Abstract
The impact of an acute coronary syndrome (ACS) event, such as an acute myocardial infarction (MI), is not limited to the acute management phase; patients face an elevated risk of residual atherothrombotic events that commonly requires chronic management for months or even years. Significant advances have been made in both the acute and chronic management of patients with acute MI over the past decade, resulting in improved prognoses. One of the hallmarks of modern treatment strategies is more aggressive antiplatelet treatment regimens. However, the risks of further ACS events, stroke and premature death remain elevated in these patients, and addressing this residual risk is challenging owing to interpatient variability, differences in management strategies between centres and countries, incomplete understanding of the specific pathophysiology of post-ACS thrombosis and limitations of current therapeutic approaches. The recent approval in Europe of the direct oral anticoagulant rivaroxaban for use in this setting in combination with clopidogrel and acetylsalicylic acid offers another strategy to consider in the management of these patients, and clinical strategies in this area continue to evolve. In this review, we chart the progress made over the past decade in reducing the burden of secondary thromboembolic events after acute MI and discuss the current position of and future perspectives on the inclusion of oral anticoagulants into care pathways in this setting.
Keywords: acute coronary syndrome, anticoagulants, mortality, myocardial infarction, stent, thrombosis
Introduction
Acute coronary syndrome (ACS) comprises myocardial infarction (MI) and unstable angina (UA) arising from the obstruction of the coronary arteries, usually as a result of a coronary thrombosis 1. After the acute management of an ACS event, patients remain at increased risk of secondary atherothrombotic events, including recurrent ACS events and stroke, and continue to face an increased risk of premature death 2,3.
Preventing a recurrence of life-threatening thrombotic events is a critical part of the ongoing management of these patients 1,4. However, prevention of secondary thrombotic events after an ACS event remains challenging, owing to interpatient variability, differences in management strategies between centres and countries, incomplete understanding of the specific pathophysiology of post-ACS thrombosis and limitations of current therapeutic approaches.
A decade ago, standard care involved an approach targeted primarily at inhibiting platelet activation – using acetylsalicylic acid (ASA) or the emerging P2Y12 inhibitors – in some patients 5–7. Anticoagulation with warfarin was also recommended for some patient subgroups. At that time, death rates in the year after an ACS event were high 8: a prospective registry for the period 2002–2003 found that 9% of all patients had died in the 12 months after an acute ischaemic event and almost 16% experienced a secondary MI or died 9. Since then, the benefits of a dual-pathway (anticoagulation + antiplatelet) approach to secondary prevention after ACS have become more evident and this approach is now recommended in evidence-based guidelines 1,10, but the increased risk of bleeding and the practical management challenges associated with warfarin use have continued to limit the implementation of this approach.
During the same period, major advances have been made with antiplatelet agents, in both optimizing the use of clopidogrel and introducing newer platelet-targeted drugs. This optimization of dual antiplatelet (DAPT) regimens has contributed to the marked reductions in post-ACS event rates and deaths in more recent years 11–15. However, there remains a sizeable unmet need in secondary prevention of ischaemic events after ACS, with estimates suggesting that up to 14% of patients will experience a recurrent cardiovascular (CV) event in the year after an acute ACS event 16. This residual recurrence rate has fuelled the continued evaluation of the dual-pathway approach to secondary prevention in this setting.
The aim of this review is to examine the rationale for oral anticoagulation after an MI with the aim of preventing secondary thrombotic events, thereby reducing the wider burden of ACS.
The Dual-Pathway Approach to Preventing Recurrent Events After Myocardial Infarction
Prevention of thrombotic events after an acute ACS event, such as an MI, is a critical component of the ongoing care for these patients. An understanding of the biologic processes that underlie the persistent risk of thrombus formation after an acute ACS event provides a rationale for incorporating inhibition of thrombin generation or activity into the pharmacologic management regimen for such patients.
Acute coronary syndrome events are most often a result of thrombus formation after atherosclerotic plaque disruption (either plaque rupture or plaque erosion) 17,18. Passing platelets adhere to the exposed subendothelial proteins, resulting in their aggregation; tissue factors released by these newly formed plaques initiate coagulation and thrombin generation (Figure 1) 19,20. Increased thrombin levels result in further thrombus growth (as platelet aggregation continues) and the stabilization of the resulting thrombi (through the conversion of fibrinogen to fibrin). The increasing thrombin levels trigger further thrombus growth, which in turn drives further thrombin generation. In addition to these localized events, thrombus formation is accompanied by systemic persistent thrombin generation that lasts much longer than the residual platelet activation that typically follows an MI 20.
Figure 1.
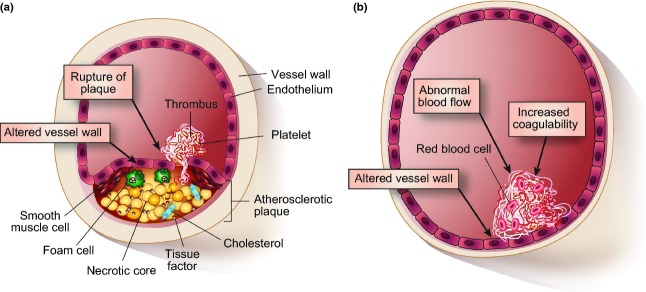
Triggers of (a) arterial thrombosis and (b) venous thrombosis 20.
Clinical studies have shown that long-term DAPT with ASA and an antiplatelet such as clopidogrel, prasugrel or ticagrelor reduces the risk of death from CV causes, nonfatal MI or stroke after an acute ACS event 21–23. The first of the antiplatelets to demonstrate a benefit was clopidogrel. In the Clopidogrel in Unstable Angina to Prevent Recurrent Events (CURE) trial, 12 562 patients who presented within 24 h of the onset of ACS symptoms were randomly assigned to receive either clopidogrel (300 mg loading dose then 75 mg once daily) or placebo, in addition to ASA 23. During the 12 months of follow-up, significantly fewer patients assigned to the clopidogrel + ASA arm experienced the composite endpoint of nonfatal MI, stroke or death from CV causes than patients assigned to the ASA-only arm [9.3% vs. 11.4%; relative risk 0.80; 95% confidence interval (CI) 0.72–0.90; P < 0.001]. In 2007, the results of the Trial to Assess Improvement in Therapeutic Outcomes by Optimizing Platelet Inhibition with Prasugrel–Thrombolysis in Myocardial Infarction (TRITON-TIMI) 38 study were reported 22. In this study, 13 608 patients with moderate- to high-risk ACS scheduled for percutaneous coronary intervention received either clopidogrel (300 mg loading dose then 75 mg once daily) or prasugrel (60 mg loading dose then 10 mg once daily) in addition to ASA. Fewer patients in the prasugrel arm experienced the composite endpoint of nonfatal MI, nonfatal stroke or death from CV causes than patients in the clopidogrel arm (9.9% vs. 12.1%; hazard ratio [HR] 0.81; 95% CI 0.73–0.90; P < 0.001). Most recently, the results of the Study of Platelet Inhibition and Patient Outcomes (PLATO) of ticagrelor in 18 624 patients hospitalized with an ACS showed that the same composite endpoint as in the CURE trial (nonfatal MI, stroke or death from CV causes) occurred significantly less frequently among patients treated with ASA + ticagrelor (loading dose 180 mg then 90 mg twice daily) than among those treated with ASA + clopidogrel (loading dose 300–600 mg then 75 mg once daily) for up to 1 year (9.8% vs. 11.7%; HR 0.84; 95% CI 0.77–0.92; P < 0.001) 21. All three antiplatelets offer significant benefits to patients after an ACS event compared with ASA alone in terms of reducing the risk of nonfatal MI, nonfatal stroke or death from CV causes; however, even with a DAPT approach, a residual risk of these adverse outcomes persists for a significant proportion of patients. Therefore, it would seem that although antiplatelet-only regimens address the platelet activation that occurs after an acute MI, they are insufficient to eliminate the increased risk of subsequent thrombus formation. A likely reason for this may be that even the newer antiplatelet agents do not address the persistent procoagulant state owing to the prolonged elevation of thrombin generation that is apparent after an acute MI.
