Summary
Physical activity is an important component in weight loss treatment and weight maintenance. We evaluated the physical activity component of two weight loss programmes, either standard care (SC) as defined by national guidelines, or a commercial programme (CP; Weight Watchers) over the period of weight loss and follow-up. 772 adults (mean body mass index: 31.4 ± 2.6 kg m−2) were recruited by primary care practices in Australia, the United Kingdom, and Germany, and randomly assigned to 12 months SC, or the CP. They were then followed up at 24 months. Change in physical activity levels were assessed by the International Physical Activity Questionnaire (IPAQ)-short form, and pedometer recordings. Both groups reported increases in physical activity using the IPAQ from baseline to 12 months and 24 months (within groups P < 0.0001) and in pedometer steps from baseline to 12 months only (within groups P < 0.0001). Differences between groups with both methods of assessment were not significant. There was a significant difference in weight loss between the groups at 12 months favouring the CP group; however, this statistical difference was not maintained at 24 months. In conclusion, despite similar increases in reported activity, there were significant differences in weight loss and regain between groups. Therefore, greater weight loss seen with the CP is unlikely to be due to increases in physical activity. Trends in pedometer steps mirrored changes in weight over time more closely than the IPAQ; however, both assessment tools have limitations. Better activity assessment measures are needed to more accurately gauge changes in physical activity during weight loss interventions.
Keywords: Commercial programme; IPAQ; obesity, pedometer
What is already known about this subject
Despite the reported efficacy of commercial programmes, there has been very little data investigating the possible mechanisms underlying the resulting weight loss.
Survey-based data has examined changes in physical activity with commercial weight management programmes but little beyond this limited assessment on intended behaviour change has been reported.
What this study adds
The current study used both a subjective and objective physical activity measure to report on various programme components from a randomized controlled trial.
It also addresses the specific amount of exercise that may be required for weight maintenance, as minimal data exists in studies of greater than 6 to 12 months duration. This is important as a better understanding of the association between physical activity patterns and body weight change is required to produce accurate clinical guidelines and to develop consistent public health messages.
Introduction
Physical activity is recommended in population guidelines for the prevention of weight gain and to improve health outcomes, and usually forms part of weight management interventions. Physical activity alone as a lifestyle intervention for weight loss has only a modest effect with a weight loss of less than 3% of initial body weight over a one year period, but it may be more pronounced when combined with dietary restriction 1. Even when weight loss is not achieved, increases in physical activity can result in significant health benefits such as reductions in abdominal fat 2 and body fat 3,4, reduction in diabetes and cardiovascular risk 5, and increased life expectancy 5,6. Studies including both dietary and exercise interventions can produce weight losses of approximately 6% of initial body weight at 12 months; however, the weight loss is generally not well maintained at later follow-up 7. Post-intervention, physical activity levels decrease over time 4,8,9. It is known that physical activity prevents greater loss of fat-free mass than is seen with dieting alone 10, and is therefore, a likely contributor to successful weight loss maintenance 1.
Our randomized controlled trial in overweight and obese adults showed that referral to a commercial weight loss programme (CP) led to significantly greater weight loss at 12 months than standard care (SC). In all three countries involved (Australia, United Kingdom, and Germany), participants referred to the CP (Weight Watchers [WW]) lost twice as much weight, and were three times more likely to lose more than 5% of initial weight, than were those who received SC 11. At 24 months (12 months after the completion of the intervention period) weight loss tended to be greater in the CP than in the SC group although accurate interpretation was confounded by high attrition 12. To date, despite the reported efficacy of commercial programmes on weight loss, there has been very little data reporting their effect on physical activity levels and the contribution that this makes to weight loss. Survey-based data has examined changes in physical activity with commercial weight management programmes 13,14, but little beyond this limited assessment on intended behaviour change has been reported. Furthermore, a better understanding of the association between physical activity patterns and body weight change is required to produce accurate clinical guidelines and to develop consistent public health messages.
This analysis considers the specific changes in physical activity that occurred during the 12-month intervention by a CP and SC as well as during a further 12-month follow-up using data from all three countries (Australia, United Kingdom and Germany). Using both a subjective and an objective measure for activity assessment, the changes in physical activity achieved with the two interventions are examined, as well as the association between physical activity and the amount of weight loss regardless of intervention group. It was expected that the larger weight loss achieved by the CP during the intervention and follow-up was in part due to a greater physical activity level.
