Abstract
Objective
To report an in-depth analysis of policy change for integrated community case management of childhood illness (iCCM) in six sub-Saharan African countries. We analysed how iCCM policies developed and the barriers and facilitators to policy change.
Methods
Qualitative retrospective case studies drawing from document reviews, semi-structured interviews and in-country validation workshops were conducted in Burkina Faso, Kenya, Malawi, Mali, Mozambique and Niger. These countries were selected to maximise variation in iCCM policy status, community health worker (CHW) models and different African regions.
Results
Country iCCM policies evolved in an ad hoc fashion, but were substantially influenced by the history of primary health care and the nature of CHW programmes. Technical officers within Ministries of Health led iCCM policy change with support from international donors, but neither communities nor political leadership was mobilised. Concerns about achieving the Millennium Development Goals, together with recognition of the shortcomings of existing child health programmes, led to the adoption of iCCM policies. Availability of external financing played a critical role in facilitating policy change.
Conclusions
iCCM policy change has been promoted by international agencies, but national governments have struggled to align iCCM with country health systems. Greater investment is needed in tailoring global policy initiatives to match country needs. High-level, political ownership of iCCM policies could facilitate policy change, as could clearer strategies for ensuring the long-term sustainability of such policies.
Keywords: child health services, community health services, health policy
Introduction
In 2004, WHO and UNICEF issued joint statements supporting the clinical management of diarrhoea and pneumonia at community levels (WHO / UNICEF 2004a; WHO/UNICEF 2004b), while WHO issued programme guidelines for the home management of malaria (WHO 2004). Subsequently, international actors supported joint statements on community management of severe acute malnutrition and home visits for newborns (WHO 2007; WHO/UNICEF 2009), as well as programme guidelines for community case management (CORE Group 2010). In 2012, elements of these community-based services were brought together in a package known as integrated community case management (iCCM) (UNICEF 2012). iCCM is typically delivered by community health workers at the community level and encompasses treatment for (i) childhood pneumonia with antibiotics, (ii) diarrhoea with zinc and oral rehydration salts (ORS) and (iii) malaria with artemisinin combination therapy (ACT). The joint statement on iCCM also supports the identification (but not treatment) of severe acute malnutrition and home visits (but not treatment) for newborns (UNICEF 2012).
While the scientific evidence supporting the different components of iCCM is relatively clear and there is an established global consensus regarding the need for integrated community services for childhood illness, country-level formulation of iCCM policy has not advanced equally. Some countries have rapidly reformed policy and implemented iCCM programmes, while others have taken much longer (Marsh et al. 2008; George et al. 2012; de Sousa et al. 2012). Existing studies have documented the status of iCCM policy change in priority ‘Countdown to 2015’ countries and noted remaining gaps, but have not explored in detail how and why policy change has occurred or the impediments faced. This paper reports an in-depth analysis of national policy change for iCCM in six sub-Saharan African countries. We analysed whether, how and why iCCM policies were made or reformed, and how actors, institutional processes, ideas, context and policy content affected this process. In doing so, we sought to explain some of the underlying iCCM policy processes across the region and inform discussions about how best to support iCCM policy.
iCCM policy change also provides a lens through which to examine health policies in low- and middle-income countries. iCCM typically seeks to provide services to remote rural areas and involves strengthening primary health care. Further, it encapsulates many frequently contested issues in international health today, such as the scalability and sustainability of CHW programmes, and professional resistance to task shifting (Haines et al. 2007; Lehmann et al. 2009; Fulton et al. 2011; Singh & Sachs 2013). Our study of iCCM policy was intended to cast light on these broader policy questions.
Study methods
We pursued the research aims through qualitative retrospective case studies in Burkina Faso, Kenya, Malawi, Mali, Mozambique and Niger. These countries were purposively selected to reflect maximum variation (Yin 2009) and differed according to iCCM policy status, the subregion within Africa to which they belonged, and CHW models (Table1).
Table 1.