Interfering in the thrombin pathway, either directly or indirectly, has emerged as an approach that may have an impact on the formation of thrombi and may also influence platelet activation to some extent – a so-called dual-pathway approach. However, despite evidence that anticoagulation in addition to platelet inhibition is effective and that the combination of the two is more effective than either treatment alone in non-ST-elevation MI, many patients continue to be discharged from hospital after an ACS event without a prescription for an oral anticoagulation agent 24–26. The reasons for this may be related to the key limitations of the vitamin K antagonists (VKAs) that complicate their use, which include an increased risk of bleeding and logistical challenges in managing these drugs 26. The situation in patients suffering ST-elevation MI is even more challenging, and evidence of the benefit of VKAs in these patients is limited 10.
The development of novel oral anticoagulants (OACs) in recent years may go some way to overcoming the limitations of VKA-based anticoagulant therapy. During the past decade, several novel OACs have been studied in patients with ACS and the first of these, rivaroxaban, received marketing authorization from the European Commission in May 2013 27.
Studies of Oral Anticoagulants for Secondary Prevention After an Acute Coronary Syndrome Event
Vitamin K antagonists
The evaluation of oral anticoagulant therapy alongside antiplatelet therapy after an acute ACS event began in the 1990s with studies of VKAs + ASA, either alone or in combination with clopidogrel. The initial challenge was to establish an optimal regimen, because many of the early studies that evaluated fixed-dose or low-intensity VKA regimens failed to demonstrate a benefit associated with the addition of anticoagulant therapy to ASA, compared with ASA alone 28,29. However, studies utilizing a moderate-intensity VKA regimen (target international normalized ratio 2.0–3.0) did reveal a modest benefit compared with ASA alone 30–34. In 2006, the results of a meta-analysis of data from 14 trials that included >25 000 patients were reported 35. Although the analysis failed to demonstrate a benefit for VKA (of any intensity) + ASA over ASA alone, analysis of the subset of studies that evaluated moderate-intensity VKA therapy did indicate a benefit for the combination regimen (odds ratio [OR] 0.73; 95% CI 0.63–0.84; P < 0.0001). However, this benefit was accompanied by an increased risk of major bleeding events (OR 1.77; 95% CI 1.47–2.13; P < 0.00001).
A further meta-analysis reported in 2007 included data from >69 000 patients who had taken part in 13 studies comparing either moderate-intensity VKA +ASA or clopidogrel + ASA with ASA alone 36. Although both regimens were associated with significant reductions in major adverse events (all-cause death, acute MI, thromboembolic stroke, major bleeding events and overall risk of stroke) compared with ASA alone, there was no apparent benefit for one regimen over the other in terms of the overall rate of major adverse events. When individual events were examined, the addition of a VKA to ASA was associated with a significantly reduced risk of any type of stroke (OR 0.58; 95% CI 0.35–0.94; P = 0.038) and more specifically of thromboembolic stroke (OR 0.53; 95% CI 0.31–0.88; P = 0.03). However, this beneficial effect was accompanied by an increase in the risk of major bleeding events with ASA + VKA compared with ASA + clopidogrel (OR 1.9; 95% CI 1.2–2.8; P = 0.005).
Direct thrombin inhibitors
The oral, direct thrombin inhibitors ximelagatran and dabigatran have also been evaluated in the management of patients post-ACS. Ximelagatran was evaluated in the phase II dose-finding Efficacy and Safety of the oral direct Thrombin inhibitor ximelagatran in patients with recent Myocardial damage (ESTEEM) study 37, in which CV events were significantly reduced but bleeding events were increased compared with ASA alone. This agent was subsequently withdrawn from development owing to drug-related liver toxicity 38.
The 6-month phase II dabigatran RE-DEEM study, which compared twice-daily doses of dabigatran (50, 75, 110, or 150 mg) in combination with ASA and either clopidogrel or ticlopidine with a standard DAPT regimen, failed to reveal a reduction in the rate of MI, stroke or CV death, although, compared with the DAPT regimen, a significant reduction in coagulation activity was noted 39. At the time of writing, phase III evaluation of dabigatran in ACS has not been initiated.
Direct Factor Xa inhibitors
Factor Xa is upstream of prothrombin in the coagulation cascade and Factor Xa inhibition downregulates thrombin generation 20. Oral direct Factor Xa inhibitors have, therefore, been investigated as potential partners for antiplatelet therapy after an acute ACS event.
Data from two placebo-controlled studies have been reported for the oral, direct Factor Xa inhibitor apixaban: the phase II Apixaban for Prevention of Acute Ischaemic Events (APPRAISE)-1 study and the phase III APPRAISE-2 study 40,41. In APPRAISE-1 (which studied 1715 patients with ACS), doses ranging from 2.5 mg twice daily to 20 mg once daily were evaluated. A trend towards a reduction in ischaemic events with the addition of apixaban to DAPT was accompanied by a dose-related increase in bleeding events; treatment with the two higher doses of apixaban was discontinued because of an excess of total bleeding events. Rates of ischaemic events (CV death, MI, severe recurrent ischaemia or ischaemic stroke) compared with placebo were nonsignificantly reduced with apixaban 2.5 mg twice daily (HR 0.73; P = 0.21) and apixaban 10 mg once daily (HR 0.61; P = 0.07). In APPRAISE-2, the subsequent phase III study (which included >7000 patients with ACS), addition of a 5 mg dose of apixaban twice daily to ASA alone or to a DAPT regimen (predominantly ASA + clopidogrel) was terminated early owing to an excess of major bleeding events and failure to achieve a significant reduction in ischaemic events compared with either ASA or DAPT alone. The primary efficacy endpoint (CV death, MI or ischaemic stroke) occurred in 7.5% of patients treated with apixaban vs. 7.9% of those who received placebo + antiplatelet therapy (HR 0.95; P = 0.51; Figure 2). However, it is worth noting that this study recruited a population of patients who were already at high risk of recurrent CV events and included a high proportion of patients with diabetes, prior MI and cerebrovascular disease, as well as patients who had not undergone revascularization for their index event.