Materials and methods
Study design and participants
The data used is from a multicentre, international randomized controlled trial with a parallel design. Participants were recruited by their primary care providers in Australia, the United Kingdom and Germany between September 2007 and December 2008. A full list of inclusion and exclusion criteria, as well as a description of the two intervention groups and trial procedures, can be found in an earlier publication reporting the primary findings from the study 11. At baseline, the mean (standard deviation [SD]) age of subjects was 47.4 (12.9) years, the mean (SD) body mass index was 31.4 (2.6) kg m−2, and 87% were females. Participants randomized to the CP received vouchers to attend a CP meeting each week for 12 months and had free access to the online tool of the provider. Those randomized to the SC group received weight loss advice delivered by a primary care professional at their local medical practice over the same period. An optional follow-up was offered to all participants at the end of the 12-month intervention period. No further intervention was prescribed and follow-up visits took place at 18 and 24 months at the research centre (Australia) or at general practices (United Kingdom and Germany). Ethical approval was received from the Royal Prince Alfred Hospital zone of the Sydney South West Area Health Service (Australia), the Nottingham Research Ethics Committee (UK) and the Faculty of Medicine of the Technische Universität München (Germany). All patients provided written informed consent. This trial is registered, number ISRCTN85485463.
Commercial programme (CP)
The CP promotes weight loss through a hypo-energetic, balanced diet based on healthy eating habits, increased physical activity and behavioural changes, primarily by providing group support. Weight loss goals were self-selected with input from the group leader, and participants were encouraged to attend weekly meetings for a ‘weigh-in’ and group discussion that included behavioural and motivational counselling. The plan promoted a 500-calorie deficit per day, with the aim of 0.5–1.0 kilogram of weight loss per week.
Standard care (SC)
SC was delivered by primary care professionals at the participant’s local general practice. Professionals delivering this intervention were provided with, and encouraged to use, national clinical guidelines for treatment 11 and were made aware of available patient literature with reference to advice on weight loss.
Outcomes
The anthropometric methods used in this study have been described previously 11. The International Physical Activity Questionnaire (IPAQ) – short form 15 was used to assess physical activity and administered to participants in all three countries at baseline, and 6, 12, 18 and 24 months, and scored using established methods 16. The data is reported as a continuous measure in median metabolic equivalent of task (MET)-minutes per week. The MET is a multiple of the resting metabolic rate that is assigned to a given activity and a MET-minutes is calculated by multiplying the MET score of an activity by the minutes performed 16.
Prior to the baseline visit, all participants in both groups were provided with a pedometer (made by Weight Watchers International, Inc., New York, NY, USA). Pedometer steps over a 7-d period were recorded by participants in their activity diaries prior to baseline, and 6 and 12-month visits in Australia, the UK and Germany. Pedometer data was also collected during the follow-up (18 and 24 months) in Australia and Germany. When calculating a participant’s average steps per day, only those days with recordings >1000 steps were included. Incomplete activity diaries (i.e. with less than 4 out of a total of 7 d recorded) were excluded from the analyses.
Statistical analyses
Statistical analysis was performed using the SPSS 19.0 software (SPSS, Chicago, IL, USA). All participants who were randomized to a treatment group and whom completed a baseline assessment were included in the final results by an intention to treat (ITT) analysis. Multiple imputations using linear regression were used to impute missing values from baseline to 12 or 24 months, respectively, and were based on the assumption that data were missing at random. Five imputed datasets were created for each variable. Quantile regression was used to compare treatment outcome between groups for the IPAQ data, and an analysis of covariance was used to compare treatment groups for the pedometer data. An analysis of variance with repeated measures was used for within group comparisons with post hoc analysis utilizing a Bonferroni correction if results were significant. A completer’s analysis was also performed, whereby only those who completed the outcome measures (measured weight and physical activity) at 12 or 24 months, respectively, were included. Analyses for differences between groups were adjusted for country (Australia, UK and Germany) and the baseline physical activity data. A two-sided P < 0.05 was considered as statistically significant. Values are presented as median (interquartile range) for the IPAQ data (as recommended by the IPAQ Research Committee 16), and as mean (SD) for pedometer steps. Subjects were also grouped according to the percentage weight loss achieved at 12 or 24 months, respectively, for completers only. Weight loss categories for this analysis were less than 0%, 0% to 4.9%, 5.0% to 9.9% and ≥10% of initial body weight. Pearson’s correlation coefficient was performed for the 12- and 24-month completers to determine whether there was a relationship between physical activity level and amount of weight loss.
Results
The characteristics of participants at baseline and follow-up have been reported previously 12. In brief, 772 participants entered the trial and completed a baseline assessment. 444 (58%) participants completed the 12-month assessment and 203 (26%) participants completed the 24-month assessment.
Weight change
As reported previously 11,12, both treatment groups lost weight from baseline to 12 and 24 months. Weight loss at 12 months was −5.9 kg for CP vs. −3.0 kg for SC (between groups; P < 0.0001), and at 24 months was −3.0 kg for CP vs. −1.9 kg for SC (between groups; P = 0.150). During the follow-up (from 12 to 24 months), both treatment groups gained weight but the weight gain was significantly greater for the CP than the SC group (adjusted difference +2.0 kg; P < 0.001).
