Abstract
Objectives
We have previously reported that a multifaith spiritually based intervention (SBI) may have efficacy in the treatment of generalized anxiety disorder (GAD). This randomized pilot trial tested whether the SBI had greater efficacy than a nonspecific control condition in GAD.
Method
Twenty-three participants with GAD of at least moderate severity were randomized to 12 individual sessions of the SBI (n = 11) or supportive psychotherapy (SP)—our control condition (n = 12).
Results
Intent-to-treat analysis revealed the SBI fared better than SP in decreasing blind clinician ratings of anxiety and illness severity and self-report worry and intolerance of uncertainty, with large between-group effect sizes. The SBI also produced greater changes in spiritual well-being. Results remained the same when supplementary analyses were performed on the completer sample. Treatment gains were maintained at 3-months follow-up.
Conclusions
This small pilot trial demonstrates that a nondenominational SBI has greater efficacy than a rigorous control in improving symptoms of GAD and enhancing spiritual well-being. These results are encouraging and further research on the efficacy of the SBI and its underlying mechanisms is warranted.
Keywords: spirituality, religion, psychotherapy, spiritual psychotherapy, anxiety, generalized anxiety disorder, randomized controlled trial
Much attention has been paid to the relationship between positive mental health, religion, and spirituality in recent decades. Although not all studies agree (e.g., King, Marston, McManus, Brugha, Meltzer, & Beggington, 2013; Laurent et al., 2013; Schuurmans-Stekhoven, 2010) and a causal relationship has not been established (Miller & Thoreson, 2003), on average, cross-sectional and prospective studies with community and clinical samples have linked religious and spiritual beliefs and practices to mental well-being across the lifespan (Baetz, Bowen, Jones, & Koru-Sengul, 2006; Bonelli & Koenig, 2013; Koenig & Larson 2001; Levin 1996; Sternthal, Williams, Muscik, & Buck, 2010), better perceived quality of life (Lucchetti et al., 2011), reduced psychological distress in response to negative life events (Koenig, 2009; McCaffrey, Eisenbert, Legedza, Davis, & Phillips, 2004; Pargament, 1997), better adjustment and mental health outcomes following exposure to trauma (Ahrens, Abeling, Ahmad, & Hinman, 2010; Connor, Davidson, & Lee, 2003; McIntosh, Poulin, Silver, & Holman, 2011), and shorter hospital stays and recovery in individuals with psychiatric problems (Leamy, Bird, LeBoutillier, Williams, & Slade, 2011; Koenig, 2008; Webb, Charbonneau, McCann, Gayle, & Kristin, 2011).
Although these and other studies published in the last two decades have found a generally positive effect of religious and spiritual activities on mental health (Bonelli & Koenig, 2013), the religion–mental health connection has been a source of controversy (Sloan, Bagiella, & Powell, 1999), and research has been criticized for relying on correlational and cross-sectional designs, using unrepresentative samples, employing diverse definitions and measure of religion and spirituality and not adequately controlling for potential confounders (Dien, Cook, & Koenig, 2012).
In contrast to the large literature linking religion and spirituality with positive mental health outcomes, there is a relative lack of research on underlying mechanisms. Existing studies have produced ambiguous findings and research in this area is complicated by the lack of consensus on how to best conceptualize and measure the distinct yet overlapping constructs of religion and spirituality (Hall, Meador, & Koenig, 2008; King & Koenig, 2009; Shreve-Neiger & Edelstein, 2004). Despite these limitations, available data have generated several explanatory models of how religion, spirituality, and psychological well-being may be functionally connected. These include social pathways (e.g. social connectedness, compassion towards others), cognitive pathways (e.g., providing a sense of purpose and meaning in life and framework for making sense of the world), behavioral pathways (e.g. avoidance of high risk behaviors), and biological pathways including changes in neurobiological, neurohormonal, neuroimmunologic, and cardiovascular functioning (Baetz & Toews, 2009; Levin, 2010; Rosmarin, Wachholtz, & Ai, 2011; Seybold, 2007). While available research offers important insights into how religion and spirituality may contribute to positive mental health outcomes, little is known about how these diverse mechanisms interact.
An outgrowth of research on the generally positive effects of religious or spiritual beliefs and practices on psychological well-being has been the incorporation of spirituality in mental health care. Until recently, religion and spirituality were largely ignored in clinical practice and even considered by some prominent figures in psychiatry and psychology to be detrimental to psychological health (Plante, 2008). Although certain religious beliefs and practices can contribute to psychopathology (Ano & Vasconcelles, 2004; Koenig, 2009; Pargament, Koenig, Tarakeshwar, & Hahn, 2004; Shreve-Neiger & Edelstein, 2004; Sternthal et al., 2010), the documented salutary effect of religion and spirituality on mental health–coupled by findings that religious and spiritual beliefs and practices are widespread in the general population (Koenig, 2009), that many individuals turn to religion to cope with adversity and daily difficulties and frustrations (Koneig 2009; Pargament et al., 2004; Pargament, 1997; Tepper, Rogers, Coleman, & Malony, 2001; Wacholtz & Sambamoorthi, 2011), and that patients increasingly desire spiritually integrated care (Baetz, Griffin, Bowen, & Marcoux, 2004; Lake, Helgason, & Sarris, 2012; Post & Wade, 2009)–has shifted clinicians’ perspective on the relevance of religious and spiritual issues and experiences in their patients’ lives (Koenig, 2009; Plante, 2007).
In addition to engaging in a dialogue with patients on faith, religion, spirituality, and mental well-being, there has been a trend for some mental health practitioners to employ a range of practices derived from religious and spiritual traditions as an adjunct to mainstream psychotherapies or as a stand-alone intervention. The most well-known example is mindfulness training, which has been secularized and integrated into a number of efficacious therapies without reference to Buddhist teachings and philosophy (Marchand, 2012). There has also been growing interest in evaluating therapies that explicitly integrate religious and spiritual practices and teachings. For example, interventions that blend faith-based principles and practices with cognitive-behavioral therapy (CBT) have been found to be effective in treating a number of psychological problems in religious patients (Propst, Ostrom, Watkins, Dean, & Mashburn, 1992; Propst, 1980; Worthington, Hook, Davis, & McDaniel, 2011; Xiao, Young, & Zhang, 1998). Religious CBT for depression has the most evidence and meets criteria for an empirically validated treatment (Hodge, 2006).
Despite promising findings (Hook et al., 2010; Smith, Bartz, & Scott Richards, 2007; Worthington et al., 2011), the evidence base for spiritually focused interventions for psychiatric disorders is sparse and existing studies have been criticized for lack of scientific rigor. Further, much of the research has been conducted with devout patients affiliated with a specific religious community or medically ill patients who experience psychological distress but who do not necessarily meet criteria for an Axis I psychiatric disorder, limiting generalizability of findings. More outcome research is needed to support the use of spiritually focused therapies for psychiatric disorders, including research on interventions that can accommodate patients from diverse religions and those who are not bound to a specific religious tradition but for whom spiritual values play an important role in their lives.
To address this research gap, our group recently evaluated the acceptability and initial efficacy of a multifaith spiritually based intervention (SBI) in 22 patients with generalized anxiety disorder (GAD; Koszycki, Raab, Adlosary, & Bradwejn, 2010). The intervention was adapted from Roger Walsh's “Essential Spirituality” (1999) and focused on core teachings found in many religious traditions rather than on the teachings of a specific faith group, making it applicable to patients of diverse religious and spiritual backgrounds. Although the majority of patients who participated in this pilot trial came from Christian backgrounds, few were actively involved in organized or nonorganized religious or spiritual practices. Using manualized CBT as our active comparator, intent-to-treat (ITT) analysis revealed that the SBI and CBT demonstrated comparable efficacy in reducing anxiety, excessive worry, depressive symptoms, and impaired role functioning. Response and remission rates were also comparable across treatments. Retention with the SBI was high, with 82% of patients completing the 12 therapy sessions. Treatment gains persisted at 6-months follow-up. Our pilot data are broadly consistent with other studies demonstrating that spiritually accommodative psychotherapy is beneficial in devout patients with GAD (Azhar, Varma, & Dharap, 1994; Razali, Amenah, & Shan, 2002).
While findings of this first trial are promising and indicate a nondenominational SBI is well accepted by patients and has comparative efficacy to a gold standard treatment for GAD, a limitation of the study was the lack of a nonspecific control condition. Recent meta-analyses of CBT revealed no difference between CBT and supportive therapy for the treatment of GAD (Hunot, Churchill, de Lima, & Teixeira, 2007; Ott, 2011), suggesting CBT offers no benefits over and beyond nonspecific factors such as therapist attention and support. Thus, it is unclear to what extent the SBI does what ”any” psychotherapy would (Wampold, 2001) or offers specific antianxiety benefits. Accordingly, the primary objective of this second pilot study was to extend research on the SBI for GAD by comparing its effects to supportive therapy, a moderately active condition that controls for nonspecific factors that account for almost half of psychotherapy outcome variance (Hellerstein & Markowitz, 2008). We also explored whether changes in spirituality was an outcome of treatment.
Method
Participants
The institutional research ethics board approved the study and participants provided written informed consent. The sample comprised men and women 18 years and older who were recruited via flyers placed in local media, the Internet, university bulletin boards, and physician offices. To reduce risk of recruiting a self-selected sample of individuals who were specifically seeking a spiritual intervention, our recruitment flyer did not specify the nature of the psychological interventions being investigated. The advertisement stated the study was evaluating two forms of psychological interventions for GAD and interested individuals could contact the study number for more information. Individuals who inquired about the study participated in a telephone prescreen interview with a research assistant who provided a detailed description of the study interventions and procedures, confirmed the presence of GAD symptoms, and excluded those who were clearly ineligible to participate.
After the telephone prescreen, potentially eligible participants were given an appointment with the study investigators for confirmation of GAD and other eligibility criteria. To be eligible, participants needed to meet GAD criteria based on the Structured Clinical Interview for DSM-IV Mental Disorders-Patient Version (SCID-P; First, Spitzer, Gibbon, & Williams, 1997), with scores ≥15 on the Hamilton Anxiety Rating Scale (HAM-A; Hamilton, 1959) and ≥4 on the Clinical Global Impression-Severity (CGI-S) scale (Guy, 1976) at screen and baseline visits. Individuals from diverse religious or spiritual pathways, either formal or informal, and those who did not engage in any formal or informal religious or spiritual practice but who were comfortable being randomized to the SBI were also eligible to participate.
Exclusion criteria included a lifetime history of psychosis or bipolar disorder, history of substance use disorders in the last 6 months, history of psychotic features of affective disorder, and high suicide risk. Other comorbidities were allowed so long as the GAD was the primary and predominant disorder. Participants with depressive disorders who obtained a score ≥ 21 on the Montgomery-Åsberg Depression Rating Scale (Montgomery & Åsberg, 1979) at screen visit were excluded. Concurrent use of antidepressants, anxiolytics, hypnotics, and herbal products with psychoactive substances was allowed as long as the medication type and dose had remained stable for 6 weeks prior to randomization and there was no change in medication type and dose after randomization. Concomitant treatment with any psychotherapy or spiritual counseling was proscribed during the study. Concomitant treatment was recorded at each assessment.