Figure 2.
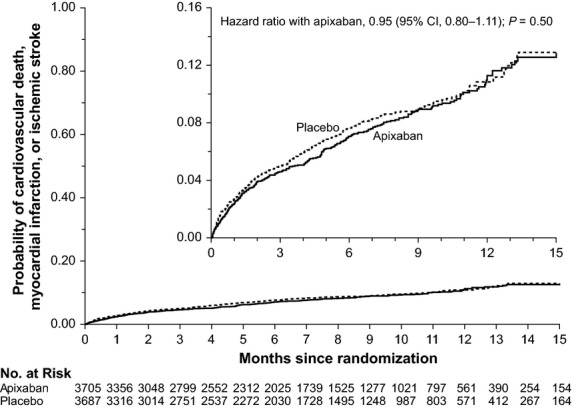
The probability of CV death, MI or ischaemic stroke during 15 months of follow-up among patients treated with apixaban or placebo after an ACS event 41. ACS, acute coronary syndrome; CI, confidence interval; CV, cardiovascular; MI, myocardial infarction.
More positive data have emerged for another oral, direct Factor Xa inhibitor: rivaroxaban. Data from the phase II Anti-Xa Therapy to Lower Cardiovascular Events in Addition to Standard Therapy in Subjects with Acute Coronary Syndrome–Thrombolysis in Myocardial Infarction-46 (ATLAS ACS TIMI 46) study and the phase III ATLAS ACS 2 TIMI 51 trial are available 42,43. The phase II ATLAS ACS TIMI 46 study was a comprehensive dose-finding exercise in which total daily doses of rivaroxaban ranging from 5 to 20 mg, administered as once- or twice-daily regimens, were evaluated in a cohort of 3491 patients with ACS when added either to ASA alone (Stratum 1) or to DAPT (principally ASA + clopidogrel; Stratum 2) 42. Patients were randomized within each stratum to receive either rivaroxaban or placebo. Consistent with the observations from trials of other direct Factor Xa inhibitors, a dose-dependent increase in bleeding events was noted. In general, lower rates of bleeding events were observed when rivaroxaban was administered in twice-daily divided doses rather than as a single, once-daily dose. In terms of efficacy, with the addition of rivaroxaban (all doses pooled), a trend towards a reduction in the time to the first episode of death, MI, stroke or severe recurrent ischaemia requiring revascularization was noted (5.6% vs. 7.0%; HR 0.79; 95% CI 0.60–1.05; P = 0.10). To determine the most appropriate doses for phase III evaluation, an exploratory net clinical benefit analysis was conducted and showed that the two lowest doses (2.5 and 5 mg twice daily) were associated with a reduced risk for the composite endpoint of death, MI, stroke or Thrombolysis in Myocardial Infarction major or minor bleeding events. The analysis also showed that the two lowest doses (2.5 and 5 mg twice daily) in combination with ASA alone or DAPT alone were associated with a trend towards a net clinical benefit compared with placebo in combination with ASA alone (HR 0.59; 95% CI 0.30–1.16) or DAPT alone (HR 0.85; 95% CI 0.47–1.54); these were the doses that were selected for further evaluation in the phase III ATLAS ACS 2 TIMI 51 study 44.
The phase III ATLAS ACS 2 TIMI 51 study randomized 15 526 patients, 15 350 of whom received one of the two rivaroxaban dose regimens or placebo, in addition to standard medical therapy of ASA with (Stratum 2) or without (Stratum 1) a thienopyridine (DAPT was the intended therapy for 93% of the study population) 43. Both doses were associated with a significant reduction in the risk of the composite endpoint of death from CV causes, MI or stroke (Figure 3). For the 2.5 mg dose of rivaroxaban, the reduction in risk of the composite primary endpoint was 16% compared with placebo (HR 0.84; 95% CI 0.72–0.97; P = 0.02), with a 34% reduction in the risk of death from CV causes alone (HR 0.66; 95% CI 0.51–0.86; P = 0.002) and a 32% reduction in the risk of death from all causes (HR 0.68; 0.53–0.87; P = 0.002) (Table I). For the 5 mg twice-daily dose, the reduction in risk of the composite primary endpoint was 15% compared with placebo (HR 0.85; 95% CI 0.73–0.98; P = 0.03), with a more modest and not statistically significant risk reduction of 6% for CV mortality (HR 0.94; 95% CI 0.75–1.20; P = 0.63). The reduction in the risk of the primary endpoint was consistent across all patient subgroups analysed except for those with a history of prior stroke. Furthermore, a statistically significant reduction in the risk of stent thrombosis was observed with rivaroxaban 2.5 mg twice daily compared with placebo in patients with a pre-existing stent or who had a stent placed for their index event (HR 0.61; 95% CI 0.39–0.94; P = 0.023) 45. However, the reduction did not reach statistical significance for the 5 mg twice-daily dose (P = 0.089) 45.
Figure 3.
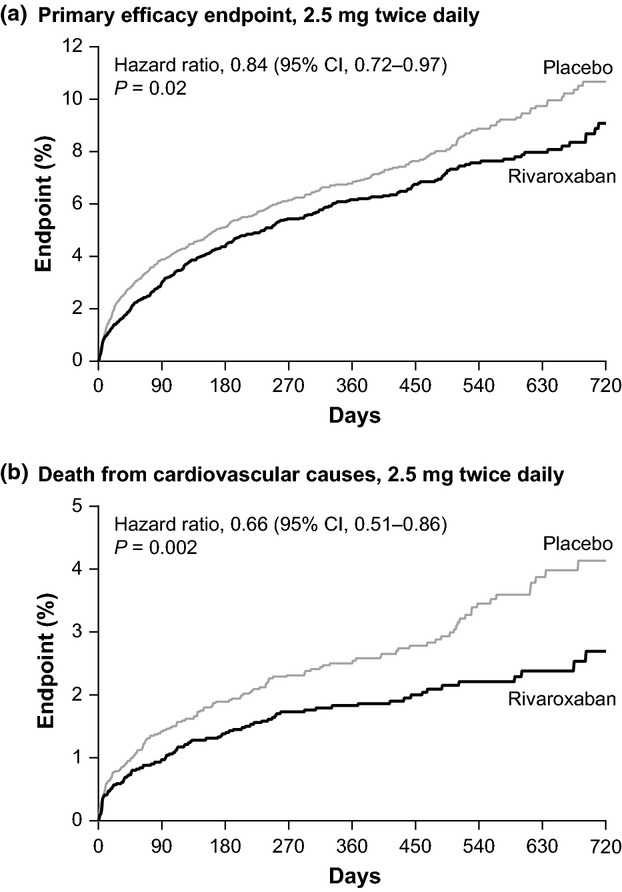
The probability of (a) CV death, MI, stroke, or (b) death from CV causes during follow-up in patients treated with rivaroxaban 2.5 mg bid or placebo after an ACS event 43. ACS, acute coronary syndrome; CI, confidence interval; CV, cardiovascular; MI, myocardial infarction.