Contexts and chw programmes in case study countries
| Burkina Faso | Mali | Niger | Kenya | Malawi | Mozambique | |
|---|---|---|---|---|---|---|
| Language/Region | Francophone/West Africa | Francophone/West Africa | Francophone/West Africa | Anglophone/East Africa | Anglophone/Southern Africa | Lusophone/Southern Africa |
| iCCM policy status & coverage | Policy in place. Implementation in pilot phase | Policy in place, being implemented by donors in 5/8 regions | Policy in place. Fully implemented at scale | No iCCM policy or implementation, only pilot projects | Policy in place. Fully implemented at scale | Policy in place. Implementation in scale-up phase. |
| Nature of CHW cadre | In process of re-engaging volunteer cadre | In process of establishing new CHW cadre | Existing, paid, CHW cadre | Policy on CHWs exists, but not fully implemented. | Existing, paid, CHW cadre | In process of upgrading CHW cadre |
| CHW Payment | Volunteer, but keeps 25% of some drug revenues | US$67–89 monthly for full time, to be paid by community health associations | US$100 monthly salary for full time paid by government | US$24 monthly (if available) part time. In principle agreement, but unbudgeted | US$100 monthly for full time, paid by government | Government standard of US$43 monthly part time agreed to by implementing NGOs, but not budgeted for by government |
| CHW training | Unclear | Health aide diploma | 6 months | 2–6 weeks | 3 months basic, more added due to specific programmes | 14 weeks |
| CCM training | 1 week | 15 days | 1 week | 1 week | 1 week | 4 weeks |
Data were collected between May 2011 and March 2012 in Burkina Faso and between January and September 2012 in all other countries (Table2). We performed a document review in each country to create a detailed timeline, as well as an initial picture of iCCM-related policy development and an initial list of respondents involved in the policy process. Subsequently, semi-structured interviews were conducted with respondents from government, multilateral organisations, donors, NGOs and civil society organisations, with additional interviewees selected through snowball sampling. A common interview guide was refined during a workshop with research teams and used to guide all interviews. Interviews were conducted usually in the national language of each country and transcribed in-country, with interviewers also taking written notes.
Table 2.
Overview of data sources
| Burkina Faso | Mali | Niger | Kenya | Malawi | Mozambique | |
|---|---|---|---|---|---|---|
| Number of documents reviewed | 80+ | 45 | 113 | 41 | 54 | 50 |
| Interviews completed by category | ||||||
| Government officials, incl. MoH and other government ministries | 14 | 15 | 18 | 10 | 5 | 8 |
| Multilateral agencies, for example UNICEF, WHO | 5 | 5 | 8 | 3 | 4 | 5 |
| Donors and bilateral agencies, for example USAID, CIDA | 0 | 3 | 3 | 1 | 2 | 1 |
| NGOs, incl. national and international | N/A | 9 | 2 | 3 | 5 | 5 |
| Other actors, incl. civil society, researchers, professional associations, etc. | 1 | 1 | 1 | 2 | 4 | 2 |
| Total respondents interviewed/approached | 20/30 | 33/35 | 32/37 | 19/31 | 20/30 | 21/40 |
The research team employed a standard case definition of iCCM across the study countries that matched the definition in the joint statement (UNICEF 2012) and encompassed treatment for childhood pneumonia (with antibiotics), treatment for diarrhoea (with zinc and ORS) and treatment for malaria (with ACT and other antimalarials), generally by community or lay health workers (CHWs) at household and/or community levels. However, as described in the results, each country had its own slightly different definition of iCCM, and in practice, the researchers had to employ the country's own definition in interviews, while tracking this against the standard case definition.
The Johns Hopkins Internal Review Board exempted the study as it was not considered to be human subjects research. Ethics review committees reviewed and approved the study in all study countries.
The analytical process was guided by a conceptual framework known as the policy triangle (Walt & Gilson 1994) (Figure1), which posits that policy change is shaped by policy content, context, actors, and policy processes and the interaction between these. In addition, we sought to build on existing frameworks and studies that investigate how evidence is used in policy development in low- and middle-income countries (Elliott & Popay 2000; Woelk et al. 2009). The core research team at Johns Hopkins University developed analytical codes within the following broad categories: policy content, evolution, context, actors, process, evidence, implementation, financing, CHWs, newborn, barriers and facilitators. These codes were discussed and finalised with country teams who then coded the data and undertook primary thematic analysis with additional support and cross-country analyses from the core team at Johns Hopkins University. We triangulated across respondents and between interview and documentary data throughout the analytical process. Outliers and negative cases were pursued to provide further nuance within case study findings. We held validation workshops at country and global levels to share draft reports with stakeholders and solicit feedback on emerging findings.
Figure 1.
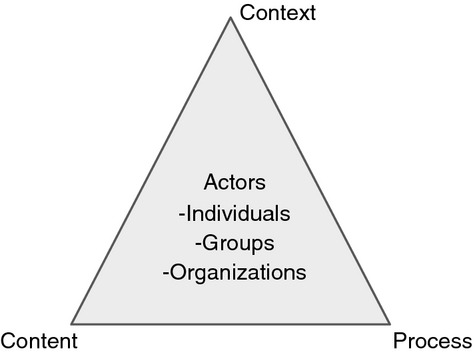
Policy analysis triangle.
