Abstract
Objectives
The consequences of inflammatory arthritis can include depression, anxiety and low mood, reducing patients’ quality of life and increasing pressure on the healthcare system. Treatment guidelines recommend psychological support, but data are lacking on the provision available.
Methods
A postal survey concerning psychological support provision was sent to rheumatology units in 143 acute trusts across England. Nurses from 73 rheumatology units (51%) responded.
Results
Overall, 73% rated their unit's psychological support provision as ‘inadequate’ and only 4% rated it as ‘good’. Few units believed that psychological support did not fall within their remit (12%), yet only 8% had a psychologist in the team. Most units (68%) did not routinely screen patients to identify psychological difficulties. Referral to other service providers was reported in 42% of units, with 3% very satisfied with this provision. Within units, services containing elements of psychological support ranged from occupational therapy (81%) to psychology/counselling (14%). Psychological approaches used by team members ranged from shared decision making (77%) to cognitive–behavioural approaches (26%). The current barriers to providing psychological support were lack of clinical time and available training (86% and 74%, respectively), and delivery costs (74%). Future facilitators included management support (74%) and availability of skills training (74%).
Conclusions
Rheumatology units viewed psychological support provision as part of their remit but rated their overall provision as inadequate, despite some team members using psychological skills. To improve provision, clinicians’ training needs must be addressed and organizational support generated, and further research needs to define adequate psychological support provision from the patient perspective. © 2014 The Authors. Musculoskeletal Care published by John Wiley & Sons Ltd.
Keywords: Barriers and facilitators, inflammatory arthritis, psychological support provision, resources
Introduction
Inflammatory arthritis (IA) is an umbrella term for several long-term, progressive musculoskeletal diseases, including rheumatoid arthritis (RA), ankylosing spondylitis (AS), connective tissue disease (CTD), psoriatic arthritis (PsA) and systemic lupus erythematosus (SLE). RA is the most common of these diseases, affecting an estimated 580,000 people in England, with 26,000 new cases diagnosed each year (House of Commons Committee of Public Accounts, 2010). There is substantial evidence that IA can have an adverse psychological impact, including elevated levels of anxiety and depression (Treharne et al., 2007). Manifestations of anxiety include worrying, tension, rumination and avoidance behaviours – for example, in relation to pain and fatigue. Symptoms of depression include feelings of sadness, helplessness, and loss of feelings of pleasure and interest to the extent that they interfere with daily functioning (Geenen et al., 2012). Conservative figures suggest that the prevalence of depressive disorder in patients with RA ranges from 13–20% (Sheehy et al., 2006). In a systematic review and meta-analysis of 12 studies, depression was more common in patients with RA than in control respondents (Dickens et al., 2002). Although the majority of research to date has focused on serious psychological consequences such as clinical levels of anxiety and depression, it is recognized that most patients face a degree of psychological challenge. The occurrence of psychological distress that does not fulfil diagnostic criteria of anxiety and depression is estimated to be as high as 65% in patients with RA (Vriezekolk et al., 2010). Such psychological distress can be in relation to dealing with fluctuating physical symptoms (pain, fatigue, flares); restricted mobility and participation in valued activities; emotional impact (changes to roles and relationships); and managing complex medication regimens (Homer, 2005). A survey on the emotional impact of arthritis found that when arthritis pain was at its worst, 68% of respondents felt depressed and 50% felt helpless (Arthritis Care, 2011).
Research findings on the interaction of somatic and psychological factors in the development of depression and anxiety are mixed. There is growing evidence of pain and fatigue as predictors but controversy remains regarding the strength and causal direction of these associations (Nagyova et al., 2005; Wolfe and Michaud, 2009). One consistent finding is that disease status and disease activity alone are not good predictors of psychological distress (Wolfe and Hawley, 1993; Curtis et al., 2005). Influential psychological factors include illness beliefs, locus of control, social support, self-esteem, body image and coping strategies (Groarke et al., 2004; Homer, 2005; Nagyova et al., 2005; Zyrianova et al., 2011). The consequences of psychological difficulties include poorer quality of life, the loss of valued social roles, body image disturbance and a reduced capacity to work (Jenkinson, 2009). In addition to the distress experienced by patients, there is evidence that depression can increase the burden on the healthcare system, through repeated consultations, reduced treatment adherence and poorer treatment outcomes (Covic et al., 2006; Hider et al., 2009).
