Abstract
This Review describes the rationale for the use of cervical pessaries to prevent spontaneous preterm birth and their gradual introduction into clinical practice, discusses technical aspects of the more commonly used designs and provides guidance for their use and future evaluation. Possible advantages of cervical pessaries include the easy, ‘one-off’ application, good side-effect profile, good patient tolerance and relatively low cost compared with current alternatives. Use of transvaginal sonography to assess cervical length in the second trimester allows much better selection of patients who may benefit from the use of a cervical pessary, but future clinical trials are needed to establish clearly the role of pessaries as a preterm birth prevention strategy worldwide.
Keywords: cervical pessary, polyclinic setting, spontaneous preterm birth, transvaginal sonography in obstetrics
INTRODUCTION
Spontaneous preterm birth (SPTB) is a syndrome with many causes1,2. Twenty years ago, Romero et al.3 proposed stratification of the pathophysiology of SPTB into uterine factors, decidual membrane activation and precocious cervical ripening. However, despite much research into the etiology of the condition, the rate of SPTB has increased annually and it is regarded as a global healthcare burden4–6.
For centuries, vaginal pessaries have been used to treat uterine or vaginal vault prolapse. Although most gynecologists have received no training in pessary fitting and management, 86% of them nonetheless prescribe pessaries for this indication in the USA7 and their use is still emphasized in papers on the management of such conditions8. Different pessary designs originally used for the treatment of genital prolapse have also been used sporadically for prevention of SPTB, but this has not been promoted actively by academic leaders of opinion or evaluated formally in a research setting until very recently.
DEVELOPMENT OF CONCEPTS OF PESSARY TREATMENT FOR PREVENTION OF SPTB
Why design a pessary to prevent SPTB?
Early reports on the use of pessaries for the prevention of SPTB used models originally designed to treat genital prolapse (Figure 1a). In 1959, Cross described his experience using a ring pessary in 13 patients with either a history of cervical lacerations, cervical incompetence or uterus didelphus9, as cited by Dharan and Ludmir10. Vitsky described the use of a Hodge pessary in seven patients and in a further 14 of his colleagues' patients, postulating that the reduction of pressure on the internal os prevented the protrusion of membranes11,12. He also suggested that a pessary might change the inclination of the cervical canal and compress the cervix, but this was never tested and, considering the large openings of the Hodge and ring pessaries, this does not seem likely. Oster and Javert also used a Hodge pessary in 29 patients with ‘cervical incompetence’ defined by different criteria13, arguing that treatment with a pessary would be superior to surgical cerclage due to the reduced risk of bleeding or maternal sepsis13. Even a donut pessary has been used with the intention of preventing SPTB (R. Romero, pers. comm.). However, it is likely that the donut pessary can be used effectively to treat only genital prolapse, and not cervical incompetence, since the inner opening is too small to enclose or to incline the cervix (Figure 1a).
Figure 1.

Different models of pessaries used to prevent spontaneous preterm birth. (a) Ring pessary (top left), Hodge pessary (top right) and donut pessary (bottom left), all originally designed to prevent genital prolapse or uterine retroflexion, and butterfly-shaped pessary to support the cervix according to Jorde and Hamann (bottom right). (b) Arabin cervical pessary, designed to enclose, incline and possibly rotate the cervix as high as possible.
Pessaries designed specifically for pregnant women emanated mainly from East European countries. Jiratko et al. described a ‘Mayer ring pessary’ made of organic glass14. In 1978, Jorde and Hamann in East Germany developed a pessary that was supposed to surround the remaining cervix within a butterfly-shaped design, with a larger diameter towards the sacrum and a smaller diameter towards the symphysis (Figure 1a)15. It was made originally of plastic and eventually of silicone and was compared in two randomized controlled trials (RCT) with either surgical cerclage or no intervention16,17. However, since the authors used unclear selection criteria or inadequate methodology for randomization, these studies were not considered eligible for inclusion in the Cochrane review entitled ‘Cervical pessary for preventing preterm birth’18. In addition, up until the present day, patients who receive this pessary complain about stiffness and pain during insertion and during therapy (N. Sakvarelidze, pers. comm.), while others refuse this model, being aware of the alternatives (J. Jani, pers. comm.).
