Abstract
Aims
To investigate the rates and risk of hospitalisations in patients with type 2 diabetes (T2D) mellitus in England.
Methods
This retrospective population-based cohort study used computerised records from the General Practice Research Database linked to Hospital Episode Statistics data in England. Patients with T2D from January 2006 to December 2010 were selected. Primary outcome measures were all-cause, non-diabetes-related, diabetes-related and hypoglycaemia-related hospitalisations. Factors associated with all-cause and diabetes-related hospitalisations were investigated with Cox's proportional hazards models.
Results
Amongst 97,689 patients with T2D, approximately 60% had at least one hospitalisation during the 4-year study period. Rates of hospitalisation were as follows: all-cause, 33.9 per 100 patient-years (pt-yrs); non-diabetes-related, 29.1 per 100 pt-yrs; diabetes-related, 18.8 per 100 pt-yrs and hypoglycaemia, 0.3 per 100 pt-yrs. The risk of all-cause hospitalisation increased with hospitalisation in the previous year, insulin use and the presence of major comorbidities. The risk of a diabetes-related hospitalisation increased with age, female gender, insulin use, chronic renal insufficiency, hypoglycaemia (as diagnosed by a general practitioner) and diabetes-related hospitalisation in the previous year.
Conclusions
Patients with T2D are hospitalised at a considerably high rate for causes directly related with diabetes complications and stay longer in hospital. History of hospitalisation and complications of diabetes were found to be predictive of inpatient hospitalisations suggesting previous hospitalisation episodes could serve as points of intervention. This study highlights important areas for healthcare intervention and provides a reminder for vigilance when risk factors for hospitalisation in patients with T2D are present.
What's known
The prevalence of diabetes among adults in the United Kingdom is high. Patients with type 2 diabetes (T2D) are at an increased risk of vascular complications, morbidity and mortality and are twice as likely to be admitted to hospital and experience prolonged stays, imposing a significant burden to the healthcare system. Previous studies that attempted to quantify hospitalisation rates amongst patients with T2D in England were limited to small and unrepresentative regional samples.
What's new
This study is the first to examine a cohort of nationally representative patients with T2D treated in primary care with data linked to hospital admission records in England. Results provide new important insight into the frequency and characteristics of hospitalisations amongst patients with T2D in England to help healthcare professionals improve the management of these patients and their quality of life; thus, contributing to decrease the burden to the National Health Service.
Introduction
Diabetes is a complex group of metabolic disorders associated with impaired insulin secretion and variable degrees of peripheral insulin resistance 1. A progressive condition, type 2 diabetes (T2D) is characterised by deficient insulin activity arising from decreased insulin secretion secondary to beta cell failure, compromised insulin action in peripheral target tissues, or a combination of these abnormalities. The prevalence of diabetes among adults in the United Kingdom (UK) is estimated to be 6.8% 2, of which 90% are estimated to be patients with T2D. A further million people are estimated to remain undiagnosed 3.
Poor glycaemic control, blood pressure, low-density lipoprotein and cholesterol control 4, as well as high body mass index (BMI) contribute to the high burden of T2D to the healthcare system. Patients with T2D are at an increased risk of vascular complications including cardiovascular (CV) morbidity and mortality 5–8, and are twice as likely to be admitted to hospital and experience prolonged inpatient stays 9–11. As a consequence of these complications, these patients are more than twice as costly to manage than those without diabetes 12. The direct cost is estimated to be around 7–12% of total annual National Health Service (NHS) expenditure in England 13,14; indirect societal and productivity costs have been estimated to be even higher 14,15.
Evidence has shown that tight glycaemic control (fasting blood glucose concentration less than 6 mmol/l) has an effect on reducing the risk of microvascular complications 16 and optimal patient management involves a challenging interplay of factors 17. For example, striving for ideal glycaemic control may result in episodes of hypoglycaemia, which may in turn have negative effects on medication adherence 18, while untreated severe hypoglycaemia can lead to inpatient hospital admissions 19, and in rare cases, brain damage and death.
Current NHS policy targets improving the management of chronic disease patients, including those with T2D, as an important strategy for improving health outcomes and controlling healthcare expenditure 20. Furthermore, identification of risk factors for hospitalisation of patients with T2D and patient subgroups who may be managed as outpatients is important in reducing healthcare costs. Previous studies have attempted to quantify hospitalisation rates amongst patients with T2D in England; however, conclusions were limited to small and unrepresentative samples in specific regions 21–23.
Accordingly, the aim of this study was to quantify the frequency of hospitalisation amongst patients with T2D in England and describe their characteristics. Specifically, the objectives were to estimate the rate of hospitalisations, report common primary causes and characteristics of hospitalisations, and to identify demographic, clinical and treatment-related factors associated with all-cause and diabetes-related hospitalisations amongst patients with T2D.
Methods
Data source
This retrospective cohort study utilised the linkage of the General Practice Research Database (GPRD) and the Hospital Episode Statistics (HES) data warehouse in England, being the first known diabetes study of this nature in the UK.
The GPRD1 24, managed by the MHRA, comprises diagnostic and prescription data of 5.2 million active patients from 640 practices which have passed quality control validation. These practices are considered to be broadly representative of the wider UK population 25.
The HES is a data source containing details of all admissions to NHS hospitals in England 26, including demographic data, dates of hospital admission, diagnoses and surgical procedures. Records are coded using a combination of International Statistical Classification of Disease and Related Health Problems (ICD-10) and Office of Population, Censuses and Surveys Classification of Surgical Operations and Procedure (OPCS4) codes for diagnoses and procedures, respectively.
At the time of the study, 56% of the 640 general practices within the GPRD had individual patient data anonymously linked to HES (KC, Personal Communication, GPRD). Linkages were performed using unique NHS number, date of birth, gender and postcode of residence, and contained information on admissions from 1 April 1997 through to 31 December 2011.