After verification of eligibility, informed consent, and baseline assessments, participants were randomized to the SBI or SP using a computer-based random number generation program prepared in advance by a research assistant. Allocations were generated using blocks of four to maintain close balance of the numbers of patients in each treatment group at any time during the trial.
Interventions
Participants in the SBI condition attended 12 weekly 50-minute individual sessions. A doctoral-level mental health chaplain and psychologist conducted therapy and a manual was developed to standardize therapist behavior during the sessions. The intervention is multicomponent and formulated from Walsh's (1999) Essential Spirituality: The 7 Central Practices to Awaken Heart and Mind. Consistent with other definitions of spirituality (Hill & Pargament, 2003; Pargament, 2007), Walsh conceptualizes spirituality as a direct experience of the sacred and the practices and exercises described in Essential Spirituality are intended to help one experience the sacred. Derived from seven religious traditions (Christianity, Judaism, Islam, Buddhism, Hinduism, Taoism, Confucianism), the spiritual practices are designed to cultivate such virtues as kindness, love, joy, peace, vision, wisdom, and generosity.
Many of the spiritual practices described in Walsh's book and incorporated in our SBI are relevant for individuals with GAD and their beneficial effects are supported by empirical research in diverse clinical and nonclinical samples. For example, contemplative practices can help one decenter from worry and decrease physiological concomitants of anxiety (Sipe & Eisendrath, 2012; Knabb, 2012; Rapgay & Bystrisky, 2009); cultivating awareness and spiritual wisdom can provide a more adaptive and flexible framework for understanding the self and the world and promote increased tolerance to uncertainty and an enhanced sense of coping resourcefulness and optimism (Keefe et al., 2001; King & Koenig, 2009; Koenig, 2009; Pargament, 2007); and cultivating compassion, love, forgiveness, gratitude, and generosity can reduce relationship difficulties that often contribute to anxiety and worry, facilitate social connectedness, dampen stress-induced behavioral and hormonal responses, and improve psychological well-being (Emmons & McCullough, 2003; Fujiwara, 2007; Pace et al., 2009; Sternthal et al., 2010; Wood, Maltby, Gillett, Linley, & Joseph, 2008).
A description of the weekly sessions is described in Table1. Briefly, the first session was devoted to providing psychoeducation about GAD, discussing the spiritual framework for anxiety reduction, developing treatment goals, and addressing concerns about the intervention. Contemplative practices (concentration meditation, prayer) were introduced in the second session and participants were encouraged to establish a daily practice during the trial to calm their minds. Subsequent sessions focused on discussion of an array of spiritual themes, participants' experiences with the spiritual practices, and the effect the practices had on their anxiety and well-being.
Table 1.
Content of the Spiritual Intervention
| Session | Session themes |
|---|---|
| 1 | Psychoeducation about GAD. Provide rationale for a spiritual approach for GAD. Identify treatment goals. |
| 2 | Introduce contemplative practices to developing a calm and concentrated mind. |
| 3 | Respond skillfully to difficult emotions. Explore and learn from painful emotions. Release and transform painful emotions and use them appropriately. |
| 4 | Understand the power of forgiveness in releasing emotional pain from the past. The connection between gratitude and positive emotions. |
| 5 | Being mindful. Understand the benefits of awareness and the costs of living mindlessly |
| 6 | Awaken spiritual vision by recognizing the sacred in people, things, and within ourselves. Understanding the transforming power of seeing the sacred in all things. |
| 7 | Attachment can be a source of suffering. Happiness lies in reducing and relinquishing attachments. |
| 8 | Cultivating higher motivation is a central goal of spiritual practice. Our deepest desires are healthy and altruistic. |
| 9 | Ethical living. Unethical living springs from and leads to negative emotional states. Ethical living and treating others as you wish to be treated improves emotional well-being. |
| 10 | Express spirit in action. Cultivate generosity and service to others. |
| 11 | Cultivate spiritual intelligence. Seek wisdom in nature, silence, xc and solitude, and reflect on the nature of life and death. Importance of self-acceptance and relinquishing self-attack and condemnation |
| 12 | Wrap up and Evaluation |
Note. The spiritual intervention was adapted from the spiritual teachings described in Essential Spirituality (Walsh, 1999).
Participants were given a copy of Walsh's Essential Spirituality (1999) and were assigned readings and spiritual practices from the book each week. Compliance with homework was monitored at each session by the therapist. Participants were asked if they read the assigned readings and whether they attempted the spiritual practices. While the same general practices were assigned to every participant, flexibility was permitted regarding how to practice them. For example, to calm and focus the mind, a participant might choose to establish a regular practice of contemplative prayer, while another might prefer sustained concentration on the breath. In the final session, treatment gains were reviewed and participants were encouraged to continue with the spiritual practices.
Doctoral-level clinicians experienced in supportive interventions delivered the SP. SP was structurally similar to the SBI in frequency and duration of individual sessions. The SP manual developed by Markowitz and colleagues (Markowitz, Manber, & Rosen, 2008) and used in several previous psychotherapy trials (Markowitz, Kocsis, Bleiberg, Christos, & Sacks, 2005; Markowitz et al., 1998; Koszycki, Bisserbe, Blier, Bradwejn, & Markowitz, 2012), including the large multisite REVAMP trial (Koscis et al. 2009), was used to promote standardization of therapist treatment behavior. Briefly, SP emphasizes nonspecific common factors that are important across psychotherapeutic modalities and includes reflective listening, empathy, eliciting affect, therapeutic optimism, and acknowledgment of the patient's assets. The intervention is not structured and the therapist allows the patient to determine the focus of each session. SP offers no explicit explanatory mechanism for treatment effects and techniques of other treatment modalities such as interpersonal, psychodynamic, cognitive, and behavioral therapies are proscribed. Similarly, in current study, the SP did not offer participants a spiritual framework for therapy and spiritual themes and practices were not a focus of the intervention. SP does not include homework.
All psychotherapy sessions were audiotaped and adherence to the treatment protocols was monitored throughout the trial.
Measures
Primary Outcomes
HAM-A (Hamilton, 1959)
The HAM-A is a 14-item clinician-rated scale that provides an overall measure of global anxiety. The scale is one of the most widely used primary outcome measures in treatment studies of anxiety and is considered the gold standard for pharmacological treatment studies of GAD. A total HAM-A score ≤ 7 is considered to be in the normative range. The scale has been shown to have good psychometric properties, including internal consistency (αs range from 0.79 to 0.86), test-retest reliability (r = 0.96), inter-rater reliability (rs range from 0.74 to 0.97), and concurrent and discriminant validity (Beck & Steer, 1991; Gjerris et al., 1983; Shear et al., 2001). An independent assessor who was blind to treatment assignment administered the HAM-A. The evaluator began each assessment by reminding patients not to reveal the treatment they had been assigned to.
Penn State Worry Questionnaire (PSWQ; Meyer, Miller, Metzger, & Borkovec, 1990)
The PSWQ is a 16-item self-report questionnaire that measures frequency and intensity of worry symptoms. Items are rated on a 5-point scale (1–5), with total scores ranging from 16 to 80. The PSWQ has acceptable psychometric properties including good internal consistency (αs range from 0.86 to 0.93), test-retest reliability (rs range from 0.75 to 0.92), and convergent validity (Brown, Antony, & Barlow, 1992; Molina & Borkovec, 1994). It is widely used in GAD research and is sensitive to change in response to treatment.
Beck Anxiety Inventory (BAI; Beck, Epstein, Brown, & Steer, 1988)
The BAI is a 21-item self-report measure that assesses anxiety, with a focus on somatic symptoms. Symptoms are rated on a 4-point scale (0 to 3), and respondents are required to report how much they have been bothered by each symptom during the past week. The BAI has good psychometric properties, including high internal consistency (αs range from 0.90 to 0.94), satisfactory test-retest reliability (rs range from 0.67 to 0.93), and good convergence validity (Beck et al., 1988; Fydrich, Dowdall, & Chambless, 1992). It is a reliable and sensitive measure for assessing change with treatment.
Secondary Outcomes
Clinical Global Impression-Severity Scale (CGI-S; Guy, 1976)
The CGI-S is a standardized assessment tool, which allows clinicians to rate the severity of illness, change over time, and response to treatment. It is one of the most widely used outcome measures in clinical research and a sensitive index of treatment response. The scale has good concurrent validity and relatively good reliability (r = 0.66; Leon et al., 1993). The CGI-S was administered by an independent assessor who was blind to treatment assignment.
Beck Depression Inventory (BDI-II; Beck, Steer, & Brown, 1996)
The BDI-II is a 21-item self-report measure developed to determine the severity of depressive symptoms over a 2-week period. The scale is widely used in treatment outcome studies to monitor changes in depressive symptoms. Each item is rated on a 4-point scale (0 to 3) and added together to yield a total score. The scale has been shown to have solid psychometric properties, including good internal consistency (αs ranges from 0.89 to 0.93), test-retest reliability (r = 0.73), and concurrent and discriminant validity (Beck et al., 1996; Storch, Roberti, & Roth, 2004; Wiebe & Penley, 2005).
Intolerance of Uncertainty Scale (IUS; Freeston, Rhéaume, Letarte, Dugas, & Ladouceur, 1994; Buhr & Dugas 2002)
The IUS is a 21-item self-report scale that targets how an individual responds to uncertainty on cognitive, emotional, and behavioral levels. Items are rated on a 5-point scale ranging from 1 (not characteristic of me) to 5 (entirely characteristic of me). The scale has demonstrated good psychometric properties, including high internal consistency (α = 0.91), good test-retest reliability (r = 0.74), and good discriminant and convergent validity. It has been found to be a sensitive measure of change with psychotherapy.
Social Adjustment Scale-Self Report Version (SAS-SR; Weissman, Prusoff, Thompson, Harding, & Myers, 1978)
The SAS-SR is a 42-item scale that assesses functioning in work, social and leisure activities, extended family relationships, primary relationship, parental role, and family unit. An overall score is calculated and subscale scores are calculated, with lower scores indicating better social adjustment. The SAS-SR has satisfactory psychometric properties, including high internal consistency for the overall adjustment score (α = 0.91) and test-retest reliability (r = 0.80; Edwards, Yarvis, Mueller, Zingale, & Wagman, 1978). The SAS-SR is a sensitive measure of social functioning in treatment outcome studies.
