Abstract
Purpose:
The purpose of this study was to describe the breast ultrasonography (US) features and to investigate whether performing a core biopsy is warranted in young women having palpable solid breast masses.
Methods:
A total of 76 solid palpable masses in 68 consecutive women (≤25 years old) underwent tissue diagnosis by percutaneous core biopsy. Two radiologists, who were blinded to the clinical history and histopathology, independently evaluated the US features according to Breast Imaging-Reporting and Data System (BI-RADS) lexicon. The frequency of benign and malignant descriptor terms that were used to characterize the lesions were compared to the final pathology.
Results:
All 76 palpable solid masses yielded benign pathology. On the US, the shape of the mass was described by radiologists 1 and 2 as oval or round (63.2% and 71.1%), margin as circumscribed (68.4% and 77.6%) and orientation as parallel (85.5% and 90.8%); the frequency of using all three benign descriptors was 61.8% and 68.5%, respectively. Suspicious descriptors were used less frequently by radiologists 1 and 2 including irregular shape (9.2% and 13.1%), non-circumscribed margin (31.6% and 22.4%) and non-parallel orientation (14.5% and 9.2%); the frequency of using all three suspicious descriptors was 9.2% and 11.8%, respectively.
Conclusion:
Despite the variable US features, breast malignancy seems extremely low in 25 years or younger women for palpable breast lesions. Using the BI-RADS lexicon, US accurately predicted benignity in about two thirds of our patients, supporting US surveillance as a safe alternative to invasive tissue sampling in this setting.
Keywords: Breast, Breast diseases, Young adult, Ultrasonography
Introduction
Breast ultrasonography (US) is widely accepted as an adjunct to mammography in the diagnosis and management of breast masses, but its role as a primary diagnostic tool is not fully established. When evaluating non-palpable breast lesions, Breast Imaging-Reporting and Data System (BI-RADS) lexicon based on Stavros sonographic criteria of US [1] is a validated method to identify probably benign masses, which can be managed with short interval follow-up. However, at many institutions, palpable breast masses often undergo biopsy despite likely benign US characteristics [2,3]. While tissue sampling can diagnose the rare malignancy among breast masses with probably benign features, the downsides of biopsy procedures are cost, patient anxiety, and potential risks, such as bleeding, infection and hematoma formation [4-7].
Young women usually undergo US alone in the diagnostic evaluation of a palpable breast mass [3,8-11]. Most solid palpable masses in young women are biopsied regardless of US features and despite a very low incidence of breast malignancy in this age group [2,3,9,12]. Recent studies demonstrated that US reliably identified probably benign palpable masses with a negative predictive value of 98.0% to 99.5% [2,3,12-14]. Given this high negative predictive value, investigation is needed to find more non-invasive management for these young women presenting with a palpable breast mass. Even in very high risk patients for breast cancer with BRCA mutation, the current guideline recommends screening imaging studies starting at age 25 given the low likelihood of earlier cancer development in these patients [15]. The purpose of this study was to correlate US features with histopathology of palpable solid breast masses in young women and to identify a subgroup for that follow-up is a safe alternative to the biopsy.
Materials and Methods
A Health Insurance Portability and Accountability Act (HIPAA) compliant, internal review board approved study was performed retrospectively investigating women 25 years or younger, who presented to our institution consecutively for a palpable concern and were found to have corresponding mass on US that underwent percutaneous US-guided core biopsy during the time period of 2002-2009. Informed consent was waived for each patient due to retrospective review nature of the study. We identified a total of 76 solid masses that underwent biopsy in 68 consecutive patients. We identified a total of 76 solid masses that underwent biopsy in 68 consecutive patients after excluding patients who were referred to our institution with known malignancy (3 patients), patients without a US correlate to the palpable concern (44 patients) and patients with corresponding benign findings including cysts (144 patients).
US examinations were performed using 8-15-MHz small-parts transducers (Acuson Sequoia 512, Siemens Healthcare, Malvern, PA, USA). The examinations targeted to the area of palpable concern by one of six specialized breast imaging radiologists with each of minimum of 3 years of experience. Corresponding solid masses were labeled with breast side, location (clock position), distance from the nipple and size. All 76 masses underwent ultrasound guided core biopsy using a spring loaded 14 gauge needle (Bard, Reusable or Disposable Core Biopsy Instrument, Tempe, AZ, USA) obtaining at least five core samples for each mass.