Cohort identification
We identified all active patients registered at GPRD practices, 18 years of age and over, with T2D diagnosed or treated during, or prior to, the study period (January 2006 to December 2010). We defined patients with T2D as either requiring: (i) a diagnosis of T2D or a prescription for an oral antidiabetic or glucagon-like peptide 1 (GLP-1) or (ii) a diagnosis of T2D and insulin using Read codes, a standardised clinical coding system used by general practitioners (GPs) in the UK 27 (Data S1). Patients were excluded if diagnosed with type 1 diabetes (T1D) mellitus, gestational diabetes, polycystic ovary syndrome, were pregnant at the start of or during the study period, did not have at least 1 day of follow-up in their medical record or if the practice where they received care did not meet data quality standards 24. The date of first diagnosis or prescription of anti-diabetic medication in the study period defined entry to the cohort. If patients were diagnosed or prescribed treatment prior to the study period, they were defined as ‘prevalent’ and entry to the study (index date) was set to 1 January 2006, the start of the study period. Follow-up was defined as time from study entry to the end of patient follow-up (last data collection date [December 2011], transfer out of the practice, end of HES record or death, whichever came first, allowing for the opportunity of at least 1 year, up to 5 years of follow-up). We restricted our study sample to patients from practices that had consented to linkage with HES records, if available, in accordance with the study objectives. No statistically significant differences in demographic and relevant clinical data were found between linked and non-linked patients (data not shown).
Outcome measures
The primary outcome of this study was hospital admission in the HES records. The primary reason for admission was identified by the responsible healthcare practitioner at the time of hospital admission and used to classify admission by type: (i) diabetes-related (including those related to hypoglycaemia) and (ii) non-diabetes-related. Classification of reason for admission as diabetes-related was based on a previously identified list of ICD-9 and OPCS4 codes as described by Donnan et al. 28, as appropriate, which included neurological, renal, endocrine/metabolic, ophthalmic and CV complications. Non-diabetes-related hospitalisations included all other reasons for hospitalisation not classified as diabetes-related. Hospitalisation admission rates were calculated overall and by age groups in 10-year bands. A sensitivity analysis was conducted amongst those who experienced a hypoglycaemia-related hospitalisation as either the primary, or ‘other’ cause of hospitalisation. Predictors of all-cause hospitalisations and diabetes-related hospitalisations were also examined.
Analysis
Survival analysis was used to calculate unadjusted rates of hospitalisation. All hospitalisation events during follow-up, defined as the period from study entry until end of follow-up or a hospital admission, were used. Patients who experienced more than one hospitalisation re-entered the study after the preceding hospitalisation event. To take account of the probability of repeated hospitalisation for the same patient, hospitalisation events were clustered by patient and hospitalisation type 29. Rates and 95% confidence intervals (CIs) were reported by age group and hospitalisation type.
Length of stay (LOS) and frequency of admission were calculated using summary statistics (mean, standard deviation [SD], median, interquartile ranges [IQR]) on all hospital events from a subsample of patients with at least 12 months of follow-up, excluding those with a missing discharge date. Same day admissions and discharges were counted as 1 day admissions.
To investigate potential risk factors associated with hospitalisation, a subgroup of prevalent patients was used, as the risk factors (due to disease severity and treatment patterns) for hospitalisation are likely to differ from newly diagnosed patients. Two groups of patients were analysed: (i) all prevalent patients, to investigate factors associated with all-cause hospitalisation and (ii) a subset of prevalent patients who had experienced at least one hospitalisation, to investigate factors associated with a diabetes-related hospitalisation. A set of demographic, clinical and laboratory variables based on previous studies were selected (a priori) as potential risk factors, as defined by clinical Read codes, and investigated for possible confounding effects, as appropriate, at the start of the study period. Percentages of missing data were reported. The first hospitalisation event in the study period was used for the analysis, and the type of event (i.e., diabetes vs. non-diabetes hospitalisation) determined categorisation of hospitalisation. Univariate analyses were conducted using χ2 tests for categorical variables and t-test/Wilcoxon rank sum tests for continuous variables. Multivariable Cox regression models were used to identify factors associated with a hospitalisation, and a backward stepwise selection process was used to identify the included covariates as those statistically significant at 95% level of confidence. Hazard ratios and 95% CIs were reported. The proportional hazard assumption was investigated by testing for a non-zero slope of the scaled Schoenfeld residuals on functions of time.
Analyses were performed using Stata/mp v.11 64bit software package (StataCorp LP, College Station, TX). The study was approved by the Independent Scientific Advisory Committee that provides advice to the MHRA on study design (ISAC protocol 11-072).
Results
Population demographics
We identified 97,689 patients with T2D and a HES-linked GPRD record; mean age 64.9 years, 54.4% male, mean BMI 30.8 kg/m2 (SD: 6.3, 20.3% missing). Clinical records from the 12 months prior to the study period indicated that 44.7% of patients had reasonably well-controlled levels of blood sugar (median HbA1c 7.1%; IQR: 6.4–8.1; 26.1% missing). Average total cholesterol was 149.8 mg/dl (SD: 39.9; 42.8% missing). Mean estimated glomerular filtration rate (eGFR) values were 68.3 ml/min (SD: 19.6; 9.9% missing). Overall 28,487 (29.2%) patients were ‘incident’ cases diagnosed during the study period. Of these patients, 23.6% received diabetes treatment at the time of diagnosis: biguanides (87.8%) or sulphonylureas (11.6%). The remaining 69,202 (70.8%) patients were prevalent (i.e., had been diagnosed prior to the study period). Amongst these patients, 69.0% were receiving drug treatment at the start of the study period: biguanides (69.2%), sulphonylureas (41.5%) and long/intermediate acting insulin (19.8%). Median time since T2D diagnosis for the prevalent patient group was 4.6 (IQR: 1.9–6.2) years at the start of the study period.
Rates of hospitalisation
The median follow-up duration per patient was 4.8 years (IQR: 2.9–4.9), which represented 763,292 patient-years (pt-yrs). During follow-up, 59.4% of patients had at least one hospitalisation (65.0% in the prevalent cohort; 45.8% in the incident cohort) accounting for a total of 258,383 hospitalisation admissions. The rates of hospitalisation were 33.9, 29.1, 18.8 and 0.3 per 100 pt-yrs for all-cause, non-diabetes-related, diabetes-related and hypoglycaemia related hospitalisations, respectively. Patients who were hospitalised due to causes unrelated to diabetes showed a higher rate of hospitalisation in younger age groups. This pattern was not seen in patients who were hospitalised for diabetes-related causes, where rates increased steadily with age (Figure1).