Many of the psychological factors influencing adaptation to IA are amenable to intervention (Astin et al., 2002). Meeting psychological support needs can improve the quality of life of those affected and can result in economic benefits as fewer healthcare resources are used (Sharpe et al., 2008; NHS confederation, 2012). This evidence has led a coalition of charities working on behalf of people with long-term conditions, including Arthritis Research UK, to urge national policy-makers and clinical commissioning groups to provide access to services such as counselling and self-management programmes. They argue that prevention of psychological difficulties and support for self-management are key to reducing the impact of these diseases on individuals and society (Arthritis Research UK, 2012). The importance of addressing psychological needs is acknowledged in treatment guidelines from the National Institute for Health and Care Excellence (NICE), which state that people with RA should be offered psychological interventions such as relaxation, stress management and cognitive coping skills, to help them adjust to living with their condition (National Institute for Health and Care Excellence, 2013). As the management of IA is still largely based in secondary care, the rheumatology team might be those best placed to provide such support (National Audit Office, 2009). In addition, the European League Against Rheumatism (EULAR) recommends that the role of the rheumatology nurse includes the provision of psychosocial and self-management support for patients with IA (van Eijk-Hustings et al., 2012). In practice, treatment of IA targets the underlying disease process and primary physical symptoms, while attention to psychological status and the psychosocial factors that might impact on the disease is inconsistent and fragmented (Gettings, 2010; Geenen et al., 2012). This was highlighted in a recent House of Commons report, which identified significant gaps and variation in access to psychological services (House of Commons Committee of Public Accounts, 2010). The present study was a first step in matching recommendations to practice by scoping the psychological support currently available in rheumatology units across England and identifying the factors that help or hinder provision. Scoping studies provide a broad overview of a topic, drawing on evidence from a range of sources, including key informants and stakeholders (Abelson et al., 2008).
The research team, comprising rheumatology and psychology clinicians, patient partners and researchers, undertook a brief descriptive survey using a questionnaire of closed and open-ended questions. The questionnaire was developed during research team discussions and shown to local rheumatology clinicians for feedback on its clarity and relevance. We defined ‘psychological support’ as covering any services that addressed social or emotional challenges in relation to rheumatic disease; examples could include psycho-educational group programmes, clinics to support behaviour change and self-management, or the incorporation of psychosocial approaches into routine consultations by members of the rheumatology team. The aims were to identify the psychological support available in rheumatology units across England, and to identify key factors influencing service provision.
Participants and methods
The survey probed three areas in relation to psychological support in rheumatology units: current practice and provision, psychological skills within the team, and the resources required to deliver services. It was estimated that it would take approximately five minutes to complete. Ethics approval to conduct the survey was obtained from the Faculty Research Ethics Committee at the University of the West of England, Bristol (reference: HLS/12/06/70). Rheumatology units were identified via the NHS Choices website, which lists the acute trusts in England. Within each trust, contact details for their rheumatology unit were available under ‘Departments and Services’. A total of 143 questionnaires were sent, addressed to the ‘nurse specialist’ or a named nurse, where known (19 hospitals). Nurses were also offered the option of an email version of the survey.
Results
Nurses from 73 units (51%) responded, including 15 using the email version. Overall, 73% of respondents rated their unit's psychological support provision as inadequate and 4% rated it as good (18% as adequate, 4% not sure and 1% did not answer) (Figure 1).
Figure 1.
