Abstract
Purpose: We conducted a clinical study to evaluate the effects of neurotization, especially comparing the total contralateral C7 (CC7) root transfer to hemi-CC7 transfer, on total root avulsion brachial plexus injuries (BPI). Methods: Forty patients who received neurotization for BPI were enrolled in this prospective study. Group 1 (n = 20) received hemi-CC7 transfer for hand function, while group 2 (n = 20) received total-CC7 transfer. Additional neurotization included spinal accessory, phrenic, and intercostal nerve transfer for shoulder and elbow function. The results were evaluated with an average of 6 years follow-up. Results: Group 1 had fewer donor site complications (15%) than group 2 (45%); group 2 had significantly better hand M3 and M4 motor function (65%) than group 1 (30%; P = 0.02). There was no difference in sensory recovery. Significantly, better shoulder function was obtained by simultaneous neurotization on both suprascapular and axillary nerves. Conclusions: Total-CC7 transfer had better hand recovery but more donor complications than hemi-CC7. Neurotization on both supra-scapular and axillary nerves improved shoulder recovery. © 2013 The Authors. Microsurgery published by Wiley Periodicals, Inc. Microsurgery 34:91–101, 2014.
Brachial plexus injuries (BPI) are devastating injuries for trauma patients, especially when presenting with total trunk C5-T1 (the fifth cervical to the first thoracic nerve root) avulsion type, which means, “nothing left over the injured limb.”1,2 These high-energy injuries are mostly caused by traffic accidents, and especially motorcycle accidents.2–4 The mainstream treatments for adult BPI generally focus on surgery and postoperative rehabilitation. The outcomes of nonsurgical conservative treatments such as physical therapy alone and pain-relief medication are seldom satisfactory, especially in root avulsion and complete palsy BPI.2–9
The treatment for brachial plexus avulsion lesions invariably involves the use of neurotization procedures, because neither direct repair nor interpositional nerve grafting can be performed for these irreparable preganglionic lesions.2,3,7,10,11 New treatment guidelines for total root avulsion emphasize the combination of various types of neurotization with ipsilateral intraplexus and extraplexus nerve donors, contralateral cervical seventh (CC7) root donor, and primary or secondary free functioning muscle transfer.1,2,8,9,12 The most commonly used extraplexal nerve donors include the spinal accessory, intercostal, and phrenic nerves (PN).2,7,12,13 The spinal accessory and PNs are frequently used as a neurotizer and transferred to the suprascapular nerve (SSN) for shoulder function recovery.2,11,12 Some surgeons prefer to use the spinal accessory nerve (SAN) in combination with sural nerve graft transfer for neurotization on the musculocutaneous nerve for elbow flexion function.14,15 The intercostal nerves (ICNs) are mainly used for neurotization on the musculocutaneous nerve for elbow flexion, and they may also serve as a neurotizer for axillary nerve function.2,4,11,16,17 After previous success with the proximal portion of the injured upper limb, surgeons have attempted to innervate forearm and hand muscles by using these donor nerves. However, most of the results with neurotization for hand function were disappointing until 1992 when Gu et al. reported success in the restoration of hand function by CC7 transfer.1 Although a number of groups have reported performing CC7 transfer for total avulsion type BPI reconstruction, the results have been variable.1–3,11–13,15,18,19 Some surgeons have used the entire CC7 root as the donor,1,18–23 while others have used selective hemi-CC7 as the donor nerve.3,11–13,15 The purposes of this study were to evaluate the effect of neurotization on total root avulsion type BPI, and to compare the outcomes of hemi-CC7 versus total-CC7 neurotization on median nerve (MN) function.
PATIENTS AND METHODS
We conducted a prospective randomized control trial involving E-Da Hospital, Kaohsiung, and the Department of Biomedical Engineering, National Cheng Kung University, Taiwan. The study was approved by the medical ethics review board of both institutes, and written informed consent was obtained from each patient.
From 2004 to 2008, 105 patients who suffered from total root avulsion BPI were surgically treated by CC7 transfer. The selection criteria of the patients were age under 40 years, the interval between injury and surgery within 6 months, no soft tissue defects of the arm and forearm, undamaged flexor tendons in the hand and forearm, and no previous nerve surgery performed for this BPI.2,10 In addition, the selected patients were required to be motivated and have adequate family and financial support to be able to continue post-operative rehabilitation for at least 2 years. In total, 42 patients suffering from traumatic total arm avulsion type BPI were enrolled from 2004 to 2008. The diagnosis of total arm avulsion type BPI was confirmed by physical examination, electrodiagnostic evaluations including needle electromyography and nerve conduction velocity studies, and magnetic resonance myelography.2,11,12
All of the 42 patients received three to four concomitant surgical procedures at the same time, which included exploration of the injured nerve roots, neurotization (with the spinal accessory, phrenic, and ICN transfer or sural nerve graft) for shoulder and elbow function, and CC7 transfer for hand function. Two patients dropped out of the study after being put in jail due to committing crimes during the third and fourth years of follow-up. Therefore, a total of 40 patients were studied, all of whom received evaluations and complete follow-up for at least 4.5 years. There were 36 male and 4 female patients, ranging in age from 16 to 40 years (average 26.8 ± 6.4 years). We divided the patients into two groups: group 1, using hemi-CC7 for the reconstruction of hand function; group 2, using total-CC7 for hand reconstruction. The surgical procedures for hand reconstruction (hemi-CC7 or total-CC7) were performed after randomization. Permuted block randomization was adopted with blocks of four allocations, with each block containing two hemi-CC7 and two total-CC7 procedures in random order. This allocation was based on a computer-generated list from an independent hand therapist and a research assistant. This randomization method ensured that treatment group numbers were evenly balanced at the completion of each block.24,25 However, taking into consideration the availability of spinal accessory, phrenic, and intercostals nerves, the surgical procedures for reconstructing shoulder and elbow functions were not randomized. The characteristics of the patients in group 1 are listed in Table1, and those of group 2 in Table2.
Table 1.