Figure 1.
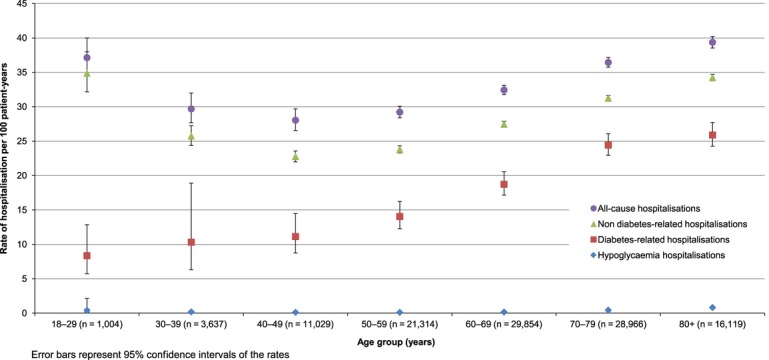
Hospitalisation rates per 100 patient-years amongst patients with T2D by age group. Error bars represent 95% confidence intervals of the rates
Reasons and characteristics of hospitalisation
The characteristics of hospitalisation by type of admission are summarised in Table1. The median LOS was 1 day (IQR: 1–4) as more than half of the hospitalisations (58.6%) were same day admissions and did not require an overnight stay. For episodes that required at least one overnight stay, median LOS was 6 days (IQR: 3–13) for diabetes-related hospitalisations and 5 days (IQR: 3–11) for non-diabetes-related hospitalisations.
Table 1.
Characteristics of hospitalisations by type of admission amongst patients with T2D with at least 12 months of follow-up
| Hospitalisation characteristics | All hospitalisations | Diabetes-related hospitalisations | Non-diabetes-related hospitalisations | |
|---|---|---|---|---|
| Number of patients* | 57,993 (100.00%) | 27,441 (47.32%) | 50,387 (86.88%) | |
| Number of hospitalisation events | n (%) | 257,826 (100.00%) | 97,759 (37.92%) | 160,067 (62.08%) |
| Length of stay† (days) for each event | Mean (SD) | 5.11 (12.40) | 4.19 (10.71) | 5.67 (13.30) |
| Median (min, max) | 1 (1, 673) | 1 (1, 372) | 1 (1, 673) | |
| IQ range | 1–4 | 1–2 | 1–5 | |
| Number of hospitalisation events with ≥ 1 overnight | n (%) | 106,797 (41.42%) | 29,460 (30.14%) | 77,337 (48.32%) |
| Length of stay (days) for events requiring ≥ 1 overnight | Mean (SD) | 10.93 (17.71) | 11.59 (17.39) | 10.67 (17.83) |
| Median (min, max) | 6 (2, 673) | 6 (2, 372) | 5 (2, 673) | |
| IQ range | 3–12 | 3–13 | 3–11 |
Patients may be included twice if they had a diabetes and non-diabetes-related hospitalisation.
Length of stay = 1 day for patients admitted and discharged on the same day.
Amongst hospitalisation events classified as diabetes-related, the most frequently occurring reasons were: renal failure (33.6%), hypertension (12.6%) and cataract (12.0%), which seldom required an overnight stay. For those who did, admissions due to renal failure had a mean LOS longer than the average diabetes-related episodes. Hypoglycaemia-related admissions accounted for 1.2% of diabetes-related admissions, and more than 80% required an overnight stay. For non-diabetes-related hospitalisations, the most frequently occurring reasons were: atherosclerotic heart disease (3.1%), anaemia (1.7%) and ‘unspecified’ illness (1.4%).
Factors associated with hospitalisation
Among prevalent patients with T2D in the cohort, 40,770 (62.0%) had at least one (all-cause) hospitalisation after the start of the study period and complete information for variables included in the Cox model. Of these, a subset of 20,706 (50.8%) patients had one or more diabetes-related hospitalisation(s) during follow-up. Key demographic features and comorbidities are summarised in Table2.
Table 2.