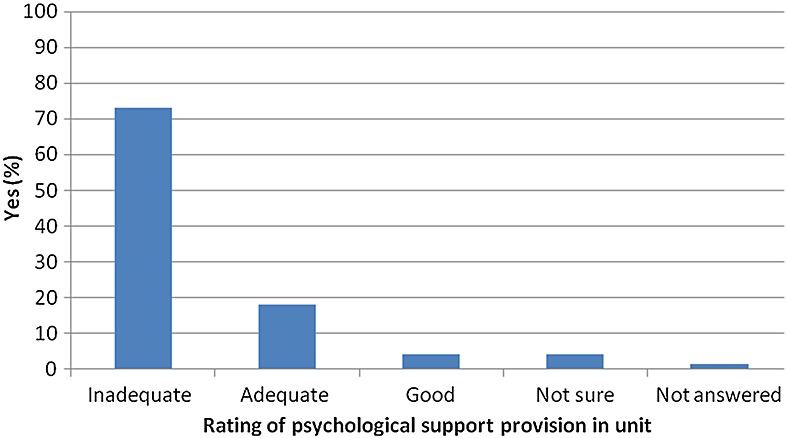
Overall rating of psychological support provision
Current practice and provision
While only 12% of respondents reported a team view that psychological support did not fall within the unit's remit and only 19% expressed a preference to refer to psychological support elsewhere, very few rheumatology teams had a psychologist (8%). In relation to the detection of psychological difficulties, 27% units reported routinely screening patients, while 34% sometimes screened (33% did not, and 6% were not sure). Among 42 (58%) respondents who answered an open-ended question about screening processes, 31 (42%) indicated that assessments were informal (for example, asking about mood and coping in clinic) and 11 (15%) reported that that they also used formal measures, such as the Arthritis Impact Measurement Scales 2 (AIMS2) (Meenan et al., 1980), the Hospital and Anxiety Depression Scale (HADS) (Zigmond and Snaith, 1983), the 36-Item Short Form Health Survey (SF36) (Ware and Sherbourne, 1992) or a two-question depression screening tool. Referrals to other service providers for psychological support, including clinical psychology services, GPs, Increasing Access to Psychological Therapies (IAPT) services, and liaison psychiatry, were reported in 42% of units, with 32% not referring, 22% sometimes referring and 4% not sure. Where referrals were made, 3% were very satisfied with the provision (21% fairly; 29% not very), while 14% were not sure and 33% did not answer. Open-ended data about the reasons for dissatisfaction showed that they included long waiting lists, a limited service and local variations in availability.
Services that contained some elements of psychological support and were available within the responding rheumatology units included occupational therapy (81%), patient education programmes (58%), pain management clinics (30%), facilitated peer support groups for patients (30%), self-management clinics (27%) and psychology/counselling (14%) (Figure 2). Open-ended responses describing any other services available in the unit included nurse-led clinics following diagnosis, one-to-one counselling by a rheumatology clinical nurse specialist, psychological assessment for patients with RA as part of their annual review and support from the clinical nurse specialists via the telephone helpline.
Figure 2.
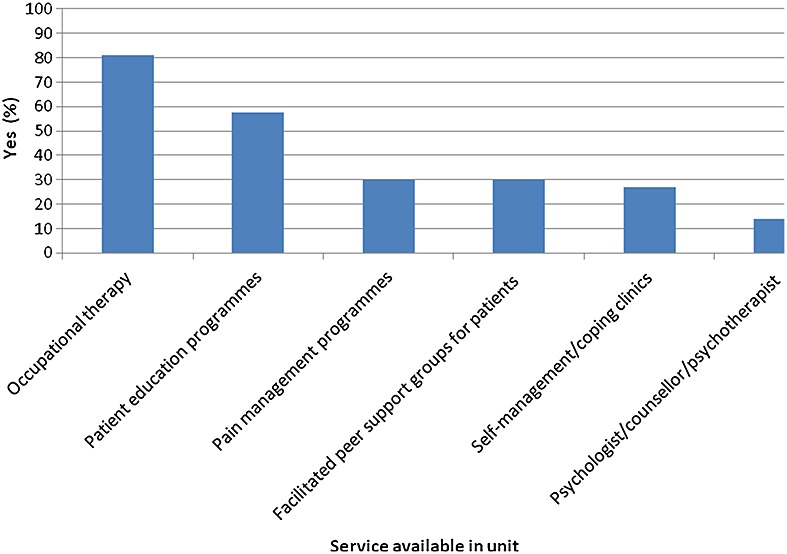
Services available that contain elements of psychological support
Psychological skills within the team
Respondents reported that a range of psychological approaches were used by team members in their clinical role – mainly shared decision-making and pain management skills (77% and 63%, respectively), followed by counselling (48%) and relaxation/mindfulness techniques (36%), while a quarter used cognitive–behavioural (CB) approaches (26%) or motivational interviewing (MI; 25%) (Figure 3). Responses to an open-ended question to describe any other skills showed that some team members were providing psychological support without formal training in specific approaches, and some clinicians expressed a need to receive additional support to utilize the training they had undertaken.
Figure 3.
