroke belt the disparity in access between stroke belt and non-belt states is underestimated. The traditional definition of the stroke belt was used in this analysis, though there recent evidence suggests that the stroke belt may now extend further north and west.45 Because we used factor analysis to create composite variables, we are unable to quantifying the association between individual demographic variables and access to care. Finally, as an ecologic analysis conducted at a single time point we are unable to ascertain whether differential access to stroke care affects outcomes at the population level or if disparities are changing over time.
Conclusion
There are significant geographic disparities in access to PSCs. Access is limited in suburban and rural areas. Despite the higher burden of cerebrovascular disease in stroke belt states, access to care is lower in these areas. Demographic factors are strongly associated with access to care in smaller cities, but were found to have very little impact elsewhere, including major cities. Within smaller cities, areas with lower income, less education, more uninsured, more Medicare and/or Medicaid eligible individuals, lower healthcare utilization and healthcare resources were less likely to have access. Public policy and health systems planning are needed to ensure stroke care is rapidly accessibly to all Americans.
Supplementary Material
ACKNOWLEDGEMENTS
Dr. Mullen had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
The authors would like to thank the Cartographic Modeling Lab at the University of Pennsylvania, in particular Tara Jackson, Karl Dailey, Vicky Tam, & Krista Heinlen.
SOURCES OF FUNDING
This research was supported by a grant from the Agency for Healthcare Research & Quality (R01HS010914 – Branas, Carr, Mullen)
Dr. Carr is funded by a career development award from the Agency for Healthcare Research & Quality (K08 HS017960)
Dr. Albright is supported by Award Numbers 5 T32 HS013852-10 from The Agency for Healthcare Research and Quality (AHRQ) and 3 P60 MD000502-08S1 from The National Institute on Minority Health and Health Disparities (NIMHD), National Institutes of Health (NIH).
CONFLICT(S) OF INTEREST/DISCLOSURES
Dr. Albright is funded by the AHRQ and NIH. This content is solely the responsibility of the authors and does not necessarily represent the official views of the AHRQ or the NIH.
Dr. Carr spends a portion of his time as a Senior Policy Analyst in the Office of the Assistant Secretary for Preparedness and Response. The findings and conclusions in this report are those of the author and do not necessarily represent the views of the Department of Health and Human Services or its components.
REFERENCES
- 1.Xu JK, Kenneth D, Murphy, Sherry L Tejada-Vera, Betzaida. Deaths: Final data for 2007. National Vital Stat. 2010;58 [PubMed] [Google Scholar]
- 2.National Heart, Lung, and Blood Institute. Bethesda, MD: National Heart, Lung, and Blood Institute; [Accessed April 1st 2014]. Incidence and Prevalence: 2006 CDC Chart Book on Cardiovacsular and Lung Diseases. Website. Available at: http://www.nhlbi.nih.gov/resources/docs/06a_ip_chtbk.pdf. [Google Scholar]
- 3.Centers for Disease Control and Prevention. Disparities in deaths from stroke among persons aged <75 years--united states, 2002. MMWR Morb Mortal Wkly Rep. 2005;54:477–481. [PubMed] [Google Scholar]
- 4.Adams PF, Hendershot GE, Marano MA. Current estimates from the national health interview survey, 1996. Vital Health Stat 10. 1999:1–203. [PubMed] [Google Scholar]