Patients With Hemi-CC7 for the Hand (Group 1)
| Case No. | Gender | Age (years) | Injury mechanism | OP time after trauma (months) | Shoulder OP | Elbow OP |
|---|---|---|---|---|---|---|
| 1–1 | Male | 28 | MCA | 4 | SA-SS, ICN-Axi | ICN-MCN |
| 1–2 | Male | 19 | High fall | 3.5 | SA-SS | ICN-MCN |
| 1–3 | Female | 23 | MCA | 2 | SA-SS, ICN-Axi | ICN-MCN |
| 1–4 | Male | 40 | MCA | 4 | PN-SS | SA-NG-MCN |
| 1–5 | Male | 37 | MCA | 3.5 | SA-SS | ICN-MCN |
| 1–6 | Male | 35 | MCA | 3 | SA-SS | ICN-MCN |
| 1–7 | Male | 26 | MCA | 3.5 | SA-SS, ICN-Axi | ICN-MCN |
| 1–8 | Female | 28 | MCA | 4 | SA-SS, ICN-Axi | ICN-MCN |
| 1–9 | Male | 22 | MCA | 3.5 | SA-SS | ICN-MCN |
| 1–10 | Male | 30 | High fall | 3 | SA-SS, ICN-Axi | ICN-MCN |
| 1–11 | Male | 38 | MCA | 3 | SA-SS | ICN-MCN |
| 1–12 | Male | 31 | MCA | 4 | SA-SS | ICN-MCN |
| 1–13 | Male | 24 | MCA | 3.5 | PN-SS | SA-NG-MCN |
| 1–14 | Male | 21 | MCA | 4 | SA-SS, ICN-Axi | ICN-MCN |
| 1–15 | Male | 16 | MCA | 3 | SA-SS | ICN-MCN |
| 1–16 | Male | 18 | MCA | 4 | SA-SS | ICN-MCN |
| 1–17 | Male | 26 | MCA | 3.5 | SA-SS, ICN-Axi | ICN-MCN |
| 1–18 | Male | 23 | MCA | 3 | SA-SS | ICN-MCN |
| 1–19 | Male | 27 | MCA | 5 | SA-SS, ICN-Axi | ICN-MCN |
| 1–20 | Male | 19 | MCA | 3.5 | SA-SS | ICN-MCN |
ICN-Axi: Intercostal nerve neurotization on axillary nerve; ICN-MCN: Intercostal nerve neurotization on the musculocutaneous nerve; MCA: Motorcycle accident; OP: Operation; PN-SS: Phrenic nerve neurotization on the suprascapular nerve; SA-NG-MCN: Spinal accessory nerve combined sural nerve graft, and neurotization on the musculocutaneous nerve; SA-SS: Spinal accessory nerve neurotization on the suprascapular nerve.
Table 2.
Patients With Total-CC7 for the Hand (Group 2)
| Case No. | Gender | Age (years) | Injury mechanism | Delay time (months) | Shoulder OP | Elbow OP |
|---|---|---|---|---|---|---|
| 2–1 | Male | 22 | MCA | 3 | SA-SS | ICN-MCN |
| 2–2 | Male | 30 | MCA | 4 | PN-SS | SA-NG-MCN |
| 2–3 | Male | 18 | MCA | 3.5 | SA-SS, ICN-Axi | ICN-MCN |
| 2–4 | Male | 25 | MCA | 4 | SA-SS | ICN-MCN |
| 2–5 | Male | 28 | MCA | 3.5 | SA-SS, ICN-Axi | ICN-MCN |
| 2–6 | Female | 19 | MCA | 2 | SA-SS | ICN-MCN |
| 2–7 | Male | 33 | MCA | 4 | SA-SS, ICN-Axi | ICN-MCN |
| 2–8 | Male | 40 | MCA | 3.5 | SA-SS | ICN-MCN |
| 2–9 | Male | 16 | MCA | 3 | SA-SS, ICN-Axi | ICN-MCN |
| 2–10 | Male | 28 | MCA | 3 | SA-SS, ICN-Axi | ICN-MCN |
| 2–11 | Male | 27 | MCA | 3.5 | SA-SS | ICN-MCN |
| 2–12 | Male | 31 | High fall | 4 | SA-SS, ICN-Axi | ICN-MCN |
| 2–13 | Male | 21 | MCA | 4 | PN-SS | SA-NG-MCN |
| 2–14 | Male | 30 | MCA | 5 | SA-SS, ICN-Axi | ICN-MCN |
| 2–15 | Male | 26 | MCA | 4 | SA-SS | ICN-MCN |
| 2–16 | Male | 23 | MCA | 3.5 | SA-SS | ICN-MCN |
| 2–17 | Male | 29 | MCA | 4 | PN-SS | SA-NG-MCN |
| 2–18 | Male | 35 | MCA | 3.5 | SA-SS, ICN-Axi | ICN-MCN |
| 2–19 | Female | 28 | MCA | 4 | SA-SS, ICN-Axi | ICN-MCN |
| 2–20 | Male | 32 | MCA | 3.5 | SA-SS | ICN-MCN |
ICN-Axi: Intercostal nerve neurotization on axillary nerve; ICN-MCN: Intercostal nerve neurotization on the musculocutaneous nerve; MCA: Motorcycle accident; OP: Operation; PN-SS: Phrenic nerve neurotization on the suprascapular nerve; SA-NG-MCN: Spinal accessory nerve combined sural nerve graft, and neurotization on the musculocutaneous nerve; SA-SS: Spinal accessory nerve neurotization on the suprascapular nerve
Surgical Technique
The technique of dissection and division of the CC7 nerve followed by its transfer to the injured brachial plexus by means of pedicle vascularized ulnar nerve grafting (VUNG) has been well described in the literature.1–3,12,13,15,18–23 In this study, we performed combined neurotization procedures for reconstruction of shoulder and elbow functions, and CC7 neurotization on the MN for reconstruction of hand function as one stage surgery. We used two surgical positions for our patients as described below.
Under general anesthesia, the patient was placed in a semi-sitting position with bilateral supraclavicular approach at the same time. On the lesion side, after confirming that no proximal cervical root avulsed stump could be used as a neurotizer, we identified the SAN and PN for the subsequent shoulder and elbow neurotization procedures. The second incision was made on the contralateral healthy side, and then the SSN, C5, C6, C7, C8, and T1 were all exposed after careful dissection. In the group 1 patients, we divided the C7 nerve sheath longitudinally, and identified the nerve division that provided primarily shoulder adduction through pectoralis muscle contraction. In most cases, the anterior-superior half of the nerve was divided and transferred.2,3,12,13,15 We termed this as anterior division (AD) hemi-CC7 transfer. In the group 2 patients, we divided the C7 at the common trunk and defined this as total-CC7 transfer. For every patient who received CC7 transfer, we blocked the nerve with 2 ml of 2% lidocaine before cutting the nerve, as recommended by Gu et al.1,20
After bilateral supraclavicular exploration had been performed, we divided the motor branch of the SAN in the lesion site, and transferred it to the SSN using a 10-0 nylon coaptation suture, the so-called shoulder neurotization procedure (Fig.1). In total, 35 patients received this SAN to SSN neurotization surgery. Five patients (2 in group 1 and 3 in group 2) who had ipsilateral severe chest trauma (flail chest and multiple rib fractures with hemothorax) that was possibly damaging the ICN motor function, received PN transfer to SSN as the shoulder neurotization procedure. The reason for performing PN to SSN in reconstructing shoulder function in these five patients was that the damaged ICN could not be harvested for reconstruction of elbow function; hence, we needed to use the SAN combined with sural nerve graft transfer to the musculocutaneous nerve (MCN). In these five patients, sural nerve grafts were also harvested for the subsequent SAN neurotization to MCN procedure. These clinical conditions had been taken into considerations during the initial design of this study. Therefore, only two different CC7 transfer methods for hand function were randomized, but not in the shoulder and elbow reconstruction methods. We performed simple suturing of the bilateral neck wounds after the above procedures had been completed.
Figure 1.

SAN to SSN neurotization was performed to reconstruct shoulder function. The coaptation suture was accomplished using 10-0 nylon sutures. [Color figure can be viewed in the online issue, which is available at wileyonlinelibrary.com.]