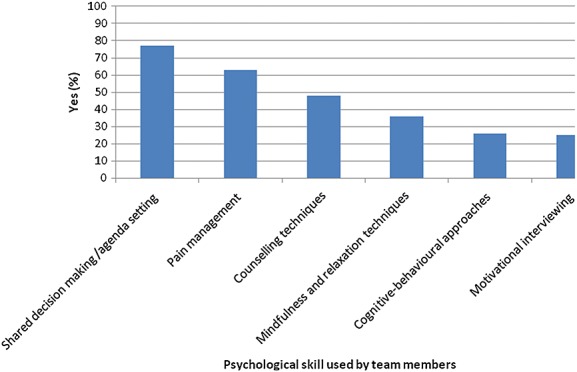
Psychological skills within the rheumatology team
The resources required to deliver services
Respondents identified the main current barriers to providing psychological support as a lack of clinical time, appropriately trained clinicians and available training (86%, 71% and 74%, respectively), and the costs of delivery (74%) (Figure 4). Open-ended data about any other barriers identified the following issues:
Difficulty getting commissioners to support and fund these services
The need for more nurses to support the number of patients requiring psychological support
The pressure to reduce the number of follow-up appointments
A concern that there was no one to refer the patient to if problems were identified
An emphasis on addressing physical limitations of the condition
Patients’ reluctance to acknowledge and talk about psychological issues.
Figure 4.
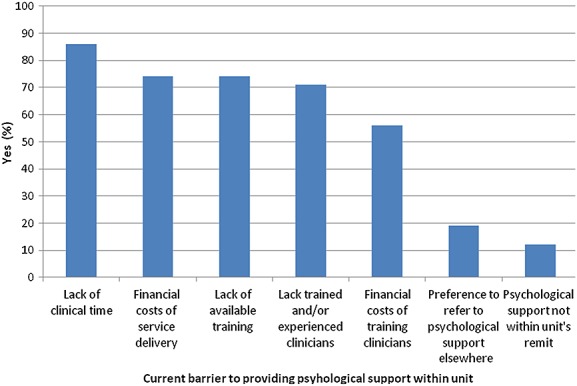
Current barriers to psychological support provision in unit
Respondents identified that in the future, the main facilitators of support provision would be management and team support for psychological services (74%; 68%), the availability of skills training for clinicians (74%), and integration of psychological support into the care pathway (73%) (Figure 5). Responses to an open-ended question about any other potential facilitators included the importance of recognition by the clinical commissioning groups that psychological support is an important part of patient care.
Figure 5.
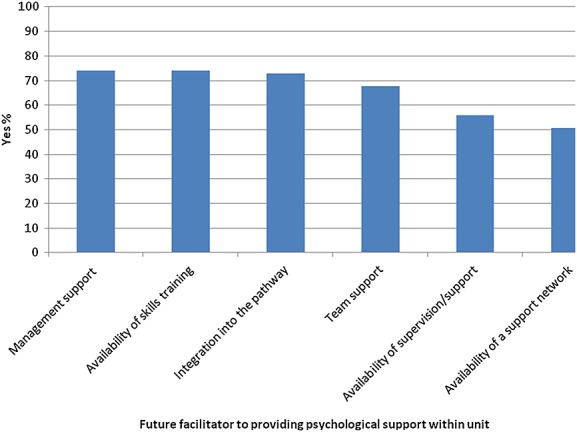
Future facilitators to psychological support provision in unit
In relation to current resources, the responses of the three units which rated their provision as good showed that their available services included patient education, pain management, occupational therapy and a psychologist/counsellor/psychotherapist. One of these units had a dedicated health psychologist for the rheumatology team, another delivered facilitated peer support groups for patients and the third offered self-management/coping clinics for patients. In addition, one of these units made referrals to a psychologist for one-to-one or group sessions and was ‘very satisfied’ with the service provision. There were numerous psychological skills in the teams at these three units; in two of the units these included CB approaches, pain management and mindfulness/relaxation techniques, and in one unit it included MI and counselling techniques.
Discussion
The aim of psychological care in IA is to prevent and reduce distress which might be causing a negative impact on patients’ wellbeing and ability to manage their illness and its impact effectively. The postal survey in the present study was designed to scope the psychological support provision available in rheumatology units across England. It was undertaken because treatment guidelines recommend that patients are offered psychological support, yet there are no data on current provision. The claim has been made that in long-term conditions generally, patients do not receive care that addresses both their physical and psychological needs for reasons, including: a lack of clinician training in psychological awareness, assessment and management, and patchy service design and provision (NHS Confederation, 2012). The present survey found that the majority of respondents supported this view and rated their unit's current psychological support provision as inadequate.