IPAQ-short form
Total physical activity (MET-minutes per week)
Baseline IPAQ data were available for 739 participants (96%) because some participants did not complete the questionnaire or needed to be excluded from the analysis as not meeting the IPAQ scoring instructions. At 12 and 24 months, 390 (51%) and 171 (22%) participants, respectively, provided completed responses, and were included in the completer’s analyses at these time points. Total physical activity increased significantly for both groups from baseline to 12 months and from baseline to 24 months (P < 0.0001; Fig. 1). No significant differences in physical activity measured in MET-minutes per week were found between the two groups at baseline, 12 or 24 months (Table 1).
Figure 1.
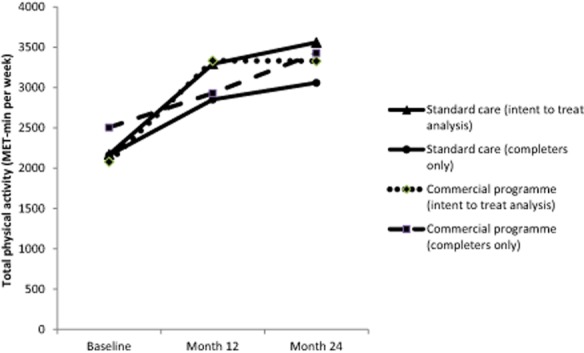
Median Metabolic Equivalent of Task (MET)-minutes per week at baseline, and 12 and 24 months for each group.
Table 1.
Median and interquartile range (25th–75th percentile) of total physical activity (MET-minutes per week) by treatment group (standard care [SC] and commercial programme [CP])
| 1a. Assessment | N | SCN = 376 | CPN = 363 | Difference between SC and CP (95% CI) | P |
|---|---|---|---|---|---|
| Baseline (intent to treat population) | 739 | 2171 (813, 4167) | 2079 (838, 4158) | −46.6 (−481.7, 388.5) | 0.83 |
| Month 12 (intent to treat population) | 739 | 3292 (1767, 5184) | 3333 (1590, 5220) | 80.1 (−353.3, 513.5) | 0.72 |
| Month 24 (intent to treat population) | 739 | 3559 (1287, 6004) | 3329 (1252, 5887) | −111.1 (−748, 525.9) | 0.73 |
| 1b. Assessment | N | SCN = 189 | CPN = 201 | Difference between SC and CP (95% CI) | P |
| Baseline (12-month completers only) | 390 | 2232 (990, 4176) | 2253 (924, 4158) | 23 (−581.9, 627.9) | 0.94 |
| Month 12 (12-month completers only) | 390 | 2994 (1584, 4746) | 2880 (1302, 5040) | 0 (−555.3, 555.3) | 0.99 |
| 1c. Assessment | N | SCN = 79 | CPN = 92 | Difference between SC and CP (95% CI) | P |
| Baseline (24-month completers only) | 171 | 2160 (924, 4398) | 2506 (977, 4455) | 589.4 (−513.1, 1691.9) | 0.29 |
| Month 12 (24-month completers only) | 164 (SC = 76; CP = 88) | 2852 (1640, 4705) | 2930 (1356, 5598) | 27.6 (−761.1, 816.2) | 0.95 |
| Month 24 (24-month completers only) | 171 | 3059 (1845, 6419) | 3429 (1419, 6132) | 16.6 (−1005.2, 1038.5) | 0.97 |
P values represent the differences between the treatment groups at each time point after adjusting for country and baseline physical activity value.
CI, confidence interval; MET, metabolic equivalent of task.
Total physical activity (min week−1)
Subjects in the CP group reported (ITT analysis) doing a mean of 205 min week−1 of combined walking, moderate and vigorous activity at baseline, which significantly increased to 255 min week−1 at 12 months and to 261 min week−1 at 24 months (Table 2). Those in the SC group reported a similar mean increase from 209 min week−1 at baseline, to 253 min week−1 at 12 months. A non-significant decrease to 238 min week−1 was reported at 24 months. No significant differences in physical activity measured in minutes per week were found between the two groups at baseline, 12 or 24 months (Table 2).
Table 2.