Patient characteristics at baseline amongst prevalent patients with T2D*
| Patients with T2D | All patients | No hospitalisation (post-index) | ≥ 1 All-cause hospitalisation (post-index) | ≥ 1 Diabetes-related hospitalisation* (post-index) | ≥ 1 Non-diabetes-related hospitalisation* (post-index) |
|---|---|---|---|---|---|
| Total patients, n (%) | 65,756 (100.0%) | 24,986 (38.0%) | 40,770 (62.0%) | 20,706 (50.8%) | 20,083 (49.2%) |
| Male, n (%) | 35,975 (54.7%) | 14,296 (57.2%) | 21,679 (53.2%) | 11,018 (53.2%) | 10,674 (53.2%) |
| Age, mean (SD) | 67.1 (12.7) | 64.5 (13.1) | 68.8 (12.2) | 70.8 (11.6) | 66.6 (12.5) |
| Years since T2D diagnosis, mean (SD) | 4.7 (3.4) | 4.4 (3.3) | 5.0 (3.6) | 5.4 (3.7) | 4.6 (3.3) |
| HbA1c value ≤ 6 months pre-index, mean (SD) | 7.4 (1.4) | 7.3 (1.4) | 7.4 (1.5) | 7.5 (1.5) | 7.3 (1.4) |
| BMI value ≤ 12 months pre-index, mean (SD), (kg/m2) | 30.2 (6.1) | 30.2 (6.1) | 30.2 (6.2) | 30.0 (6.0) | 30.5 (6.3) |
| eGFR, mean (SD), (ml/min) | 66.6 (19.8) | 69.4 (19.4) | 64.9 (19.8) | 62.0 (20.1) | 67.9 (19.0) |
| Hospitalisation in previous year, n (%) | 16,711 (25.4%) | 4208 (16.8%) | 12,503 (30.7%) | 7186 (34.7%) | 5325 (26.5%) |
| Insulin treatment, n (%) | 9603 (14.6%) | 2900 (11.6%) | 6703 (16.4%) | 4115 (19.9%) | 2597 (12.9%) |
| Sulphonylurea treatment, n (%) | 19,973 (30.4%) | 7143 (28.6%) | 12,830 (31.5%) | 6904 (33.3%) | 5933 (29.5%) |
| Peripheral circulatory disorder, n (%) | 5930 (9.0%) | 2115 (8.5%) | 3815 (9.4%) | 2063 (10.0%) | 1753 (8.7%) |
| Neurological complications, n (%) | 23,645 (36.0%) | 7340 (29.4%) | 16,305 (40.0%) | 9460 (45.7%) | 6851 (34.1%) |
| Cardiovascular complications, n (%) | 5470 (8.3%) | 1500 (6.0%) | 3970 (9.7%) | 2634 (12.7%) | 1343 (6.7%) |
| Cancer, n (%) | 6401 (9.7%) | 1782 (7.1%) | 4619 (11.3%) | 2425 (11.7%) | 2196 (10.9%) |
| Cerebrovascular complications, n (%) | 1295 (2.0%) | 401 (1.6%) | 894 (2.2%) | 558 (2.7%) | 336 (1.7%) |
| Endocrine/metabolic complications, n (%) | 3369 (5.1%) | 987 (4.0%) | 2382 (5.8%) | 1439 (7.0%) | 945 (4.7%) |
| Disorders of the liver, n (%) | 380 (0.6%) | 109 (0.4%) | 271 (0.7%) | 145 (0.7%) | 126 (0.6%) |
| Diabetes-related hospitalisation in previous year, n (%) | 6087 (9.3%) | 1472 (5.9%) | 4615 (11.3%) | 3128 (15.1%) | 1492 (7.4%) |
| Prior amputation, n (%) | 973 (1.5%) | 292 (1.2%) | 681 (1.7%) | 446 (2.2%) | 235 (1.2%) |
| Chronic renal insufficiency, n (%) | 1564 (2.4%) | 375 (1.5%) | 1189 (2.9%) | 874 (4.2%) | 316 (1.6%) |
| Hypoglycaemia (as reported by GP in previous year), n (%) | 3070 (4.7%) | 898 (3.6%) | 2172 (5.3%) | 1301 (6.3%) | 873 (4.4%) |
The number of patients in the first three columns corresponds to the complete cases used in the Cox regression analyses of all-cause vs. no hospitalisation; the latter two columns represent the complete cases used in the Cox regression analyses of diabetes vs. non-diabetes hospitalisation. Due to different variables included in the respective models, there is a difference in the patient count of 19 patients.
The results of the Cox regression analyses are presented in Tables3 and 4. For all-cause hospitalisation, hospitalisation in the previous year was the strongest predictor; these patients were almost twice as likely to experience a subsequent hospitalisation. Other factors associated with all-cause hospitalisation included insulin use, older age, male gender, higher HbA1c values and presence of major comorbidities, especially of the liver and kidney (as represented by the eGFR) (Table3). Factors associated with an increased risk of a diabetes-related compared with a non-diabetes-related hospitalisation are presented in Table4. A diabetes-related hospitalisation in previous year was the strongest predictor of subsequent diabetes-related hospitalisation. A diagnosis of chronic renal insufficiency or amputation on or prior to the start of the study and insulin use were also associated with a diabetes-related hospitalisation, as well as higher HbA1c values and previous diagnosis of hypoglycaemia.
Table 3.
Multivariable Cox regression analysis of all-cause hospitalisation (n = 40,770) vs. no hospitalisation (n = 24,986) amongst hospital episode statistics-linked patients (presented in decreasing magnitude of adjusted HR)
| Risk factors* | No. of events | Person-years at risk | Unadjusted HR (95% CI) | Adjusted HR (95% CI)† |
|---|---|---|---|---|
| Hospitalisation in previous year (yes vs. no) | 13,776 | 30,000 | 2.20 (2.15–2.24) | 1.91 (1.87–1.96) |
| Disorders of the liver (yes vs. no) | 294 | 782 | 1.53 (1.36–1.72) | 1.48 (1.31–1.67) |
| eGFR (ml/min) | ||||
| ≥ 60 | 23,987 | 110,000 | Reference | Reference |
| 31–59 | 15,398 | 51,000 | 1.41 (1.38–1.44) | 1.07 (1.05–1.10) |
| ≤ 30 | 1385 | 2400 | 2.52 (2.39–2.66) | 1.41 (1.33–1.49) |
| Cancer (yes vs. no) | 4986 | 13,000 | 1.61 (1.57–1.66) | 1.26 (1.22–1.30) |
| Cardiovascular complications (yes vs. no) | 4245 | 9400 | 1.87 (1.81–1.93) | 1.24 (1.19–1.28) |
| Insulin treatment (yes vs. no) | 7277 | 23,000 | 1.37 (1.34–1.41) | 1.23 (1.20–1.27) |
| Neurological complications (yes vs. no) | 17,372 | 56,000 | 1.46 (1.43–1.48) | 1.21 (1.19–1.23) |
| Cerebrovascular complications (yes vs. no) | 965 | 2800 | 1.42 (1.34–1.52) | 1.12 (1.04–1.19) |
| Endocrine/metabolic complications (yes vs. no) | 2594 | 7600 | 1.42 (1.37–1.48) | 1.12 (1.07–1.16) |
| Peripheral circulatory disorder (yes vs. no) | 4146 | 15,000 | 1.12 (1.09–1.16) | 1.08 (1.04–1.12) |
| Sulphonylurea treatment (yes vs. no) | 13,597 | 52,000 | 1.13 (1.10–1.15) | 1.05 (1.02–1.07) |
| Male gender | 21,679 | 92,550 | 1.11 (1.09–1.13) | 1.04 (1.02–1.07) |
| HbA1c (%) – 1 unit change | 40,770 | 165,761 | 1.02 (1.01–1.02) | 1.03 (1.02–1.04) |
| Age (year) – 1 year change | 40,770 | 165,761 | 1.02 (1.02–1.02) | 1.02 (1.02–1.02) |
| Time since diagnosis (years) – 1 year change | 40,770 | 165,761 | 1.04 (1.04–1.04) | 1.01 (1.01–1.01) |
A backwards stepwise selection process was used to identify significant covariates at the 95% level for addition to the multivariable model.