Spiritual Outcomes
Daily Spiritual Experience Scale (DSES; Underwood & Teresi, 2002)
The DSES is a 16-item self-report measure of how religiousness or spirituality is expressed in daily life and is a subscale of the Fetzer Institute's Multidimensional Measure of Religiousness/Spirituality. The DSES measures such constructs as awe, gratitude, mercy, sense of connection with the transcendent, compassionate love, and desire for closeness with a higher power. The scale is not rooted in any organized religious activity or religious worldview and is therefore suitable for individuals from a variety of religious and spiritual backgrounds. The scale has sound psychometric properties, including high internal consistency (αs range from 0.94 to 0.95) and temporal stability (rs range from 0.77 to 0.85; Underwood & Teresi, 2002; Loustalot, Wyatt, Boss, & McDyess, 2007), and is a sensitive measure of change with spiritual interventions (Geary & Rosenthal, 2011; Boelens, Reeves, Replogie, & Koenig, 2012). Item responses range from 1 (many times a day) to 6 (never or almost never) for the first 15 items and 1 (not at all close) to 4 (as close as possible) for item 16. In the current study, items were reverse scored so that higher scores indicate increased perception of daily spiritual experiences (Underwood, 2006).
Age Universal Intrinsic-Extrinsic Scale (Age Universal I-E; Maltby & Lewis, 1996; Maltby & Day, 1998)
The revised Age-Universal I-E scale is a 20-item scale that assesses intrinsic and extrinsic religious orientation. People with an intrinsic orientation live according to internalized religious values and beliefs, whereas extrinsically oriented people live a lifestyle in which religion is related to social expectations or pressures. The scale can be used with religious and nonreligious individuals. The scale has adequate psychometric properties including satisfactory internal consistency (α = 0.84 for intrinsic and 0.76 for extrinsic orientation) and convergent validity.
Statistical Method
Data were analyzed with SPSS version 20. Analyses were performed on the ITT sample using all available data. The last observation carried forward method was used to impute missing data. Supplementary analyses were also performed on participants who completed the 12 therapy sessions and participants who attended the 3-month follow-up assessment. Analysis of variance (ANOVA) and chi-square were used to assess demographic variables, clinical characteristics, and baseline outcome measures. Our main interest was in comparing groups at posttreatment. As recommended by Vickers (2005) and Vickers and Altman (2001), we used ANCOVA, with the baseline score of each measure used as covariate. Analysis of covariance (ANCOVA) was also used to compare groups at 3-month follow-up. Endpoint BAI and 3-month follow-up DSES scores were positively skewed and analysis was performed on both untransformed and logarithmically transformed data. However, as results were comparable for both analysis, untransformed results are reported herein. Chi-square was used for categorical data and Pearson's correlations were computed to assess intercorrelations among outcome variables at baseline, posttreatment, and 3-months follow-up. Within- and between-group effect sizes (Cohen's d) and the 95% confidence interval (CI) around the between-group effect size were calculated using ClinTools Software (Devilly, 2005). Calculation of within group effect sizes accounted for correlations between repeated measures. Significance was established at p < 0.05, two-tailed tests.
Results
Flow of Participants
Figure1 displays the flow of participants during the trial. One hundred and twenty-seven individuals inquired about the study and agreed to complete the telephone prescreen after a description of the study and interventions was provided. Of these, 73 were eligible for a structured face-to-face interview and 56 attended the interview. Of the 56 individuals, 26 were excluded at the screen visit because they did not meet study criteria. Of those who were eligible for the baseline visit, three withdrew prior to the visit, three were excluded because they did not have a baseline HAM-A score ≥15, and one was excluded because GAD criteria were not met. Twenty-three participants, comprising 41% of screened individuals, were randomized to the SBI (n = 11) or SP (n = 12). Four participants were treated in a psychiatric setting and the remainder at a university-based community counseling service. Twenty participants (87%) completed the 12 therapy sessions, including all participants assigned to the SBI and 75% (9/12) assigned to SP (Fisher's's exact, p = .22). Of the SP participants who terminated early (one male, two females), one dropped out before beginning therapy, one completed six sessions, and another completed 10 sessions. Postbaseline assessments were available for two of the three dropouts. Reasons for early termination appear in Figure1.
Figure 1.
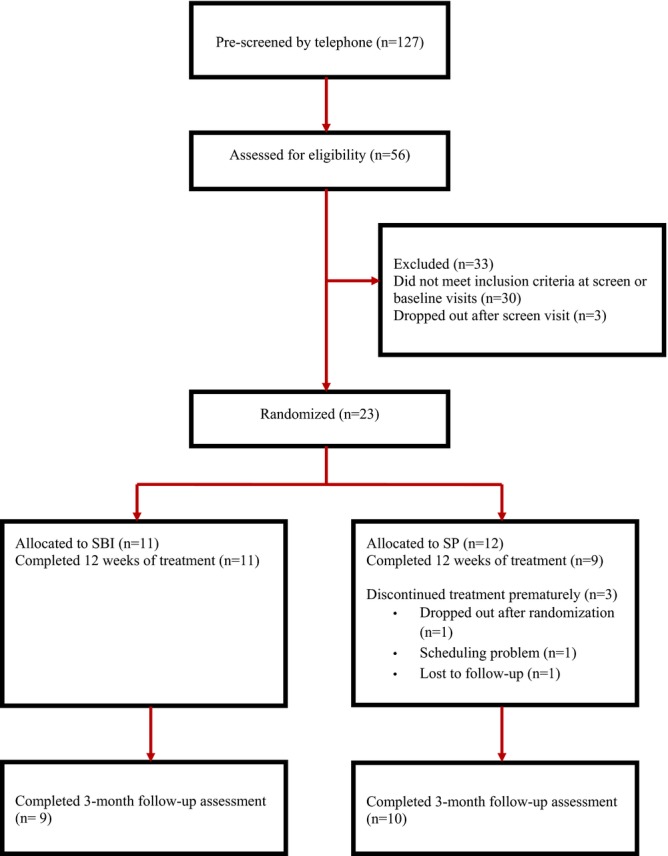
Flow of participants during the trial.
Baseline Demographic and Clinical Characteristics
Demographic and clinical characteristics of the sample are presented in Table2. The treatment groups were comparable with respect to age, F(1,22) = 0.49, p = 0.49, ethnicity (Fisher's's exact, p = .22), and gender (Fisher's exact, p = .19). Most participants (70%) came from Christian backgrounds but the majority was not religiously or spiritually observant. No group difference emerged for religious background, χ2(1) = 4.21, p = .12, or religious adherence (Fisher's exact, p = .37). Roughly half of participants had a concurrent threshold or subthreshold Axis I disorder, including another anxiety disorder (n = 9), depressive disorders (n = 5), and eating disorder (n = 2). No difference emerged between the groups on Axis I comorbidity, χ2(1) = 0.05, p = .83, or use of prescription psychotropic medication (Fisher's exact, p = .67). The mean baseline HAM-A score was 19.9 ± 3.0, reflecting moderately severe anxiety. Completers and dropouts did not differ on demographic and baseline clinical characteristics, although we had little power to find such a difference.
Table 2.
Demographic and Baseline Characteristics of the ITT Sample
| Variable | SBI (n = 11) | SP (n = 12) |
|---|---|---|
| Mean (SD) age | 39.82 ± 14.9 | 44.75 ± 18.3 |
| Gender (% female) | 82% | 50% |
| Ethnicity (% Caucasian) | 82% | 100% |
| Religious background (%) | ||
| None | 9% | 25% |
| Christian | 64% | 75% |
| Other | 27% | 0% |
| Currently practicing religion (%) | 36% | 17% |
| Axis I comorbidity (%) | 54% | 50% |
| Concurrent use psychotropic medication (%) | 36% | 25% |
Note. SBI = spiritually based intervention; SP = supportive psychotherapy. No differences between treatment groups were found for baseline demographic and clinical variables.
Efficacy Analyses
Intercorrelations among outcome variables at baseline and endpoint are presented in Table3. Table4 provides the mean baseline and endpoint scores for efficacy outcomes, effect sizes (Cohen's d), and 95% CI around the between-group effect size for the ITT sample. Baseline scores did not differ between conditions (ps ranged from .13 to .84). Both treatments improved primary and secondary outcomes at endpoint. Large (d > 0.80) within-group effect sizes appeared for the SBI on all outcomes and on the HAM-A, CGI-S, and BDI for SP. The ANCOVA yielded a significant treatment effect for mean scores on the primary outcomes HAM-A, F(1,20) = 13.57, p = .001, and PSWQ, F(1,20) = 9.92, p = 0.005, and the secondary outcomes CGI-S, F(1,20) = 17.51, p < .001, and IUS, F(1,20) = 11.93, p = .003. On all measures, the SBI produced better outcome than SP, with large between-group effect sizes. Analysis of the HAM-A scale also revealed that a greater percentage of SBI-treated participants obtaining a score in the normative range, defined a priori as a score ≤7: 82% (9/11) versus 25% (3/12) (Fisher's exact, p = .012). No significant differences at endpoint emerged for the BAI, F(1,20) = 0.79, p = .39, BDI, F(1,20) = 1.07, p = .31, or SAS-SR total score, F(1,20) = 1.89, p = .13.
Table 3.
Intercorrelations Among Outcome Measures at Baseline, Endpoint, and 3-Month Follow-Up for the Intent-to-Treat Sample
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. HAM-A | ||||||||||
| Baseline | – | |||||||||
| Endpoint | ||||||||||
| 3-MFU | ||||||||||
| 2. PSWQ | ||||||||||
| Baseline | .20 | – | ||||||||
| Endpoint | .68** | |||||||||
| 3-MFU | .65** | |||||||||
| 3. BAI | ||||||||||
| Baseline | .51* | .09 | – | |||||||
| Endpoint | .36 | .51* | ||||||||
| 3–MFU | .35 | .26 | ||||||||
| 4. CGI-S | ||||||||||
| Baseline | .73* | .26 | .33 | – | ||||||
| Endpoint | .91** | .59** | .29 | |||||||
| 3-MFU | .94** | .57** | .36 | |||||||
| 5. BDI-II | ||||||||||
| Baseline | .44* | .09 | .26 | .26 | – | |||||
| Endpoint | .59** | .57** | .65** | .56** | ||||||
| 3-MFU | .60** | .57** | .45* | .64** | ||||||
| 6. IUS | ||||||||||
| Baseline | .33 | .53* | .45* | .11 | .51* | – | ||||
| Endpoint | .54** | .74** | .59** | .36 | .54* | |||||
| 3-MFU | .11 | .24 | .20 | .08 | .09 | |||||
| 7. SAS-SR | ||||||||||
| Baseline | .08 | .04 | .07 | .01 | .47* | .31 | – | |||
| Endpoint | .44 | .63** | .64** | .39 | .71** | .65** | ||||
| 3-MFU | .59** | .66** | .47* | .62** | .69** | .001 | ||||
| 8. DSES | ||||||||||
| Baseline | .35 | .37 | .24 | .25 | −.003 | .29 | .18 | – | ||
| Endpoint | −.43* | −.35 | −.12 | −.45* | −.28 | −.28 | −.28 | |||
| 3-MFU | −.56** | −.36 | −.25 | −.49* | −.29 | −.05 | −.26 | |||
| 9. I-R | ||||||||||
| Baseline | .49* | .26 | .22 | .19 | .10 | .30 | .09 | .78* | – | |
| Endpoint | −.31 | −.20 | .07 | −.37 | −.13 | .05 | −.12 | .84** | ||
| 3-MFU | −.44* | −.23 | −.08 | −.38 | −.31 | .03 | .12 | .75** | ||
| 10. E-R | ||||||||||
| Baseline | .44* | .19 | .33 | .22 | .07 | .37 | −.04 | .55* | .70** | – |
| Endpoint | −.25 | −.26 | −.008 | −.28 | −.10 | .08 | −.15 | .57** | .73** | |
| 3-MFU | −.23 | −.09 | .02 | −.28 | .001 | .18 | −.02 | .45* | .63** |
Note. 3-MFU = 3-month follow-up; HAM-A = Hamilton Anxiety Rating Scale; PSWQ = Penn State Worry Questionnaire; BAI = Beck Anxiety Inventory; CGI-S = Clinical Global Impression-Severity; BDI-II = Beck Depression Inventory; IUS = Intolerance of Uncertainty Scale; SAS-SR = Social Adjustment Scale-Self Report; DSES = Daily Spiritual Experiences Scale; I-R = Age Universal Intrinsic Religiosity subscale; E-R = Age Universal Extrinsic Religiosity subscale.
p ≤ .05
p ≤ .01.