Two of the six breast imaging radiologists with 8 and 18 years of experience who were blinded to the clinical history and histopathology, independently re-evaluated the US images of the 76 benign masses retrospectively on a high resolution monitor. The updated BI-RADS lexicon was used to define the US features including shape (round/oval, lobular, and irregular), echogenic pattern (hyper, hypo, iso, and mixed-echogenic), orientation (parallel and anti-parallel), margins (circumscribed or non-circumscribedindistinct, micro-lobulated, angular, and spiculated), boundary (abrupt, halo) and posterior acoustic features (enhancement, shadowing, mixed, and none) (Table 1). The frequency of benign and malignant descriptor terms that were used to characterize the lesions was compared to the final pathology. Inter-observer agreement between the two readers was assessed for each US characteristic with Cohen’s kappa coefficient (>0.75, excellent; 0.40 to 0.75, fair to good; <0.40, poor) using a SYSTAT software (SPSS Inc., Chicago, IL, USA).
Table 1.
Frequency of ultrasonographic descriptors used for 76 benign masses by the two reviewers
| Characteristic | Radiologist 1 | Radiologist 2 |
|---|---|---|
| Shape | ||
| Round/oval | 48 (63.2) | 54 (71.1) |
| Irregular | 7 (9.2) | 10 (13.1) |
| Lobular | 21 (27.6) | 12 (15.8) |
| Margin | ||
| Circumscribed | 52 (68.4) | 59 (77.6) |
| Non-circumscribeda) | 24 (31.6) | 17 (22.4) |
| Indistinct | 14 (58.3) | 10 (58.8) |
| Angular | 5 (20.8) | 4 (23.5) |
| Micro-lobulated | 3 (12.5) | 2 (11.8) |
| Spiculated | 2 (8.3) | 1 (5.9) |
| Orientation | ||
| Parallel | 65 (85.5) | 69 (90.8) |
| Not parallel | 11 (14.5) | 7 (9.2) |
| Lesion boundary | ||
| Abrupt interface | 69 (90.8) | 71 (93.4) |
| Echogenic halo | 7 (9.2) | 5 (6.6) |
| Echo pattern | ||
| Hyperechoic | 1 (1.3) | 2 (2.6) |
| Mixed echogenic | 20 (26.3) | 17 (22.4) |
| Hypoechoic | 51 (67.1) | 54 (71.1) |
| Isoechoic | 4 (5.3) | 3 (3.9) |
| Posterior acoustic features | ||
| None | 58 (76.3) | 56 (73.7) |
| Shadowing | 4 (5.3) | 3 (3.9) |
| Enhancement | 14 (18.4) | 17 (22.4) |
Values are presented as number (%).
For non-circumscribed masses, four additional suspicious descriptors (indistinct, angular, micro-lobulated, and spiculated) were used.
Results
A total of 76 solid masses with a mean size of 1.9 cm based on US measurements (range 0.4 to 5.1 cm) were identified in 68 patients with a mean age of 21.8 years (range, 14 to 25 years). Sixty-two patients had a solitary mass, four patients had two masses, and two patients had three masses. All 76 solid masses yielded benign pathology on core biopsy and were interpreted to be concordant with the imaging findings: 19 fibroepithelial lesions, 54 fibroadenomas (2 juvenile fibroadenomas), 1 pseudoangiomatous stromal hyperplasia (PASH), and 2 stromal fibroses. Of 19 fibroepithelial lesions, 11 underwent surgical excision yielding three benign phyllodes tumors and 8 fibroadenomas. Forty-seven masses in 41 patients underwent additional follow-up ultrasound (mean, 22.9 months; range, 6 to 33 months). These 47 masses included stromal fibrosis, PASH, fibroepithelial lesions that did not undergo excision and fibroadenomas with one or more suspicious sonographic features. One patient with fibroepithelial lesion was lost to follow up. Two juvenile fibroadenomas underwent benign surgical excisions.