Table 1.
| Endpoint, n (%)b | Rivaroxaban 2.5 mg bid | Rivaroxaban 5 mg bid | Placebo | Rivaroxaban 2.5 mg bid vs. Placebo | Rivaroxaban 5 mg bid vs. Placebo | ||
|---|---|---|---|---|---|---|---|
| HR (95% CI)c | P-valued | HR (95% CI)c | P-valued | ||||
| Efficacy outcomese | N = 5114 | N = 5115 | N = 5113 | ||||
| Primary endpointf | 313 (9.1) | 313 (8.8) | 376 (10.7) | 0.84 (0.72–0.97) | P = 0.02 | 0.85 (0.73–0.98) | P = 0.03 |
| Death from CV causes | 94 (2.7) | 132 (4.0) | 143 (4.1) | 0.66 (0.51–0.86) | P = 0.002 | 0.94 (0.75–1.20) | P = 0.63 |
| MI | 205 (6.1) | 179 (4.9) | 229 (6.6) | 0.90 (0.75–1.09) | P = 0.27 | 0.79 (0.65–0.97) | P = 0.02 |
| Stroke | |||||||
| Any | 46 (1.4) | 54 (1.7) | 41 (1.2) | 1.13 (0.74–1.73) | P = 0.56 | 1.34 (0.90–2.02) | P = 0.15 |
| Ischaemic | 30 (1.0) | 35 (0.9) | 34 (1.0) | 0.89 (0.55–1.45) | P = 0.64 | 1.05 (0.65–1.68) | P = 0.84 |
| All-cause death | 103 (2.9) | 142 (4.4) | 153 (4.5) | 0.68 (0.53–0.87) | P = 0.002 | 0.95 (0.76–1.19) | P = 0.66 |
| Stent thrombosis | 47 (2.2) | 51 (2.3) | 72 (2.9) | 0.65 (0.45–0.94) | P = 0.02 | 0.73 (0.51–1.04) | P = 0.08 |
| Safety outcomesf | N = 5115 | N = 5110 | N = 5125 | ||||
| TIMI major bleeding not related to CABG | 65 (1.8) | 82 (2.4) | 19 (0.6) | 3.46 (2.08–5.77) | P < 0.001 | 4.47 (2.71–7.36) | P < 0.001 |
| TIMI minor bleeding | 32 (0.9) | 49 (1.6) | 20 (0.5) | 1.62 (0.92–2.82) | P = 0.09 | 2.52 (1.50–4.24) | P < 0.001 |
| Intracranial haemorrhage | 14 (0.4) | 18 (0.7) | 5 (0.2) | 2.83 (1.02–7.86) | P = 0.04 | 3.74 (1.39–10.07) | P = 0.005 |
| Fatal bleeding | 6 (0.1) | 15 (0.4) | 9 (0.2) | 0.67 (0.24–1.89) | P = 0.45 | 1.72 (0.75–3.92) | P = 0.20 |
bid, twice-daily; CABG, coronary artery bypass graft; CI, confidence interval; CV, cardiovascular; HR, hazard ratio; MI, myocardial infarction; PCI, percutaneous coronary intervention; TIA, transient ischaemic attack.
Event rates are reported as Kaplan–Meier estimates through 24 months and so are not presented as numerical percentages.
n (%): n is the number of subjects with event, % = hazard rate in the corresponding treatment group based on a stratified Cox proportional hazards model.
HR (95% CI): Hazard ratios (95% confidence interval) as compared to placebo arm are based on the stratified (by standard of care with ASA or ASA + thienopyridine) Cox proportional hazards model.
P-values (two-sided) as compared to placebo arm are based on the stratified (by standard of care with ASA or ASA + thienopyridine) log rank test.
n = number of subjects at risk; for efficacy events the mITT (excluding three potentially noncompliant study sites) Analysis Set was used; for safety events the treatment-emergent Safety Analysis Set was used.
Primary efficacy endpoint as adjudicated by the CEC: first occurrence of CV death, MI or stroke.
An iterative landmark analysis showed that mortality outcomes of patients who experienced major bleeding and survived for at least a further 30 days were similar to outcomes for propensity-matched controls 46. Although the overall rate of major bleeding events in ATLAS ACS 2 TIMI 51 was higher with rivaroxaban than with placebo (2.1% vs. 0.6%, respectively; P < 0.001), fatal bleeding events were rare and occurred at a similar rate with both rivaroxaban and placebo (0.3% vs. 0.2%, respectively; P = 0.66) 43. This finding mirrored the noted increase in intracranial haemorrhage events but not in fatal intracranial haemorrhage events associated with rivaroxaban (Table I). The safety analysis favoured the 2.5 mg twice-daily dose with a lower rate of clinically significant bleeding (1.8% compared with 2.4% with 5 mg twice daily) 43.
The 2.5 mg twice-daily dose was subsequently selected for regulatory submission based in part on a more detailed comparison of the balance between efficacy and safety for the 5 and 2.5 mg doses 47. Although both doses reduced the rate of CV events in patients with ACS receiving antiplatelet therapy, the 2.5 mg dose was associated with lower incidence of mortality and fewer bleeding complications. In a net clinical benefit analysis (to evaluate fatal or irreversible events prevented or caused) for the rivaroxaban 2.5 mg dose, presented at the American Heart Association Scientific Sessions in 2012, it was found that 87 patients would need to be treated for 1 year to prevent one fatal or irreversible ischaemic event, compared with 984 patients to cause one fatal or irreversible harmful event 48.