Results
iCCM policy content and expression
There are potentially multiple policy documents at national levels that might refer to iCCM, ranging from programme implementation or training guidelines to high-level policies such as health sector strategic plans. iCCM and the role of CHWs in treatment were more likely to be consistently mentioned in programme implementation or training guidelines compared with higher-level policies (Table3).
Table 3.
Expressions of iCCM policy across country case studies
| Policy Level | Burkina Faso | Mali | Niger | Kenya | Malawi | Mozambique |
|---|---|---|---|---|---|---|
| Broad health sector strategies and policies | 2011–2020 National Health Plan, supports C-IMCI 2008 Integrated Community Health Intervention Strategy (no curative) |
2009 Health Sector Policy does not mention CHWs or iCCM (section on improving human resources for health does not mention CHWs) | 2002 National Health Policy (does not mention iCCM) | 2005–2010 Health Sector Strategic Plan recognises CHWs 2007 Community Strategy recognises CHWs as first level of care |
2011–2016 Malawi Health Sector Strategic Plan mentions iCCM and recommends its expansion to all ages 2007 National Policy: Acute Respiratory Infections Control authorises antibiotics by Health Surveillance Assistants (HSAs) for pneumonia |
2007–2012 National Health Strategic Plan mentions CHWs and community treatment 2004 Community Involvement Strategy mentions CHWs and community treatment |
| Child health plans | 2007 Child Survival Strategy only covers facility level | 2008 Child Survival Strategy acknowledges C-IMCI: volunteers for health promotion | 2008–2015 Child Survival and Development Strategy mentions strengthening community-level interventions with curative care at facilities | 2008–2012 Strategic Plan for Accelerated Child Survival and Development | 2006 National Newborn and Child Health Policy proposes revitalisation of CHWs (APEs), treatment at community level and newborn care | |
| CCM and IMCI Programme Implementation guidelines | 2010–2014 Strategic Plan for C-IMCI details treatment by CHWs for malaria, diarrhoea and pneumonia 2009 CHW training guidelines for acute respiratory infections |
2010 Implementation Guidelines for Essential Community Services (SEC) details treatment by CHWs for malaria, diarrhoea, pneumonia and home visits 2011 CHW training guidelines for treatment of malaria, pneumonia, diarrhoea and home visits |
2012 Minimum Package of Services for Case de Santé: paid ASCs and nurses treating malaria, diarrhoea and pneumonia, newborn 2006 CHW (ASC) training guidelines for treatment of malaria, diarrhoea and pneumonia |
2011 Household and Community Integrated Management of Child Illness Strategy includes iCCM components 2012 draft CHW training guidelines for treatment of malaria, diarrhoea and home visits |
2008 HSA Training Manual for iCCM 2010 Maternal and Neonatal Health Community-Based Maternal and Neonatal Care: HSA Manual |
2010 CHW (APE) Revitalisation Programme details treatment for malaria, diarrhoea and pneumonia 2010 CHW (APE) curriculum for treating malaria, diarrhoea, pneumonia and home visits |
Across all country case studies, iCCM did not exist as a standalone policy nor was it referred to by this name. In Burkina Faso, Niger, Malawi and Kenya, it was viewed and referred to as a community-based form of the predecessor programme ‘Integrated Management of Childhood Illness’ (IMCI). In Mozambique, it was seen as a revitalisation of the CHW programme, and in Mali, it was viewed as a reformulation of essential, community-level services (this was also somewhat the case in Niger). In all study countries, CHWs responsible for providing iCCM also provided other child health services, as well as some services for adults. While in all six countries, the policy intended for CCM services to be integrated, in reality, and as described below in the section on policy process, there were often obstacles to achieving this.
Context
The history of primary health care (PHC) and CHW programmes in each country had a substantial, albeit nuanced, impact on iCCM policies. In general, commitment to PHC was supportive of iCCM policy as iCCM was perceived to fit well within the PHC tradition. The Francophone countries and Mozambique all had strong PHC commitments. However, in Mali, despite this commitment, community organisations (ASACO) that were responsible for primary care services strongly resisted iCCM policy change as it involved the establishment of a new paid cadre of CHWs, and the ASACO were concerned about the feasibility of sustaining CHW payments. Conversely, Malawi, which had a less strong tradition of PHC, moved forward rapidly with iCCM, in part because it had already developed a cadre of paid CHWs in response to the country's health worker shortages.