The patient was then put in the supine position and redraped. We performed an anterior chest wall incision to explore the third to seventh ribs, and then harvested four to five branches of ICNs. The axillary nerve was also identified from anterior subaxillary exploration in 17 patients (8 in group 1 and 9 in group 2). The anterior chest wall incision was then extended to the injured arm and forearm. The MCN and MN were identified over the upper third of the medial aspect of the arm, and dissection was then extended to the forearm and wrist level. The VUNG, based on the superior ulnar collateral vessels (SUCV) was harvested from the injury side upper extremity. It was very important to identify and protect the SUCV during ulnar nerve dissection, as the blood supply of this entire pedicle vascularized VUNG was based on the patency of this vessel (Fig.2). At this point, the neurotization procedures including the coaptation of 2 or 3 ICN with the MCN in 35 patients, SAN combined with sural nerve graft transfer to the MCN in 5 patients, and ICN coaptation with the axillary nerve (ICN-Axi) in 17 patients were performed (Fig.3).11,14,16,17 All of the nerve coaptation procedures were performed using 10-0 nylon sutures.
Figure 2.

The SUCV for the VUNG was identified and well protected. [Color figure can be viewed in the online issue, which is available at wileyonlinelibrary.com.]
Figure 3.
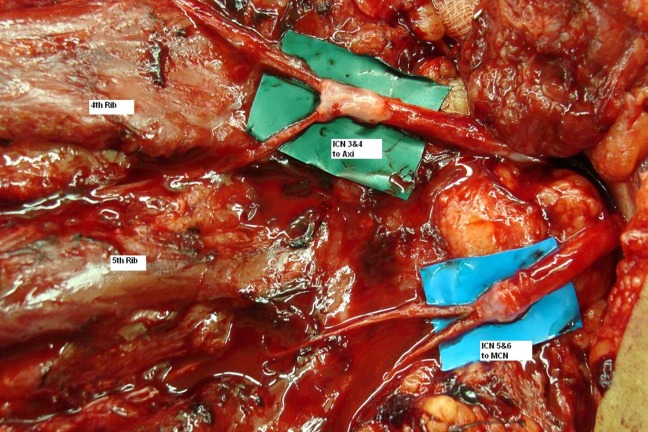
Neurotization procedures were performed with third and fourth ICN transfer to Axi, and fifth and sixth ICN transfer to MCN. The nerve coaptations were done using 10-0 nylon sutures and tissue glue. [Color figure can be viewed in the online issue, which is available at wileyonlinelibrary.com.]
After the neurotization procedures for shoulder and elbow function had been completed, we divided the proximal end of VUNG and performed end-to-end suturing on the entire cross-sectional area of the MN using 9-0 nylon sutures. The distal end of VUNG was then brought through the cross-chest route, above the previous ICN to the MCN coaptation site, and then passed underneath the dissected subcutaneous tunnel to the opposite side of the supraclavicular area for CC7 coaptation. The hemi-CC7 in group 1 and total-CC7 in group 2 were coapted with the nerve ends of VUNG by using 10-0 nylon microsutures (Fig.4). We did not perform ulnar vessel anastomosis (the so called supercharge procedure) in our series,19 because the distal stumps of VUNG nerve ends showed adequate blood supply coming from the SUCV in all of the patients. The whole surgical field, including the ICN-MCN and cross-chest CC7 is shown in Figure5. After all of the wounds had been sutured, a custom made brace with a halo was placed on the patient. This brace kept the injured arm at 45° abduction and in anterior flexion. The halo prevented lateral movement of the head, and reduced the risk of tearing the coaptation sutures.12
Figure 4.
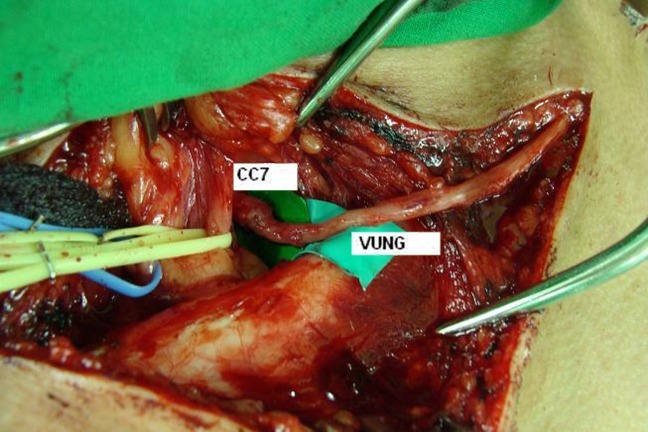
After a cross-chest route transfer, the distal end of VUNG was sutured to the nerve ending of total-CC7 (group 2 patients) with 10-0 nylon microsutures. [Color figure can be viewed in the online issue, which is available at wileyonlinelibrary.com.]
Figure 5.
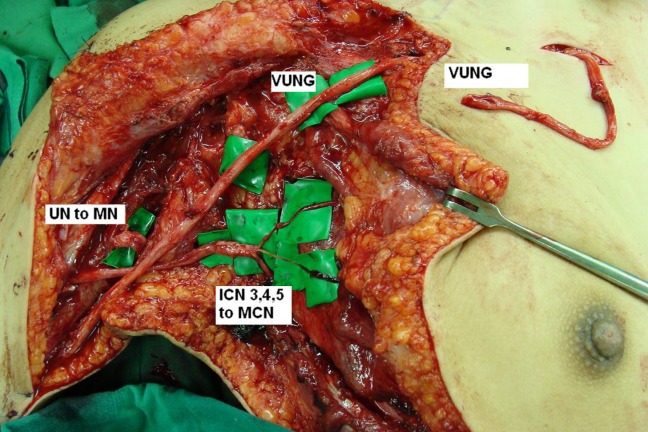
The whole surgical field of neurotization for BPI, including ICN-MCN and cross-chest CC7 transfer with VUNG through the subcutaneous tunnel. [Color figure can be viewed in the online issue, which is available at wileyonlinelibrary.com.]
Post-Op Rehabilitation
The custom made halo brace was used for 6 weeks, and then physical therapy with a passive range of motion and slow-pulse electrical stimulation was started immediately.2,12 Home electrical stimulation was provided for all of the patients with a portable slow pulse stimulation device that the patient was instructed to use for 4 to 6 hours per day for a minimum of 2 years, or until antigravity motor function (M3) occurred. The rehabilitation programs also included contralateral shoulder training in forceful repeated adduction and internal rotation, repeated elbow extension, and forearm rotation. These physical therapy maneuvers might enhance the dependent motor recovery of the lesion site.2,12,15,19,26
Post-Op Evaluation
Each patient was followed up at the outpatient clinic 2 weeks after hospital discharge, then 1 month later, and every 3 months thereafter. The results of motor recovery (based on British Medical Research Council scale, BMRC),2,3,11,15 shoulder range of motion, sensory recovery,12,26 and donor site complications were evaluated in all patients by an independent hand therapist with average of 6 years of follow-up. We defined the donor complications as significant if either the sensory or motor defect over the donor's upper limb persisted for more than 6 months without improvement.13,27
Statistics
Statistical analysis was performed with SPSS version 17.0 (SPSS, Chicago, IL). Independent t-tests were used to examine the differences between groups 1 and 2 in age, surgical delay time, motor recovery, shoulder range of motion, and sensory recovery. The complications in both groups were compared by the chi-square test. One-way ANOVA was used to compare the effects of the neurotization procedures (SA-SS, PN-SS, and SA-SS + ICN-Axi) on shoulder function. The differences in elbow function between SA-NG-MCN and ICN-MCN were examined by the independent t-test. The significant level was set at P < 0.05.