Acute coronary syndrome is an umbrella term that covers both MI (with or without ST-elevation) and UA. To make a differential diagnosis between MI and UA, the cardiac biomarker level must be determined, with elevated levels supporting a diagnosis of MI. Cardiac troponin is a biomarker currently recommended in clinical guidelines to distinguish between MI and UA 1, although others, such as CK-MB, are also used. A retrospective analysis of data from the ATLAS ACS 2 TIMI 51 trial in patients with elevated cardiac biomarkers (and without prior stroke or transient ischaemic attack) revealed a greater efficacy benefit for rivaroxaban 2.5 mg twice daily in this subgroup compared with the overall study population 27. For the composite primary endpoint of CV death, MI or stroke, the absolute risk reduction was 1.3% for rivaroxaban versus placebo in the overall population (HR 0.84; P = 0.02) compared with 1.7% in the subgroup of patients with elevated biomarkers (HR 0.80; P = 0.007) (Table 2). A similar pattern – for a numerically increased risk – was observed for CV death (P < 0.001).
Table 2.
ATLAS ACS 2 TIMI 51 trial – incidence rates of efficacy and safety outcomes in all patients and in those with elevated cardiac biomarkers and without prior stroke/transient ischaemic attack 27.
| Endpoint | Populationa | Incidence rate, % | ARRe, % | HR (95% CI)f | P-valueg | |
|---|---|---|---|---|---|---|
| Rivaroxaban 2.5 mg bidg | Placebog | |||||
| CV death, MI or stroke | Overall | 6.1 | 7.4 | 1.3 | 0.84 (0.72–0.97) | P = 0.020* |
| Elevated biomarkers (without prior stroke/TIA) | 6.2 | 7.9 | 1.7 | 0.80 (0.68–0.94) | P = 0.007** | |
| CV death | Overall | 1.8 | 2.8 | 1.0 | 0.66 (0.51–0.86) | P = 0.002** |
| Elevated biomarkers (without prior stroke/TIA) | 1.7 | 3.1 | 1.4 | 0.55 (0.41–0.74) | P < 0.001** | |
| Stroke (ischaemic or haemorrhagic) | Overall | 0.9 | 0.8 | 0.1 | 1.13 (0.74–1.73) | P = 0.562 |
| Elevated biomarkers (without prior stroke/TIA) | 0.9 | 0.7 | 0.2 | 1.23 (0.75–2.02) | P = 0.403 | |
| MI | Overall | 4.0 | 4.5 | 0.5 | 0.90 (0.75–1.09) | P = 0.270 |
| Elevated biomarkers (without prior stroke/TIA) | 4.3 | 4.9 | 0.6 | 0.88 (0.72–1.08) | P = 0.215 | |
| TIMI major bleeding not related to CABGc | Overall | 1.3 | 0.4 | 0.9 | 3.46 (2.08–5.77) | P < 0.001 |
| Elevated biomarkers (without prior stroke/TIA) | 1.3 | 0.4 | 0.9 | 3.44 (1.97–6.01) | P < 0.001 | |
| Stent thrombosis (in patients who underwent PCI)d | Overall | 1.3 | 2.0 | 0.7 | 0.64 (0.43–0.95) | P = 0.026 |
| Elevated biomarkers (without prior stroke/TIA) | 1.4 | 2.0 | 0.6 | 0.64 (0.42–0.96) | P = 0.028 | |
bid, twice-daily; CABG, coronary artery bypass graft; CI, confidence interval; CV, cardiovascular; HR, hazard ratio; MI, myocardial infarction; PCI, percutaneous coronary intervention; TIA, transient ischaemic attack.
Statistically superior.
Nominally significant.
For efficacy events, the mITT (excluding three potentially noncompliant study sites) Analysis Set was used; for safety events, the treatment-emergent Safety Analysis Set was used. For stent thrombosis, the component of the mITT population who had undergone PCI (either history of stent or for the index event) was used.
mITT populations: Rivaroxaban 2.5 mg bid: N = 5114 overall, n = 4104 elevated biomarkers; Placebo: N = 5113 overall, n = 4160 elevated biomarkers.
Safety Analysis Set populations: Rivaroxaban 2.5 mg bid: N = 5115 overall, n = 4096 elevated biomarkers; Placebo: N = 5125 overall, n = 4157 elevated biomarkers.
mITT population for PCI patients: Rivaroxaban 2.5 mg bid: N = 3114 overall, n = 2757 elevated biomarkers; Placebo: N = 3096 overall, n = 2759 elevated biomarkers.
ARR = Absolute risk reduction (percentage points) vs. placebo (difference of incidence rates between placebo and rivaroxaban).
HR (95% CI): Hazard ratios (95% confidence interval) as compared to placebo arm are based on the stratified (by standard of care with ASA or ASA + thienopyridine) Cox proportional hazards model.
P-values (two-sided) as compared to placebo arm are based on the stratified (by standard of care with ASA or ASA + thienopyridine) log rank test.
Based on the results of these two studies, in May 2013, the European Commission approved the use of rivaroxaban 2.5 mg twice daily in patients with elevated biomarkers after ACS; specifically rivaroxaban 2.5 mg, co-administered with ASA alone or with ASA plus clopidogrel or ticlopidine, is indicated for the prevention of atherothrombotic events in adult patients after an ACS with elevated cardiac biomarkers 27.
Lessons from the Past
The past two decades have witnessed marked improvements in the care available for patients after an ACS event. The recognition that these patients face a significant and ongoing risk of recurrent and potentially life-threatening CV events has driven the search for suitable long-term treatments to reduce this risk. Antiplatelet therapy is the cornerstone of this long-term risk reduction strategy and, in recent years, oral anticoagulation therapy has shown a potential for additional efficacy benefits, particularly in patients with non-ST-elevation MI 1.
The safety and logistic limitations of ‘triple therapy’ regimens including VKAs continue to restrict their clinical utility as a long-term solution for patients after an ACS event 1,10, and a number of novel OACs have been evaluated as potential alternative candidates to overcome the limitations of warfarin. The greatest challenge has been and continues to be achieving an acceptable balance between the risk of bleeding (which is a challenge with all antithrombotic agents) and efficacy in terms of clinically relevant reductions in the risk of further CV events. In this regard, dose selection may be an important consideration for the novel OACs. In the phase III APPRAISE-2 study for apixaban, the dose selected for evaluation (5 mg twice daily) was the same as that trialled for stroke prevention in patients with atrial fibrillation 41. By contrast, in the phase III ATLAS ACS 2 TIMI 51 study for rivaroxaban, the total daily doses administered were equivalent to one-quarter to one-half of the dose regimen trialled and approved for stroke prevention in atrial fibrillation (20 mg once daily) 43. However, other differences between the trials, such as the populations enrolled, may also have contributed to the different results obtained.
Looking to the Future
The past decade has seen a significant amount of activity in evaluating oral anticoagulation strategies for secondary prevention after ACS. One outcome of this activity is the approval of the OAC rivaroxaban for use in the prevention of atherothrombotic events after an ACS in adult patients with elevated cardiac biomarkers 49. But what can we expect to achieve in the future?