Countries with existing CHW programmes that provided a strong platform for the provision of iCCM services had an easier process of policy development. All six countries had existing CHW cadres, but their history, characteristics and ability to support iCCM policy varied widely (Table1). Both Niger and Malawi had pre-existing cadres of paid and relatively well-trained CHWs that facilitated iCCM policy. In Mozambique and Mali, iCCM policy development became entwined with, and slowed by, the need to create a new cadre or upgrade existing cadres of CHWs. In Kenya, most CHWs to date have worked with NGO projects, and the government is struggling with how to expand NGO CHW volunteer programmes into a national programme. Burkina Faso faced similar challenges in terms of expanding CHW volunteer programmes.
Other contextual factors such as legal frameworks (for example, regulations prohibiting CHWs from dispensing antibiotics that existed in Burkina Faso, Kenya and Mozambique), technological factors (such as the availability of rapid diagnostic tests for malaria, enabling CHWs to target the use of expensive artemisinin combination therapies) and political factors (such as changes in political leadership) were all found to be relevant to iCCM policy development, but in no cases proved to be insurmountable barriers or critical determining factors.
Actors
High-level policy champions for iCCM were rare. While President Mamadou Tandja championed community health posts in Niger and Minister Ivo Garrido pushed for the revitalisation of the CHW programme in Mozambique, their support was broadly around community health, rather than iCCM specifically.
The most critical actors in driving iCCM policy development were technical officers within the Ministry of Health (MoH), supported by key development partners, particularly WHO and UNICEF and, to a slightly lesser extent, USAID and its collaborating agencies. Often senior MoH policymakers, particularly those with a clinical background, were initially resistant to iCCM due to concerns about CHWs treating more complex conditions, and it took time and effort to convince them of the benefits of this strategy. Support for iCCM varied across different MoH technical units and depended on where responsibility for iCCM was located within the ministry. For example, where malaria control programmes were well established, well funded and distinct from iCCM (as was the case in Burkina Faso), there were greater obstacles to progress on integration, as malaria control programmes had little incentive to participate in iCCM when they were already providing home-based care for both children and adults. In contrast, progress was easier in contexts such as Mozambique, where CHWs implementing iCCM received high-level support from two strong departments (Women and Child Health, and Health Promotion) and were integrated into the malaria programme.
Professional associations, such as medical associations, provided some resistance to iCCM policy, but typically did not have a powerful voice in the policy process. While Ministries of Health sometimes engaged other Ministries, the Ministry of Finance was not involved in iCCM policy discussions in any of the six countries. Finally, there were several stakeholders – such as communities, CHWs and civil society – who likely held positive positions regarding iCCM policy, but were not mobilised through the policy process.
Policy process
iCCM policy often came onto the policy agenda in response to countries' ambitions to achieve the Millennium Development Goals (MDGs), particularly MDG 4. There was a widespread perception that existing strategies (such as IMCI) were not working and ‘children were dying at home’. This perception was supported by a number of country-specific reviews that demonstrated that IMCI was not being implemented as planned, and in particular its community component was weak (Ministry of Health & Population Malawi 2006; Mullei et al. 2008). At the same time, policymakers were learning about iCCM strategies from trusted development partners, such as the UN agencies, who were beginning to promote this strategy. Thus, there was a window of opportunity for policy reform.
The speed with which policymakers seized upon this window depended upon the contextual factors described earlier and the availability of funding, particularly external funding. For example, in Burkina Faso, the promise of a grant from the Partnership for Maternal, Neonatal and Child Health encouraged policymakers to move forward with iCCM; funding negotiations also led to the inclusion of CCM for pneumonia, to which policymakers were initially resistant. Even in Malawi and Niger, where the government pays CHW salaries, the remaining funding for iCCM programmes came from development partners. In other countries, to date, development partners have been supporting CHW salaries, supplies and training.
Policy formulation was often lengthy, and countries approached it in a piecemeal fashion, developing parts of the iCCM policy as opportunities presented themselves (for example, as new training guidelines for CHWs were being developed, or a new community health strategy produced). iCCM touches upon multiple actors within the MoH, and the need to consult with different technical units also slowed policy formulation. Issues around coordination within the MoH were particularly problematic when programme-specific funding, such as for malaria programmes, reduced incentives for an integrated approach. Coordinating mechanisms such as technical working groups helped to address some coordination issues, but did not fully resolve them.