Table 4.
Means (SD) and Within- and Between-Group Effect Sizes (Cohen's d) for Primary and Secondary Continuous Outcomes at Posttreatment and 3-Month Follow-up for the Intent-to-Treat Sample
| Measure | Mean (SD) | Within-group effect size | Between-group effect size (95% CI) | ||||
|---|---|---|---|---|---|---|---|
| Pre | Post | 3-MFU | Pre-Post | Pre-3-MFU | Pre-Post | Pre-3-MFU | |
| HAM-A | |||||||
| SBI | 20.1 ± 3.1 | 4.8 ± 3.1*** | 5.3 ± 4.2* | 4.90 | 3.85 | 1.50 (0.70, 2.58) | 0.98 (0.11, 1. 84 ) |
| SP | 19.7 ± 3.0 | 11.0 ± 4.8 | 10.0 ± 5.4 | 2.14 | 1.63 | ||
| PSWQ | |||||||
| SBI | 68.6 ± 4.5 | 49.1 ± 9.6** | 49.2 ± 8.8* | 2.51 | 2.48 | 0.90 (0.05, 1.80) | 0.79 (−0.06, 1.64) |
| SP | 64.6 ± 8.7 | 59.9 ± 13.8 | 58.4 ± 13.7 | 0.38 | 0.52 | ||
| BAI | |||||||
| SBI | 17.2 ± 7.2 | 9.0 ± 4.0 | 6.4 ± 3.3** | 1.13 | 1.55 | 0.40 (−0.42, 1.23) | 1.18 (0.29, 2.07) |
| SP | 18.2 ± 8.9 | 12.6 ± 11.8 | 12.6 ± 6.4 | 0.53 | 0.70 | ||
| CGI-S | |||||||
| SBI | 4.18 ± 0.4 | 1.7 ± 0.8*** | 1.6 ± 1.0* | 7.42 | 4.03 | 1.64 (0.70, 2.58) | 0.86 (0.003, 1.71) |
| SP | 4.1 ± 0.3 | 2.9 ± 0.7 | 2.5 ± 1.0 | 1.21 | 0.89 | ||
| BDI-II | |||||||
| SBI | 20.2 ± 11.6 | 8.0 ± 8.7 | 8.0 ± 8.9 | 1.15 | 1.15 | 0.44 (−0.39, 1.27) | 0.37 (−0.46, 1.19) |
| SP | 21.1 ± 7.0 | 11.7 ± 8.0 | 11.2 ± 8.4 | 1.25 | 1.28 | ||
| IUS | |||||||
| SBI | 81.2 ± 16.5 | 57.0 ± 13.2** | 56.0 ± 16.2 | 1.48 | 1.52 | 1.04 (0.17, 1.92) | 0.53 (−0.30, 1.37) |
| SP | 78.3 ± 17.4 | 73.3 ± 17.7 | 66.1 ± 21.0 | 0.28 | 0.63 | ||
| SAS-SRa | |||||||
| SBI | 2.1 ± 0.3 | 1.8 ± 0.3 | 1.8 ± 0.4 | 1.23 | 1.08 | 0.54 (−0.30, 1.37) | 0.63 (−0.21, 1.47) |
| SP | 2.1 ± 0.3 | 2.0 ± 0.4 | 2.0 ± 0.4 | 0.40 | 0.31 | ||
Note. SD = standard deviation; SBI = spiritually based intervention; SP = supportive psychotherapy; HAM-A = Hamilton Anxiety Rating Scale; PSWQ = Penn State Worry Questionnaire; BAI = Beck Anxiety Inventory; CGI-S = Clinical Global Impression-Severity; BDI-II = Beck Depression Inventory; IUS = Intolerance of Uncertainty Scale; SAS-SR = Social Adjustment Scale-Self-Report; ES = effect size; CI = confidence interval
a Low scores on the SAS-SR indicate better psychosocial functioning.
p ≤ .05
p ≤ .01
p ≤ .001 comparing the SBI with SP.
Results remained the same when supplementary ANCOVAs were performed on the completer sample (n = 11, SBI; n = 9 SP). At endpoint, mean (standard deviation [SD]) scores were significantly lower for the SBI than SP, respectively, for the primary outcomes HAM-A, 4.8 ± 3.1 versus 9.4 ± 3.5, F(1,17) = 11.37, p = .004, Cohen's d = 1.40 (95% CI: 0.42, 2.38) and PSWQ, 49.1 ± 9.6 versus 59.7 ± 15.7, F(1,17) = 9.92, p = .006, Cohen's d = 0.83 (95% CI: 0.08, 1.75), and for secondary outcomes CGI-S, 1.7 ± 0.8 versus 2.7 ± 0.5, F(1,17) = 12.09, p = .003, Cohen's d = 1.39 (95% CI: 0.41, 2.37) and IUS, 57.0 ± 13.2 versus 74.9 ± 19.5, F(1,17) = 10.12, p = .005, Cohen's d = 1.09, (95% CI: 0.15, 2.04). Differences in the percentage of patients who achieved a HAM-A score in the normative range approached significance; 82% (9/11) for the SBI and 33% (3/9) for SP (Fisher's exact, p = .065). Mean (SD) scores did not differ significantly between the SBI and SP, respectively, for the BAI, 9.0 ± 4.0 versus 12.0 ± 13.6, F(1,17) = 0.36, p = .55, Cohen's d = 0.31 (95% CI: −0.74, 1.02), BDI-II, 8.0 ± 8.7 versus 9.1 ± 7.1, F(1,17) = 0.12, p = 0.73, Cohen's d = 0.14 (95% CI: −0.74, 1.02), or SAS-SR total score, 1.8 ± 0.3 versus 2.0 ± 0.5, F (1,17) = 1.61, p = .22, Cohen's d = 0.44 (95% CI: −0.45, 1.33).
Maintenance of Treatment Gains
Nineteen (83%) participants (SBI, n = 9; SP, n = 10) completed the 3-month follow-up assessment. As shown in Table4, the ANCOVAs for the ITT sample revealed sustained improvement for both interventions over the follow-up period, with pre- to follow-up within-group effect sizes ranging from 1.08 (SAS-SR) to 4.03 (CGI-S) for the SBI, and 0.31 (SAS-SR) to 1.63 (HAM-A) for SP (see Table3). Participants assigned to the SBI continued to have better outcome on the HAM-A, F(1,20) = 5.31, p = .032, CGI-S, F(1,20) = 5.26, p = .033, and PSWQ, F(1,20) = 6.20, p = .022, with large between-group effect sizes. The number of participants with HAM-A scores in the normative range also remained higher for the SBI (82% [9/11]) than SP (33% [4/12]; Fisher's exact, p = .036). In contrast to acute treatment findings, the SBI yielded a better follow-up outcome on the BAI, F(1,20) = 8.57, p = .008, with a similar trend for the SAS-R, F(1,20) = 3.26, p = .086. However, differences between treatment conditions were no longer significant for the IUS, F(1,20) = 2.57, p = .12.
Supplementary ANCOVAs for the 19 participants who attended the 3-month follow-up assessment yielded comparable results. Outcome was better with the SBI than SP, respectively, on the primary outcomes PSWQ, 47.7 ± 7.9 versus 58.0 ± 14.7, F(1,16) = 5.41, p = .034, Cohen's d = 0.87 (95% CI: −0.07, 1.81) and BAI, 5.3 ± 2.4 versus 12.6 ± 7.0, F(1,16) = 8.99, p = .009, Cohen's d = 1.35 (95% CI: 0.35, 2.35), and approached significance for the HAM-A, 4.7 ± 4.0 versus 9.4 ± 5.4. F(1,16) = 4.29, p = .055, Cohen's d = 0.99 (95% CI: 0.04, 1.94) and CGI-S, 1.4 ± 1.0 versus 2.3 ± 0.9, F(1,16) = 4.25, p = .056, Cohen's d = 0.87 (95% CI: −0.07, 1.82). Between-group effect sizes on these outcomes were large. The number of patients who obtained a normative score on the HAM-A remained higher for the SBI (89% [8/9]) than SP (40% [4/10]), although differences approached significance (Fisher's exact, p = .057). No treatment effects were found between the SBI and SP, respectively, for mean (SD) scores on the IUS, 54.3 ± 17.4 versus 66.8 ± 23.0, F(1,16) = 1.41, p = .25, Cohen's d = 0.60 (95% CI: −0.31, 1.53), BDI-II, 5.4 ± 5.5 versus 8.9 ± 7.1, F(1,16) = 0.70, p = .27, Cohen's d = 0.54 (95% CI: −0.37, 1.45), or SAS-SR, 1.7 ± 0.3 versus 2.0 ± 0.4, F(1,16) = 1.78, p = .20, Cohen's d = 0.66 (95% CI: −0.27, 1.58).
Few changes in treatment were reported during the follow-up interval. Three participants changed their medication, including changing the type of antidepressant medication (n = 1 SBI), initiating antidepressant medication (n = 1 SP), and reducing the dose of benzodiazepine (n = 1 SP).
Effect of Treatment of Spiritual Outcomes
Mean scores, effect sizes and the 95% CI for the between-group effect size for spiritual outcomes for the ITT sample are shown in Table5. Baseline levels of religiosity and spirituality were comparable across groups (ps range from .32 to .45). The ANCOVA revealed a significant treatment effect for the DSES, F(1,20) = 12.31, p = .002, and a marginally significant effect for the intrinsic subscale of the Age Universal I-E scale, F(1,20) = 4.07, p = .056, at endpoint. For both measures, participants assigned to the SBI reported higher levels of daily spiritual experiences and intrinsicness, with large between-group effect sizes. No difference between groups emerged for the extrinsic subscale of the Age Universal I-E scale, F(1,20) = 0.22, p = .64. At 3-month follow-up, participants assigned to the SBI continued to have higher scores on the DSES, F(1,20) = 16.50, p = .001, than those assigned to SP, with a similar trend for the intrinsic subscale of the Age Universal I-E scale, F(1,20) = 3.69, p = .069. Group differences on the extrinsic scale were not significant, F(1,20) = 2.38, p = 0.14.