- 5.Howard G, Evans GW, Pearce K, Howard VJ, Bell RA, Mayer EJ, et al. Is the stroke belt disappearing? An analysis of racial, temporal, and age effects. Stroke; a journal of cerebral circulation. 1995;26:1153–1158. doi: 10.1161/01.str.26.7.1153. [DOI] [PubMed] [Google Scholar]
- 6.Perry HM, Roccella EJ. Conference report on stroke mortality in the southeastern united states. Hypertension. 1998;31:1206–1215. doi: 10.1161/01.hyp.31.6.1206. [DOI] [PubMed] [Google Scholar]
- 7.Mensah GA. State of disparities in cardiovascular health in the united states. Circulation. 2005;111:1233–1241. doi: 10.1161/01.CIR.0000158136.76824.04. [DOI] [PubMed] [Google Scholar]
- 8.Cruz-Flores S, Rabinstein A, Biller J, Elkind MS, Griffith P, Gorelick PB, et al. Racial-ethnic disparities in stroke care: The american experience: A statement for healthcare professionals from the american heart association/american stroke association. Stroke; a journal of cerebral circulation. 2011;42:2091–2116. doi: 10.1161/STR.0b013e3182213e24. [DOI] [PubMed] [Google Scholar]
- 9.Stroke Unit Trialists Collaborations. Organised inpatient (stroke unit) care for stroke. Cochrane Database Syst Rev. 2007:CD000197. doi: 10.1002/14651858.CD000197.pub2. [DOI] [PubMed] [Google Scholar]
- 10.Seenan P, Long M, Langhorne P. Stroke units in their natural habitat: Systematic review of observational studies. Stroke; a journal of cerebral circulation. 2007;38:1886–1892. doi: 10.1161/STROKEAHA.106.480871. [DOI] [PubMed] [Google Scholar]
- 11.Smith EE, Hassan KA, Fang J, Selchen D, Kapral MK, Saposnik G. Do all ischemic stroke subtypes benefit from organized inpatient stroke care? Neurology. 2010;75:456–462. doi: 10.1212/WNL.0b013e3181ebdd8d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alberts MJ, Hademenos G, Latchaw RE, Jagoda A, Marler JR, Mayberg MR, et al. Recommendations for the establishment of primary stroke centers. Brain attack coalition. JAMA. 2000;283:3102–3109. doi: 10.1001/jama.283.23.3102. [DOI] [PubMed] [Google Scholar]
- 13.Alberts MJ, Latchaw RE, Selman WR, Shephard T, Hadley MN, Brass LM, et al. Recommendations for comprehensive stroke centers: A consensus statement from the brain attack coalition. Stroke; a journal of cerebral circulation. 2005;36:1597–1616. doi: 10.1161/01.STR.0000170622.07210.b4. [DOI] [PubMed] [Google Scholar]
- 14.Schwamm LH. Recommendations for the establishment of stroke systems of care: Recommendations from the american stroke association's task force on the development of stroke systems. Circulation. 2005;111:1078–1091. doi: 10.1161/01.CIR.0000154252.62394.1E. [DOI] [PubMed] [Google Scholar]
- 15.Mullen MT, Kasner SE, Kallan MJ, Kleindorfer DO, Albright KC, Carr BG. Joint commission primary stroke centers utilize more rt-pa in the nationwide inpatient sample. Journal of the American Heart Association. 2013;2:e000071. doi: 10.1161/JAHA.112.000071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Prabhakaran S, McNulty M, O'Neill K, Ouyang B. Intravenous thrombolysis for stroke increases over time at primary stroke centers. Stroke; a journal of cerebral circulation. 2012;43:875–877. doi: 10.1161/STROKEAHA.111.640060. [DOI] [PubMed] [Google Scholar]