Adjusted for age, gender, eGFR values, HbA1c values, time since diagnosis, hospitalisation in the previous year, insulin treatment, sulphonylurea treatment, peripheral circulatory disorders, neurological complications, cardiovascular complications, cancer, cerebrovascular complications, renal complications, endocrine complications and liver disorders.
Table 4.
Multivariable Cox regression analysis of diabetes-related (n = 20,706) hospitalisations vs. non-diabetes-related (n = 20,083) hospitalisation
| Risk factors* | No. of events | Person-years at risk | Unadjusted HR (95% CI) | Adjusted HR (95% CI)† |
|---|---|---|---|---|
| Diabetes-related hospitalisation in previous year (yes vs. no) | 1301 | 10,700 | 2.03 (1.96–2.10) | 1.70 (1.63–1.76) |
| eGFR (ml/min) | ||||
| ≥ 60 | 10,841 | 82,000 | Reference | Reference |
| 31–59 | 8806 | 46,000 | 1.47 (1.43–1.52) | 1.17 (1.13–1.20) |
| ≤ 30 | 1059 | 2800 | 2.93 (2.75–3.12) | 1.71 (1.59–1.84) |
| Prior amputation (yes vs. no) | 446 | 1680 | 1.73 (1.58–1.89) | 1.38 (1.26–1.52) |
| Diagnosis of chronic renal insufficiency (yes vs. no) | 874 | 2540 | 2.29 (2.15–2.45) | 1.34 (1.25–1.45) |
| Insulin treatment (yes vs. no) | 4115 | 19,100 | 1.47 (1.42–1.51) | 1.26 (1.22–1.31) |
| Diagnosis of hypoglycaemia (yes vs. no) | 1301 | 6140 | 1.39 (1.32–1.47) | 1.09 (1.03–1.15) |
| HbA1c (%) – 1 unit change | 20,706 | 130,858 | 1.07 (1.06–1.08) | 1.08 (1.07–1.09) |
| Age (year) – 1 unit change | 20,706 | 130,858 | 1.03 (1.02–1.03) | 1.02 (1.02–1.02) |
| Time since diagnosis (years) – 1 unit change | 20,706 | 130,858 | 1.05 (1.04–1.05) | 1.02 (1.01–1.02) |
| Male gender | 11,018 | 69,580 | 0.99 (0.96–1.01) | 0.93 (0.91–0.96) |
A backwards stepwise selection process was used to identify significant covariates at the 95% level for addition to the multivariable model.
Adjusted for age, gender, time since diagnosis, eGFR value, prior diabetes-related hospitalisation, prior amputation, chronic renal insufficiency, insulin treatment and diagnosis of hypoglycaemia.
Discussion
The rates of all-cause, non-diabetes-related and diabetes-related hospitalisations amongst patients with T2D in England represent a significant burden to the NHS 13,30. Approximately half the hospitalisation events observed in this study were day admissions. For those requiring at least one overnight stay, LOS was higher for diabetes-related admissions. The most frequent diabetes-related hospitalisations were related to renal failure, hypertension and cataract; whilst for non-diabetes-related hospitalisations atherosclerotic heart disease, anaemia and ‘unspecified’ illness were most frequently reported. Factors associated with all-cause hospitalisation included hospitalisation in the previous year, low eGFR, insulin use and presence of major comorbidities. Although men were more likely to be hospitalised, women were more likely to be hospitalised for a diabetes-related cause. The risk of a diabetes-related hospitalisation was found to increase with insulin use, age, presence of chronic renal insufficiency, hypoglycaemia (as diagnosed by a GP) and diabetes-related hospitalisation in the previous year.
Comparison with previous literature
In the current study, the observed rate for all-cause hospitalisations amongst patients with T2D (33.8 per 100 pt yrs) was higher than estimated from most previous reports. Rates of 24.2% and 27.1% per year were reported in patients from the Italian region of Turin 31 and from Tayside, Scotland 28 additionally, rates of 31.5% and 50.7% were found in a 4-year follow-up study in England 21 and over 3-year follow-up in Finland 32, respectively. However, these studies included limited populations restricted to a specific geographic location, age group or specific anti-diabetic treatment.
Furthermore, the rate of a diabetes-related hospitalisation in the current study was higher than an Italian study of patients with both T1D and T2D which reported a proportion of 23.9% per year 33. Direct comparison is difficult, as definitions of hospitalisations due to diabetes-related complications and healthcare settings that may influence inpatient admissions are variable across studies and countries. This study included a broad range of diabetes patients at various stages of disease progression and severity, and included day admissions as collected from hospital records, in contrast with previous reports.
The rate of hospitalisation related to hypoglycaemia reported was lower than found in previous studies 19,34,35. This may be due to our methodology, limiting the cause of admission to the primary diagnosis, or the possibility of misclassification of hypoglycaemia admissions. Service 36 reported that hypoglycaemia has numerous causes including severe systemic illness, advanced malnutrition, various medication use, malignancy and frailty. If recorded in place of hypoglycaemia as the primary cause for hospital admission, such cases would not be included in the estimated rate. Previous studies reporting higher prevalence of hypoglycaemia-related admissions verified the occurrence of hypoglycaemia with additional information from the clinical records 21,34, while others have used discharge data rather than admission data 37. To test the sensitivity of our estimate, the rate of hypoglycaemia-related admission was calculated when hypoglycaemia was recorded either as the primary, or ‘other’ cause of hospitalisation. This doubled the rate from 0.30 to 0.62 per 100 pt-yrs. This remains lower than that seen in other studies focussing on insulin or sulphonylurea use, which are known to be predictors of severe hypoglycaemia 19,34,37–39, in patients with T2D. In our study, both incident and prevalent patients were included, and only 14.6% and 30.4% were being treated with insulin and sulphonylureas (with or without insulin), respectively. For treated patients, both insulin treatment and sulphonylurea use were significantly associated with all-cause hospitalisation. Insulin treatment was also significantly associated with diabetes-related hospitalisations.