The role of evidence
A variety of types of scientific evidence, both local and international, was perceived to have contributed to policy development. Research studies, such as the Lancet series on child survival (Black et al. 2003; Bryce et al. 2003; Jones et al. 2003), and local studies were used to identify potential interventions, assess their feasibility and prioritize them. Evidence from in-country sources (such as Demographic and Health Surveys, Multiple Indicator Cluster Surveys, IMCI evaluations, and routine data) was used to identify the most critical issues facing children under 5, geographical areas of the country to prioritize, and to justify expansion of services through community-based care. In-country pilots were commonly used, but were employed in different ways: sometimes to convince policymakers (for example, through pneumonia pilots in Kenya and Burkina Faso), sometimes as a means to demonstrate feasibility (for example, for newborn CCM in Malawi) and sometimes almost as a step in project implementation (as in Niger).
Experiences of other countries were widely referred to by policymakers and were disseminated through site visits and regional meetings. Development partners, notably WHO and UNICEF, acted as knowledge brokers, synthesising and bringing experiences from other countries to the attention of policymakers. The UN agencies were widely perceived to be ‘trusted partners’, and they exercised substantial influence through this role.
In-country policymakers valued local evidence highly and at times questioned the relevance of iCCM evidence from other countries to their own setting. For example, Kenyan policymakers pointed out that their CHW cadres were volunteer community members who were quite different from Malawi's well-trained health surveillance assistants. Where policymakers were initially resistant to elements of iCCM, such as treatment of pneumonia, local evidence could make a critical difference in shifting their views. For example, in Mali, policy resistance was partially overcome by a local study that demonstrated that communities were already practising irrational antibiotic use by purchasing drugs on the market (CREDOS 2009). Where local evidence on key issues was lacking, this had the potential to slow the policy process.
Discussion
Our findings on how iCCM policy content, context, actors, processes and the role of evidence interacted to either facilitate or hinder iCCM policy change across the study countries are summarised in Table4. Commonalities as well as singularities mark how iCCM policy evolved at country level. For example, the MDGs proved a particularly powerful stimulus towards iCCM policy change in all six countries, but many other enabling factors were more nuanced in their effect. While the presence of an existing cadre of CHWs may, a priori, be thought to support iCCM policy change, in Burkina Faso and Mali, concerns about the technical capacity of current CHW cadres limited support. Similarly, evidence and experience from other countries were often an important facilitator, although its effects were mixed in Kenya where policy-makers pointed out differences in country context that potentially undermined the transferability of lessons from elsewhere.
Table 4.
Summary of iCCM policy facilitators and barriers by country
| Burkina | Mali | Niger | Kenya | Malawi | Mozambique | |
|---|---|---|---|---|---|---|
| iCCM Policy Facilitators | ||||||
| Concerns about failure to achieve MDGs | Influential | Influential | Influential | Influential | Influential | Influential |
| Low levels of facility utilisation/children dying at home | Influential | Influential | Influential | Influential | Influential | Influential |
| Established CHW cadre | Unclear or mixed | Unclear or mixed | Influential | Unclear or mixed | Influential | Influential |
| Reinvigoration of community health strategy | Influential | Influential | No effect | Influential | No effect | Influential |
| Exposure to experience of other countries | Influential | Influential | Influential | Unclear or mixed | Influential | Influential |
| Funding opportunity for iCCM | Influential | Influential | Influential | No effect | Unclear or mixed | Influential |
| Donor advocacy | Influential | Influential | Influential | Influential | No effect | Influential |
| High-level political support | No effect | No effect | Influential | No effect | No effect | Unclear or mixed |
| iCCM policy barriers | ||||||
| Concerns about drug resistance (antibiotics and/or antimalarials) | Influential | Influential | No effect | Influential | Influential | Influential |
| Technical capacity of existing CHW Cadre | Influential | Influential | No effect | Unclear or mixed | No effect | Influential |
| Lack of coordination within MOH | Influential | Influential | No effect | Influential | Unclear or mixed | Influential |
| Concerns about long-term financial sustainability | Unclear or mixed | Influential | No effect | Influential | No effect | Influential |
| Laws preventing CHWs from prescribing certain drugs | Influential | No effect | No effect | Influential | No effect | Influential |
Based on the different themes and patterns across the six country cases, we further synthesise the findings into three key areas for future focus:
The alignment of iCCM with existing health systems
The extent to which iCCM policies have been framed to promote strong country ownership and leadership
The sustainability of iCCM programmes.