- 17.Xian Y, Holloway RG, Chan PS, Noyes K, Shah MN, Ting HH, et al. Association between stroke center hospitalization for acute ischemic stroke and mortality. JAMA. 2011;305:373–380. doi: 10.1001/jama.2011.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lichtman JH, Jones SB, Wang Y, Watanabe E, Leifheit-Limson E, Goldstein LB. Outcomes after ischemic stroke for hospitals with and without joint commission-certified primary stroke centers. Neurology. 2011;76:1976–1982. doi: 10.1212/WNL.0b013e31821e54f3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Facts About Primary Stroke Centers. [Accessed 6/28/2012, 2012e];2011 Website. Available at: http://www.jointcommission.org/AboutUs/Fact_Sheets/psc_certification.htm. [Google Scholar]
- 20.Branas CC, MacKenzie EJ, Williams JC, Schwab CW, Teter HM, Flanigan MC, et al. Access to trauma centers in the united states. JAMA. 2005;293:2626–2633. doi: 10.1001/jama.293.21.2626. [DOI] [PubMed] [Google Scholar]
- 21.Saver JL. Time is brain--quantified. Stroke; a journal of cerebral circulation. 2006;37:263–266. doi: 10.1161/01.STR.0000196957.55928.ab. [DOI] [PubMed] [Google Scholar]
- 22.Lees KR, Bluhmki E, von Kummer R, Brott TG, Toni D, Grotta JC, et al. Time to treatment with intravenous alteplase and outcome in stroke: An updated pooled analysis of ecass, atlantis, ninds, and epithet trials. Lancet. 2010;375:1695–1703. doi: 10.1016/S0140-6736(10)60491-6. [DOI] [PubMed] [Google Scholar]
- 23.Penchansky R, Thomas JW. The concept of access: Definition and relationship to consumer satisfaction. Medical care. 1981;19:127–140. doi: 10.1097/00005650-198102000-00001. [DOI] [PubMed] [Google Scholar]
- 24.Albright KC, Branas CC, Meyer BC, Matherne-Meyer DE, Zivin JA, Lyden PD, et al. Access: Acute cerebrovascular care in emergency stroke systems. Arch Neurol. 2010;67:1210–1218. doi: 10.1001/archneurol.2010.250. [DOI] [PubMed] [Google Scholar]
- 25.Carr BG, Caplan JM, Pryor JP, Branas CC. A meta-analysis of prehospital care times for trauma. Prehosp Emerg Care. 2006;10:198–206. doi: 10.1080/10903120500541324. [DOI] [PubMed] [Google Scholar]
- 26.Carr BG, Branas CC, Metlay JP, Sullivan AF, Camargo CA., Jr Access to emergency care in the united states. Annals of emergency medicine. 2009;54:261–269. doi: 10.1016/j.annemergmed.2008.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.USDA. Rural-Urban Continuum Codes. [Accessed April 9th, 2014]; Available at: http://www.ers.usda.gov/data-products/rural-urban-continuum-codes/documentation.aspx#referencedate.
- 28.Gorsuch RL. Factor analysis. Hillsdale, New Jersey: Lawrence Erlbaum Associated, Inc; 1983. [Google Scholar]
- 29.Howard G. Why do we have a stroke belt in the southeastern united states? A review of unlikely and uninvestigated potential causes. The American journal of the medical sciences. 1999;317:160–167. doi: 10.1097/00000441-199903000-00005. [DOI] [PubMed] [Google Scholar]
- 30.Lanska DJ. Geographic distribution of stroke mortality in the united states: 1939–1941 to 1979–1981. Neurology. 1993;43:1839–1851. doi: 10.1212/wnl.43.9.1839. [DOI] [PubMed] [Google Scholar]
- 31.Sergeev AV. Racial and rural-urban disparities in stroke mortality outside the stroke belt. Ethnicity & disease. 2011;21:307–313. [PubMed] [Google Scholar]
- 32.Carr BG, Asplin BR. Regionalization and emergency care: The institute of medicine reports and a federal government update. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2010;17:1351–1353. doi: 10.1111/j.1553-2712.2010.00944.x. [DOI] [PubMed] [Google Scholar]
- 33.Wheatley B Institute of Medicine (U.S.) Regionalizing emergency care : Workshop summary. Washington, D.C.: National Academies Press; 2010. Planning Committee on Regionalizing Emergency Care Service., National Academies Press (U.S.) [PubMed] [Google Scholar]