Mean (±standard deviation) of total physical activity (min week−1) by treatment group (standard care [SC] and commercial programme [CP])
| 2a. Assessment | N | SCN = 376 | CPN = 363 | Difference between SC and CP (95% CI) | P |
|---|---|---|---|---|---|
| Baseline (intent to treat population) | 739 | 209 (191) | 205 (194) | −1.8 (−29.5, 25.9) | 0.90 |
| Month 12 (intent to treat population) | 739 | 253 (188) | 255 (194) | 3.1 (−23.4, 29.6) | 0.82 |
| Month 24 (intent to treat population) | 739 | 238 (207) | 261 (195) | 25.4 (−1.8, 52.7) | 0.07 |
| 2b. Assessment | N | SCN = 189 | CPN = 201 | Difference between SC and CP (95% CI) | P |
| Baseline (12-month completers only) | 390 | 212 (181) | 206 (188) | −4.5 (−41.6, 32.7) | 0.81 |
| Month 12 (12-month completers only) | 390 | 236 (192) | 238 (199) | 1.6 (−36.7, 39.9) | 0.93 |
| 2c. Assessment | N | SCN = 79 | CPN = 92 | Difference between SC and CP (95% CI) | P |
| Baseline (24-month completers only) | 171 | 204 (190) | 202 (171) | −2.0 (−56.6, 52.6) | 0.94 |
| Month 12 (24-month completers only) | 164 (SC = 76; CP = 88) | 242 (203) | 251 (214) | −0.3 (−62.6, 62.0) | 0.99 |
| Month 24 (24-month completers only) | 171 | 249 (204) | 256 (211) | 3.4 (−53.9, 60.6) | 0.91 |
P values represent the differences between the treatment groups at each time point after adjusting for country and baseline physical activity value.
CI, confidence interval.
Sitting time (min per weekday)
Those in the CP group reported (ITT analysis) the same amount of time spent sitting at baseline (360 min per weekday) and 12 months (360 min), which then increased (not statistically significant) at 24 months (387 min). There was no change in sitting time in the SC group from baseline (360 min per weekday) to 12 months (360 min) to 24 months (362 min). When analysing the 24-month completers, there was a non-significant decrease in sitting minutes per weekday from baseline (390 min) to 12 months (360 min) to 24 months (325 min) for the SC group; however, this finding was not consistent for the CP group, where there was a decrease from baseline (360 min) to 12 months (300 min), and an increase to 24 months (330 min). No significant differences in sitting times were found between the two groups at baseline, 12 or 24 months.
Pedometer steps
709 (92%) participants provided complete pedometer diaries (as per requirements listed in the methods section) at baseline and thus could be included in the ITT analysis. At 12 and 24 months, 377 (Australia, UK and Germany) and 112 participants (Australia and Germany) provided complete pedometer diaries, respectively, and were included in the completer’s analyses at these time points. From both ITT and completers only analyses, both groups significantly increased their pedometer steps per day from baseline to 12 months (P < 0.0001), with a trend towards a decrease during the follow-up period (Fig. 2). For the ITT analysis, the CP group were doing a mean (SD) of 7068 (3364) steps at baseline, 8152 (4052) steps at 12 months, and 7875 (3136) steps at 24 months. The SC group were doing a mean (SD) of 7194 (3220) steps at baseline, 7936 (3831) steps at 12 months and 7624 (2952) steps at 24 months. No significant differences in average pedometer steps per day were found between the two groups at baseline, 12 or 24 months.
Figure 2.
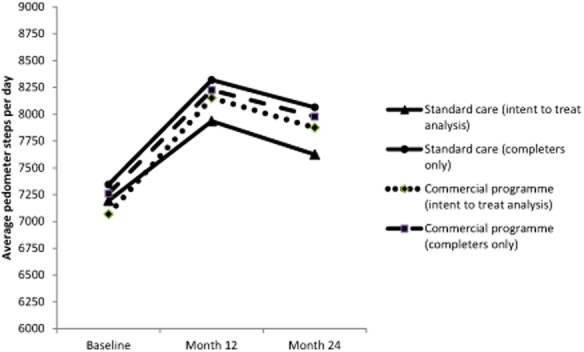
Average pedometer steps per day at baseline, and 12 and 24 months for each group.
Association between weight loss and physical activity
Regardless of the group allocation, those who completed the 12-month intervention period and whom achieved 5–9.9% weight loss (n = 97) were performing a median activity level of 2598 (interquartile range: 1294, 4638) MET-minutes per week, a mean (SD) of 208 (165) min per week (combination of walking, moderate and vigorous activity) and 8026 (4332) steps (n = 91) per day. Those who achieved ≥ 10% weight loss (n = 91) were performing a median activity level of 3444 (interquartile range: 2090, 4975) MET-minutes per week, a mean of 261 (220) min week−1 (combination of walking, moderate and vigorous activity) and 9517 (4797) steps (n = 91) per day.
When analysing those who maintained 5.0–9.9% weight loss at 24 months (n = 41), the median activity level was 3157 (interquartile range: 1928, 5981) MET-minutes per week, a mean of 217 (191) min week−1 (combination of walking, moderate and vigorous activity) and 8361 (4428) steps (n = 28) per day. For those who maintained ≥10% weight loss at 24 months (n = 34), they were performing a median of 4107 (interquartile range: 2364, 6314) MET-minutes per week, a mean of 277 (220) min week−1 (combination of walking, moderate and vigorous activity) and 9022 (3672) steps (n = 23) per day. The average pedometer steps at baseline, and 6, 12, 18 and 24 months for each category of 24-month weight loss are shown in Fig. 3.