Alignment
In some study countries (such as Malawi and Niger), iCCM fits easily into the country's health system and policy uptake was rapid, whereas elsewhere, substantial reform was required. Both Mozambique and Mali have long-standing systems of community-level care. In Mali, however, decision-makers concluded that these structures were not suitable for a range of service delivery needs, including iCCM. In Mozambique, existing structures needed to be revitalised. Thus, iCCM policy became entangled in a broader process of reform of community services and CHW cadres.
iCCM was developed as a global strategy, but each country had to review how best to accommodate this new policy and its attending programmatic changes within its own particular policy environment, institutional structures and health system. Policies developed at the global level may take little heed of country-level circumstances: more work with country partners on the adaptations required is needed (Paina & Peters 2012). This may entail changing the nature of the global strategy to align more closely to local environments or investing in policy reform that supports the broader health system investments required.
Efforts to enhance the fit of iCCM with country health systems were not helped by the lack of continuity with predecessor global programmes, notably IMCI. Country policy processes do not occur in a linear or top down way, but in a highly incremental fashion (Lindblom 1959), and country policymakers typically sought to build on the IMCI legacy by aligning iCCM programmes with the community component of IMCI. However, the international community had not framed iCCM in a way that took advantage of this legacy or sought to promote continuity.
Ownership and leadership
Leadership for iCCM policy change came primarily from technical officers, based both in the MoH and in the international organisations, with relatively weak support from political leadership and civil society (including community-based stakeholders or organisations). iCCM was also vulnerable to bureaucratic contestation as it touches upon the mandates of multiple MoH departments and units. It was frequently challenging for technical officers in the maternal and child health department to play a leadership role across other technical units at a similar level within the ministry hierarchy. Where strong, high-level leadership and coordination were exercised, this both eased policy development and was conducive to creating a more integrated policy. Unsurprisingly, leadership by mid-level technical officers was particularly contested in settings where multiple programmes competed with each other, and donor support reinforced siloed programmes dependent upon external funding, rather than a more integrated approach driven by government leadership (Kapilashrami & McPake 2012).
Study findings also emphasised the need for both local and global evidences to support and enable policy development. Typically, there was little local evidence available, and policymakers questioned the relevance of evidence from other countries. Setting aside flexible funding to address country-specific research questions could help facilitate the uptake of new health strategies.
Sustainability
This study casts light on the importance of secure and sustainable funding, often neglected during policy formulation processes. In countries that have been hesitant about proceeding with iCCM policy, concerns about sustainable funding were uppermost in policymakers' minds. Conversely, countries that moved forward quickly have identified funding, albeit frequently external funding, to support their initiatives. The long-term sustainability of funding for iCCM is unclear in many countries. The start-up costs of iCCM alone are not large (comprising mainly of training for CHWs and additional drugs), but the real cost lies with creating a strong community-level service delivery platform, including ongoing supervision and salaries for CHWs, as well as reliable drug supplies. Despite the critical need to secure sustainable financing, to date, Ministries of Finance have not been involved in policy discussions on iCCM, nor are there open discussions with development partners about this issue, and plans to ensure financial sustainability are weak or non-existent. Additional economic analysis to demonstrate the cost-effectiveness of iCCM compared with other strategies to expand service coverage, open discussions regarding financing strategies to sustain CHW and iCCM programmes and active engagement of political leadership are all needed in order to promote long-term sustainability.
As with any retrospective qualitative study, there are some limitations to our research. In some instances, iCCM policy change took place several years prior to data collection and respondents may have had difficulty recalling details of the policy process. Triangulation between documents and interviews helped with this issue. Study teams also sought to collect data on levels of external funding for iCCM, but such data were not easily available. Despite these limitations, the analytic generalizations drawn from examining six diverse case studies in depth give pause for reflection and also suggest strategies to facilitate policy change for iCCM and similar programmes.
Conclusion
While other studies have reported on the development of iCCM policy (Marsh et al. 2008; George et al. 2012; de Sousa et al. 2012) and on the role of CHWs in providing iCCM (George et al. 2012), these are based on quantitative surveys. As such they describe the extent of policy change in Sub-Saharan Africa, but are less helpful in explaining why this policy change has or has not occurred. Our research also found that there is a plethora of documents at country level and that while iCCM tends to be detailed in operational documents, the evolution of policy documents or processes is neither linear nor immediate. The detailed case studies reported here help explain different patterns in policy adoption across countries, and the considerations involved.
There are many possible barriers to pro-poor policy change; the scale of problems affecting the poor may not be appreciated, solutions may be complex and expensive and therefore unappealing, and the poor often lack influence at the policy level (Bird & Busse 2006). While it is critical to recognise that there are no ‘magic bullets’ that support pro-poor policy change, and that a deep understanding of the country context and interests of the actors involved is key, Box 1 summarises some of the main policy-relevant lessons from this study of iCCM in six countries.