The achievement of an acceptable benefit–risk profile with rivaroxaban in this setting, and the subsequent approval of the therapy, gives us the opportunity to evaluate this approach on a larger scale. Data from postmarketing surveillance studies and registries, and growing clinical experience will be extremely valuable for assessing the utility of the dual-pathway approach using rivaroxaban in ACS and providing further refinement about how, in whom and when anticoagulant therapy should be implemented after an ACS event. As reported, the benefit of OAC compared with placebo was greater in the subgroup of patients with elevated cardiac biomarkers and without prior stroke or transient ischaemic attack than in the overall population included in the phase III study of rivaroxaban, forming the basis for this agent's approved indication 27. The introduction of the newer antiplatelet agents ticagrelor and prasugrel will necessitate further studies to determine the benefit–risk profile of dual-pathway strategies involving these newer agents.
These remaining questions notwithstanding, this is an exciting time in secondary prevention of ischaemic events after ACS. It is not only encouraging to look back to where we were a decade ago and to review the reduction in recurrence rates we have since achieved but also exciting to look forward to what further progress we may achieve for patients with ACS in the coming years.
Summary
An ACS event is a medical emergency that requires rapid, potentially life-saving medical intervention. After an ACS event, patients face an increased and ongoing risk of further CV events and now routinely receive antiplatelet therapy to reduce this risk. Evidence suggests a period of elevated thrombin generation of at least 6 months after an ACS event, a phenomenon that is thought to contribute to this residual risk in patients receiving therapies targeted predominantly at platelets. Given that the addition of anticoagulant therapy to antiplatelet therapy has been shown to provide an additional risk reduction, research efforts are now focused on evaluating the efficacy of novel OACs in this setting. Although trials with the direct thrombin inhibitor dabigatran and the direct Factor Xa inhibitor apixaban were disappointing, more positive data have recently emerged for another oral, direct Factor Xa inhibitor, rivaroxaban. Despite the failure of the apixaban phase III trial to demonstrate a benefit in terms of ischaemic risk reduction, the efficacy trends in several of the trials described in this review provide evidence that inhibition of coagulation may yield benefits in ACS. The achievement of an acceptable benefit–risk profile with rivaroxaban in this setting provides vindication of the dual-pathway approach in ACS.
Acknowledgments
The authors would like to thank Peter Hopkins and Tracey Lonergan who provided editorial support with funding from Bayer HealthCare Pharmaceuticals and Janssen Scientific Affairs LLC.
Glossary
- ACS
acute coronary syndrome
- ARR
absolute risk reduction
- ASA
acetylsalicylic acid (aspirin)
- bid
twice daily
- CABG
coronary artery bypass graft
- CEC
clinical events committee
- CI
confidence interval
- CV
cardiovascular
- DAPT
dual antiplatelet therapy
- HR
hazard ratio
- MI
myocardial infarction
- mITT
modified intent-to-treat
- OAC
oral anticoagulant
- OR
odds ratio
- PCI
percutaneous coronary intervention
- TIA
transient ischaemic attack
- TIMI
Thrombosis in Myocardial Infarction
- UA
unstable angina
- VKA
vitamin K antagonist
Conflicts of Interest
DA reports speakers and advisory honoraria from Nycomed-Takeda, Sanofi-Aventis, AstraZeneca, Bayer HealthCare, BMS/Pfizer and Boehringer Ingelheim. CB reports research grants from Merck and honoraria from AstraZeneca, Bayer, Boehringer Ingelheim, Daiichi-Sankyo and Sanofi-Aventis. AS is an employee of Bayer HealthCare. FWAV reports educational and research grants from Bayer HealthCare, Eli Lilly and Boehringer Ingelheim, as well as honoraria for consultancies/presentations from Daiichi-Sankyo, Eli Lilly and Bayer HealthCare.
References
- 1.Hamm CW, Bassand JP, Agewall S, et al. ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: the task force for the management of acute coronary syndromes (ACS) in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC) Eur. Heart J. 2011;32:2999–3054. doi: 10.1093/eurheartj/ehr236. [DOI] [PubMed] [Google Scholar]
- 2.Bhatt DL, Eagle KA, Ohman EM, et al. Comparative determinants of 4-year cardiovascular event rates in stable outpatients at risk of or with atherothrombosis. JAMA. 2010;304:1350–1357. doi: 10.1001/jama.2010.1322. [DOI] [PubMed] [Google Scholar]
- 3.Menzin J, Wygant G, Hauch O, Jackel J, Friedman M. One-year costs of ischemic heart disease among patients with acute coronary syndromes: findings from a multi-employer claims database. Curr. Med. Res. Opin. 2008;24:461–468. doi: 10.1185/030079908x261096. [DOI] [PubMed] [Google Scholar]
- 4.Jneid H, Anderson JL, Wright RS, et al. 2012 ACCF/AHA focused update of the guideline for the management of patients with unstable angina/non-ST-elevation myocardial infarction (updating the 2007 guideline and replacing the 2011 focused update): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J. Am. Coll. Cardiol. 2012;60:645–681. doi: 10.1016/j.jacc.2012.06.004. [DOI] [PubMed] [Google Scholar]
- 5.Bertrand ME, Simoons ML, Fox KA, et al. Management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur. Heart J. 2002;23:1809–1840. doi: 10.1053/euhj.2002.3385. [DOI] [PubMed] [Google Scholar]
- 6.Braunwald E, Antman EM, Beasley JW, et al. ACC/AHA 2002 guideline update for the management of patients with unstable angina and non-ST-segment elevation myocardial infarction–summary article: a report of the American College of Cardiology/American Heart Association task force on practice guidelines (committee on the management of patients with unstable angina) J. Am. Coll. Cardiol. 2002;40:1366–1374. doi: 10.1016/s0735-1097(02)02336-7. [DOI] [PubMed] [Google Scholar]