In the late 1970s, Hans Arabin in West Germany designed a round cone-shaped pessary made of flexible silicone. Its dome-like design resembled the vaginal fornix, with the aim of surrounding the cervix as close as possible to the internal os (Figure 1b)19. The smaller, proximal, inner opening within the flattened surface should be directed towards the cervix, whereas the wider, distal ring stayed within the vagina. The Arabin pessary was designed with the intention not only to support and compress, but also to incline the cervix and possibly rotate it more towards the sacrum. Originally, the described effects were suggested by clinical examination and by transabdominal sonography (TAS) (Figure 2). Only later was transvaginal sonography performed to visualize the reduction or at least stabilization of cervical funneling after placement of a pessary in selected patients (Figure 3)19–21. The design of this pessary was first published in a book chapter by Kubli and Arabin with the following short comment: ‘Pessaries have the advantage that anesthesia can be avoided and that insertion or removal are easy, but there are up to now no controlled trials to prove their effectiveness.’22
Figure 2.
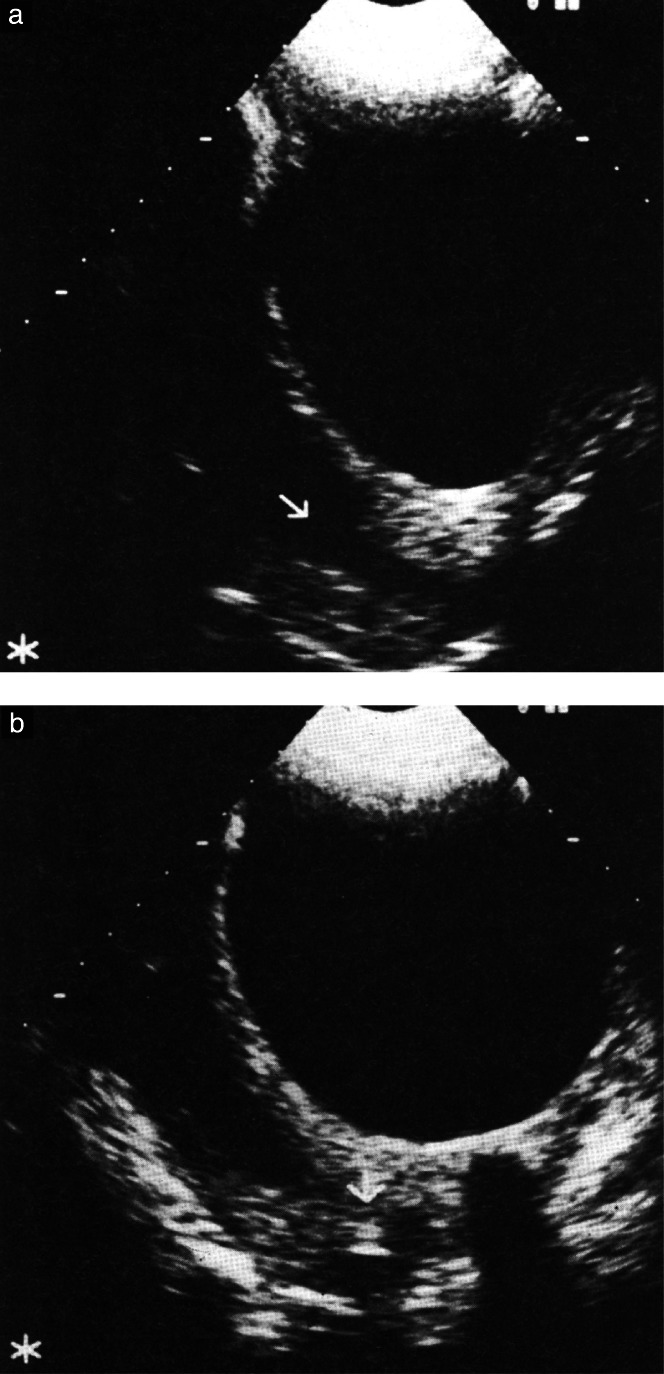
Historic transabdominal sonographic images from 1988, article by H. Arabin19 on pessary treatment, in a patient with full bladder, showing a cervix with funneling (arrow) before (a) and after (b) pessary placement. The pessary appears as a shadow around the cervical tissue and there is apparently reduction of funneling and closer attachment of the remaining cervix following placement. Images reproduced from Arabin19 with kind permission from Thieme (©1991 Georg Thieme Verlag KG 2013).
Figure 3.