- 34.Song S, Saver J. Growth of regional acute stroke systems of care in the united states in the first decade of the 21st century. Stroke; a journal of cerebral circulation. 2012;43:1975–1978. doi: 10.1161/STROKEAHA.112.657809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Barber PA, Zhang J, Demchuk AM, Hill MD, Buchan AM. Why are stroke patients excluded from tpa therapy? An analysis of patient eligibility. Neurology. 2001;56:1015–1020. doi: 10.1212/wnl.56.8.1015. [DOI] [PubMed] [Google Scholar]
- 36.O'Connor RE, McGraw P, Edelsohn L. Thrombolytic therapy for acute ischemic stroke: Why the majority of patients remain ineligible for treatment. Annals of emergency medicine. 1999;33:9–14. doi: 10.1016/s0196-0644(99)70411-7. [DOI] [PubMed] [Google Scholar]
- 37.Chiu D, Krieger D, Villar-Cordova C, Kasner SE, Morgenstern LB, Bratina PL, et al. Intravenous tissue plasminogen activator for acute ischemic stroke: Feasibility, safety, and efficacy in the first year of clinical practice. Stroke; a journal of cerebral circulation. 1998;29:18–22. doi: 10.1161/01.str.29.1.18. [DOI] [PubMed] [Google Scholar]
- 38.Kazley AS, Hillman DG, Johnston KC, Simpson KN. Hospital care for patients experiencing weekend vs weekday stroke: A comparison of quality and aggressiveness of care. Arch Neurol. 2010;67:39–44. doi: 10.1001/archneurol.2009.286. [DOI] [PubMed] [Google Scholar]
- 39.Murata A, Matsuda S. Association between ambulance distance to hospitals and mortality from acute diseases in japan: National database analysis. Journal of public health management and practice : JPHMP. 2013;19:E23–E28. doi: 10.1097/PHH.0b013e31828b7150. [DOI] [PubMed] [Google Scholar]
- 40.Mullen MT, Judd S, Howard VJ, Kasner SE, Branas CC, Albright KC, et al. Disparities in evaluation at certified primary stroke centers: Reasons for geographic and racial differences in stroke. Stroke; a journal of cerebral circulation. 2013;44:1930–1935. doi: 10.1161/STROKEAHA.111.000162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ahuja C, Mamdani M, Saposnik G. Influence of socioeconomic status on distance traveled and care after stroke. Stroke; a journal of cerebral circulation. 2012;43:233–235. doi: 10.1161/STROKEAHA.111.635045. [DOI] [PubMed] [Google Scholar]
- 42.Ramanujam P, Castillo E, Patel E, Vilke G, Wilson MP, Dunford JV. Prehospital transport time intervals for acute stroke patients. J Emerg Med. 2009;37:40–45. doi: 10.1016/j.jemermed.2007.11.092. [DOI] [PubMed] [Google Scholar]
- 43.Wojner-Alexandrov AW, Alexandrov AV, Rodriguez D, Persse D, Grotta JC. Houston paramedic and emergency stroke treatment and outcomes study (hopsto) Stroke; a journal of cerebral circulation. 2005;36:1512–1518. doi: 10.1161/01.STR.0000170700.45340.39. [DOI] [PubMed] [Google Scholar]
- 445.Acker JE, 3rd, Pancioli AM, Crocco TJ, Eckstein MK, Jauch EC, Larrabee H, et al. Implementation strategies for emergency medical services within stroke systems of care: A policy statement from the american heart association/american stroke association expert panel on emergency medical services systems and the stroke council. Stroke; a journal of cerebral circulation. 2007;38:3097–3115. doi: 10.1161/STROKEAHA.107.186094. [DOI] [PubMed] [Google Scholar]
- 45.Centers for Disease Control and Prevention. Stroke death rates 2008–2010, adults age 35+, by county. [Accessed June 30th, 2014];2014 Available at: www.cdc.gov/dhdsp/maps/national_maps/stroke_all.htm.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.