- 7.Van de Werf F, Ardissino D, Betriu A, et al. Management of acute myocardial infarction in patients presenting with ST-segment elevation. The task force on the management of acute myocardial infarction of the European Society of Cardiology. Eur. Heart J. 2003;24:28–66. doi: 10.1016/s0195-668x(02)00618-8. [DOI] [PubMed] [Google Scholar]
- 8.Goldberg RJ, Glatfelter K, Burbank-Schmidt E, Lessard D, Gore JM. Trends in community mortality due to coronary heart disease. Am. Heart J. 2006;151:501–507. doi: 10.1016/j.ahj.2005.04.024. [DOI] [PubMed] [Google Scholar]
- 9.Hutchinson-Jaffe AB, Goodman SG, Yan RT, et al. Comparison of baseline characteristics, management and outcome of patients with non-ST-segment elevation acute coronary syndrome in versus not in clinical trials. Am. J. Cardiol. 2010;106:1389–1396. doi: 10.1016/j.amjcard.2010.06.070. [DOI] [PubMed] [Google Scholar]
- 10.Steg PG, James SK, Atar D, et al. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force on the management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology (ESC) Eur. Heart J. 2012;33:2569–2619. doi: 10.1093/eurheartj/ehs215. [DOI] [PubMed] [Google Scholar]
- 11.Fox KA, Steg PG, Eagle KA, et al. Decline in rates of death and heart failure in acute coronary syndromes, 1999-2006. JAMA. 2007;297:1892–1900. doi: 10.1001/jama.297.17.1892. [DOI] [PubMed] [Google Scholar]
- 12.Peterson ED, Shah BR, Parsons L, et al. Trends in quality of care for patients with acute myocardial infarction in the national registry of myocardial infarction from 1990 to 2006. Am. Heart J. 2008;156:1045–1055. doi: 10.1016/j.ahj.2008.07.028. [DOI] [PubMed] [Google Scholar]
- 13.Yan AT, Yan RT, Tan M, et al. Optimal medical therapy at discharge in patients with acute coronary syndromes: temporal changes, characteristics, and 1-year outcome. Am. Heart J. 2007;154:1108–1115. doi: 10.1016/j.ahj.2007.07.040. [DOI] [PubMed] [Google Scholar]
- 14.Nauta ST, Deckers JW, Akkerhuis M, Lenzen M, Simoons ML, van Domburg RT. Changes in clinical profile, treatment, and mortality in patients hospitalised for acute myocardial infarction between 1985 and 2008. PLoS One. 2011;6:e26917. doi: 10.1371/journal.pone.0026917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schmidt M, Jacobsen JB, Lash TL, Botker HE, Sorensen HT. 25 year trends in first time hospitalisation for acute myocardial infarction, subsequent short and long term mortality, and the prognostic impact of sex and comorbidity: a Danish nationwide cohort study. BMJ. 2012;344:e356. doi: 10.1136/bmj.e356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Steg PG, Bhatt DL, Wilson PW, et al. One-year cardiovascular event rates in outpatients with atherothrombosis. JAMA. 2007;297:1197–1206. doi: 10.1001/jama.297.11.1197. [DOI] [PubMed] [Google Scholar]
- 17.Falk E, Nakano M, Bentzon JF, Finn AV, Virmani R. Update on acute coronary syndromes: the pathologists' view. Eur. Heart J. 2013;34:719–728. doi: 10.1093/eurheartj/ehs411. [DOI] [PubMed] [Google Scholar]
- 18.Fuster V, Badimon L, Badimon JJ, Chesebro JH. The pathogenesis of coronary artery disease and the acute coronary syndromes (1) N. Engl. J. Med. 1992;326:242–250. doi: 10.1056/NEJM199201233260406. [DOI] [PubMed] [Google Scholar]
- 19.Abbate R, Cioni G, Ricci I, Miranda M, Gori AM. Thrombosis and acute coronary syndrome. Throm. Res. 2012;129:235–240. doi: 10.1016/j.thromres.2011.12.026. [DOI] [PubMed] [Google Scholar]
- 20.Mackman N. Triggers, targets and treatments for thrombosis. Nature. 2008;451:914–918. doi: 10.1038/nature06797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wallentin L, Becker RC, Budaj A, et al. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N. Engl. J. Med. 2009;361:1045–1057. doi: 10.1056/NEJMoa0904327. [DOI] [PubMed] [Google Scholar]
- 22.Wiviott SD, Braunwald E, McCabe CH, et al. Prasugrel versus clopidogrel in patients with acute coronary syndromes. N. Engl. J. Med. 2007;357:2001–2015. doi: 10.1056/NEJMoa0706482. [DOI] [PubMed] [Google Scholar]
- 23.Yusuf S, Zhao F, Mehta SR, Chrolavicius S, Tognoni G, Fox KK. Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation. N. Engl. J. Med. 2001;345:494–502. doi: 10.1056/NEJMoa010746. [DOI] [PubMed] [Google Scholar]
- 24.Amad H, Yan AT, Yan RT, et al. The association between prior use of aspirin and/or warfarin and the in-hospital management and outcomes in patients presenting with acute coronary syndromes: insights from the global registry of acute coronary events (GRACE) Can. J. Cardiol. 2012;28:48–53. doi: 10.1016/j.cjca.2011.09.003. [DOI] [PubMed] [Google Scholar]
- 25.Depta JP, Cannon CP, Fonarow GC, Zhao X, Peacock WF, Bhatt DL. Patient characteristics associated with the choice of triple antithrombotic therapy in acute coronary syndromes. Am. J. Cardiol. 2009;104:1171–1178. doi: 10.1016/j.amjcard.2009.06.027. [DOI] [PubMed] [Google Scholar]
- 26.Pelc-Nowicka A, Bryniarski L, Mirek-Bryniarska E, Zabojszcz M. Dual antiplatelet therapy and antithrombotic treatment in patients with acute coronary syndrome - does everyday medical practice reflects current recommendations? A pilot study. Kardiol. Pol. 2009;67:1335–1341. [PubMed] [Google Scholar]
- 27.European Medicines Agency. Assessment report: Xarelto (Procedure No. EMEA/H/C/000944/X/00017) 2013. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Assessment_Report_-_Variation/human/000944/WC500144718.pdf (accessed 10 July 2013)
- 28.Coumadin Aspirin Reinfarction Study (CARS) Investigators. Randomised double-blind trial of fixed low-dose warfarin with aspirin after myocardial infarction. Coumadin aspirin reinfarction study (CARS) investigators. Lancet. 1997;350:389–396. [PubMed] [Google Scholar]
- 29.Fiore LD, Ezekowitz MD, Brophy MT, Lu D, Sacco J Combination Hemotherapy and Mortality Prevention (CHAMP) Study Group. Department of Veterans Affairs Cooperative Studies Program Clinical Trial comparing combined warfarin and aspirin with aspirin alone in survivors of acute myocardial infarction: primary results of the CHAMP study. Circulation. 2002;105:557–563. doi: 10.1161/hc0502.103329. [DOI] [PubMed] [Google Scholar]