Historically, rheumatology services have been configured around a biomedical model of care that focused primarily on ‘physical’ symptoms (Abelson et al., 2008). Increasingly, the need to heighten rheumatology teams’ awareness of the psychological aspects of IA and to find ways of incorporating psychological approaches into routine clinical practice has been acknowledged (Keefe and Somers, 2010). This is based on the understanding that disease management is strengthened when psychological input is part of care (Naylor et al., 2013). The present findings suggest that respondents were aware of the psychological challenges faced by patients with IA and viewed addressing them as part of their remit, but struggled to deliver adequate services. Respondents reported that the main challenges included a lack of clinical time and available training, and the cost of delivering psychological support. In their view, service improvements could be facilitated by management support and increased skills training.
A first step to meeting psychological needs is the detection of psychological distress (Currid, 2012). Although it has been proposed that screening should become part of routine clinical care in rheumatology (Nichol and Zhang, 2005), this was not common practice in the majority of units surveyed. Once needs have been determined, the question arises of who addresses them and in which setting. This survey found that very few rheumatology teams had a psychologist, with almost half of respondents referring patients to other service providers. There were low levels of satisfaction with these referrals, often due to difficulty in accessing appropriate services in a timely manner. In addition, over one-third of respondents did not state whether or not they were satisfied. This might indicate that once the referral had been made, the rheumatology team was not informed of the subsequent outcome. In a stepped approach to care, patients are treated at the lowest appropriate intervention in the first instance, only stepping up to more intensive or specialist services as clinically required (Bower and Gilbody, 2005). This offers clinical and financial advantages that can benefit patients, local trusts and commissioners. A model of enhanced support provision in rheumatology could involve a two-pronged approach: developing the psychology-based skills and confidence of rheumatology clinicians to support the majority of patients who do not require intense input; plus strengthening links with local specialist services (e.g. clinical psychology and liaison psychiatry) for the minority of patients experiencing high levels of psychological difficulty. This would fit well with recent research supporting the idea that the rheumatology team, with their understanding of IA and its treatment, can play a vital therapeutic role in helping patients to increase their sense of control and improve their quality of life (Hill and Ryan, 2000; Dures and Gilbody, 2012). It would also reflect EULAR recommendations that specialist and practice nurses and other allied health professionals should be trained to provide support to patients with IA on managing the emotional impact of their condition (van Eijk-Hustings et al., 2012). A focus on developing appropriate training would fit with respondents’ identification of a lack of available training as a current barrier to psychological support provision. Just over a quarter of units reported delivering self-management clinics and only 14% offered counselling, suggesting that these approaches are still not common practice. Although training clinicians to incorporate psychology skills into their role is a fairly new area within rheumatology, there is evidence emerging that training can impact positively on clinicians’ confidence to address psychosocial issues in the consultation (Dures et al., 2014). The efficacy of non-psychologists using a range of less intensive skills and approaches to support patients is currently being evaluated in several clinical areas, such as palliative care and chronic obstructive pulmonary disorder (Mannix et al., 2006; Heslop et al., 2013).
The survey found that even those units whose team members used some psychological approaches, typically rated their provision as inadequate. One possible explanation is that respondents felt that provision was inadequate in relation to supporting a particular group of patients – for example, those with higher levels of distress. This would reinforce a stepped-care strategy of improving access to specialist psychology services. Another possible explanation is the role and influence of the wider team on the implementation of psychologically informed practice. For example, research found that shared decision making was less effectively implemented when it was not a whole team activity and there were diverse and conflicting attitudes among team members (King et al., 2013). The perceived barrier of a lack of managerial support contributes to the evidence of the need to adopt a whole-systems model, based on the requirements of patients, clinicians and organizations, when introducing changes to clinical practice (Eaton et al., 2012). Research with GPs concluded that to utilize fully their training in patient-centred approaches, they required the support of practice level systems and structures (Robertson et al., 2013).