Figure 3.
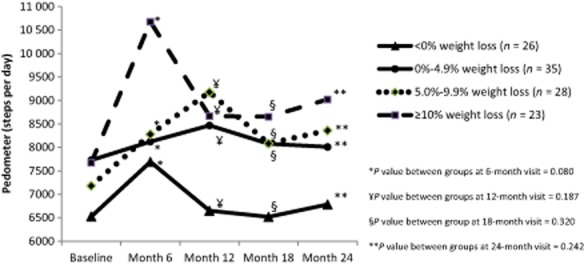
Average pedometer steps at baseline, and months 6, 12, 18 and 24 for categories of 24-month weight loss (n = 112).
There was no statistical evidence of a relationship between reported physical activity level from the IPAQ and amount of weight loss for the 12-month completers (r = 0.004; P = 0.943) or the 24-month completers (r = 0.027; P = 0.727). A weak correlation between pedometer steps and amount of weight loss was evident for the 12-month completers (r = 0.177; P = 0.001), which was less apparent for the 24-month completers (r = 0.182; P = 0.055).
Discussion
The current study used both a subjective and objective activity measure to report on various programme components from a randomized controlled trial. Little is known regarding the relative contribution of diet and activity components as contributors to weight change among individuals enrolled in commercial weight loss programmes. Furthermore, minimal data exists as to the specific amount of exercise that may be required for weight maintenance, particularly in studies of greater than 6 to 12 months duration.
In our study, there were no significant differences in activity level between the CP and SC group when assessed with the IPAQ-short form either during the intervention or follow-up period. This suggests that the primary care professionals (SC group) and the CP were both as effective in promoting and increasing physical activity levels. Both groups increased their total physical activity from baseline to 12 months. There was an increase of more than 1000 MET-minutes per week for both groups, which is probably an overestimation of the true physical activity level due to the misinterpretations noted when completing this particular questionnaire. During the study period, individuals may get better at filling in the questionnaire and hence a ‘learning effect’ may exist. As participants were not blinded to the outcome measure and are often aware that exercise has many health benefits, this may have also resulted in an over-reporting of physical activity. Individuals would have had to incorporate approximately a 45 min brisk walk for 7 d week−1 to see an increase of more than 1000 MET-minutes per week. A further increase in activity was evident between 12 and 24 months, despite a weight regain for both groups during this period. Over-reporting of physical activity by self-reported measures remains a key limitation of most studies 17. Specifically, the IPAQ-short form typically overestimates activity level as measured by objective criterion with a mean over-estimate of 84% 18.
Pedometer steps significantly increased for both groups from baseline to 12 months; however, unlike the increase in MET-minutes per week reported by both groups during the follow-up (from 12 to 24 months), a decrease in pedometer steps was recorded during this period. The decrease in pedometer steps for both groups during the follow-up better reflects the weight regain that was evident during this period. This is in support of a systematic review of the validity of the IPAQ showing only small correlations in total physical activity level with objective measuring devices 18; therefore, despite IPAQ validity being comparable with other self-report validation studies 15, the use of the questionnaire as an indicator of relative or absolute physical activity is weak. Inconsistency between the estimates from IPAQ and objective measurement tools may also be attributed to the IPAQ measuring activities longer than 10 min in duration, whereas a pedometer or accelerometer tends to measure all movement 19.
As all participants were provided with a pedometer, this may have been a simple effective message that helped promote activity awareness for all participants, regardless of the intervention. The immediate feedback provided by the pedometer has been shown to be an important factor in motivating the patient to move, with steps increasing significantly when individuals are aware that they have been provided with a pedometer (as opposed to being provided with a sealed device and told that it is a ‘body posture monitor’) and required to complete an activity log 20. Furthermore, the provision of pedometers to individuals has shown to increase physical activity levels by approximately 2500 more steps per day than non-users 21. However, the fact that pedometers act as pedagogical incentives in intervention studies aimed at increasing physical activity, also weakens their suitability as outcomes measures. A systematic review showed that the use of a pedometer is associated with significant increases in physical activity over a mean intervention of 18 weeks 21. Further evidence for the success of pedometers, particularly as a tool for general practitioners in increasing physical activity levels of their patients, comes from a study by Armit and colleagues 22. The general practitioner plus exercise specialist and pedometer intervention resulted in a greater proportion of participants meeting the activity guidelines after 24 weeks compared with the general practitioner group receiving ‘brief’ advice’. Despite not including a general practitioner plus pedometer intervention, it does suggest a benefit in focusing activity counselling on pedometer step count targets. Regardless of the promising data related to pedometer use, it is also important to note that several limitations exist with their use, particularly the type used in this study. They do not measure non-body weight-bearing activities like rowing and cycling, or decreased sitting vs. standing time. These activities often form the basis of any initial exercise prescription for the overweight and obese group with progression towards more body weight-bearing activities like the use of a treadmill incorporated later as an individual loses weight. In addition, people may often forget or avoid wearing pedometers for parts of the day. This can occur when changing clothes for structured activity or when partaking in an activity outside of their normal routine, or when wearing clothes that are less convenient for pedometer use. All of these factors would suggest that pedometers are a more accurate reflection of incidental activity due to the complex nature of different activities in daily life and the limited ability of pedometers to be able to measure all movement. Despite this, our data would suggest that this is a useful measurement done in a cheap and effective manner.