No malignancy was detected in any of the 76 solid masses found in 68 patients. The 76 benign masses were characterized by two reviewers (blinded regarding pathology) using the updated Stavros criteria (Table 1). On the US, the shape of the mass was described by radiologist 1 as oval or round (63.2%), margin as circumscribed (68.4%) and orientation as parallel (85.5%). By radiologist 2, the shape of the mass was described as oval or round (71.1%), margin as circumscribed (77.6%) and orientation as parallel (90.8%). The frequency of using all three benign descriptors was 61.8% by radiologist 1 and 68.5% by radiologist 2 (Fig. 1). All of these masses corresponded to benign fibroadenomas. Less frequently, suspicious descriptors were used. Suspicious descriptors were used less frequently by radiologist 1 including irregular shape (9.2%), noncircumscribed margin (31.6%), and non-parallel orientation (14.5%) and by radiologist 2 including irregular shape (13.1%), noncircumscribed margin (22.4%), and non-parallel orientation (9.2%). The frequency of using all three suspicious descriptors was 9.2% by radiologist 1 and 11.8% by radiologist 2 (Fig. 2). There showed good agreements for the shape, margin, echogenicity pattern and posterior acoustic features, and excellent agreements for the orientation and lesion boundary between the two readers (Table 2).
Fig. 1. A 23-year-old woman with left breast palpable concern.
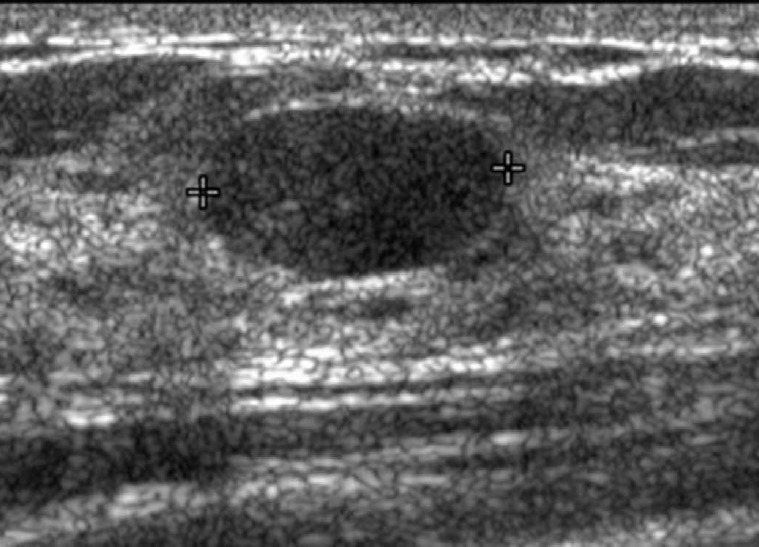
Ultrasonogram shows corresponding mass (between crosshairs) with characteristics described as “oval, circumscribed and parallel” by both radiologists. Biopsy yielded fibroadenoma.
Fig. 2. A 20-year-old woman with left breast palpable concern.
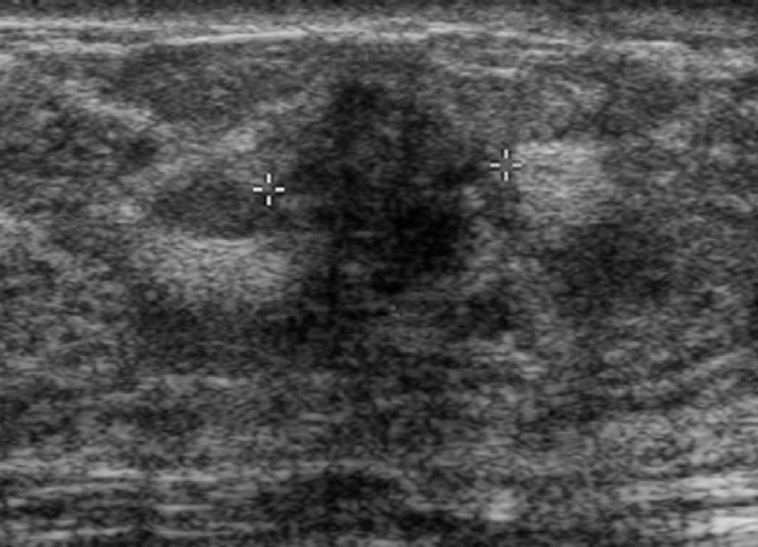
Ultrasonogram shows corresponding mass (between crosshairs) with characteristics described as “irregular, non-circumscribed and nonparallel” by both radiologists. Biopsy yielded stromal fibrosis.