Several limitations to the present study have implications for the generalizability of the conclusions that can be drawn. In the majority of cases, the survey packs were addressed to the ‘nurse specialist’, who was not named. Among the units that did not respond (49%), it is not known whether they chose not to participate or whether the pack did not reach the addressee. For those who took part, it is not known whether they consulted colleagues before responding on behalf of the team, or whether answers reflected their individual perceptions of service provision – for example, the extent of routine screening or satisfaction with other service providers. A definition of psychological support was included in the survey, but the questions and the terminology used might have been interpreted differently between respondents. In the final question, respondents were asked to rate the adequacy of their unit's psychological support provision; this was a subjective evaluation as no set criteria were provided. In addition, the survey asked about the support available within rheumatology units but it is possible that, in some locations, team boundaries are not clear cut – for example, occupational therapists who work in several hospital departments. Strengths of the study included the high number of units in England that were approached, and the input from patient partners (JC and AP) in the design and interpretation of the survey.
Conclusions
The present scoping study on psychological support in rheumatology reinforced the evidence from a range of long-term conditions that service provision is patchy, and suggests that NICE treatment guidelines are not being met. Most rheumatology units viewed psychological support provision as part of their remit but perceived a lack of resources in relation to time, training and cost. Despite some team members using psychological skills in their role, units rated their overall provision as inadequate. To improve provision requires a whole-systems approach that addresses the training needs of clinicians and teams, understands patients’ views on services, and builds organizational support for implementation. The lack of psychologists in rheumatology units, the low levels of satisfaction with other service providers, and the EULAR recommendation that nurses provide psychosocial support all highlight the value of testing whether the usual team can be effective in this capacity. Further research is needed to understand what constitutes adequate psychological support provision from clinical and patient perspectives, and whether patients perceive that they are being offered this.
Acknowledgments
The authors thank the rheumatology nurses who participated in the study. Grant support for the study was provided by Arthritis Research UK, Grant number 19755.
REFERENCES
- Abelson B, Rupel A, Pincus T. Limitations of a biomedical model to explain socioeconomic disparities in mortality of rheumatic and cardiovascular diseases. Clinical and Experimental Rheumatology. 2008;26(Suppl. 51):S25–S34. [PubMed] [Google Scholar]
- Arthritis Care. Arthritis hurts: The emotional impact of arthritis. London: Arthritis Care; 2011. [Google Scholar]
- Arthritis Research UK. Twice as likely: Putting long term conditions and depression on the agenda. 2012. Available at http://www.arthritisresearchuk.org/news/press-releases/2012/april/twice-as-likely-call-for-better-care-and-support-for-people-with-long-term-conditions-and-depression.aspx [Accessed 19 March 2014]
- Astin J, Beckner W, Soeken K, Hochberg M, Berman B. Psychological interventions for rheumatoid arthritis: A meta-analysis of randomized controlled trials. Arthritis and Rheumatology. 2002;47:291–302. doi: 10.1002/art.10416. [DOI] [PubMed] [Google Scholar]
- Bower P, Gilbody S. Stepped care in psychological therapies: Access, effectiveness and efficiency. British Journal of Psychiatry. 2005;186:11–17. doi: 10.1192/bjp.186.1.11. [DOI] [PubMed] [Google Scholar]
- Covic T, Tyson G, Spencer D, Howe G. Depression in rheumatoid arthritis patients: Demographic, clinical, and psychological predictors. Journal of Psychosomatic Research. 2006;60:469–76. doi: 10.1016/j.jpsychores.2005.09.011. [DOI] [PubMed] [Google Scholar]