- 30.Brouwer MA, van den Bergh PJ, Aengevaeren WR, et al. Aspirin plus coumarin versus aspirin alone in the prevention of reocclusion after fibrinolysis for acute myocardial infarction: results of the antithrombotics in the prevention of reocclusion in coronary thrombolysis (APRICOT)-2 trial. Circulation. 2002;106:659–665. doi: 10.1161/01.cir.0000024408.81821.32. [DOI] [PubMed] [Google Scholar]
- 31.Cohen M, Adams PC, Parry G, et al. Combination antithrombotic therapy in unstable rest angina and non-Q-wave infarction in nonprior aspirin users. Primary end points analysis from the ATACS trial. Antithrombotic therapy in acute coronary syndromes research group. Circulation. 1994;89:81–88. doi: 10.1161/01.cir.89.1.81. [DOI] [PubMed] [Google Scholar]
- 32.Hurlen M, Abdelnoor M, Smith P, Erikssen J, Arnesen H. Warfarin, aspirin, or both after myocardial infarction. N. Engl. J. Med. 2002;347:969–974. doi: 10.1056/NEJMoa020496. [DOI] [PubMed] [Google Scholar]
- 33.OASIS Investigators. Effects of long-term, moderate-intensity oral anticoagulation in addition to aspirin in unstable angina. The organization to assess strategies for ischemic syndromes (OASIS) investigators. J. Am. Coll. Cardiol. 2001;37:475–484. doi: 10.1016/s0735-1097(00)01118-9. [DOI] [PubMed] [Google Scholar]
- 34.van Es RF, Jonker JJ, Verheugt FW, Deckers JW, Grobbee DE. Antithrombotics in the secondary prevention of events in coronary thrombosis-2 (ASPECT-2) research group. Aspirin and coumadin after acute coronary syndromes (the ASPECT-2 study): a randomised controlled trial. Lancet. 2002;360:109–113. doi: 10.1016/S0140-6736(02)09409-6. [DOI] [PubMed] [Google Scholar]
- 35.Andreotti F, Testa L, Biondi-Zoccai GG, Crea F. Aspirin plus warfarin compared to aspirin alone after acute coronary syndromes: an updated and comprehensive meta-analysis of 25,307 patients. Eur. Heart J. 2006;27:519–526. doi: 10.1093/eurheartj/ehi485. [DOI] [PubMed] [Google Scholar]
- 36.Testa L, Zoccai GB, Porto I, et al. Adjusted indirect meta-analysis of aspirin plus warfarin at international normalized ratios 2 to 3 versus aspirin plus clopidogrel after acute coronary syndromes. Am. J. Cardiol. 2007;99:1637–1642. doi: 10.1016/j.amjcard.2007.01.052. [DOI] [PubMed] [Google Scholar]
- 37.Wallentin L, Wilcox RG, Weaver WD, et al. Oral ximelagatran for secondary prophylaxis after myocardial infarction: the ESTEEM randomised controlled trial. Lancet. 2003;362:789–797. doi: 10.1016/S0140-6736(03)14287-0. [DOI] [PubMed] [Google Scholar]
- 38.European Medicines Agency. Press release: AstraZeneca withdraws its application for ximelagatran 36-mg film-coated tablets. 2006. http://www.ema.europa.eu/docs/en_GB/document_library/Press_release/2010/02/WC500074073.pdf (accessed 5 March 2013)
- 39.Oldgren J, Budaj A, Granger CB, et al. Dabigatran vs. placebo in patients with acute coronary syndromes on dual antiplatelet therapy: a randomized, double-blind, phase II trial. Eur. Heart J. 2011;32:2781–2789. doi: 10.1093/eurheartj/ehr113. [DOI] [PubMed] [Google Scholar]
- 40.APPRAISE Steering Committee and Investigators. Alexander JH, Becker RC, et al. Apixaban, an oral, direct, selective factor Xa inhibitor, in combination with antiplatelet therapy after acute coronary syndrome: results of the Apixaban for prevention of acute ischemic and safety events (APPRAISE) trial. Circulation. 2009;119:2877–2885. doi: 10.1161/CIRCULATIONAHA.108.832139. [DOI] [PubMed] [Google Scholar]
- 41.Alexander JH, Lopes RD, James S, et al. Apixaban with antiplatelet therapy after acute coronary syndrome. N. Engl. J. Med. 2011;365:699–708. doi: 10.1056/NEJMoa1105819. [DOI] [PubMed] [Google Scholar]
- 42.Mega JL, Braunwald E, Mohanavelu S, et al. Rivaroxaban versus placebo in patients with acute coronary syndromes (ATLAS ACS-TIMI 46): a randomised, double-blind, phase II trial. Lancet. 2009;374:29–38. doi: 10.1016/S0140-6736(09)60738-8. [DOI] [PubMed] [Google Scholar]
- 43.Mega JL, Braunwald E, Wiviott SD, et al. Rivaroxaban in patients with a recent acute coronary syndrome. N. Engl. J. Med. 2012;366:9–19. doi: 10.1056/NEJMoa1112277. [DOI] [PubMed] [Google Scholar]
- 44.Gibson CM, Mega JL, Burton P, et al. Rationale and design of the Anti-Xa Therapy to Lower cardiovascular events in Addition to standard therapy in Subjects with Acute Coronary Syndrome-Thrombolysis in Myocardial Infarction 51 (ATLAS-ACS 2 TIMI 51) trial: a randomized, double-blind, placebo-controlled study to evaluate the efficacy and safety of rivaroxaban in subjects with acute coronary syndrome. Am. Heart J. 2011;161:815–821. doi: 10.1016/j.ahj.2011.01.026. [DOI] [PubMed] [Google Scholar]
- 45.Gibson CM, Chakrabarti AK, Mega JL, et al. Reduction of stent thrombosis in patients with acute coronary syndrome treated with rivaroxaban in ATLAS ACS 2-TIMI 51. J. Am. Coll. Cardiol. 2013;62:286–290. doi: 10.1016/j.jacc.2013.03.041. [DOI] [PubMed] [Google Scholar]
- 46.Pride Y, Mohanavelu S, Mega J, Braunwald E, Gibson CM. Temporal relationship between major hemorrhagic events and mortality among patients with recent acute coronary syndrome: insights from ATLAS ACS 2-TIMI 51. Circulation. 2012;126:A9944. [Google Scholar]
- 47.Mega JL, Braunwald E, Wiviott SD, et al. Comparison of the efficacy and safety of two rivaroxaban doses in acute coronary syndrome (from ATLAS ACS 2-TIMI 51) Am. J. Cardiol. 2013;112:472–478. doi: 10.1016/j.amjcard.2013.04.011. [DOI] [PubMed] [Google Scholar]
- 48.Gibson CM, Levitan B, Murphy SA, et al. A net clinical outcome analysis comparing fatal or irreversible ischemic and bleeding events in ATLAS ACS 2 - TIMI 51. Circulation. 2012;126:A13152. [Google Scholar]
- 49.Bayer Pharma AG. Xarelto® (rivaroxaban) Summary of Product Characteristics. 2013. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/000944/WC500057108.pdf (accessed 13 August 2013)