Table 5.
Means (SD) and Within- and Between-Group Effect Sizes for Measures of Spirituality for the Intent-to-Treat Sample at Endpoint and 3-Month Follow-up
| Measure | Mean (SD) | Within-group effect size | Between-group effect size (95% CI) | ||||
|---|---|---|---|---|---|---|---|
| Pre | Post | 3-MFU | Pre-Post | Pre-3-MFU | Pre-Post | Pre-3-MFU | |
| DSES | |||||||
| SBI | 39.7 ± 11.0 | 52.6 ± 12.9** | 53.9 ± 12.2*** | 0.23 | 0.49 | 1.29 (0.39–2.19) | 1.46 (0.54–2.38 ) |
| SP | 34.7 ± 18.6 | 34.1 ± 15.6 | 32.9 ± 16.2 | 0.10 | 0.09 | ||
| Age Universal-Intrinsic Religiosity | |||||||
| SBI | 13.8 ± 5.3 | 16.9 ± 5.1 | 16.1 ± 3.7 | 0.59 | 0.49 | 0.84 (−0.01–1.70) | 0.83 (−0.02–1.68) |
| SP | 11.9 ± 6.4 | 11.9 ± 6.6 | 12.0 ± 5.8 | 0.00 | 0.09 | ||
| Age Universal-Extrinsic Religiosity | |||||||
| SBI | 19.2 ± 5.1 | 20.4 ± 6.0 | 21.4 ± 3.7 | 1.07 | 1.22 | 0.46 (−0.37–1.28) | 0.78 (−0.07–1.63) |
| SP | 16.5 ± 7.3 | 17.2 ± 7.7 | 17.2 ± 6.8 | 0.03 | 0.10 | ||
Note. SBI = spiritually based intervention; SP = supportive psychotherapy; DSES = Daily Spiritual Experience Scale; CI = confidence interval; high scores on the DSES indicate higher levels of daily spiritual experiences.
p ≤ .01 and ***p ≤ .001 comparing the SBI versus SP.
For the completer sample, mean (SD) endpoint DSES scores were significantly higher in participants allocated to the SBI than SP condition, respectively, with a large between-group effect size, 52.6 ± 12.9 versus 37.4 ± 16.4, F(1,17) = 8.46, p = .01, Cohen's d = 1.04 (95% CI: 0.10, 1.98). However, no differences between the interventions were detected for mean (SD) scores on the intrinsic, 16.9 ± 5.4 versus 13.6 ± 6.1, F(1,17) = 2.62, p = .12, Cohen's d = 0.60 (95% CI: −0.30, 1.50) or extrinsic, 20.4 ± 6.0 versus 19.0 ± 7.1, F(1,17) = 0.31, p = .58, Cohen's d = 0.22 (95% CI: −0.66, 1.10) subscales of the Age Universal I-E scale. Analysis of 3-month follow-up data of participants who attended the follow-up assessment indicated that DSES scores remained significantly higher for the SBI than SP, respectively, 53.0 ± 14.0 versus 36.7 ± 15.6, F(1,16) = 11.43, p = .004, Cohen's d = 1.25 (95% CI: 0.27, 2.24), whereas no difference emerged for the intrinsic, 16.6 ± 5.2 versus 13.5 ± 5.7, F(1,16) = 3.03, p = .10, Cohen's d = 0.49, (95% CI: −0.25, 1.40) or extrinsic, 20.3 ± 6.5 versus 19.1 ± 6.7, F(1,16) = 0.33, p = .57, Cohen's d = 0.55, (95% CI: −0.39, 1.47) subscales of the Age Universal I-E.
Discussion
This study demonstrates that a multicomponent SBI is a potentially efficacious treatment for GAD and has effects over and beyond nonspecific factors that contribute to therapy outcome. While patients in both treatment arms improved from baseline to endpoint, the SBI was better than SP in reducing blind clinician-ratings of anxiety and severity of illness and self-report worry and intolerance of uncertainty, with large between group effect sizes. The SBI and SP were similarly efficacious in improving self-report social adjustment, somatic anxiety, and depression, but we did find moderate treatment effects favoring the SBI on these outcomes. The percentage of participants who attained a total HAM-A score in the normative range was also greater for the SBI at endpoint. Overall, results were similar when supplementary analyses were performed on the completer sample. Improvement proved durable at 3-month follow-up, and with the exception of the IUS, the SBI still showed better outcome than SP on clinician and self-report measures. Our follow-up data are important given the beneficial effects psychotherapy tend to diminish following termination of treatment (Butler, Chapman, Forman, & Beck, 2006).
Similar to our first pilot study, retention with the SBI in the current study was high, with all randomized participants completing the 12 therapy sessions. Compliance with the assigned readings and spiritual practices was also satisfactory. Although attrition was somewhat higher for SP, study retention did not significantly differ by treatment group. Further, the rate of attrition with SP observed in this study is comparable or lower to other psychotherapy trials that have used SP as a nonspecific control condition (Koszycki et al., 2012; Markowitz et al. 1998; Markowitz et al., 2005) and comparable to other interventions known to be effective for GAD (Arntz, 2003; Koszycki et al., 2010). Our high retention rate with the SBI indicates that a spiritually focused approach to anxiety reduction is attractive, acceptable, and credible to individuals with GAD, including those who are not religiously adherent, and has importance as an adequate trial of psychotherapy is usually associated with better outcome (Lambert, 2007).
Other studies evaluating interventions tailored for religious patients with syndromal or subsyndromal GAD have similarly reported good retention rates (Azhar et al., 1994; Razali et al., 1998; Rosmarin, Pargament, Pirutiasky, & Mahoney, 2010). The overall favorable retention rate observed in studies using interventions within a religious framework has relevance for the treatment of devout clients who may prefer religious-oriented psychotherapy to secular approaches for treating mental health problems (Rosmarin et al., 2010; Smith et al., 2007). Although client religion is purported to be a potential barrier to compliance with secular psychological interventions (Koenig, 2012), there is limited research on whether religious psychotherapy fosters greater acceptance and engagement in treatment than secular therapeutic interventions among religious individuals.
Recent research has shown that religious psychotherapy (Rosmarin et al., 2010), prayer intervention (Boelens et al., 2012), secular forms of mindfulness meditation (Carmody, Reed, Kristeller, & Merriam, 2008; Geary & Rosenthal, 2011; Zernicker et al., 2012), and other forms of spiritual practices (Kohls, Walach, & Lewith, 2009) can enhance spiritual well-being. Other studies report that spiritual outcome is more pronounced with religious and spiritual interventions than with mainstream psychotherapies (Worthington et al., 2011). Consistent with these findings, the SBI in the present study resulted in higher day-to-day spirituality than SP at endpoint and at 3-month follow-up, suggesting the prescribed spiritual practices facilitated spiritual experiences and strengthened participants’ connection with the sacred. Although these data are very preliminary and the sample size was too small to reliably perform meditation analysis, it is plausible that enhancement of spiritual experiences contributed to the better outcome with the SBI.
Consistent with this view, cross-sectional studies have reported that higher levels of daily spiritual experiences correlate with less psychopathology (Boelens et al., 2012; Keefe et al., 2001) and that intrinsic religiousness is linked with lowered anxiety (Baker & Gorsuch, 1982; Bergin, Masters, & Richards, 1987; Sturgeon & Hamley, 1979) and less fear of the unknown (Roff, Butkeviciene, & Klemmack, 2002). Other studies, however, have found either no relationship or a positive relationship between religiosity, spirituality, and level of anxiety. In the present study, a modest but significant positive correlation emerged between baseline levels of intrinsic and extrinsic religiosity and clinician-rated anxiety but not with any of the self-report measures of anxiety and worry. Conversely, at endpoint and 3-month follow-up, higher levels of daily spiritual experiences were significantly associated with lower levels of clinician-rated anxiety. Despite mixed results of cross-sectional studies, our prospective findings are notable and suggest that understanding spiritual mechanisms of outcome with the SBI is an important avenue for future research.
In our previous trial (Koszycki et al., 2010), the SBI was delivered by a doctoral-level hospital chaplain working in a psychiatric setting, whereas in the current study, a psychologist was also involved in the delivery of this intervention. Although the sample was too small to make meaningful comparisons between types of provider, the percentage of participants achieving a HAM-A score in the normative range was equivalent for both therapists. This suggests that appropriately trained mental health chaplains can play an important role in the delivery of care to anxious individuals and that an intervention that incorporates a range of spiritual practices that are universal and not tied to a particular religious tradition can be effectively implemented by psychologists. Although integrating spirituality in psychotherapy is still controversial (Hefti, 2011; Plante, 2007), many psychologists already use interventions rooted in religious and spiritual traditions in clinical practice but have secularized them and reframed them within a positive psychology framework (Plante, 2008).
Whether secularized and nonsecularized religious and spiritual practices produce comparable outcomes in clinical populations has not been researched, but studies involving nonclinical samples suggest that nonsecularized practices may have greater psychological benefit (Rosmarin, Pirutinsky, Cohen, Galler, & Krumrei, 2011; Wacholtz & Pargament, 2005). While some religious patients may prefer a therapist who shares their religious views and traditions, research by Propst and colleagues (1992) suggests that shared religious orientation does not predict outcome with religious psychotherapy. Their research with clinically depressed devout Christian patients demonstrated that outcome with religious accommodative CBT was comparable for religious and nonreligious therapists.
While we are encouraged by these pilot data, study limitations should be noted. First, the sample size was small and results should therefore be viewed with caution. Second, the sample comprised predominantly Caucasian participants from Christian backgrounds with little formal religious or spiritual involvement, limiting generalizability of findings. Third, although differences did not attain statistical significance, women were overrepresented in the SBI and the extent to which findings can be fully extended to men is not clear. Fourth, our follow-up did not extend beyond 3 months and we cannot ascertain that the benefits of the SBI would have continued beyond this assessment period. Fifth, we did not measure social desirability and cannot rule out the possibility that participants in the SBI responded in a biased fashion to self-report and blind clinical assessments.
Sixth, selection bias may have influenced outcome. Although attrition did not differ significantly between the study treatments, participants allocated to SP may have been less motivated to remain in the study and perhaps had lower expectations for improvement than those assigned to the SBI. Relatedly, 17 of the 73 telephone prescreened participants who were invited for the face-to-face screen interview cancelled or did not show up for their appointment. While this is not unusual in clinical trials, participants who attended the screen visit may represent a self-selected sample that was more receptive to participating in a trial investigating a psychospiritual approach to anxiety management. Seventh, the study therapists were aware that the aim of the study was to determine whether the SBI had effects over and beyond nonspecific factors. Although the study interventions were manual guided to ensure treatment integrity and therapists in both treatment arms delivered the interventions competently, it is possible that therapist knowledge of the study objectives or other therapist factors biased the study in subtle or unknown ways.