- Currid T. Meeting the psychological needs of the physically ill. Nursing Times. 2012;108:22–5. [PubMed] [Google Scholar]
- Curtis R, Groarke A, Coughlan R, Gsel A. Psychological stress as a predictor of psychological adjustment and health status in patients with rheumatoid arthritis. Patient Education and Counselling. 2005;59:192–8. doi: 10.1016/j.pec.2004.10.015. [DOI] [PubMed] [Google Scholar]
- Dickens C, McGowan L, Clark-Carter D, Creed F. Depression in rheumatoid arthritis: A systematic review of the literature with meta-analysis. Psychosomatic Medicine. 2002;64:52–60. doi: 10.1097/00006842-200201000-00008. [DOI] [PubMed] [Google Scholar]
- Dures E, Hewlett S. Cognitive-behavioural approaches to self-management in rheumatic disease. Nature Reviews Rheumatology. 2012;8:553–9. doi: 10.1038/nrrheum.2012.108. [DOI] [PubMed] [Google Scholar]
- Dures E, Hewlett S, Ambler N, Jenkins R, Clarke J, Gooberman-Hill R. Rheumatology clinicians' experiences of brief training and implementation of skills to support patient self-management. BMC Musculoskeletal Disorders. 2014;15:108. doi: 10.1186/1471-2474-15-108. DOI: 10.1186/1471-2474-15-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton S, Collins A, Coulter A, Elwyn G, Grazin N, Roberts S. Putting patients first. British Medical Journal. 2012;344:e2006. doi: 10.1136/bmj.e2006. [DOI] [PubMed] [Google Scholar]
- van Eijk-Hustings Y, van Tubergen A, Boström C, Braychenko E, Buss B, Felix J, Firth J, Hammond A, Harston B, Hernandez C, Huzjak M, Korandová J, Kukkurainen ML, Landewé R, Mezieres M, Milincovic M, Moretti A, Oliver S, Primdahl J, Scholte-Voshaar M, de la Torre-Aboki J, Waite-Jones J, Westhovens R, Zangi HA, Heiberg T, Hill J EULAR. EULAR recommendations for the role of the nurse in the management of chronic inflammatory arthritis. Annals of the Rheumatic Diseases. 2012;71:13–19. doi: 10.1136/annrheumdis-2011-200185. [DOI] [PubMed] [Google Scholar]
- Geenen R, Newman S, Bossema E, Vriezekolk J, Boelen P. Psychological interventions for patients with rheumatic diseases and anxiety or depression. Best Practice and Research Clinical Rheumatology. 2012;26:305–19. doi: 10.1016/j.berh.2012.05.004. [DOI] [PubMed] [Google Scholar]
- Gettings L. Psychological well-being in rheumatoid arthritis: A review of the literature. Musculoskeletal Care. 2010;8:99–106. doi: 10.1002/msc.171. [DOI] [PubMed] [Google Scholar]
- Groarke A, Curtis R, Coughlan R, Gsel A. The role of perceived and actual disease status in adjustment to rheumatoid arthritis. Rheumatology. 2004;43:1142–9. doi: 10.1093/rheumatology/keh262. [DOI] [PubMed] [Google Scholar]
- Heslop K, Newton J, Baker C, Burns G, Carrik-Sen D, De Soyza A. Effectiveness of cognitive behavioural therapy (CBT) interventions for anxiety in patients with chronic obstructive pulmonary disease (COPD) undertaken by respiratory nurses. BMC Pulmonary Medicine. 2013;13:62. doi: 10.1186/1471-2466-13-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hider S, Tanveer W, Brownfield A, Mattey D, Packham J. Depression in RA patients treated with anti-TNF is common and under-recognized in the rheumatology clinic. Rheumatology. 2009;48:1152–4. doi: 10.1093/rheumatology/kep170. [DOI] [PubMed] [Google Scholar]
- Hill J, Ryan S. Rheumatology. A Handbook for Community Nurses. London: Whurr Publishers Ltd; 2000. [Google Scholar]
- Homer D. Addressing psychological and social issues of rheumatoid arthritis within the consultation: A case report. Musculoskeletal Care. 2005;3:54–9. doi: 10.1002/msc.26. [DOI] [PubMed] [Google Scholar]
- House of Commons Committee of Public Accounts. Services for people with rheumatoid arthritis. London: The Stationery Office Limited; 2010. HC46. [Google Scholar]
- Jenkinson C. The psychological well-being of patients with rheumatoid arthritis. British Journal of Anaesthetic and Recovery Nursing. 2009;10:47–50. [Google Scholar]
- Keefe F, Somers T. Psychological approaches to understanding and treating arthritis pain. Nature Reviews Rheumatology. 2010;6:10–216. doi: 10.1038/nrrheum.2010.22. [DOI] [PubMed] [Google Scholar]
- King E, Taylor J, Williams R, Vanson T. The MAGIC programme: Evaluation. London: The Health Foundation; 2013. [Google Scholar]