As no difference was found between groups with either the IPAQ score or the objective pedometer measure, the significant difference in weight loss between groups favouring the CP may be due to the more frequent meetings 23, or to dietary changes 24, and hence greater behavioural change. The CP group based sessions may have also resulted in greater motivation to achieve weight loss and therefore there may have been a greater effect on weight change from dietary changes. The CP has been shown to offer a clinically useful early intervention for weight management and improve the health burden of overweight and obese individuals 11,23, and therefore better identification of strategies to assist in the promotion of physical activity and exercise could enhance these health benefits.
The follow-up data (18 and 24 months) was also analysed for completers only. The high dropout rate does not allow for sufficient assumptions to be made regarding the missing data and hence large limitations exist when attempting to impute missing values. A completer’s analysis has its limitations and biases, as those who adhere to all visits are likely to be more physically active and to have achieved and maintained more weight loss than those who dropped out, but it still allows an estimate of how much exercise might be required for weight loss maintenance. However, as alluded to previously, there is a large amount of error using this self-reported measure, and the total amount of physical activity that is required to achieve and maintain a certain percentage of weight loss is also dependent on caloric intake. We found that those achieving ≥10% weight loss at 24 months were doing more activity than other weight loss categories; however, this was not statistically significant. Participants reported performing 277 min of activity per week to maintain ≥10% weight loss, which is similar to other findings. Previous research has shown that individuals sustaining a weight loss of ≥10% of initial body weight at 24 months reported approximately 1500 kilocalories week−1 or 275 min week−1 (55 min d−1 for 5 d week−1) above baseline activity levels for relatively sedentary overweight adults. This is equivalent to 1800 kilocalories week−1 or 338 min week−1 (68 min d−1 for 5 d week−1) to sustain a 10% weight loss 9. Individuals from the National Weight Control Registry who have maintained ≥ 13.6 kilograms of weight loss have reported expending 2800 kilocalories week−1 through physical activity 25.
With respect to sitting time, representative population samples from 20 countries reported a median of 300 min d−1, with an interquartile range of 180–480 min 26. In our study, median baseline values of 360 sitting minutes per day were found for both groups. There was no significant change in sedentary activity between groups. As pedometers were used in this study, we were not able to compare the self-reported sitting time with an objective measure.
Strengths and limitations
Consistent with weight loss trials, there was a large dropout rate (42%), which might be expected for a study of 12 months 9,27. However, further dropout (74%) at 24 months 12 meant that caution needed to be taken with interpretation of the data to ensure appropriate conclusions were drawn. Despite this, the data is from an international randomized controlled trial with a large sample size, and includes long-term follow-up data using two different physical activity measurement tools.
Furthermore, even though the IPAQ-short form was used to measure activity levels in this randomized controlled trial, it has been suggested that the long version may be better for research purposes as it also allows for a more detailed assessment of the separate domains of physical activity 15. Despite this, the IPAQ-short form has been shown to be more widely accepted by both investigators and survey respondents 15 and hence was used in this study. Similarly, Kim et al. found that mean effect size for levels of physical activity obtained on a continuous measure for the IPAQ-short form was comparable to or even larger than that of the IPAQ-long form, and therefore, using the short form is acceptable if not accessing domain-specific measures 19. However, rather than simply providing participants with a questionnaire to complete (which can lead to misinterpretation or lack of understanding and hence over- or under-reporting), cognitive interviewing is a recognized method for identifying problems in this situation so that respondents gain a better understanding of the questions at hand 28,29. This may have improved the data quality that was captured which is supported by a meta-analytic study whereby interviewer-administered studies had a greater mean effect size than those utilizing the self-reported measure of IPAQ 19. However, as we have baseline measurements, there is unlikely to be differences in under- or overestimation between groups.
Lastly, despite the pedometer being an objective physical activity measurement tool, participants were required to self-report their own step counts in each of the activity diaries. This was performed for 7 d prior to each clinic visit, and therefore more prone to self-report bias. Ideally, pedometer steps from a 7-d memory would have been collected by the researcher at the measurement visit. Accelerometers (particularly tri-axial) would be a more suitable objective measure whereby the data could be directly downloaded from the device by the researcher at each visit.