RESULTS
The average operation time for the 40 patients was 12.5 hours (range 9.5–16.5 hours), and the results are shown in Table3 (group 1) and Table4 (group 2). The average follow-up time was 6 years (range 4.5–8 years). There were no differences in age and surgical delay between the groups (Table5).
Table 3.
Postoperative Evaluation in Group 1 (Hemi-CC7)
| Case No. | SMR | SEL (degree) | SAB (degree) | EMR | HMR | Hand sensory | Complications |
|---|---|---|---|---|---|---|---|
| 1–1 | M2 | 30 | 35 | M4 | M1 | S2 | No |
| 1–2 | M4 | 100 | 70 | M4 | M3 | S3 | No |
| 1–3 | M4 | 125 | 80 | M4 | M2 | S3 | No |
| 1–4 | M2 | 15 | 30 | M2 | M1 | S2 | DN, MW |
| 1–5 | M3 | 80 | 60 | M3 | M1 | S2 | No |
| 1–6 | M2 | 25 | 30 | M3 | M0 | no | No |
| 1–7 | M4 | 95 | 105 | M4 | M3 | S3 | DN |
| 1–8 | M3 | 90 | 85 | M4 | M2 | S2 | No |
| 1–9 | M3 | 75 | 85 | M4 | M2 | S2 | No |
| 1–10 | M4 | 125 | 100 | M4 | M4 | S3 | No |
| 1–11 | M3 | 60 | 80 | M4 | M2 | S3 | No |
| 1–12 | M2 | 35 | 30 | M3 | M1 | S2 | DN, MW |
| 1–13 | M3 | 70 | 80 | M3 | M1 | S2 | No |
| 1–14 | M4 | 130 | 100 | M4 | M3 | S3 | No |
| 1–15 | M3 | 75 | 85 | M2 | M1 | no | No |
| 1–16 | M3 | 90 | 75 | M4 | M2 | S2 | No |
| 1–17 | M4 | 120 | 90 | M4 | M3 | S3 | No |
| 1–18 | M3 | 65 | 60 | M3 | M0 | No | No |
| 1–19 | M4 | 145 | 120 | M4 | M3 | S3 | No |
| 1–20 | M3 | 75 | 90 | M4 | M2 | S3 | No |
DN: Donor numbness; EMR: Elbow motor recovery; HMR: Hand motor recovery; MW: Motor weakness; SAB: Shoulder abduction; SEL: Shoulder elevation; SMR: Shoulder motor recovery.
Table 4.
Postoperative Evaluation in Group 2 (total-CC7)
| Case No. | SMR | SEL (degree) | SAB (degree) | EMR | HMR | Hand sensory | Complications |
|---|---|---|---|---|---|---|---|
| 2–1 | M3 | 70 | 75 | M4 | M3 | S3 | DN, MW |
| 2–2 | M3 | 60 | 50 | M2 | M1 | no | DN |
| 2–3 | M4 | 120 | 100 | M4 | M4 | S3 | no |
| 2–4 | M3 | 75 | 65 | M4 | M3 | S3 | no |
| 2–5 | M4 | 110 | 90 | M4 | M4 | S3 | no |
| 2–6 | M3 | 85 | 100 | M3 | M2 | S3 | no |
| 2–7 | M4 | 140 | 130 | M4 | M2 | S2 | no |
| 2–8 | M2 | 25 | 20 | M3 | M2 | S3 | DN, MW |
| 2–9 | M3 | 95 | 85 | M4 | M3 | S3 | no |
| 2–10 | M4 | 120 | 115 | M4 | M3 | S3 | no |
| 2–11 | M3 | 60 | 95 | M3 | M3 | S3 | DN, MW |
| 2–12 | M4 | 110 | 95 | M4 | M4 | S3 | no |
| 2–13 | M2 | 15 | 10 | M2 | M1 | no | no |
| 2–14 | M4 | 95 | 85 | M4 | M4 | S3 | no |
| 2–15 | M3 | 75 | 80 | M3 | M3 | S2 | no |
| 2–16 | M3 | 65 | 75 | M3 | M2 | S2 | DN, MW |
| 2–17 | M3 | 90 | 75 | M3 | M3 | S2 | DN |
| 2–18 | M3 | 85 | 95 | M4 | M3 | S3 | DN, MW |
| 2–19 | M4 | 135 | 120 | M4 | M2 | S2 | DN |
| 2–20 | M4 | 95 | 100 | M4 | M3 | S2 | DN, MW |
DN: Donor numbness; EMR: Elbow motor recovery; HMR: Hand motor recovery; MW: Motor weakness; SAB: Shoulder abduction; SEL: Shoulder elevation; SMR: Shoulder motor recovery
Table 5.
Comparison Between Group 1 and 2
| Group 1 (N = 20) | Group 2 (N = 20) | |
|---|---|---|
| Age (years) | 26.6 ± 6.9 | 27.1 ± 6.0 |
| Surgical delay (months) | 3.5 ± 0.6 | 3.6 ± 0.6 |
| SELV (degree) | 81.3 ± 36.8 | 86.2 ± 32.5 |
| SABD (degree) | 74.5 ± 26.3 | 83.0 ± 29.8 |
| SMR | 3.2 ± 0.7 | 3.3 ± 0.7 |
| EMR | 3.6 ± 0.7 | 3.5 ± 0.7 |
| HNRa | 1.9 ± 1.1 | 2.8 ± 0.9 |
| Complicationsa | 15% | 45% |
| Hand sensory ≥ S2 | 85% | 90% |
Significant difference between group 1 and group 2, P < 0.05.
Surgical delay: Interval between trauma and surgery.
EMR: Elbow motor recovery; HMR: Hand motor recovery; SAB: Shoulder abduction; SEL: Shoulder elevation; SMR: Shoulder motor recovery
Shoulder Function
Sixteen patients (80%) in group 1 and 18 patients (90%) in group 2 obtained at least M3 motor recovery of shoulder function. The average degree of shoulder elevation was 81.3 ± 36.8° in group 1 and 86.2 ± 32.5° in group 2, and the average degree of shoulder abduction was 74.5 ± 26.3° in group 1 and 83.0 ± 29.8° in group 2. There were no significant differences in shoulder motor recovery and extent of shoulder elevation and abduction between group 1 and 2 (Table5). In addition to the comparisons between the two groups, we also evaluated the effect of single nerve neurotization (SA-SS or PN-SS) compared to the effects of double nerve neurotization (SA-SS combined with ICN-Axi). Of the patients who received double nerve neurotization, 94.1% had shoulder motor recovery ≥ M3, compared with only 78.2% who received single nerve neurotization. SA-SS combined with ICN-Axi had significant better BMRC scores than SA-SS (P < 0.01) and PN-SS (P < 0.01) alone (Fig.6). In addition, the average range of shoulder elevation and abduction in double nerve neurotization (elevation = 110.0 ± 27.3°; abduction = 95.9 ± 21.2°) were significant larger than for single nerve neurotization with SA-SS (elevation = 68.3 ± 21.5°; abduction = 70.8 ± 23.6°) or PN-SS (elevation = 50.0 ± 33.7°; abduction = 49.0 ± 29.7°; Fig.7).
Figure 6.