A final limitation is that we did not collect data on participant preference for treatment prior to randomization, as treatment preference is known to have an important impact on outcome.
Despite these limitations, we believe this study has a number of strengths including a low dropout rate, use of a rigorous control psychotherapy which enhances the internal validity of our findings, and use of standardized diagnostic interviews, well-established and validated scales for assessing clinical outcome in GAD, blind clinical evaluators, and manualized interventions.
Conclusion
To summarize, this small, randomized controlled trial confirms earlier findings that clinically significant improvements in symptoms of GAD can be achieved with a brief spiritually focused intervention. These findings are preliminary and require replication in a larger trial that addresses the above-noted limitations. Understanding the therapeutic processes and mechanisms underlying the anxiety-reducing effects of the SBI also merits research attention. With growing interest in spiritual growth (Thoresen & Harris, 2002) and spiritually integrated mental health care (Lake et al. 2012; Post & Wade, 2009), spiritually focused therapies may emerge in the next few years as an important alternative and complementary approach to conventional psychotherapies for anxious individuals. In view of this trend, rigorously designed controlled efficacy studies of spiritually integrated therapies are needed.
References
- Ahrens CE, Abeling S, Ahmad S. Hinman J. Spirituality and well-being: The relationship between religious coping and recovery from sexual assault. Journal of Interpersonal Violence. 2010;25:1242–1263. doi: 10.1177/0886260509340533. doi: 10.1177/0886260509340533. [DOI] [PubMed] [Google Scholar]
- Ano GG. Vasconcelles EB. Religious coping and psychological adjustment to stress: a meta-analysis. Journal of Clinical Psychology. 2004;61:461–480. doi: 10.1002/jclp.20049. doi: 10.1002/jclp.20049. [DOI] [PubMed] [Google Scholar]
- Arntz A. Cognitive therapy versus applied relaxation as treatment of generalized anxiety Disorder. Behaviour Research and Therapy. 2003;41:633–646. doi: 10.1016/s0005-7967(02)00045-1. doi: 10.1016/S0005-7967(02)00045-1. [DOI] [PubMed] [Google Scholar]
- Azhar MZ, Varma SL. Dharap AS. Religious psychotherapy in anxiety disorder patients. Acta Psychiatrica Scandinavica. 1994;90:1–3. doi: 10.1111/j.1600-0447.1994.tb01545.x. doi: 10.1111/j.1600-0447.1994.tb01545.x. [DOI] [PubMed] [Google Scholar]
- Baetz M, Bowen R, Jones G. Koru-Sengul T. How spiritual values and worship attendance relate to psychiatric disorders in the Canadian population. Canadian Journal of Psychiatry. 2006;51:654–661. doi: 10.1177/070674370605101005. [DOI] [PubMed] [Google Scholar]
- Baetz M, Griffin R, Bowen R. Marcoux G. Spirituality and psychiatry in Canada: Psychiatric practice compared with patient expectation. Canadian Journal of Psychiatry. 2004;49:265–271. doi: 10.1177/070674370404900407. [DOI] [PubMed] [Google Scholar]
- Baetz M. Toews SJ. Clinical implications of research on religion, spirituality, and mental health. Canadian Journal of Psychiatry. 2009;54:292–301. doi: 10.1177/070674370905400503. [DOI] [PubMed] [Google Scholar]
- Baker M. Gorsuch R. Trait anxiety and intrinsic-extrinsic religiousness. Journal for the Scientific Study of Religion. 1982;21:199–122. [Google Scholar]
- Beck AT, Epstein N, Brown G. Steer RA. An inventory for measuring clinical anxiety: Psychometric properties. Journal of Consulting and Clinical Psychology. 1988;56:893–897. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- Beck AT. Steer RA. Relationship between the Beck Anxiety Inventory and the Hamilton Anxiety Rating Scale with anxious outpatients. Journal of Anxiety Disorders. 1991;5:213–223. [Google Scholar]
- Beck AT, Steer RA. Brown GK. Beck Depression Inventory manual. San Antonio, TX: Psychological Corporation; 1996. 2nd. [Google Scholar]
- Bergin AE, Masters KS. Richards PS. Religiousness and mental health reconsidered: A study of an intrinsicially religious sample. Journal of Counseling Psychology. 1987;34:197–204. [Google Scholar]
- Boelens PA, Reeves RR, Replogie WH. Koenig HG. The effects of prayer on depression and anxiety: Maintenance of positive influence one year after prayer intervention. International Journal of Psychiatry and Medicine. 2012;43:85–98. doi: 10.2190/PM.43.1.f. [DOI] [PubMed] [Google Scholar]
- Bonelli RM. Koenig HG. Mental disorders, religion and spirituality 1990–2010: A systematic evidence-based review. 2013. doi: 10.1007/s10943-013-9691-4. [DOI] [PubMed]
- Brown TA, Antony MM. Barlow DH. Psychometric properties of the Penn State Worry Questionnaire in a clinical sample of anxiety disorders sample. Behaviour Research and Therapy. 1992;30:33–37. doi: 10.1016/0005-7967(92)90093-v. doi: 10.1016/0005-7967(92)90093-V. [DOI] [PubMed] [Google Scholar]
- Buhr K. Dugas MJ. The intolerance of uncertainty scale: sychometric properties of the English version. Behaviour Research and Therapy. 2002;40:931–945. doi: 10.1016/s0005-7967(01)00092-4. doi: 10.1016/S0005-7967(01)00092-4. [DOI] [PubMed] [Google Scholar]
- Butler AC, Chapman JER, Forman EM. Beck AT. The empirical status of cognitive-behavioral therapy: A review of meta-analyses. Clinical Psychology Review. 2006;26:17–31. doi: 10.1016/j.cpr.2005.07.003. doi: 10.1016/j.cpr.2005.07.003. [DOI] [PubMed] [Google Scholar]
- Carmody J, Reed G, Kristeller J. Merriam P. Mindfulness, spirituality, and health-related symptoms. Journal of Psychosomatic Research. 2008;64:393–403. doi: 10.1016/j.jpsychores.2007.06.015. doi: 10.1016/j.jpsychores.2007.06.015. [DOI] [PubMed] [Google Scholar]
- Connor KM, Davidson JRT. Lee L-C. Spirituality, resilience, and anger in survivors of violent trauma: A community survey. Journal of Traumatic Stress. 2003;16:487–494. doi: 10.1023/A:1025762512279. doi: 10.1023/A:1025762512279. [DOI] [PubMed] [Google Scholar]
- Devilly GJ. ClinTools Software for Windows: Version 4. 2005. Retrieved from http://www.clintools.com.
- Dien S, Cook CCH. Koenig H. Religion, spirituality, and mental health: Current controversies and future directions. The Journal of Nervous and Mental Disease. 2012;200:852–855. doi: 10.1097/NMD.0b013e31826b6dle. doi: 10.1097/NMD.0b013e31826b6dle. [DOI] [PubMed] [Google Scholar]
- Edwards DW, Yarvis RM, Mueller DP, Zingale HC. Wagman WJ. Test-taking and the stability of adjustment scales: Can we assess patient deterioration? Evaluation Quarterly. 1978;2:275–291. doi: 10.1177/0193841x7800200206. [Google Scholar]
- Emmons RA. McCullough ME. Counting blessings versus burdens: an experimental investigation of gratitude and subjective well-being in daily life. Journal of Personality and Social Psychology. 2003;84:377–389. doi: 10.1037//0022-3514.84.2.377. doi: 10.1037/0022-3514.84.2.377. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M. Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders, Patient Edition (SCID-P) New York: New York State Psychiatric Institute, Biometrics Research; 1995. [Google Scholar]
- Freeston MH, Rhéaume J, Letarte H, Dugas MJ. Ladouceur R. Why do people worry? Personality and Individual Differences. 1994;17:791–802. doi: 10.1016/0191-8869(94)90048-5. [Google Scholar]
- Fujiwara T. The role of altruistic behavior in generalized anxiety disorder and major depression among adults in the United States. Journal of Affective Disorders. 2007;101:219–225. doi: 10.1016/j.jad.2006.11.024. doi: 10.1016/j.jad.2006.11.024. [DOI] [PubMed] [Google Scholar]
- Geary C. Rosenthal SL. Sustained impact of MBSR on stress, well-being, and daily spiritual experiences for 1 year in academic health employees. Journal of Alternative and Complementary Medicine. 2011;17:939–944. doi: 10.1089/acm.2010.0335. doi: 10.1089/acm.2010.0335. [DOI] [PubMed] [Google Scholar]
- Gjerris A, Bech P, Bøjholm S, Bolwig TG, Kramp P, Clemmensen L. Rafaelsen OJ. The Hamilton Anxiety Scale. Evaluation of homogeneity and inter-observer reliability in patients with depressive disorders. Journal of Affective Disorders. 1983;5:163–170. doi: 10.1016/0165-0327(83)90009-5. [DOI] [PubMed] [Google Scholar]
- Guy W. ECDEU assessment manual for psychopharmacology. Rockville, MD: US Department of Health, Education, and Welfare publication (ADM), National Institute of Mental Health; 1976. pp. 218–222. [Google Scholar]
- Hall DE, Meador KG. Koenig HG. Measuring religiousness in health research: Review and critique. Journal of Religion and Health. 2008;47:134–163. doi: 10.1007/s10943-008-9165-2. doi: 10.1007/s10943-008-9165-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton M. The assessment of anxiety states by rating. British Journal of Medical Psychology. 1959;32:50–55. doi: 10.1111/j.2044-8341.1959.tb00467.x. [DOI] [PubMed] [Google Scholar]
- Hefti R. Integrating religions and spirituality into mental health care. Religions. 2011;2:611–627. doi: 10.3390/rel2040611. [Google Scholar]
- Hellerstein DJ. Markowitz JC. Developing supportive psychotherapy as an evidence-based treatment (letter) American Journal of Psychiatry. 2008;165:1355–1356. doi: 10.1176/appi.ajp.2008.08040565. doi: 10.1176/appi.ajp.2008.08040565. [DOI] [PubMed] [Google Scholar]
- Hill PC. Pargament KI. Advances in the conceptualization and measurement of religion and spirituality: Implications for physical and mental health research. American Psychologist. 2003;58:64–74. doi: 10.1037/0003-066x.58.1.64. doi: 10.1037/0003-066X.58.1.64. [DOI] [PubMed] [Google Scholar]
- Hodge DR. Spiritually modified cognitive therapy: A review of the literature. Social Work. 2006;51:157–166. doi: 10.1093/sw/51.2.157. doi: 10.1093/sw/51.2.157. [DOI] [PubMed] [Google Scholar]