- Mannix K, Blackburn I, Garland A, Gracie J, Moorey S, Reid B, Standart S, Scott J. Effectiveness of brief training in cognitive-behavioural therapy techniques for palliative care practitioners. Palliative Medicine. 2006;20:579–84. doi: 10.1177/0269216306071058. [DOI] [PubMed] [Google Scholar]
- Meenan R, Gertman P, Mason J. Measuring health status in arthritis: The Arthritis Impact Measurement Scales. Arthritis and Rheumatism. 1980;23:146–52. doi: 10.1002/art.1780230203. [DOI] [PubMed] [Google Scholar]
- Nagyova I, Stewart R, Macejova Z, van Dijk J, van den Heuvel W. The impact of pain on psychological well-being in rheumatoid arthritis: The mediating effects of self-esteem and adjustment to disease. Patient Education and Counselling. 2005;58:55–62. doi: 10.1016/j.pec.2004.06.011. [DOI] [PubMed] [Google Scholar]
- National Audit Office. Services for people with rheumatoid arthritis. London: National Audit Office Press Office; 2009. ( http://www.nao.org.uk) [Google Scholar]
- National Institute for Health and Care Excellence. Rheumatoid arthritis: The management of rheumatoid arthritis in adults. 2013. CG79 issued February 2009, modified August 2013. Available at http://www.nice.org.uk/CG79 [Accessed 19 March 2014]
- Naylor C, Imison C, Addicott R, Buck D, Goodwin N, Harrison T, Ross S, Sonola L, Tian Y, Curry N. Transforming our health care system. 2013. Available at http://www.kingsfund.org.uk [Accessed 19 March 2014]
- NHS Confederation. Long-term health gains: Investing in emotional and psychological wellbeing for patients with long-term conditions and medically unexplained symptoms. 2012. Issue 23. Available at http://www.nhsconfed.org/publications [Accessed 19 March 2014]
- Nichol M, Zhang L. Depression and health-related quality of life in patients with rheumatoid arthritis. Expert Review of Pharmacoeconomics and Outcomes Research. 2005;5:645–53. doi: 10.1586/14737167.5.5.645. [DOI] [PubMed] [Google Scholar]
- Robertson S, Witty K, Braybrook D, Lowcock D, South J, White A. ‘It's coming at things from a very different standpoint’: Evaluating the ‘Supporting Self-Care in General Practice Programme’ in NHS East of England. Primary Health Care Research and Development. 2013;14:113–25. doi: 10.1017/S1463423612000151. [DOI] [PubMed] [Google Scholar]
- Sharpe L, Allard S, Sensky T. Five-year followup of a cognitive–behavioral intervention for patients with recently-diagnosed rheumatoid arthritis: Effects on health care utilization. Arthritis and Rheumatism. 2008;59:311–16. doi: 10.1002/art.23312. [DOI] [PubMed] [Google Scholar]
- Sheehy C, Murphy E, Barry M. Depression in rheumatoid arthritis – Underscoring the problem. Rheumatology. 2006;45:1325–7. doi: 10.1093/rheumatology/kel231. [DOI] [PubMed] [Google Scholar]
- Treharne G, Lyons A, Booth D, Kitas G. Psychological well-being across 1 year with rheumatoid arthritis: Coping resources as buffers of perceived stress. British Journal of Health Psychology. 2007;12:323–45. doi: 10.1348/135910706X109288. [DOI] [PubMed] [Google Scholar]
- Vriezekolk J, Eijsbouts A, Evers A, Stenger A, Van Den Hoogen F, Van Lankveld W. Poor psychological health status among patients with inflammatory rheumatic diseases and osteoarthritis in multidisciplinary rehabilitation: Need for a routine psychological assessment. Disability and Rehabilitation. 2010;32:836–44. doi: 10.3109/09638280903323250. [DOI] [PubMed] [Google Scholar]
- Ware J, Sherbourne C. The MOS 36-item short-form health survey (SF-36) 1: Conceptual framework and item selection. Medical Care. 1992;30:473–83. [PubMed] [Google Scholar]
- Wolfe F, Hawley D. The relationship between clinical activity and depression in rheumatoid arthritis. Journal of Rheumatology. 1993;20:2032–7. [PubMed] [Google Scholar]
- Wolfe F, Michaud K. Predicting depression in rheumatoid arthritis: The signal importance of pain extent and fatigue, and comorbidity. Arthritis and Rheumatism. 2009;61:667–73. doi: 10.1002/art.24428. [DOI] [PubMed] [Google Scholar]
- Zigmond A, Snaith R. The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica. 1983;67:361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- Zyrianova Y, Kelly B, Sheehan J, McCarthy C, Dinan T. The psychological impact of arthritis: The effects of illness perception and coping. Irish Journal of Medical Science. 2011;180:203–10. doi: 10.1007/s11845-010-0522-2. [DOI] [PubMed] [Google Scholar]