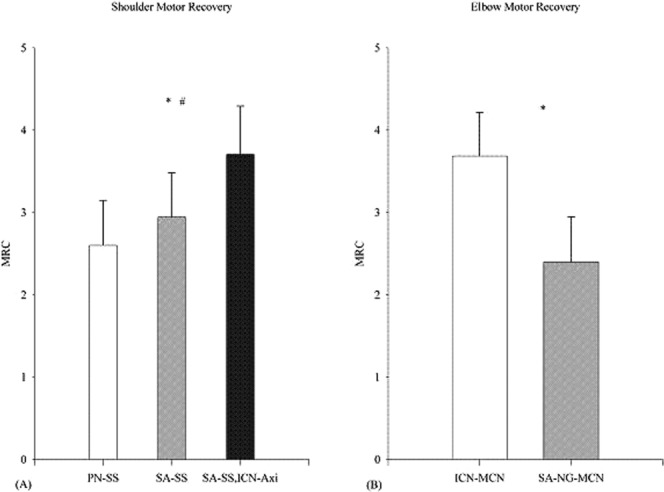
A: Comparison of shoulder motor recovery in single nerve (PN-SS or SA-SS) and double nerve (SA-SS+ ICN-AXI) procedures. B: Comparison of elbow motor recovery in ICN-MCN and SA-NG-MCN.
Figure 7.
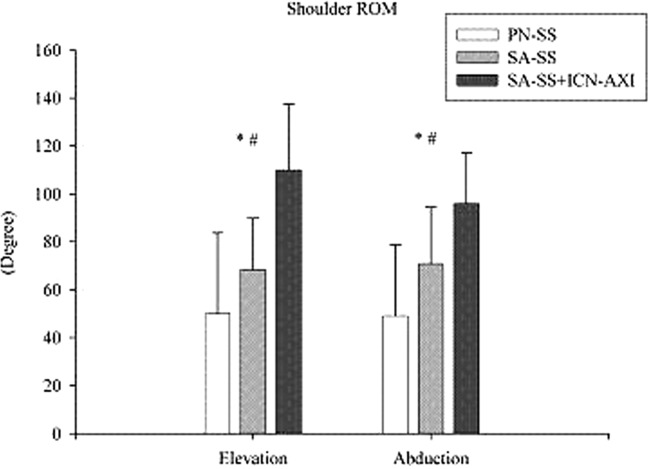
Comparisons of shoulder range of motion in single nerve (PN-SS or SA-SS) and double nerve (SA-SS+ ICN-AXI) procedures. *: PN-SS vs. SA-SS + ICN-AXI, P < 0.05. #: SA-SS vs. SA-SS + ICN-AXI, P < 0.05.
Elbow Flexion Function
Eighteen patients (90%) in groups 1 and 18 patients (90%) in group 2 obtained at least M3 motor recovery of elbow flexion function. There was no difference in elbow motor function recovery between the groups (Table5). However, only 40% of those receiving SA-NG-MCN neurotization had a recovery ≥ M3, compared with 97.1% in those receiving ICN-MCN neurotization. SA-NG-MCN had a significantly worse motor recovery than ICN-MCN (P < 0.01; Fig.6).
Hand Function
Six patients (30%) in group 1 and 13 patients (65%) in group 2 obtained at least M3 motor recovery of hand grip function (Figs.8 and 9). The most significant finding when comparing both groups was in hand motor recovery, and group 2 had a significantly better hand motor recovery than group 1 (P = 0.02; Table5). However, all of the patients who had clinically useful hand function recovery (≥ M3) only had a hook-grip function of the digits. None of the patients achieved intrinsic hand functions. Since no surgical reconstructive procedure was performed for wrist and hand extension function during the neurotization surgery, all patients who obtained ≥ M3 hand function (6 in group 1 and 13 in group 2) needed a secondary dorsal wrist extensor tenodesis procedure to prevent finger and wrist contracture. All these 19 patients who obtained ≥M3 hand grip function were observed to have dependent motor function (initiation of lesion site hand grip by adduction and internal rotation of the contralateral shoulder, extension of elbow, and rotation of forearm) until 4 years after CC7 transfer surgeries. Four (all in group 2) of these 19 patients subsequently developed clinical independence of lesion site hand function in an average 5 years (4.5–6 years) after CC7 transfer procedures. However, we also noticed that these so-called independent motions were merely based on our clinical observations that these four patients could perform hand grip without obvious contralateral upper limb motion. In fact, these four patients received continuous rehabilitation programs of motor relearning, and then developed their individual maneuvers for igniting contralateral hand grip function. These individual maneuvers included subtle contralateral shoulder muscle and pectoral muscle contraction, and unnoticed elbow and forearm muscle contraction. Sensory recovery of the hand (S2 and S3; 85% in group 1 and 90% in group 2) was similar in both groups (Table5).
Figure 8.

Patients in group 1 received hemi-CC7 transfer for right total root avulsion BPI. The right hand shows M3 motor recovery with hook grip function. [Color figure can be viewed in the online issue, which is available at wileyonlinelibrary.com.]
Figure 9.

Patients in group 2 received total-CC7 transfer for right total root avulsion BPI. The right hand shows M4 motor recovery with hook grip function. [Color figure can be viewed in the online issue, which is available at wileyonlinelibrary.com.]
Donor Site Complications
Of the 40 patients, 36 (90%; 16 in group 1, 80%; and 20 in group 2, 100%) experienced paresthesia in the MN of the donor hand immediately after surgery. In group 1, 13 of these 16 patients had temporary donor site problems and recovered spontaneously with an average of 3.5 months (range 3 weeks to 6 months) after surgery. However, the remaining 3 patients in group 1 (3/20, 15%) developed numbness on the index pulp and paresthesia of the MN area of the palm that lasted for more than 6 months. Motor weakness of the triceps and extensor digitorum communis (EDC) of the donor limb was noted in 2 patients in group 1 (Table3). Continuous physical therapy was conducted to recover the donor site motor weakness, and the recovery of motor function was satisfactory 1 year after rehabilitation. In group 2, 11 of the 20 patients had temporary donor site paresthesia and numbness and recovered spontaneously with an average of 4.2 months (range 2–6 months) after surgery. However, 9 patients in group 2 (45%) developed donor site complications including paresthesia of the donor limb for more than 6 months (Table4). Six of these 9 patients (6/20, 30%) in group 2 developed motor weakness of the donor limb, including triceps weakness in 2 patients, combined triceps and EDC weakness in 3 patients, and very unusually, 1 patient suffered from weakness (M3) of the flexor digitorum profundus and intrinsic muscle function. This patient needed a subsequent tendon transfer procedure on the donor limb for functional recovery. Comparisons of donor site morbidity showed that group 1 had fewer donor site complications (15%) than group 2 (45%; P = 0.03; Table5).