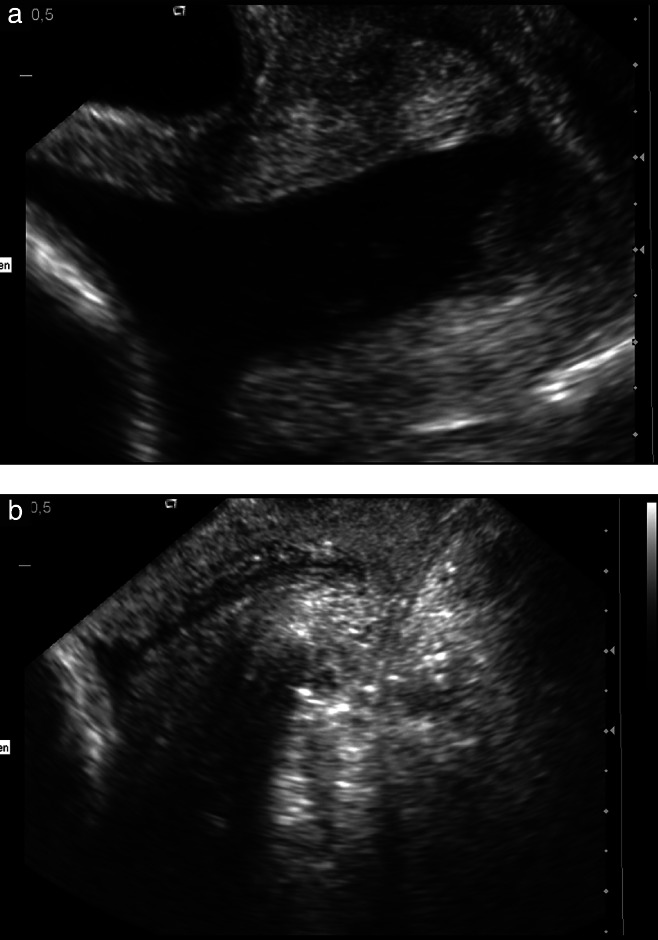
Transvaginal sonography of a cervix with U-shaped complete funneling and sludge in a nulliparous patient at 24 weeks' gestation before (a) and after (b) pessary placement (proximal inner diameter 35 mm, height 21 mm, distal outer diameter 65 mm), showing closer attachment, which suggests normal cervical gland area after placement of pessary. The patient delivered at 37 weeks after pessary removal.
In 1990, Quaas et al.23 reported an observational study of 107 patients, in whom a perforated Arabin pessary was used instead of surgical cerclage as a prophylactic or therapeutic treatment and even as emergency intervention. In 92% of the women, the pregnancy was maintained until 36 weeks of gestation and there were no complications. A full description of the pessary by H. Arabin, in a book chapter that reviewed various pessary treatments, was published in 1991, regrettably only after the death of the author19. Since at that time TVS had not yet been introduced into routine clinical practice, TAS in patients with a full bladder was used to visualize the pessary. It was suggested that the distal cervix seemed somehow more attached after pessary placement and that funneling was reduced (Figure 2). Subsequently, several relatively small case series have described the effect of the Arabin pessary23–27. Acharya et al. even demonstrated clinical images in emergency situations in patients with a dilated external os in whom the pessary caused closure of the cervix24. Two reviews10,28 and one Cochrane review18 summarized the early studies on the effect of cervical pessaries during pregnancy, which were conducted before RCTs had been finalized.
What are possible mechanisms in the prevention of SPTB?
There are several hypotheses regarding how the Arabin pessary might help to prevent SPTB and possibly preterm premature rupture of membranes (PPROM), as suggested in the first RCT of its use29. Clinical and ultrasound examinations have suggested that the pessary encompasses the cervix and changes the inclination of the cervical canal relative to the uterus20,21. This was demonstrated more systematically and objectively in an observational study using magnetic resonance imaging (MRI), which showed that placement of a pessary led to a more acute uterocervical angle and that this persisted as long as the pessary remained in situ30. This change might prevent direct pressure on the membranes at the level of internal cervical os and on the cervix itself. It is possible that the weight of the uterus is thereby directed more towards the lower anterior uterine segment.