Table 2.
Inter-observer agreement on ultrasonography characteristics
| Characteristic on ultrasonography | κa) (95% confidence interval) |
|---|---|
| Shape | 0.590 (0.311-0.870) |
| Margin | 0.679 (0.442—0.916) |
| Orientation | 0.812 (0.560-1.065) |
| Lesion boundary | 0.836 (0.614—1.057) |
| Echo pattern | 0.740 (0.569-0.911) |
| Posterior acoustic features | 0.684 (0.536—0.832) |
Kappa (κ) value greater than 0.75 is considered excellent agreement, 0.40 to 0.75 is fair to good and below 0.40 is poor (Fleiss’ guideline).
Discussion
In 1995, Stavros et al. [1] categorized US features into benign, intermediate, and malignant findings, in order to guide management of non-palpable breast lesions. Since then, several studies have emerged validating the utility of US evaluation of non-symptomatic breast lesions, allowing its incorporation into every breast imager's armamentarium [2,3,9,11-14]. While the role of US in the work-up of non-palpable breast masses is definite, its role when evaluating palpable masses remains unclear. Studies have emerged suggesting short-term follow-up for sonographically benign palpable breast masses [16,17]; however, the current paradigm is to biopsy all palpable masses, a practice based on the “triple-test” rule comprising physical examination, mammography and fine needle aspiration to decrease open surgical biopsies in women over 40 [18]. Despite advances in US technology and an increased understanding of breast cancer risk factors, many radiologists including our practice continue to biopsy all palpable masses, regardless of US features or risk factors, such as patient age [19].
Universal tissue sampling of palpable masses most negatively impacts young women. According to the National Cancer Institute, the age-specific incidence of invasive breast cancer in females less than 25 years old is 1.8 cases per 100,000 women per year [20] and in-situ breast cancer is 0.1 cases per 100,000 women per year [21]. The desire to diagnose malignancy early and to assuage doctor and patient anxiety creates an environment in which approximately 99% of biopsies of sonographically benign palpable masses in young women are negative [1,2,8]. Avoiding unnecessary biopsy in these low risk patients would provide multiple benefits including decreased post-procedural complications, decreased patient anxiety and decreased health care costs [4-7]. An additional potential implication to consider is the impact of early intervention on breast bud development of very young women.
The decision to biopsy a palpable mass in young women is usually based on the US findings. Mammography is not recommended due to radiation exposure [22] and limitations in interpretation due to dense breast tissue [19,23]. The American College of Radiology (ACR) Appropriateness Criteria [24] recommends US as the initial imaging tool in evaluating palpable breast masses in young women. Hence, this low risk group would benefit most from reliable US criteria to identify probably benign palpable breast masses and therefore decrease the number of avoidable biopsies. Recent studies demonstrate the utility and efficacy of US in evaluating palpable breast masses. Park et al. [2] examined 274 patients from 12 to 64 years old with palpable breast lesions, demonstrating probably benign morphology on US. After correlating with histopathologic results, they concluded that US has a negative predictive value of 99.4%. A study by Loving et al. [3] of 140 patients, younger than 30 with BI-RADS category 3 palpable masses, found no malignancy as confirmed by biopsy or 24-month imaging stability. They concluded that 100% sensitivity and negative predictive value of targeted US substantiates its use as an accurate primary imaging test, supporting US surveillance over biopsy in this patient population.
Our study result is consistent with the extremely low incidence of breast cancer in young women, with no malignancies detected in patients of this age group who presented with a palpable mass at our institution. All 76 palpable masses underwent benign tissue diagnosis by US-guided core biopsy. Using the BI-RADS lexicon, US would have accurately predicted benignity in more than 61.8% of our patients who had masses that demonstrated all three US characteristics of round or oval shape, circumscribed margin and parallel orientation highly correlated with benignity. These findings support that, in low risk young women, US features can adequately distinguish palpable masses for which conservative management with short-term US follow-up can be performed rather than invasive core needle biopsy.