Median duration of hospitalisation with an overnight stay was found to be 6 days for diabetes, and 5 days for non-diabetes-related admissions in England. These results are within estimates reported from comparable countries ranging from 4.9 to 10.7 days (average of 8 days), and higher than those found for non-diabetic patients 28,40–42. However, LOS is likely to be influenced by country-specific healthcare systems and coverage.
Previous studies reporting risk factors associated with hospitalisation amongst patients with T2D have reported conflicting results 21,43–45. We found insulin treatment to be predictive of both all-cause hospitalisations and diabetes-related hospitalisations, perhaps indicating increased duration and severity of disease; a finding supported by a United States claims database study and an Italian study utilising hospital admission data 19,31. Moss et al. found HbA1c level to be the strongest predictive risk factor for hospitalisations; however pre-existing chronic conditions were not evaluated 21. Similar to results of the current study, previous studies have reported chronic complications and severe comorbidities of T2D to increase risk of hospitalisation 44,46. The presence of major comorbidities as risk factors for hospitalisation further highlight the need to implement preventative strategies as recently indicated by NICE public health guidance 38, which encourage providers of public health services to perform risk assessments in higher risk population groups and match interventions to risks identified 47. Disproportionate use of healthcare resources, often as a consequence of the heavy burden of comorbidities, has been reported in previous studies of patients with diabetes 48,49. Therefore, reduction of diabetes-related complications in patients plays an important role in reducing the cost of hospital admissions by shortening and/or decreasing the frequency of hospital stays 50.
Strengths and limitations of results
This is the first study examining a cohort of nationally representative patents with T2D, treated in primary care with data linked to hospital admission records in England. Our study of observational data in general practice allows assessment of risk factors associated with hospitalisation in a UK primary care setting, given management of patients with T2D in the UK differs from management in some other countries 31.
Diagnostic coding for diabetes within GPRD is reliable with a high positive predictive value, likely owing to Quality Outcomes Framework guidelines introduced in 2004, where GPs are incentivised to keep accurate and updated clinical records for patients with specific conditions, including diabetes 30,51. Therefore, our data are likely to be more reliable and complete than other studies conducted in primary care before this period.
Hospital admissions were classified as diabetes-related according to a pre-specified list of reasons for hospital admission 28. It is possible that some of the conditions listed as non-diabetes-related, such as atherosclerotic heart disease, are in fact a complication resulting from diabetes. Similarly, some hospital admission reasons like hypertension, which may be independent of diabetes, were not classified as such in this study. These two factors have opposite effects in the true estimation of the diabetes-related hospitalisation rate. As we were unable to further investigate the timing of the original diagnoses, and information gathered was limited to reason for hospital admission, it was not possible to determine whether hospital admission was due to a condition predating diabetes diagnosis, or that developed as a result of the condition.
We acknowledge that within the GPRD, HES linkage is approximately 50% complete within England and potential differences in linked compared to non-linked populations could limit generalisability of our findings. To this end, we compared non-linked patients with T2D to the linked cohort and no important differences in demographic and clinical characteristics were found, suggesting that no systematic difference in data from the HES-linked and non-linked practices exist within our cohort of patients.
Conclusions
Patients with T2D are hospitalised at a considerably high rate for causes directly related to diabetes complications and stay longer in hospital, posing a significant burden to healthcare systems. The most common primary reasons for a diabetes-related admission are associated with renal failure, CV disease and development of cataract. This study investigated risk factors for inpatient admissions amongst patients with T2D, adding important knowledge of risk factors associated with these events in England. Previous hospitalisations and the existence of comorbidities were found to be significant predictors of inpatient hospitalisations.
As hospitalisations are both costly and can have a significant impact on a patient's quality of life, appropriate risk management plans should be developed to prevent or appropriately manage serious complications associated with diabetes. Reduction of these diabetes-related complications would reduce direct health cost by decreasing the frequency of hospital stays. Furthermore, admissions to hospital related to diabetes may be indicative of patients with a higher disease burden and, therefore, should serve as points of intervention.
Acknowledgments
This study was funded by Eli Lilly and Company. The team members reviewed and approved the study design, provided access to data, reviewed all results and manuscript development and participated in the publication decisions.
Footnotes
Since 1 April 2012, the Clinical Practice Research Datalink (CPRD) combines the resources of the GPRD and the Research Capability Programme piloted over the last 4 years by the National Institute for Health Research (NIHR). CPRD is hosted and managed by the Medicines and Healthcare Products Regulatory Agency (MHRA).
Authors’ contributions
JMK, AM, MR and KSB contributed to conception and design of the study and acquisition of data; JMK and MRC contributed to data analysis. All authors contributed to interpretation of data and drafting the article or reviewing and revising it critically for important intellectual content; all authors approved the final version to be published. JMK attests that the authors had access to all the study data, takes responsibility for the accuracy of the analysis, and had authority over manuscript preparation and the decision to submit the manuscript for publication.
Supporting Information
Additional Supporting Information may be found in the online version of this article
Read code list.