In addition, the pessary might prevent further opening of the internal os, which is frequently associated with dissociation of amnion and chorion, particularly when the pregnant woman is upright31. It is recognized that the fetal membranes are susceptible to mechanical stress and interrelated lesions from infection and inflammation, with the degree of susceptibility depending partly on genetic disposition32,33. The impact of a purely mechanical device may therefore vary between different populations or individual patients with clinical manifestations of premature cervical ripening.
Another hypothesis is that the pessary protects the cervical mucus plug. This may be achieved through the pessary supporting the attachment of the remaining cervical tissue. Clinical findings and more recent proteomic studies have suggested that the cervical mucus plug plays an important role in the maintenance of pregnancy by protecting the intrauterine cavity from ascending infection and by its resolution inducing parturition34,35.
Clinical examinations have suggested that the longer the pessary stays in place during gestation, the greater chance there is that the cervix will appear to develop some degree of thickening or edema – at least in some patients. More objectively, this has now been confirmed using MRI30.
It has also been proposed that the pessary might diminish the Ferguson reflex (A. Baschat, pers. comm.), which is a positive feedback loop whereby pressure on the cervix or vaginal walls is communicated to the hypothalamus and pituitary glands, causing oxytocin release and thus further contractions36.
TECHNICAL CONSIDERATIONS
What pessary size should be used?
Different sizes of pessary are available to allow better adaptation to the patient's individual characteristics, and the exact choice of pessary is determined according to pragmatic criteria. Perforations within the silicone allow release of vaginal discharge, which may accumulate between the pessary and the upper fornix of the vagina. The proximal inner diameter of Arabin pessaries now in use varies between 32 and 35 mm and the outer distal diameter between 65 and 70 mm. There is also variation in the height of the pessary (17, 21, 25, 30 mm), allowing the choice of pessary to take into account the uterine size and, eventually, the degree of prolapse.
In general, a proximal inner diameter of 32 mm is sufficiently wide to surround the cervix without risking lacerations. A diameter of 32 mm is used if the pessary is applied in the first trimester (e.g. after radical cone biopsy) and in the second or third trimester in patients without significant cervical funneling. In patients with an edematous wide cervix and U- or wider V-shaped cervical funneling, a proximal inner diameter of 35 mm is proposed to avoid pressure on the membranes and to minimize prostaglandin release during placement (Figure 3).
In women of smaller build and in primigravidae, a distal outer diameter of 65 mm is sufficient for the pessary to stay within the vagina. A distal diameter of 70 mm is chosen in taller patients or parous women. Smaller heights of 17–21 mm are usually applied to minimize side effects when a pessary is indicated early in singleton pregnancies, while pessaries with a greater height of 25 mm are chosen in patients with uterine extension (multiple pregnancies, polyhydramnios), or even of 30 mm in patients with symptoms of uterine prolapse during pregnancy. It is likely that pessaries with a larger surface area are associated with more complaints of intermittent discharge, since more fluid might accumulate behind the pessary. Our suggestions regarding choice of pessary size according to the characteristics of the patient are summarized in Table1.
Table 1.
Proposed sizes of the Arabin pessary for different clinical situations
| Clinical situation & results from TVS | Proximal inner diameter | Distal outer diameter | Height | |||||
|---|---|---|---|---|---|---|---|---|
| 32 mm | 35 mm | 65 mm | 70 mm | 17 mm | 21 mm | 25 mm | 30 mm | |
| Short cervix 2nd trimester | ||||||||
| Singleton | ||||||||
| No or Y-shaped funneling | ||||||||
| Nulliparous | √ | √ | √ | |||||
| Parous | √ | √ | √ | |||||
| V- or U-shaped funneling | ||||||||
| Nulliparous | √ | √ | √ | |||||
| Parous | √ | √ | √ | |||||
| Twins | ||||||||
| No funneling | ||||||||
| Nulliparous | √ | √ | √ | |||||
| Parous | √ | √ | √ | |||||
| V- or U-shaped funneling | ||||||||
| Nulliparous | √ | √ | √ | |||||
| Parous | √ | √ | √ | |||||
| Short cervix (e.g. after cone biopsy) 1st trimester | ||||||||
| Singleton | ||||||||
| Nulliparous | √ | √ | √ | |||||
| Parous | √ | √ | √ | |||||
| Twins | ||||||||
| Nulliparous | √ | √ | √ | |||||
| Parous | √ | √ | √ | |||||
| Additional signs of ‘prolapse’ in any patient | ||||||||
| Nulliparous | √ | √ | √ | |||||
| Parous | √ | √ | √ | |||||
Definition of ‘short cervix’ is relative and centile values specific for gestational age and different populations are preferred for definition of cut-off values. TVS, transvaginal sonography.