DISCUSSION
Total root avulsion type BPI has the worst prognosis and makes the reconstruction of the plexus more challenging. Unlike the favorable results in upper arm type BPI (C5 and C6 injury, or C5-6-7 injury) in which reconstruction can achieve a higher than 80% success rate in shoulder and elbow function recovery,10,11,16,28 the reported results for total arm type BPI are much worse.2,3,5,12,13,15 The current concepts for the treatment of total root avulsion BPI are focused on neurotization and free functioning muscle transfer.1–5,8,9,11–13,16–21,28–32 Neurotization for BPI has gained in popularity the since 1960s. Many studies have reported extraplexal neurotization methods to reconstruct functional deficits after BPI, especially for shoulder and elbow function. The SAN has been reported to successfully reconstruct shoulder function by direct neurotization on the SSN.16 ICNs have been reported to be successfully transferred to MCN for biceps function.2,5,6,10,18 Narakas preferred to use the SAN to neurotize the SSN, and ICN for MCN.10 However, intraplexal neurotization almost never achieves useful hand function,2,5,9 and these aforementioned extraplexal neurotization methods are seldom effective for reconstructing hand function for three reasons. First, the neurotization site is far away from the target muscle over the forearm, which causes poor reinnervation of the neuromuscular junction. Second, the axon donor nerves have insufficient numbers of myelinated fibers (1,300 in each ICN and 1,700 in the SAN) to match the recipient nerves (such as MN or ulnar nerve over the lesion site). Third, the proximal part of the peripheral nerve (such as the MN) at trunk or cord level is a mixture of motor and sensory nerve fibers, and the regenerating axons are thus frequently misdirected compromising the results.7,8 Therefore, neurotization methods such as transfer of the ICN to the MN to restore hand function yield poor results.2,6,10,16
To overcome the deficits of the limited resources of available donor nerves and insufficient myelinated axon fibers of the donor nerves, Gu first proposed the technique of contralateral C7 (CC7) transfer to achieve useful hand grip.1,20,21 The potential advantages of CC7 are because the C7 nerve contains over 25,000 myelinated fibers, and C7 also contains motor and sensory nerves, which are suitable for reconstruction of complex motor and sensory functions, such as in the MN. The surgical procedures include two stages. The first stage involves coaptation of the CC7 nerve root with a pedicled ulnar nerve graft taken from the side of the paralyzed upper limb. Eight to 12 months later, the distal part of the reinnervated ulnar nerve graft is sutured to the avulsed plexus, giving precedence to the MN, MCN, Axi, and then the other nerves.1–3,11–13,15,18–23 Chuang preferred to transfer the ulnar nerve with the ulnar artery, a procedure called “supercharge CC7”, and thus directly neurotize the plexus.18,19,29 Some surgeons use one stage surgery (CC7 to VUNG and UN to MN at the same time) instead of two stages.3,11–13,15,18,19 With the substantial advantages of CC7 transfer, Gu and Chuang have reported satisfactory results in total root avulsion BPI reconstruction1,18–23; however, other studies have reported that this CC7 method yields inferior results than Gu's series.2,3,13,15,26 Debate on the clinical applications of CC7 for the reconstruction of total root avulsion BPI is ongoing, especially with regards to donor site morbidity and the effectiveness of motor recovery.
Concerning donor site complications, a sound knowledge of the C7 anatomy and nerve supply is mandatory. Transection of the posterior division of CC7 produces a weakness of the radial nerve innervated muscles, especially the triceps and the wrist and finger extensors, although without paralysis. These muscles regain their original strength by internal sprouting.1,12,15,22,23,27 Sensory loss following sectioning of the posterior division of CC7 has been reported to cause a temporary loss of MN sensation of the palm.11,12,18,19 The AD of C7 innervates the pectoralis muscle and other muscles to a much lesser degree without visible loss of function. There is always some sensory loss in the thumb and index finger when the AD of C7 is transected.2,3,11,13,15,27,29 In some patients, this sensory loss is significant and not well tolerated. Chuang also noted that sectioning of the C7 root can create a temporary weakness of the triceps of the donor's upper limb and paresthesia over the dorsum of the hand supplied by the radial nerve.18,19 Although some surgeons have reported a very small number of donor site complications after CC7 section,1,3,12,15,19,20 Sammer and Shin reported that these donor site complications were unacceptable for some of the patients receiving CC7 surgery.13 In this study, we found a significantly lower incidence of donor site complications in group 1 than in group 2. This may imply that harvesting total CC7 incurs the risk of a high complication rate (45%) including paresthesia of the MN and radial nerve sensation in the hand, motor weakness (30%) of the triceps and EDC, and even weakness of the flexor digitorum profundus and intrinsic muscle. This unusual complication of flexor digitorum profundus and intrinsic motor weakness at the donor's upper limb in our total CC7 harvesting group was very similar to a report from the Mayo Clinic, although they only harvested hemi-CC7.13
With regards to the effectiveness of hand motor recovery using the CC7 method, debate has focused mostly on the choice of harvesting hemi-CC7 or total-CC7.1,11,12,14,30 Gu et al. and Chuang et al. harvested total CC7 as the neurotizer that was sutured onto the VUNG.1,17–23 Their results of motor recovery in hand function after total CC7 transfer were more than 50% (≥M3) satisfactory. However, to reduce the potential donor nerve complications, an increasing number of surgeons are choosing to use hemi-CC7 instead of total CC7.3,11–13,15,26,33 Waikakul et al. used hemi-CC7 and VUNG transfer to the MN for total arm type BPI in 96 patients, and obtained only 21% effective finger flexion (≥M3). Another series by Songcharoen et al. revealed that only 29% of the patients achieved M3 or M4 finger flexion by hemi-CC7 transfer.3 Sammer and Shin reported their hemi-CC7 results with very disappointing hand function recovery, and none of their 15 patients obtained ≥ M3 hand grip.13 Hierner and Berger reported the results of 10 hemi-CC7 transfers, four of which were to the MN. A functional “primitive” grip was achieved in only one patient (25%) 18 months postoperatively.33 Terzis et al. reported the results of a series of 56 hemi-CC7 transfers for traumatic BPI, 29 of which involved transfer to the MN for hand function. Ten (34%) of these 29 patients demonstrated useful hand motor recovery (≥ M3).12,26 In this study, only 30% (6/20) of hemi-CC7 transfers achieved ≥ M3 hand grip function, while total CC7 seemed to achieve more promising results (65% ≥ M3 hand grip). The reasons for CC7 transfer failure are reportedly due to two factors. First, atrophy of the target muscles innervated by the MN over the forearm occurs before the reinnervation process reaches the neuromuscular junction. Second, there is long distance between the CC7 donor nerve coaptation site and the docking site of VUNG sutured with the MN, for which the reinnervation process takes a very long time.2,3,7,11–13,15,26,30,33 Based on this study, we suggest another possibility (a third factor) for unsatisfactory CC7 outcomes, in that they may be due to differences in the number of myelinated fibers of donor CC7. This theory is supported by the significantly better outcomes when using total-CC7 than hemi-CC7 in our series. Some authors have proposed various methods to shorten the distance between the nerve cooptation site and the target muscle by pre-vertebral route CC7 transfer, or by humeral shaft bony shortening procedures.34,35 They reported improved outcomes of CC7 transfer due to effectively shortening the distance of VUNG and hence reducing the reinnervation time. However, we did not apply these techniques in our series.