Short-term imaging follow-up after a benign and concordant biopsy result is not routinely performed at our institution and is at the discretion of the radiologist performing the biopsy. In our study, 47 masses in 41 patients underwent additional follow-up US. These masses were recommended for imaging follow-up either due to the pathology result (stromal fibrosis, PASH, and fibroepithelial lesions) or due to demonstration of one or more suspicious US features. Four masses underwent subsequent benign surgical excision for demonstrating interval growth on follow-up US. No clear criteria are available to guide management after a benign and concordant biopsy result. In this age group, additional US follow-up may not be necessary given that the interval growth of these masses probably represents natural progression rather than missed cancer. More studies are needed to determine the appropriate follow-up guideline after benign biopsy in this population.
Our study has limitations. It is a single-site study with a small cohort of patients and not all 76 masses considered to be “benign” on core biopsy pathology had standardized US followup to ensure stability. In addition, selection bias may be present given retrospective nature of the study without a set management criteria for patients with a palpable concern. Additional studies are warranted to determine whether our results are generalizable to other practice settings.
In conclusion, despite the variable US features of palpable breast lesions, no malignancy was identified in our study, consistent with the extremely low incidence of breast malignancy in young women (25 years or younger). Using the BI-RADS lexicon, US would have accurately predicted benignity in about two thirds of our patients, supporting US surveillance as a safe alternative to invasive tissue sampling in this setting.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Stavros AT, Thickman D, Rapp CL, Dennis MA, Parker SH, Sisney GA. Solid breast nodules: use of sonography to distinguish between benign and malignant lesions. Radiology. 1995;196:123–134. doi: 10.1148/radiology.196.1.7784555. [DOI] [PubMed] [Google Scholar]
- 2.Park YM, Kim EK, Lee JH, Ryu JH, Han SS, Choi SJ, et al. Palpable breast masses with probably benign morphology at sonography: can biopsy be deferred? Acta Radiol. 2008;49:1104–1111. doi: 10.1080/02841850802438504. [DOI] [PubMed] [Google Scholar]
- 3.Loving VA, DeMartini WB, Eby PR, Gutierrez RL, Peacock S, Lehman CD. Targeted ultrasound in women younger than 30 years with focal breast signs or symptoms: outcomes analyses and management implications. AJR Am J Roentgenol. 2010;195:1472–1477. doi: 10.2214/AJR.10.4396. [DOI] [PubMed] [Google Scholar]
- 4.Kamath J, Cruess DG, Claffey K, Wilson L, Phoenix N, Tannenbaum S. Symptom distress associated with biopsy in women with suspect breast lesions. ISRN Oncol. 2012;2012:898327. doi: 10.5402/2012/898327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cassano E, Urban LA, Pizzamiglio M, Abbate F, Maisonneuve P, Renne G, et al. Ultrasound-guided vacuum-assisted core breast biopsy: experience with 406 cases. Breast Cancer Res Treat. 2007;102:103–110. doi: 10.1007/s10549-006-9305-x. [DOI] [PubMed] [Google Scholar]
- 6.Novy DM, Price M, Huynh PT, Schuetz A. Percutaneous core biopsy of the breast: correlates of anxiety. Acad Radiol. 2001;8:467–472. doi: 10.1016/S1076-6332(03)80617-7. [DOI] [PubMed] [Google Scholar]
- 7.Lee CI, Wells CJ, Bassett LW. Cost minimization analysis of ultrasound-guided diagnostic evaluation of probably benign breast lesions. Breast J. 2013;19:41–48. doi: 10.1111/tbj.12055. [DOI] [PubMed] [Google Scholar]