Box 1 Key policy relevent conclusions from the study.
Alignment
More systematic thought should be given to how to adapt global level policies to the specificities of different health policy and system environments
Global initiatives likely stand a better chance of adoption if they explicitly build upon prior initiatives and programs
Ownership and leadership
Certain child health issues within low income countries could benefit from more high level political leadership
Verticalized health programming, bolstered by earmarked funding from donors can undermine efforts for more integrated policy approaches, such as that embodied by iCCM
Small pots of flexible funding for local research could help provide contextspecific evidence that may be critical in influencing policy-maker positions on iCCM
Sustainability
There is an urgent need to address questions about the long term sustainability of CHW programs, that are closely linked to policy-maker positions on iCCM.
In the case of iCCM, the network of policy actors has remained small and technically focused, and there is scope for broadening engagement, and particularly for involving communities. However, the most critical concerns focus on the complexity and expense of iCCM: although it may seem a relatively small and self-contained policy, it can have far reaching implications for the health system. By and large iCCM has been disseminated internationally as a standardised package of services, and little systematic thought has been given to how to accommodate differences across countries in existing institutional and system structures. This lack of consideration for local institutional features and the fit of new programmes has previously been noted as a barrier to scaling up (Gericke et al. 2005). In terms of expense, to- date development partner support to iCCM has been a critical enabler, but donor aid is frequently unpredictable (Lane & Glassman 2007), and this unpredictability may deter policymakers from embarking on CHW programmes (Pallas et al. 2013). Finding solutions that leverage aid but also secure more sustainable domestic finance is key.
Acknowledgments
This study was funded by UNICEF (#43114640) and the USAID TRAction project (FY11-G06-6990). Both UNICEF and USAID staff advised the study team, but did not substantively affect the study design, instruments or interpretation of data. The team would like to acknowledge the support of the Technical Advisory Group, including Sam Adjei, Neal Brandes,Dave Nichols, Kumanan Rasanathan, Jim Sherry and Steve Wall. We also recognize the efforts of UNICEF regional and country offices, especially the support of Rory Nefdt and Mariame Sylla. Professor Gill Walt and Dr. Irene Agyepong kindly commented on an early draft of the report. The study team would like to thank respondents in all study countries for the time and insights they contributed to this project, without which this study would not be possible.
References
- Bird K. Busse S. Pro-poor policy: An overview. London: ODI and Swiss Agency for Development and Cooperation; 2006. poverty-wellbeing.net: [Google Scholar]
- Black RE, Morris SS. Bryce J. Where and why are 10 million children dying every year? Lancet. 2003;361:2226–2234. doi: 10.1016/S0140-6736(03)13779-8. [DOI] [PubMed] [Google Scholar]
- Bryce J, El Arifeen S, Pariyo G, et al. Reducing child mortality: can public health deliver? Lancet. 2003;362:159–164. doi: 10.1016/s0140-6736(03)13870-6. [DOI] [PubMed] [Google Scholar]
- CORE Group, Save the Children, BASICS, MCHIP. Community Case Management Essentials: Treating Common Childhood Illness in the Community, a guide for Program Managers. Washington DC: CORE Group; 2010. [Google Scholar]
- CREDOS. Prise en charge au niveau communautaire des infections respiratoires aiguës chez les enfants de moins de 5 ans. Bamako, Mali: 2009. [Google Scholar]
- Elliott H. Popay J. How are policy makers using evidence? Models of research utilisation and local NHS policy making. Journal of Epidemiology and Community Health. 2000;54:461–468. doi: 10.1136/jech.54.6.461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fulton BD, Scheffler RM, Sparkes SP, Auh EY, Vujicic M. Soucat A. Health workforce skill mix and task shifting in low income countries: a review of recent evidence. Human Resources for Health. 2011;9:1. doi: 10.1186/1478-4491-9-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- George A, Young M, Nefdt R. Community health workers providing government community case management for child survival in sub-saharan Africa: who are they and what are they expected to do? American Journal of Tropical Medicine and Hygiene. 2012;87(5 Suppl):85–91. doi: 10.4269/ajtmh.2012.11-0757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gericke CA, Kurowski C, Ranson MK. Mills A. Intervention complexity–a conceptual framework to inform priority-setting in health. Bulletin of the World Health Organization. 2005;83:285–293. [PMC free article] [PubMed] [Google Scholar]