- Hook JN, Worthington EL, Davis DE, Jennings DJ, Gartner AL. Hook JP. Empirically supported religious and spiritual therapies. Journal of Clinical Psychology. 2010;66:46–72. doi: 10.1002/jclp.20626. doi: 10.1002/jclp.20626. [DOI] [PubMed] [Google Scholar]
- Hunot V, Churchill R, de Lima MS. Teixeira V. Psychological therapies for generalized anxiety disorder. Cochrane Database of Systematic Reviews. 2007:CD001848. doi: 10.1002/14651858.CD001848.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keefe FJ, Affleck G, Lefebvre J, Underwood L, Caldwell DS, Drew J. Pargament KI. Living with rheumatoid arthritis: the role of daily spirituality and daily religious and spiritual coping. Journal of Pain. 2001;2:101–110. doi: 10.1054/jpai.2001.19296. doi: 10.1054/jpai.2001.19296. [DOI] [PubMed] [Google Scholar]
- King MB. Koenig HG. Conceptualising spirituality for medical research and health service delivery. BMC Health Services Research. 2009;9:116. doi: 10.1186/1472-6963-9-116. doi: 10.1186/1472-6963-9-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King MB, Marston L, McManus S, Brugha T, Meltzer H. Beggington P. Religion, spirituality and mental health: results from a national study of English households. British Journal of Psychiatry. 2013;2002:68–73. doi: 10.1192/bjp.bp.112.112003. doi: 10.1192/bjp.bp.112.112003. [DOI] [PubMed] [Google Scholar]
- Knabb JJ. Centering prayer as an alternative to mindfulness-based cognitive therapy for depression relapse. Journal of Religion and Health. 2012;51:908–924. doi: 10.1007/s10943-010-9404-1. doi: 10.1007/s10943-010-9404-1. [DOI] [PubMed] [Google Scholar]
- Koenig HG. Concerns about measuring “spirituality” in research. Journal of Nervous Mental Disease. 2008;196:349–355. doi: 10.1097/NMD.0b013e31816ff796. doi: 10.1097/NMD.0b013e31816ff796. [DOI] [PubMed] [Google Scholar]
- Koenig HG. Research on religion, spirituality, and mental health: A Review. Canadian Journal of Psychiatry. 2009;54:283–291. doi: 10.1177/070674370905400502. [DOI] [PubMed] [Google Scholar]
- Koenig HG. Religious versus conventional psychotherapy for major depression in patients with chronic medical illness: Rationale, methods, and preliminary results. Depression Research and Treatment. 2012:1–11. doi: 10.1155/2012/460419. doi: 10.1155/2012/460419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koenig HG. Larson DK. Religions and mental health: Evidence for an association. International Review of Psychiatry. 2001;12:67–78. doi: 10.1080/09540260124661. [Google Scholar]
- Kohls N, Walach H. Lewith G. The impact of positive and negative spiritual experiences on distress and the moderating role of mindfulness. Archive for the Psychology of Religion. 2009;31:357–374. doi: 10.1163/008467209x12524724282032. [Google Scholar]
- Koszycki D, Bisserbe J-C, Blier P, Bradwejn J. Markowitz J. Interpersonal psychotherapy versus brief supportive therapy for depressed infertile women: First pilot randomized controlled trial. Archives of Women's Mental Health. 2012;15:193–201. doi: 10.1007/s00737-012-0277-z. doi: 10.1007/s00737-012-0277-z. [DOI] [PubMed] [Google Scholar]
- Koszycki D, Raab K, Adlosary F. Bradwejn J. A multifaith spiritually based intervention for generalized anxiety disorder: A pilot randomized trial. Journal of Clinical Psychology. 2010;66:430–441. doi: 10.1002/jclp.20663. doi: 10.1002/jclp.20663. [DOI] [PubMed] [Google Scholar]
- Lake J, Helgason C. Sarris J. Integrative mental health (IMH): Paradigm, research, and clinical practice. Explore. 2012;8:50–57. doi: 10.1016/j.explore.2011.10.001. doi: 10.1016/j.explore.2011.10.001. [DOI] [PubMed] [Google Scholar]
- Lambert MJ. Presidential address: What we have learned from a decade of research aimed at improving psychotherapy outcome in routine care. Psychotherapy Research. 2007;17:1–14. doi: 10.1080/10503300601032506. [Google Scholar]
- Laurent B, Nazareth I, Bellón-Saameño J, Geerlings MI, Maaroos H, Saldivia S. King M. Spiritual and religious beliefs as risk factors for the onset of major depression: An international cohort study. 2013. doi: 10.1017/S0033291712003066. [DOI] [PubMed]
- Leamy M, Bird V, LeBoutillier C, Williams J. Slade M. Conceptual framework for personal recovery in mental health: A systematic review and narrative synthesis. British Journal of Psychiatry. 2011;199:445–452. doi: 10.1192/bjp.bp.110.083733. doi: 10.1192/bjp.bp.110.083733. [DOI] [PubMed] [Google Scholar]
- Leon AC, Shear MK, Klerman GL, Portera L, Rosenbaum JF. Goldenberg I. A comparison of symptom determinants of patients and clinician global ratings in patients with panic disorder and depression. Journal of Clinical Psychopharmacology. 1993;13:327–331. [PubMed] [Google Scholar]
- Levin JS. How religion influences morbidity and health: Reflections on a natural history, salutogenesis and host resistance. Social Sciences and Medicine. 1996;43:849–864. doi: 10.1016/0277-9536(96)00150-5. doi: 10.1016/0277-9536(96)00150-5. [DOI] [PubMed] [Google Scholar]
- Loustalot FV, Wyatt SB, Boss B. McDyess T. Psychometric examination of the daily spiritual experiences scale. Journal of Cultural Diversity. 2006;13:162–167. [PubMed] [Google Scholar]
- Lucchetti G, Lucchetti AG, Badan-Neto AM, Peres PT, Moeira-Almeida A, Gomes C. Koenig HG. Religiousness affects mental health, pain and quality of life in older people in an outpatient rehabilitation setting. Journal of Rehabilitation Medicine. 2011;43:316–322. doi: 10.2340/16501977-0784. doi: 10.2340/16501977-0784. [DOI] [PubMed] [Google Scholar]
- Maltby J. Day L. Amending a measure of the Quest Religious Orientation: Applicability of the scales use among religious and non-religious persons. Personality and Individual Differences. 1998;25:517–522. doi: 10.1016/S0191-8869(98)00078-6. [Google Scholar]
- Maltby J. Lewis CA. Measuring intrinsic and extrinsic orientation toward religion: Amendments for its use among religious and non-religious samples. Personality and Individual Differences. 1996;21:936–946. doi: 10.1016/S0191-8869(96)00154-7. [Google Scholar]
- Marchand WR. Mindfulness-based stress reduction, mindfulness-based cognitive therapy, and Zen meditation for depression, anxiety, pain, and psychological distress. Journal of Psychiatric Practice. 2012;18:233–252. doi: 10.1097/01.pra.0000416014.53215.86. doi: 10.1097/01.pra.0000416014.53215.86. [DOI] [PubMed] [Google Scholar]
- Markowitz JC, Manber R. Rosen P. Therapists’ responses to training in brief supportive psychotherapy. American Journal of Psychotherapy. 2008;62:67–81. doi: 10.1176/appi.psychotherapy.2008.62.1.67. [DOI] [PubMed] [Google Scholar]
- Markowitz JD, Kocsis JH, Bleiberg KL, Christos PJY. Sacks M. A comparative trial of psychotherapy and pharmacotherapy for “pure” dysthymic patients. Journal of Affective Disorders. 2005;89:167–175. doi: 10.1016/j.jad.2005.10.001. doi: 10.1016/j.jad.2005.10.001. [DOI] [PubMed] [Google Scholar]
- Markowitz J, Kocsis JH, Fishman B, Spielman LA, Jacobsberg LB, Frances AJ. Perry SW. Treatment of depressive symptoms in human immunodeficiency virus-positive patients. Archives of General Psychiatry. 1998;55:452–457. doi: 10.1001/archpsyc.55.5.452. [DOI] [PubMed] [Google Scholar]
- McCaffrey AM, Eisenbert DM, Legedza ATR, Davis RB. Phillips RS. Prayer for health concerns: Results of a national survey on prevalence and patterns of use. Archives of Internal Medicine. 2004;164:858–862. doi: 10.1001/archinte.164.8.858. doi: 10.1001/archinte.164.8.858. [DOI] [PubMed] [Google Scholar]
- McIntosh DN, Poulin MJ. Silver RC. Holman EA. The distinct roles of spirituality and religiosity in physical and mental health after collective trauma: a national longitudinal study of responses to the 9/11 attacks. Journal of Behavioral Medicine. 2011;34:497–507. doi: 10.1007/s10865-011-9331-y. doi: 10.1007/s10865-011-9331-y. [DOI] [PubMed] [Google Scholar]
- Meyer TJ, Miller ML, Metzger RL. Borkovec TD. Development and validation of the Penn State Worry Questionnaire. Behaviour Research and Therapy. 1990;28:487–495. doi: 10.1016/0005-7967(90)90135-6. doi: 10.1016/0005-7967(90)90135-6. [DOI] [PubMed] [Google Scholar]
- Miller WR. Thoreson CE. Spirituality, religion, and health: An emerging research field. American Psychologist. 2003;58:24–35. doi: 10.1037/0003-066x.58.1.24. doi: 10.1037/0003-066X.58.1.24. [DOI] [PubMed] [Google Scholar]
- Molina S. Borkovec TD. In: The Penn State Worry Questionnaire: psychometric properties and associated characteristics, in worrying: Perspectives on theory, assessment, and treatment. Tallis F, editor; Davey GCL, editor. New York: Wiley; 1994. pp. 265–283. [Google Scholar]
- Montgomery SA. Åsberg M. A new depression scale designed to be sensitive to change. British Journal of Psychiatry. 1979;134:382–389. doi: 10.1192/bjp.134.4.382. doi: 10.1192/bjp.134.4.382. [DOI] [PubMed] [Google Scholar]
- Ott C. Cognitive behavioral therapy in anxiety disorders: current state of the evidence. Dialogues in Clinical Neuroscience. 2011;13:413–421. doi: 10.31887/DCNS.2011.13.4/cotte. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pace TWW, Negi LT, Adame DD, Cole SP, Sivilli TI, Brown MD. Raison CL. Effect of compassion meditation on neuroendocrine, innate immune and behavioral responses to psychosocial stress. Psychoneuroendocrinology. 2009;34:87–98. doi: 10.1016/j.psyneuen.2008.08.011. doi: 10.1016/j.psyneuen.2008.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pargament KI. The psychology of religion and coping. New York, NY: The Guildford Press; 1997. [Google Scholar]
- Pargament KI. Spiritually integrated psychotherapy: Understanding and addressing the sacred. New York, NY: The Guildford Press; 2007. [Google Scholar]