Shoulder function plays an important role in the clinical results of BPI reconstruction. Surgeons have tried to reconstruct shoulder function by various methods of neurotization procedures.2,11–13,16,17,28,30,33,36 The major concern is the function of rotator cuff, which is innervated by the SSN, and the secondary concern is the function of the deltoid muscle which is innervated by the Axi.17,28,36 Possible neurotizers for shoulder function reconstruction include the SAN, ICN, PN, proximal C5-C6 stump, CC7, and triceps branch of the radial nerve. Sammer and Shin reported using CC7 as a neurotizer for shoulder function, and obtained only 23% (3/13) acceptable shoulder abduction (≥M3).13 Chuang et al. reported using eight different combinations of neurotization methods for shoulder reconstruction in BPI patients.17 They concluded that simultaneous neurotization on the SSN and Axi obtained better results than just neurotization on the SSN. In this study, our conclusions were similar to Chuang et al.'s that patients who received double nerve neurotization (SA-SS combined with ICN-Axi) had a significantly better shoulder MRC score than single neurotization with SA-SS (P < 0.01) or with PN-SS (P < 0.01). As for elbow flexion function, we found no difference in elbow motor function recovery between the groups. However, a comparison of the surgical procedures showed that SA-NG-MCN achieved a significantly inferior motor recovery than ICN-MCN (P < 0.01), with only 40% ≥ M3 elbow flexion in SA-NG-MCN neurotization compared with 97.1% ≥ M3 in ICN-MCN neurotization. Songcharoen et al. reported satisfactory results of SA-NG-MCN neurotization for 216 BPI patients, with 73% of ≥ M3 elbow flexion.14 Waikakul also reported satisfactory results in using SA-NG-MCN with elbow flexion ≥ M3 in 88% of their 96 patients.15 However, in a meta-analysis study of the English literature with 1,088 nerve transfers in 27 studies, Merrell et al concluded that direct ICN transfer to the MCN had a significantly better ability to achieve ≥ M4 elbow strength than SA-NG-MCN (41 vs. 29%),28 which is compatible with our results. The other issues concerning the recovery of total root avulsion BPI patients after surgical reconstruction are pain and neuralgia. We employed various combined methods to solve the neuropathic pain in BPI patients including oral nonsteroid anti-inflammatory drugs, narcotic medications, local steroid injections, and even surgery at the dorsal root entry zone.37 However, we did not investigate pain relief as this was not the aim of this study.
To the best of our knowledge, there are no prospective randomized studies comparing the clinical outcomes of hemi-CC7 versus total-CC7 in the English literature. Some surgeons have performed total-CC7 transfer for the reconstruction of total root avulsion BPI based on Gu's original method.1,20,22,23 However, some surgeons prefer to perform hemi-CC7 transfer due to patient safety and reducing donor limb complications. Therefore, most of the reported series are either based on the surgeons' preference of surgical methods, or on retrospective studies of CC7 methods.1,3,12,13,15,19,20,26,27,29,33–35 This study is the first prospective randomized study to analyze comparisons between both methods (hemi-CC7 vs. total-CC7) for hand reconstruction. We carefully selected the patients for this study, including those aged under 40 years, surgical delay within 6 months, and those capable of continuous rehabilitation for at least 2 years. With these well controlled conditions, this study was able to eliminate influencing factors such as age, surgical delay, and poor compliance with physical therapy found in the previous studies.3,7,11,12,15,26,28,29,33,35 Our results demonstrated that the efficacy of total-CC7 transfer for reconstructing hand grip function was significantly better than hemi-CC7 transfer. However, total-CC7 transfer incurs a high risk of donor site complications, which should be explained to the patients and families prior to surgery. Taking into consideration the availability of SAN, PN, and ICN, the surgical procedures for reconstructing shoulder and elbow functions in this study could not be randomized. However, we also found that double nerve neurotization (SA-SS combined with ICN-Axi) achieved a significantly better shoulder function recovery than single neurotization with SA-SS or PN-SS. With regards to elbow flexion motor recovery, direct neurotization by ICN-MCN was significantly better than indirect neurotization by SA-NG-MCN.
CONCLUSIONS
Using total-CC7 transfer for the reconstruction of hand function in total root avulsion BPI achieved significantly better motor recovery but a higher rate of donor complications than hemi-CC7. The possible occurrence of paresthesia and motor weakness of the donor limbs after section of CC7 should be carefully explained to the patients and families preoperatively. We also recommend neurotization on both the SSN and Axi to improve the shoulder function recovery in BPI patients.
REFERENCES
- 1.Gu YD, Zhang GM, Chen DS, Yan JG, Cheng XM, Chen L. Seventh cervical nerve root transfer from the contralateral healthy side for treatment of brachial plexus root avulsion. J Hand Surg Br. 1992;17:518–521. doi: 10.1016/s0266-7681(05)80235-9. [DOI] [PubMed] [Google Scholar]
- 2.Tu YK, Chung KC. Surgical procedures for recovery of hand function. In: Chung KC, Yang LJS, McGillicuddy JE, editors. Practical management of pediatric and adult brachial plexus palsies. Saunders Elsevier, New York; 2012. pp. 271–300. [Google Scholar]
- 3.Songcharoen P, Wongtrakul S, Mahaisavariya B, Spinner RJ. Hemi-contralateral C7 transfer to median nerve in the treatment of root avulsion brachial plexus injury. J Hand Surg Am. 2001;26:1058–1064. doi: 10.1053/jhsu.2001.27764. [DOI] [PubMed] [Google Scholar]
- 4.Thomeer RT, Malessy MJ. Surgical repair of brachial plexus injury. Clin Neurol Neurosurg. 1993;95(Suppl):S65–S72. doi: 10.1016/0303-8467(93)90038-i. [DOI] [PubMed] [Google Scholar]
- 5.Bonnard C, Anastakis DI. Complete palsy. In: Alain Gilbert., editor. Brachial plexus injuries. London: Martin Dunitz; 2001. pp. 67–75. [Google Scholar]
- 6.Narakas AO. Brachial plexus surgery. Orthop Clin North Am. 1981;12:303–323. [PubMed] [Google Scholar]
- 7.Bentolila V, Nizard R, Bizot P, Sedel L. Complete traumatic brachial plexus palsy. Treatment and outcome after repair. J Bone Joint Surg Am. 1999;81:20–28. doi: 10.2106/00004623-199901000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Doi K, Muramatsu K, Hattori Y. Restoration of prehension with the double free muscle technique following complete avulsion of the brachial plexus. J Bone Joint Surg Am. 2000;82:652–666. [PubMed] [Google Scholar]