Conclusion
Both treatment groups increased their physical activity level. The greater weight loss seen following referral to a CP compared with SC is unlikely to be due to increases in physical activity. Pedometers, particularly as a measure of incidental activity, could be a useful motivation tool to help subjects reach these targets for both weight loss and weight maintenance. Despite this, better activity assessment measures are really needed as the methods used in this study show a lack of accuracy or precision to measure changes in physical activity during weight loss interventions.
Conflict of Interest Statement
NRF and IDC have received research grants for other clinical trials funded by Sanofi-Aventis, Allergan, Roche products, MSD and GlaxoSmithKline. IDC was an Executive Steering Committee member for the SCOUT trial, is on the organizing committee of EXSCEL trial, and has received payment for lectures from iNova Pharmaceuticals, Pfizer Australia and Servier Laboratories (Australia). SAJ has received research grants for other clinical trials from Sanofi-Aventis and Coca Cola, and is a member of the Tanita Medical Advisory Board and receives a fee for nutrition articles and lectures for Rosemary Conley Enterprises. HH is on the Advisory Board for Weight Watchers International and has received payment for lectures from Sara Lee, Novartis, Sanofi-Aventis and Bristol-Myers Squibb.
Acknowledgments
We acknowledge the assistance of Julia Stoll who provided critical analysis of the draft manuscript and to the rest of the team who contributed to the acquisition of data and follow-up of study participants (Annie Simpson, James Gerofi, Julia Stoll), and study design (Ulrike Amann-Gassner, Adrian Mander). The author’s responsibilities were as follows – NRF: acquisition of data, analysis and interpretation of data, and writing of the manuscript; KW, ALA, CH: critical review and writing of the manuscript; RS: analysis of data; SAJ, HH: study design and conception, obtained funding and critical review of the manuscript; IDC: study design and conception, obtained funding and writing the manuscript. All authors read and approved the final manuscript.
References
- 1.Jakicic JM. The effect of physical activity on body weight. Obesity (Silver Spring) 2009;17:S34–S38. doi: 10.1038/oby.2009.386. [DOI] [PubMed] [Google Scholar]
- 2.Ross R, Dagnone D, Jones PJH, et al. Reduction in obesity and related comorbid conditions after diet-induced weight loss or exercise-induced weight loss in men – a randomized, controlled trial. Ann Intern Med. 2000;133:92–103. doi: 10.7326/0003-4819-133-2-200007180-00008. [DOI] [PubMed] [Google Scholar]
- 3.Donnelly JE, Jacobsen DJ, Heelan KS, Seip R, Smith S. The effects of 18 months of intermittent vs continuous exercise on aerobic capacity, body weight and composition, and metabolic fitness in previously sedentary, moderately obese females. Int J Obes. 2000;24:566–572. doi: 10.1038/sj.ijo.0801198. [DOI] [PubMed] [Google Scholar]
- 4.Dunn AL, Marcus BH, Kampert JB, et al. Comparison of lifestyle and structured interventions to increase physical activity and cardiorespiratory fitness – a randomized trial. JAMA. 1999;281:327–334. doi: 10.1001/jama.281.4.327. [DOI] [PubMed] [Google Scholar]
- 5.Fung TT, Hu FB, Yu J, et al. Leisure-time physical activity, television watching, and plasma biomarkers of obesity and cardiovascular disease risk. Am J Epidemiol. 2000;152:1171–1178. doi: 10.1093/aje/152.12.1171. [DOI] [PubMed] [Google Scholar]
- 6.Lee CD, Blair SN, Jackson AS. Cardiorespiratory fitness, body composition, and all-cause and cardiovascular disease mortality in men. Am J Clin Nutr. 1999;69:373–380. doi: 10.1093/ajcn/69.3.373. [DOI] [PubMed] [Google Scholar]
- 7.Dansinger ML, Tatsioni A, Wong JB, Chung M, Balk EM. Meta-analysis: the effect of dietary counseling for weight loss. Ann Intern Med. 2007;147:41–50. doi: 10.7326/0003-4819-147-1-200707030-00007. [DOI] [PubMed] [Google Scholar]
- 8.Jakicic JM, Winters C, Lang W, Wing RR. Effects of intermittent exercise and use of home exercise equipment on adherence, weight loss, and fitness in overweight women – a randomized trial. JAMA. 1999;282:1554–1560. doi: 10.1001/jama.282.16.1554. [DOI] [PubMed] [Google Scholar]
- 9.Jakicic JM, Marcus BH, Lang W, Janney C. Effect of exercise on 24-month weight loss maintenance in overweight women. Arch Intern Med. 2008;168:1550–1559. doi: 10.1001/archinte.168.14.1550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ballor DL, Poehlman ET. Exercise-training enhances fat-free mass preservation during diet-induced weight-loss – a meta-analytical finding. Int J Obes. 1994;18:35–40. [PubMed] [Google Scholar]