- 8.Smith GE, Burrows P. Ultrasound diagnosis of fibroadenoma: is biopsy always necessary? Clin Radiol. 2008;63:511–515. doi: 10.1016/j.crad.2007.10.015. [DOI] [PubMed] [Google Scholar]
- 9.Vade A, Lafita VS, Ward KA, Lim-Dunham JE, Bova D. Role of breast sonography in imaging of adolescents with palpable solid breast masses. AJR Am J Roentgenol. 2008;191:659–663. doi: 10.2214/AJR.07.3390. [DOI] [PubMed] [Google Scholar]
- 10.O'Neill AC, Shine S, Coffey L, Pender S, O'Doherty A, McNally S. Audit on breast ultrasound in women under 25 years. Ir J Med Sci. 2013;182:287–289. doi: 10.1007/s11845-012-0877-7. [DOI] [PubMed] [Google Scholar]
- 11.Harvey JA. Sonography of palpable breast masses. Semin Ultrasound CT MR. 2006;27:284–297. doi: 10.1053/j.sult.2006.05.003. [DOI] [PubMed] [Google Scholar]
- 12.Mainiero MB, Goldkamp A, Lazarus E, Livingston L, Koelliker SL, Schepps B, et al. Characterization of breast masses with sonography: can biopsy of some solid masses be deferred? J Ultrasound Med. 2005;24:161–167. doi: 10.7863/jum.2005.24.2.161. [DOI] [PubMed] [Google Scholar]
- 13.Graf O, Helbich TH, Hopf G, Graf C, Sickles EA. Probably benign breast masses at US: is follow-up an acceptable alternative to biopsy? Radiology. 2007;244:87–93. doi: 10.1148/radiol.2441060258. [DOI] [PubMed] [Google Scholar]
- 14.Skaane P, Engedal K. Analysis of sonographic features in the differentiation of fibroadenoma and invasive ductal carcinoma. AJR Am J Roentgenol. 1998;170:109–114. doi: 10.2214/ajr.170.1.9423610. [DOI] [PubMed] [Google Scholar]
- 15.Burke W, Daly M, Garber J, Botkin J, Kahn MJ, Lynch P, et al. Recommendations for follow-up care of individuals with an inherited predisposition to cancer. II. BRCA1 and BRCA2. Cancer Genetics Studies Consortium. JAMA. 1997;277:997–1003. [PubMed] [Google Scholar]
- 16.Harvey JA, Nicholson BT, Lorusso AP, Cohen MA, Bovbjerg VE. Short-term follow-up of palpable breast lesions with benign imaging features: evaluation of 375 lesions in 320 women. AJR Am J Roentgenol. 2009;193:1723–1730. doi: 10.2214/AJR.09.2811. [DOI] [PubMed] [Google Scholar]
- 17.Maxwell AJ, Pearson JM. Criteria for the safe avoidance of needle sampling in young women with solid breast masses. Clin Radiol. 2010;65:218–222. doi: 10.1016/j.crad.2009.11.009. [DOI] [PubMed] [Google Scholar]
- 18.Morris KT, Pommier RF, Morris A, Schmidt WA, Beagle G, Alexander PW, et al. Usefulness of the triple test score for palpable breast masses; discussion 1012-3. Arch Surg. 2001;136:1008–1012. doi: 10.1001/archsurg.136.9.1008. [DOI] [PubMed] [Google Scholar]
- 19.Foxcroft LM, Evans EB, Porter AJ. The diagnosis of breast cancer in women younger than 40. Breast. 2004;13:297–306. doi: 10.1016/j.breast.2004.02.012. [DOI] [PubMed] [Google Scholar]
- 20.National Cancer Institute . Age-specific SEER incidence rates, 2005-2009: invasive breast cancer. Rockville: National Cancer Institute; 2009. [Google Scholar]
- 21.National Cancer Institute . Age-specific SEER incidence rates, 2005-2009: in-situ breast cancer. Rockville: National Cancer Institute; 2009. [Google Scholar]
- 22.Williams SM, Kaplan PA, Petersen JC, Lieberman RP. Mammography in women under age 30: is there clinical benefit? Radiology. 1986;161:49–51. doi: 10.1148/radiology.161.1.3763885. [DOI] [PubMed] [Google Scholar]
- 23.Checka CM, Chun JE, Schnabel FR, Lee J, Toth H. The relationship of mammographic density and age: implications for breast cancer screening. AJR Am J Roentgenol. 2012;198:W292–W295. doi: 10.2214/AJR.10.6049. [DOI] [PubMed] [Google Scholar]
- 24.American College of Radiology . ACR appropriateness criteria: palpable breast masses. Reston: Americal College of Radiology; 2012. [Google Scholar]