- Pargament KI, Koenig HG, Tarakeshwar N. Hahn J. Religious coping methods as predictors of psychological, physical, and spiritual outcomes among medically ill elderly patients: A two-year longitudinal study. Journal of Health Psychology. 2004;9:713–730. doi: 10.1177/1359105304045366. doi: 10.1177/1359105304045366. [DOI] [PubMed] [Google Scholar]
- Plante TG. Integrating spirituality and psychotherapy: Ethical issues and principles to consider. Journal of Clinical Psychology. 2007;63:981–902. doi: 10.1002/jclp.20383. doi: 10.1002/jclp.20383. [DOI] [PubMed] [Google Scholar]
- Plante TB. What do the spiritual and religious traditions offer the practicing psychologist? Pastoral Psychology. 2008;56:429–444. doi: 10.1007/s11089-008-0119-0. [Google Scholar]
- Propst LR. The comparative efficacy of religious and nonreligious imagery for the treatment of mild depression in religious individuals. Cognitive Therapy and Research. 1980;4:167–178. doi: 10.1007/BF01173648. [Google Scholar]
- Propst LR, Ostrom R, Watkins P, Dean T. Mashburn D. Comparative efficacy of religious and nonreligious cognitive-behavioral therapy for the treatment of clinical depression in religious individuals. Journal of Consulting and Clinical Psychology. 1992;60:94–103. doi: 10.1037//0022-006x.60.1.94. [DOI] [PubMed] [Google Scholar]
- Post CB. Wade NG. Religion and spirituality in psychotherapy: A practice-friendly review of research. Journal of Clinical Psychology. 2009;65:131–146. doi: 10.1002/jclp.20563. doi: 10.1002/jclp.20563. [DOI] [PubMed] [Google Scholar]
- Rapgay L. Bystrisky A. Classical mindfulness: An introduction to its theory and practice for clinical application. Annals of the New York Academy of Sciences. 2009;1172:148–162. doi: 10.1111/j.1749-6632.2009.04405.x. doi: 10.1111/j.1749-6632.2009.04405.x. [DOI] [PubMed] [Google Scholar]
- Razali SM, Hasanah CI, Aminah K. Subramaniam M. Religious-sociocultural psychotherapy in patients with anxiety and depression. Australian and New Zealand Journal of Psychiatry. 1998;32:867–872. doi: 10.3109/00048679809073877. doi: 10.3109/00048679809073877. [DOI] [PubMed] [Google Scholar]
- Roff LL, Butkeviciene R. Klemmack DL. Death anxiety and religiosity among Lithuanian health and social service professionals. Death Studies. 2002;26:731–742. doi: 10.1080/07481180290106517. doi: 10.1080/07481180290106517. [DOI] [PubMed] [Google Scholar]
- Rosmarin DH, Pargament KI, Pirutiasky S. Mahoney A. A randomized controlled evaluation of a spiritually integrated treatment for subclinical anxiety in the Jewish community, delivered via the Internet. Journal of Anxiety Disorders. 2010;24:799–808. doi: 10.1016/j.janxdis.2010.05.014. doi: 10.1016/j.janxdis.2010.05.014. [DOI] [PubMed] [Google Scholar]
- Rosmarin DH, Pirutinsky S, Cohen AB, Galler Y. Krumrei EJ. Grateful to God or just plain grateful? A comparison of religious and general gratitude. The Journal of Positive Psychology. 2011;6:389–396. doi: 10.1080/17439760.2011.596557. [Google Scholar]
- Rosmarin DH, Wachholtz A. Ai A. Beyond descriptive research: Advancing the study of spirituality and health. Journal of Behavioral Medicine. 2011;34:409–413. doi: 10.1007/s10865-011-9370-4. doi: 10.1007/s10865-011-9370-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuurmans-Stekhoven J. Moved by the spirit”: Does spirituality moderate the interrelationships between subjective well-being subscales? Journal of Clinical Psychology. 2010;66:709–725. doi: 10.1002/jclp.20694. doi: 10.1002/jclp.20694. [DOI] [PubMed] [Google Scholar]
- Seybold KS. Physiological mechanisms involved in religiosity/spirituality and health. Journal of Behavioral Medicine. 2007;30:303–309. doi: 10.1007/s10865-007-9115-6. doi: 10.1007/s10865-007-9115-6. [DOI] [PubMed] [Google Scholar]
- Shear MK, Vander Bilt J, Rucci P, Endicott J, Lydiard B, Otto MW. Frank DM. Reliability and validity of a structured interview guide for the Hamilton Anxiety Rating Scale (SIGH-A) Depression and Anxiety. 2001;13:166–178. doi: 10.1002/da.1033. [PubMed] [Google Scholar]
- Shreve-Neiger AK. Edelstein BA. Religions and anxiety: A critical review of the literature. Clinical Psychology Review. 2004;24:379–397. doi: 10.1016/j.cpr.2004.02.003. doi: 10.1016/j.cpr.2004.02.003. [DOI] [PubMed] [Google Scholar]
- Sipe WEB. Eisendrath SJ. Mindfulness-based cognitive therapy: Theory and practice. Canadian Journal of Psychiatry. 2012;57:63–69. doi: 10.1177/070674371205700202. [DOI] [PubMed] [Google Scholar]
- Sloan RP, Bagiella E. Powell T. Religion, spirituality and medicine. Lancet. 1999;353:664–667. doi: 10.1016/s0140-6736(98)07376-0. [DOI] [PubMed] [Google Scholar]
- Smith TB, Bartz J. Scott Richards P. Outcomes of religious and spiritual adaptations to psychotherapy: A meta-analytic review. Psychotherapy Research. 2007;17:643–655. doi: 10.1080/10503300701250347. [Google Scholar]
- Sternthal MJ, Williams DR, Muscik MA. Buck AC. Depression, anxiety, and religious life: A search for mediators. Journal of Health and Social Behavior. 2010;51:343–359. doi: 10.1177/0022146510378237. doi: 10.1177/0022146510378237. [DOI] [PubMed] [Google Scholar]
- Storch EA, Roberti JW. Roth DA. Factor structure, concurrent validity and internal consistency of the Beck Depression Inventory-Second Edition in a sample of college students. Depression and Anxiety. 2004;19:187–189. doi: 10.1002/da.20002. doi: 10.1002/da.20002. [DOI] [PubMed] [Google Scholar]
- Sturgeon RS. Hamley RW. Religiosity and anxiety. The Journal of Social Psychology. 1979;108:137–138. doi: 10.1080/00224545.1979.9711977. [DOI] [PubMed] [Google Scholar]
- Tepper L, Rogers SA, Coleman EM. Malony HD. The prevalence of religious coping among persons with persistent mental illness. Psychiatric Services. 2001;52:660–665. doi: 10.1176/appi.ps.52.5.660. doi: 10.1176/appi.ps.52.5.660. [DOI] [PubMed] [Google Scholar]
- Thoresen CE. Harris AHS. Spirituality and health: What's the evidence and what's needed? Annals of Behavioral Medicine. 2002;24:3–13. doi: 10.1207/S15324796ABM2401_02. doi: 10.1207/S15324796ABM2401_02. [DOI] [PubMed] [Google Scholar]
- Underwood LG. Ordinary spiritual experiences: Qualitative research, interpretive guidelines, and population distribution for the Daily Spiritual Experience Scale. Archive for the Psychology of Religion. 2006;28:181–218. [Google Scholar]
- Underwood LG. Teresi JA. The Daily Spiritual Experience Scale: Development, theoretical description, reliability, exploratory factor analysis and preliminary construct validity using health related data. Annals of Behavioral Medicine. 2002;24:22–33. doi: 10.1207/S15324796ABM2401_04. doi: 10.1207/S15324796ABM2401_04. [DOI] [PubMed] [Google Scholar]
- Vickers AJ. Analysis of variance is easily misapplied in the analysis of randomized trials: a critique and discussion of alternative statistical approaches. Psychosomatic Medicine. 2005;67:652–655. doi: 10.1097/01.psy.0000172624.52957.a8. doi: 10.1097/01.psy.0000172624.52957.a8. [DOI] [PubMed] [Google Scholar]
- Vickers AJ. Altman DG. Analysing controlled trials with baseline and follow up measurements. British Medical Journal. 2001;323:1123–1124. doi: 10.1136/bmj.323.7321.1123. doi: 10.1136/bmj.323.7321.1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wacholtz AB. Pargament KI. Is spirituality a critical ingredient of meditation? Comparing the effects of spiritual meditation, secular meditation and relaxation on spiritual, psychological, cardiac, and pain outcome. Journal of Behavioral Medicine. 2005;28:369–384. doi: 10.1007/s10865-005-9008-5. doi: 10.1007/s10865-005-9008-5. [DOI] [PubMed] [Google Scholar]
- Wacholtz A. Sambamoorthi U. National trends in prayer use as a coping mechanism for health concerns: Changes from 2002 to 2007. Psychology of Religion and Spirituality. 2011;3:67–77. doi: 10.1037/a0021598. [Google Scholar]
- Walsh R. Essential spirituality: The 7 central practices to awaken heart and mind. New York: John Wiley & Sons, Inc; 1999. [Google Scholar]
- Wampold BE. The great psychotherapy debate: Models, methods, and findings. Mahwah, NJ: Lawrence Erlbaum; 2001. doi: 10.1002/pits.10115. [Google Scholar]
- Webb M, Charbonneau AM, McCann RA. Kristin R. Struggling and enduring with God, religious support, and recovery from mental illness. Journal of Clinical Psychology. 2011;67:1161–1176. doi: 10.1002/jclp.20838. doi: 10.1002/jclp.20838. [DOI] [PubMed] [Google Scholar]
- Wiebe JS. Penley JA. A psychometric comparison of the Beck Depression Inventory-II in English and Spanish. Psychological Assessment. 2005;17:481–485. doi: 10.1037/1040-3590.17.4.481. doi: 10.1037/1040-3590.17.4.481. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Prusoff BA, Thompson WD, Harding PS. Myers JK. Social adjustment by self-report in a community sample and in psychiatric outpatients. Journal of Nervous and Mental Disease. 1978;166:317–326. doi: 10.1097/00005053-197805000-00002. [DOI] [PubMed] [Google Scholar]
- Wood AM, Maltby J, Gillett R, Linley PA. Joseph S. The role of gratitude in the development of social support, stress, and depression: Two longitudinal studies. Journal of Research in Personality. 2008;43:854–871. doi: 10.1016/j.jrp.2007.11.003. [Google Scholar]
- Worthington EL, Hook JN, Davis DE. McDaniel MA. Religion and spirituality. Journal of Clinical Psychology. 2011;67:204–212. doi: 10.1002/jclp.20760. doi: 10.1002/jclp.20760. [DOI] [PubMed] [Google Scholar]
- Xiao S, Young SD. Zhang H. Taoistic cognitive psychotherapy for neurotic patients: A preliminary clinical trial. Psychiatry and Clinical Neurosciences. 1998;52(Suppl):S238–S242. doi: 10.1111/j.1440-1819.1998.tb03232.x. [DOI] [PubMed] [Google Scholar]
- Zernicker KA, Campbell TS, Blustein PK, Fung TS, Johnson JA, Bacon SL. Carlson LE. Mindfulness-based stress reduction for the treatment of irritable bowel syndrome: A randomized wait-list controlled trial. 2012. doi: 10.1007/s12529-012-9241-6. [DOI] [PubMed]