References
- 1.Kasper D, Braunwald E, Hauser S, et al. Harrison's Principles of Internal Medicine. 16. New York: McGraw-Hill Professional Publishers; 2004. [Google Scholar]
- 2.Whiting DR, Guariguata L, Weil C, et al. Diabetes Research and clinical practice IDF Diabetes Atlas: International Diabetes Federation, Brussels. Australia; Belgium: Baker IDI Heart and Diabetes Institute; 2011. [Google Scholar]
- 3. Diabetes in the UK (April 2012) – Diabetes UK http://www.diabetes.org.uk/Professionals/Publications-reports-and-resources/Reports-statistics-and-case-studies/Reports/Diabetes-in-the-UK-2012/ (accessed 29 June 2012)
- 4.American Diabetes Association. Standards of medical care in diabetes–2012. Diabetes Care. 2012;35(Suppl. 1):S11–63. doi: 10.2337/dc12-s011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.The Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. The Diabetes Control and Complications Trial Research Group. N Engl J Med. 1993;329:977–86. doi: 10.1056/NEJM199309303291401. [DOI] [PubMed] [Google Scholar]
- 6.UKPDS group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) Group. Lancet. 1998;352:837–53. [PubMed] [Google Scholar]
- 7.Gaede P, Vedel P, Larsen N, et al. Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes. N Engl J Med. 2003;348:383–93. doi: 10.1056/NEJMoa021778. [DOI] [PubMed] [Google Scholar]
- 8.Shichiri M, Kishikawa H, Ohkubo Y, et al. Long-term results of the Kumamoto Study on optimal diabetes control in type 2 diabetic patients. Diabetes Care. 2000;23(Suppl. 2):B21–9. [PubMed] [Google Scholar]
- 9.Srinivasan BT, Jarvis J, Khunti K, et al. Recent advances in the management of type 2 diabetes mellitus: a review. Postgrad Med J. 2008;84:524–31. doi: 10.1136/pgmj.2008.067918. [DOI] [PubMed] [Google Scholar]
- 10.Dawson KG, Gomes D, Gerstein H, et al. The economic cost of diabetes in Canada, 1998. Diabetes Care. 2002;25:1303–7. doi: 10.2337/diacare.25.8.1303. [DOI] [PubMed] [Google Scholar]
- 11.Simpson SH, Corabian P, Jacobs P, et al. The cost of major comorbidity in people with diabetes mellitus. CMAJ. 2003;168:1661–7. [PMC free article] [PubMed] [Google Scholar]
- 12.Zimmet P. The burden of type 2 diabetes: are we doing enough? Diabetes Metab. 2003;29:6S9–18. doi: 10.1016/S1262-3636(03)72783-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.National Collaborating Centre for Chronic Conditions (UK) Type 2 Diabetes: National Clinical Guideline for Management in Primary and Secondary Care. London: Royal College of Physicians; 2008. [PubMed] [Google Scholar]
- 14.Holmes J, Gear E, Bottomley J, et al. Do people with type 2 diabetes and their carers lose income? (T2ARDIS-4) Health Policy. 2003;64:291–6. doi: 10.1016/s0168-8510(02)00177-x. [DOI] [PubMed] [Google Scholar]
- 15.Hex N, Bartlett C, Wright D, et al. Estimating the current and future costs of type 1 and type 2 diabetes in the UK, including direct health costs and indirect societal and productivity costs. Diabet Med. 2012;29:855–62. doi: 10.1111/j.1464-5491.2012.03698.x. [DOI] [PubMed] [Google Scholar]
- 16.Holman RR, Paul SK, Bethel MA, et al. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med. 2008;359:1577–89. doi: 10.1056/NEJMoa0806470. [DOI] [PubMed] [Google Scholar]
- 17.Pouwer F, Hermanns N. Insulin therapy and quality of life. A review. Diabetes Metab Res Rev. 2009;25(Suppl. 1):S4–10. doi: 10.1002/dmrr.981. [DOI] [PubMed] [Google Scholar]
- 18.Odegard PS, Capoccia K. Medication taking and diabetes: a systematic review of the literature. Diabetes Educ. 2007;33:1014–29. doi: 10.1177/0145721707308407. ; discussion 30-1. [DOI] [PubMed] [Google Scholar]
- 19.Quilliam BJ, Simeone JC, Ozbay AB. Risk factors for hypoglycemia-related hospitalization in patients with type 2 diabetes: a nested case-control study. Clin Ther. 2011;33:1781–91. doi: 10.1016/j.clinthera.2011.09.020. [DOI] [PubMed] [Google Scholar]
- 20.Department of Health. Supporting people and integration with long term conditions: an NHS and Social Care Model to support local innovation http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_4122574.pdf (accessed 20 June, 2012)
- 21.Moss SE, Klein R, Klein BE. Risk factors for hospitalization in people with diabetes. Arch Intern Med. 1999;159:2053–7. doi: 10.1001/archinte.159.17.2053. [DOI] [PubMed] [Google Scholar]
- 22.Simmons D, Wenzel H. Diabetes inpatients: a case of lose, lose, lose. Is it time to use a ‘diabetes-attributable hospitalization cost’ to assess the impact of diabetes? Diabet Med. 2011;28:1123–30. doi: 10.1111/j.1464-5491.2011.03295.x. [DOI] [PubMed] [Google Scholar]
- 23.Williams DR, Anthony P, Young RJ, et al. Interpreting hospital admissions data across the Korner divide: the example of diabetes in the north western region. Diabet Med. 1994;11:166–9. doi: 10.1111/j.1464-5491.1994.tb02014.x. [DOI] [PubMed] [Google Scholar]
- 24.Clinical Practice Research Datalink (CPRD) http://www.cprd.com/intro.asp (accessed 20 June, 2012)
- 25.Lawrenson R, Williams T, Farmer R. Clinical information for research; the use of general practice databases. J Public Health Med. 1999;21:299–304. doi: 10.1093/pubmed/21.3.299. [DOI] [PubMed] [Google Scholar]
- 26. Hospital episode statistics http://www.hesonline.nhs.uk (accessed 14 May, 2012)
- 27.Benson T. The history of the Read Codes: the inaugural James Read Memorial Lecture 2011. Inform Prim Care. 2011;19:173–82. doi: 10.14236/jhi.v19i3.811. [DOI] [PubMed] [Google Scholar]