- 11.Jebb SA, Ahern AL, Olson AD, et al. Primary care referral to a commercial provider for weight loss treatment versus standard care: a randomised controlled trial. Lancet. 2011;378:1485–1492. doi: 10.1016/S0140-6736(11)61344-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Holzapfel C, Cresswell L, Ahern AL, et al. The challenge of two year follow-up after intervention for weight loss in primary care. Int J Obes. 2013 doi: 10.1038/ijo.2013.180. .doi: 10.1038/ijo.2013.180. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pallister C, Avery A, Stubbs J, Lavin J. Influence of Slimming World’s lifestyle programme on diet, activity behaviour and health of participants and their families. J Hum Nutr Diet. 2009;22:351–358. doi: 10.1111/j.1365-277X.2009.00959.x. [DOI] [PubMed] [Google Scholar]
- 14.Furlow EA, Anderson JWA. Systematic review of targeted outcomes associated with a medically supervised commercial weight-loss program. J Am Diet Assoc. 2009;109:1417–1421. doi: 10.1016/j.jada.2009.05.003. [DOI] [PubMed] [Google Scholar]
- 15.Craig CL, Marshall AL, Sjostrom M, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35:1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- 16.IPAQ. 2010. International Physical Activity Questionnaire scoring protocol . URL http://www.ipaq.ki.se/ipaq.htm (Access date 20 January 2013)
- 17.Sallis JF, Saelens BE. Assessment of physical activity by self-report: status, limitations, and future directions. Res Q Exerc Sport. 2000;71:S1–S14. [PubMed] [Google Scholar]
- 18.Lee PH, Macfarlane DJ, Lam TH, Stewart SM. Validity of the International Physical Activity Questionnaire Short Form (IPAQ-SF): a systematic review. Int J Behav Nutr Phys Act. 2011;8 doi: 10.1186/1479-5868-8-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kim Y, Park I, Kang M. Convergent validity of the International Physical Activity Questionnaire (IPAQ): meta-analysis. Public Health Nutr. 2013;16:440–452. doi: 10.1017/S1368980012002996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Clemes SA, Matchett N, Wane SL. Reactivity: an issue for short-term pedometer studies? Br J Sports Med. 2008;42:68–70. doi: 10.1136/bjsm.2007.038521. [DOI] [PubMed] [Google Scholar]
- 21.Bravata DM, Smith-Spangler C, Sundaram V, et al. Using pedometers to increase physical activity and improve health – a systematic review. JAMA. 2007;298:2296–2304. doi: 10.1001/jama.298.19.2296. [DOI] [PubMed] [Google Scholar]
- 22.Armit CM, Brown WJ, Marshall AL, et al. Randomized trial of three strategies to promote physical activity in general practice. Prev Med. 2009;48:156–163. doi: 10.1016/j.ypmed.2008.11.009. [DOI] [PubMed] [Google Scholar]
- 23.Fuller NR, Colagiuri S, Schofield D, et al. A within-trial cost-effectiveness analysis of primary care referral to a commercial provider for weight loss treatment, relative to standard care-an international randomised controlled trial. Int J Obes. 2013;37:828–834. doi: 10.1038/ijo.2012.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Eberhard MI, Olson AD, Ambrosini AL, et al. Greater improvemements in diet quality in participants randomised to a commercial weight loss programme compared with standard care delivered in GP practices. Proc Nutr Soc. 2011;70:E252. [Google Scholar]
- 25.Klem ML, Wing RR, McGuire MT, Seagle HM, Hill JO. A descriptive study of individuals successful at long-term maintenance of substantial weight loss. Am J Clin Nutr. 1997;66:239–246. doi: 10.1093/ajcn/66.2.239. [DOI] [PubMed] [Google Scholar]
- 26.Bauman A, Ainsworth BE, Sallis JF, et al. The descriptive epidemiology of sitting a 20-country comparison using the international physical activity questionnaire (IPAQ) Am J Prev Med. 2011;41:228–235. doi: 10.1016/j.amepre.2011.05.003. [DOI] [PubMed] [Google Scholar]
- 27.Elobeid MA, Padilla MA, McVie T, et al. Missing data in randomized clinical trials for weight loss: scope of the problem, state of the field, and performance of statistical methods. PLoS ONE. 2009;4 doi: 10.1371/journal.pone.0006624. .doi: 10.1371/journal.pone.0006624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Beatty PC, Willis GB. Research synthesis: the practice of cognitive interviewing. Public Opin Q. 2007;71:287–311. [Google Scholar]
- 29.Jobe JB, Mingay DJ. Cognitive research improves questionnaires. Am J Public Health. 1989;79:1053–1055. doi: 10.2105/ajph.79.8.1053. [DOI] [PMC free article] [PubMed] [Google Scholar]