- Haines A, Sanders D, Lehmann U, et al. Achieving child survival goals: potential contribution of community health workers. Lancet. 2007;369:2121–2131. doi: 10.1016/S0140-6736(07)60325-0. [DOI] [PubMed] [Google Scholar]
- Jones G, Steketee RW, Black RE, Bhutta ZA. Morris SS Bellagio Child Survival Study Group. How many child deaths can we prevent this year? Lancet. 2003;362:65–71. doi: 10.1016/S0140-6736(03)13811-1. [DOI] [PubMed] [Google Scholar]
- Kapilashrami A. McPake B. Transforming governance or reinforcing hierarchies and competition: examining the public and hidden transcripts of the Global Fund and HIV in India. Health Policy Plan; 2012. [DOI] [PubMed] [Google Scholar]
- Lane C. Glassman A. Bigger and better? Scaling up and innovation in health aid. Health Affairs (Millwood) 2007;26:935–948. doi: 10.1377/hlthaff.26.4.935. [DOI] [PubMed] [Google Scholar]
- Lehmann U, Van Damme W, Barten F. Sanders D. Task shifting: the answer to the human resources crisis in Africa? Human Resources for Health. 2009;7:49. doi: 10.1186/1478-4491-7-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindblom CE. The science of “muddling through”. Public Administration Review. 1959;19:79–85. [Google Scholar]
- Marsh DR, Gilroy KE, Van de Weerdt R, Wansi E. Qazi S. Community case management of pneumonia: at a tipping point? Bulletin of the World Health Organization. 2008;86:381–389. doi: 10.2471/BLT.07.048462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ministry of Health and Population Malawi. IMCI Approach Policy for Accelerated Child Survival and Development in Malawi: Scaling up of High Impact Interventions in the Context of Essential Health Package, Ministry of Health and Population, Community Health Services Unit. Lilongwe: National government of Malawi; 2006. [Google Scholar]
- Mullei K, Wafula F. Goodman C. A case study of integrated management of childhood illness (IMCI) implementation in Kenya, Consortium for Research on Equitable Health Systems. 2008.
- Paina L. Peters DH. Understanding pathways for scaling up health services through the lens of complex adaptive systems. Health Policy Plan. 2012;27:365–373. doi: 10.1093/heapol/czr054. [DOI] [PubMed] [Google Scholar]
- Pallas SW, Minhas D, Perez-Escamilla R, Taylor L, Curry L. Bradley EH. Community health workers in low- and middle-income countries: what do we know about scaling up and sustainability? American Journal of Public Health. 2013;103:e74–e82. doi: 10.2105/AJPH.2012.301102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh P. Sachs JD. 1 million community health workers in sub-Saharan Africa by 2015. Lancet. 2013;382:363–365. doi: 10.1016/S0140-6736(12)62002-9. [DOI] [PubMed] [Google Scholar]
- de Sousa A, Tiedje KE, Recht J, Bjelic I. Hamer DH. Community case management of childhood illnesses: policy and implementation in Countdown to 2015 countries. Bulletin of the World Health Organization. 2012;90:183–190. doi: 10.2471/BLT.11.093989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNICEF. Integrated Community Case Management: WHO/UNICEF Joint Statement. New York: UNICEF; 2012. [Google Scholar]
- Walt G. Gilson L. Reforming the health sector in developing countries: the central role of policy analysis. Health policy and planning. 1994;9:353–370. doi: 10.1093/heapol/9.4.353. [DOI] [PubMed] [Google Scholar]
- WHO Roll Back Malaria. Scaling up Home Based Management of Malaria: From Research to Implementation. Geneva: WHO; 2004. [Google Scholar]
- WHO. Community-based management of Severe Acute Malnutrition: Joint statement by WHO, WFP and UNICEF. Geneva: WHO; 2007. [Google Scholar]
- WHO/UNICEF FCH. Management of Pneumonia in Community Settings: WHO/UNICEF joint statement. UNICEF/WHO Geneva; 2004a. , (ed. [Google Scholar]
- WHO/UNICEF. Clinical Management of Acute Diarrhoea: WHO/UNICEF Joint Statement. WHO: Geneva; 2004b. [Google Scholar]
- WHO/Unicef. WHO/Unicef Joint Statement on Home Visits for the Newborn Child: A strategy to Improve Survival. Geneva: WHO; 2009. [PubMed] [Google Scholar]
- Woelk G, Daniels K, Cliff J, et al. Translating research into policy: lessons learned from eclampsia treatment and malaria control in three southern African countries. Health Research Policy and Systems. 2009;7:1–14. doi: 10.1186/1478-4505-7-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yin RK. Case Study Research: Design and Methods. Thousand Oaks, CA: SAGE; 2009. 5th edn. [Google Scholar]