- 9.Doi K, Sakai K, Kuwata N, Ihara K, Kawai S. Double free-muscle transfer to restore prehension following complete brachial plexus avulsion. J Hand Surg Am. 1995;20:408–414. doi: 10.1016/S0363-5023(05)80097-8. [DOI] [PubMed] [Google Scholar]
- 10.Narakas AO, Hentz VR. Neurotization in brachial plexus injuries: Indications and results. Clin Orthop. 1988;237:43–75. [PubMed] [Google Scholar]
- 11.Terzis JK, Kostopoulos VK. The surgical treatment of brachial plexus injuries in adults. Plast Reconstr Surg. 2007;119:73e–92e. doi: 10.1097/01.prs.0000254859.51903.97. [DOI] [PubMed] [Google Scholar]
- 12.Terzis JK, Kokkalis ZT, Kostopoulos E. Contralateral C7 transfer in adult plexopathies. Hand Clin. 2008;4:389–400. doi: 10.1016/j.hcl.2008.04.003. [DOI] [PubMed] [Google Scholar]
- 13.Sammer DM, Kircher MF, Bishop AT, Spinner RJ, Shin AY. Hemi-contralateral C7 transfer in traumatic brachial plexus injuries: Outcome and complications. J Bone Joint Surg Am. 2012;94:131–137. doi: 10.2106/JBJS.J.01075. [DOI] [PubMed] [Google Scholar]
- 14.Songcharoen P, Mahaisavariya B, Chotigavanich C. Spinal accessory neurotization for restoration of elbow flexion in avulsion injuries of brachial plexus. J Hand Surg Am. 1996;21:387–390. doi: 10.1016/S0363-5023(96)80349-2. [DOI] [PubMed] [Google Scholar]
- 15.Waikakul S, Orapin S, Vanadurongwan V. Clinical results of contralateral C7 root neurotization to the median nerve in brachial plexus injuries with total root avulsions. J Hand Surg Br. 1999;24:556–560. doi: 10.1054/jhsb.1999.0264. [DOI] [PubMed] [Google Scholar]
- 16.Millesi H. Brachial plexus injuries. Nerve grafting. Clin Orthop. 1988;237:36–42. [PubMed] [Google Scholar]
- 17.Chuang DCC, Lee GW, Hashem F, Wei FC. Restoration of shoulder abduction by nerve transfer in avulsed brachial plexus injury: Evaluation of 99 patients with various nerve transfers. Plast Reconstr Surg. 1995;96:122–128. doi: 10.1097/00006534-199507000-00019. [DOI] [PubMed] [Google Scholar]
- 18.Chuang DC. Neurotization procedures for brachial plexus injuries. Hand Clin. 1995;4:633–645. [PubMed] [Google Scholar]
- 19.Chuang DC, Cheng SL, Wei FC, Wu CL, Ho YS. Clinical evaluation of C7 spinal nerve transaction: 21 patients with at least 2 years follow-up. Br J Plast Surg. 1998;51:285–290. doi: 10.1054/bjps.1997.0193. [DOI] [PubMed] [Google Scholar]
- 20.Gu YD, Chen DS, Zhang GM, Cheng XM, Xu JG, Zhang LY, Cai PQ, Chen L. Long-term functional results of contralateral C7 transfer. J Reconstr Microsurg. 1998;14:57–59. doi: 10.1055/s-2007-1006902. [DOI] [PubMed] [Google Scholar]
- 21.Chen L, Gu YD. An experimental study of contralateral C7 root transfer with vascularized nerve grafting to treat brachial plexus root avulsion. J Hand Surg Br. 1994;19:60–66. doi: 10.1016/0266-7681(94)90051-5. [DOI] [PubMed] [Google Scholar]
- 22.Gu YD. Distribution of the sensory endings of the C7 nerve root and its clinic significance. J Hand Surg Br. 1994;19:67–68. doi: 10.1016/0266-7681(94)90052-3. [DOI] [PubMed] [Google Scholar]
- 23.Gu YD, Shen LY. Electrophysiological changes after severance of the C7 root. J Hand Surg Br. 1994;19:69–71. doi: 10.1016/0266-7681(94)90053-1. [DOI] [PubMed] [Google Scholar]
- 24.Beller EM, Gebski V, Keech AC. Randomization in clinical trials. Med J Aust. 2002;177:565–567. doi: 10.5694/j.1326-5377.2002.tb04955.x. [DOI] [PubMed] [Google Scholar]
- 25.Leung F, Tu YK, Chew WYC, Chow SP. Comparison of external and percutaneous pin fixation with plate fixation for intra-articular distal radial fractures - A randomized study. J Bone Joint Surg Am. 2008;90:16–22. doi: 10.2106/JBJS.F.01581. [DOI] [PubMed] [Google Scholar]
- 26.Terzis JK, Kokkalis ZT. Selective contralateral C7 transfer in posttraumatic brachial plexus injuries: A report of 56 cases. Plast Reconstr Surg. 2009;123:927–938. doi: 10.1097/PRS.0b013e31819ba48a. [DOI] [PubMed] [Google Scholar]
- 27.Liu J, Pho RW, Kour AK, Zhang AH, Ong BK. Neurological deficit and recovery in the donor limb following cross-C7 transfer in brachial-plexus injury. J Reconstr Microsurg. 1997;13:237–243. doi: 10.1055/s-2007-1000230. [DOI] [PubMed] [Google Scholar]
- 28.Merrell GA, Barrie KA, Katz DL, Wolfe SW. Results of nerve transfer techniques for restoration of shoulder and elbow function in the cortex of a meta-analysis of the English literature. J Hand Surg Am. 2001;26:303–314. doi: 10.1053/jhsu.2001.21518. [DOI] [PubMed] [Google Scholar]
- 29.Chuang DC. Contralateral C7 transfer for avulsion injury of the brachial plexus. Tech Hand Up Extrem Surg. 1999;3:185–192. doi: 10.1097/00130911-199909000-00007. [DOI] [PubMed] [Google Scholar]
- 30.Millesi H. Update on the treatment of adult brachial plexus injuries. In: Alain Gilbert., editor. Brachial plexus injuries. London: Martin Dunitz; 2001. pp. 77–90. [Google Scholar]
- 31.Tu YK, Chang CH, Tsai YJ, Hsiao CK, Sanapanich K. Triple free functioning muscle transfer for the reconstruction of total arm type BPI. In: Chung MS, Baek GH, Gong HS, editors. Hand Surgery, 2010 IFSSH. Koonja Publishing; 2010. pp. 230–231. [Google Scholar]
- 32.Sananpanich K, Tu YK, Pookhang S, Chalidapong P. Anatomical variance in common vascular pedicle of the gracilis and adductor longus muscles: Feasibility of double functioning free muscle transplantation with single pedicle anastomosis. J Reconstr Microsurg. 2008;24:231–238. doi: 10.1055/s-2008-1076096. [DOI] [PubMed] [Google Scholar]
- 33.Hierner R, Berger AK. Did the partial contralateral C7 transfer fulfill our expectations? Results after 5 years experience. Acta Neurochir Suppl. 2007;100:33–35. doi: 10.1007/978-3-211-72958-8_7. [DOI] [PubMed] [Google Scholar]
- 34.Yu ZJ, Sui S, YU S, Huang Y, Sheng JG. Contralateral normal C7 nerve transfer after upper arm shortening for the treatment of total root avulsion of the brachial plexus: A preliminary report. Plast Reconstr Surg. 2003;111:1465–1469. doi: 10.1097/01.PRS.0000049634.97185.2D. [DOI] [PubMed] [Google Scholar]
- 35.Wang SF, Yiu HW, Li PC, Li YC, Wang HH, Pan YW. Contralateral C7 nerve root transfer to neurotize the upper trunk via a modified prespinal route in repair of brachial plexus avulsion injury. Microsurg. doi: 10.1002/micr.20963. DOI 10.1002/micr.20963:183-188. [DOI] [PubMed] [Google Scholar]
- 36.Leechavengvongs S, Witoonchart K, Uerpairojkit C, Thuwasethkul P. Nerve transfer to deltoid muscle using the nerve to the long head of the triceps. Part II: A report of 7 cases. J Hand Surg Am. 2003;28:633–638. doi: 10.1016/s0363-5023(03)00199-0. [DOI] [PubMed] [Google Scholar]
- 37.Chen HJ, Tu YK. Long term follow up results of dorsal root entry zone lesions for intractable pain after brachial plexus avulsion injuries. Acta Neurochir. 2006;99:73–75. doi: 10.1007/978-3-211-35205-2_14. [DOI] [PubMed] [Google Scholar]