- 28.Donnan PT, Leese GP, Morris AD, et al. Hospitalizations for people with type 1 and type 2 diabetes compared with the nondiabetic population of Tayside, Scotland: a retrospective cohort study of resource use. Diabetes Care. 2000;23:1774–9. doi: 10.2337/diacare.23.12.1774. [DOI] [PubMed] [Google Scholar]
- 29.Cleves M, Gould W, Gutierrez RG, et al. An Introduction to Survival Analysis Using Stata. 3rd edn. College Station, TX: Stata Press; 2010. [Google Scholar]
- 30.Department of Health. Quality and Outcomes Framework (QOF) http://webarchive.nationalarchives.gov.uk/+/www.dh.gov.uk/en/Healthcare/Primarycare/Primarycarecontracting/QOF/index.htm (accessed 20 June, 2012)
- 31.Bo S, Ciccone G, Grassi G, et al. Patients with type 2 diabetes had higher rates of hospitalization than the general population. J Clin Epidemiol. 2004;57:1196–201. doi: 10.1016/j.jclinepi.2004.02.015. [DOI] [PubMed] [Google Scholar]
- 32.Aro S, Kangas T, Reunanen A, et al. Hospital use among diabetic patients and the general population. Diabetes Care. 1994;17:1320–9. doi: 10.2337/diacare.17.11.1320. [DOI] [PubMed] [Google Scholar]
- 33.De Berardis G, D'Ettorre A, Graziano G, et al. The burden of hospitalization related to diabetes mellitus: a population-based study. Nutri Metab Cardiovasc Dis. 2012;22:605–12. doi: 10.1016/j.numecd.2010.10.016. [DOI] [PubMed] [Google Scholar]
- 34.Davis TM, Brown SG, Jacobs IG, et al. Determinants of severe hypoglycemia complicating type 2 diabetes: the Fremantle diabetes study. J Clin Endocrinol Metab. 2010;95:2240–7. doi: 10.1210/jc.2009-2828. [DOI] [PubMed] [Google Scholar]
- 35.Asuncion MM, Shaheen M, Ganesan K, et al. Increase in hypoglycemic admissions: California hospital discharge data. Ethn Dis. 2007;17:536–40. [PubMed] [Google Scholar]
- 36.Service FJ. Hypoglycemic disorders. N Engl J Med. 1995;332:1144–52. doi: 10.1056/NEJM199504273321707. [DOI] [PubMed] [Google Scholar]
- 37.Schejter YD, Turvall E, Ackerman Z. Characteristics of patients with sulphonurea-induced hypoglycemia. J Am Med Dir Assoc. 2012;13:234–8. doi: 10.1016/j.jamda.2010.07.014. [DOI] [PubMed] [Google Scholar]
- 38.Mäkimattila S, Korhonen P, Haukka J, et al. 2012. Type of insulin and age are predictors of hospitalization due to severe hypoglycemia: the EpiHypo Study Berlin, Germany European Association for the Study of Diabetes (EASD)
- 39.van Staa T, Abenhaim L, Monette J. Rates of hypoglycemia in users of sulfonylureas. J Clin Epidemiol. 1997;50:735–41. doi: 10.1016/s0895-4356(97)00024-3. [DOI] [PubMed] [Google Scholar]
- 40.Ray NF, Thamer M, Taylor T, et al. Hospitalization and expenditures for the treatment of general medical conditions among the U.S. diabetic population in 1991. J Clin Endocrinol Metab. 1996;81:3671–9. doi: 10.1210/jcem.81.10.8855821. [DOI] [PubMed] [Google Scholar]
- 41.Aro S, Koivisto VA, Reunanen A, et al. Influence of morbidity and health care structure on hospitalization among adult diabetic patients. Diabet Med. 1996;13:376–81. doi: 10.1002/(SICI)1096-9136(199604)13:4<376::AID-DIA70>3.0.CO;2-2. [DOI] [PubMed] [Google Scholar]
- 42.Lee CH, Tey BH, Chew W. Epidemiology of diabetes mellitus in a regional hospital medical unit. Ann Acad Med Singapore. 1993;22:864–9. [PubMed] [Google Scholar]
- 43.Rosenthal MJ, Fajardo M, Gilmore S, et al. Hospitalization and mortality of diabetes in older adults. A 3-year prospective study. Diabetes Care. 1998;21:231–5. doi: 10.2337/diacare.21.2.231. [DOI] [PubMed] [Google Scholar]
- 44.Panser LA, Naessens JM, Nobrega FT, et al. Utilization trends and risk factors for hospitalization in diabetes mellitus. Mayo Clin Proc. 1990;65:1171–84. doi: 10.1016/s0025-6196(12)62741-4. [DOI] [PubMed] [Google Scholar]
- 45.Goyder E, Spiers N, McNally P, et al. Do diabetes clinic attendees stay out of hospital? A matched case-control study. Diabet Med. 1999;16:687–91. doi: 10.1046/j.1464-5491.1999.00100.x. [DOI] [PubMed] [Google Scholar]
- 46.Roesler J, Bishop D, Walseth J. Economic cost of diabetes mellitus – Minnesota, 1988. MMWR Morb Mortal Wkly Rep. 1991;40:229–31. [PubMed] [Google Scholar]
- 47.NICE. Preventing type 2 diabetes: risk identification and interventions for individuals at high risk. Issued: July 2012, NICE public health guidance 38.
- 48.Guo JJ, Gibson JT, Gropper DM, et al. Empiric investigation on direct costs-of-illness and healthcare utilization of Medicaid patients with diabetes mellitus. Am J Manag Care. 1998;4:1433–46. [PubMed] [Google Scholar]
- 49.Ashton CM, Septimus J, Petersen NJ, et al. Healthcare use by veterans treated for diabetes mellitus in the Veterans Affairs medical care system. Am J Manag Care. 2003;9:145–50. [PubMed] [Google Scholar]
- 50.Gray A, Raikou M, McGuire A, et al. Cost effectiveness of an intensive blood glucose control policy in patients with type 2 diabetes: economic analysis alongside randomised controlled trial (UKPDS 41). United Kingdom Prospective Diabetes Study Group. BMJ. 2000;320:1373–8. doi: 10.1136/bmj.320.7246.1373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Khan NF, Harrison SE, Rose PW. Validity of diagnostic coding within the General Practice Research Database: a systematic review. Br J Gen Pract. 2010;60:e128–36. doi: 10.3399/bjgp10X483562. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Read code list.