How should the pessary be inserted?
The cervix should be examined by TVS and the results of cervical length measurement, evaluation of funneling and any specific tests used in different settings, such as assessment of fibronectin or interleukins, should be documented. For pragmatic reasons, it is advisable to take vaginal/cervical swabs before placement and to treat positive results according to local protocols for patients without a pessary29. There is usually no need to use anesthesia or analgesia or to wait for the results of the swabs before pessary placement.
The pessary is covered with antibacterial cream, gel or fluid to provide lubrication for easier fitting. The pessary is then squeezed between thumb and fingers and introduced longitudinally into the introitus. Within the vagina the pessary is unfolded, so that the smaller inner ring is directed upwards towards the cervix. The proximal part of the pessary's dome is carefully pushed towards the upper fornix until the cervix is completely surrounded, and the anterior part of the pessary is then pressed slightly towards the sacrum. It is advisable to ask the patient to stand up and walk a few steps after insertion, and to enquire about any sensations – the inserted pessary should no longer be ‘felt’ by the patient. Some patients even report some relief of pressure sensations. If a patient complains of any discomfort, either the size or position of the pessary should be reconsidered. Thereafter, the patient should be examined again, by either clinical or sonographic evaluation or both, to reconfirm that the complete cervix is protruding through the proximal inner ring. A speculum examination may be indicated in a few patients, for reassurance. In patients with complete cervical funneling, extensive digital examinations should be avoided if possible.
How and when should the pessary be changed or removed?
On a routine basis, the pessary is removed at around 37 weeks. Before removal it is advisable to ensure that the cervix is pushed back through the inner ring of the dome of the pessary. When there are signs of cervical edema, the woman should be informed that removal may be painful.
There are a few indications for removal and reinsertion of the pessary. If a woman complains of discomfort or minor bleeding, a speculum examination or even a cervical smear should be performed, to exclude erosions and lacerations. It might be advisable to remove and clean the pessary with running water and reinsert it if there are no suspicious findings.
The pessary should always be removed when there are signs of imminent delivery, and removal must not be forgotten in patients admitted in labor or undergoing Cesarean delivery. We have reported a case in which the pessary was not removed until an advanced stage of labor, resulting in the loss of a small ring of cervical tissue shortly after delivery20. Severe contractions should indicate removal of a pessary in order to avoid increasing pressure on the cervix, with the associated risk of lesions or venous congestion.
In the case of PPROM confirmed by biochemical testing and ultrasound, the pessary may only stay in place when chorioamnionitis can be ruled out confidently and uterine contractions are not present, particularly at an early gestational age. In the RCT conducted by Goya et al.29, the pessary was left in place in women with PPROM without signs of contractions or chorioamnionitis. The opening of the pessary allows fluid to pass; however, if there are any additional risk factors for infection, we advise removal.
CLINICAL CONSIDERATIONS
The following recommendations are based primarily on consensus and the expert opinion of those who have long-term experience with the Arabin pessary, as there is limited scientific evidence. Our intention was not to produce guidelines and, therefore, we have not formally graded our recommendations and the evidence that underpins them. Such work is yet to be done and will be facilitated as new evidence emerges, including more formally conducted systematic reviews37.
What are possible indications for pessary use?
The question as to whether universal TVS screening should be implemented for all singleton pregnancies remains hotly debated. Since several RCTs and a subsequent meta-analysis have demonstrated that vaginal progesterone can effectively reduce the rate of SPTB due to short cervical length38–40, this discussion has gathered significant momentum. Whereas in the eyes of many ‘to do nothing is not any longer an option’41, the American College of Obstetricians and Gynecologists and a Cochrane review acknowledge concerns regarding both quality assurance and the risk of unnecessary intervention in singleton pregnancies without a history of SPTB42,43. Some obstetricians claim the cost-effectiveness of a universal ‘screen and treat’ policy41, but for most healthcare systems a high-quality screening program using mid-trimester ultrasound to detect short cervical length may be prohibitively expensive42,43. The emphasis on quality assurance of any such program is critically important. In the context of nuchal translucency scanning, Nicolaides demanded that ‘care givers should be trained, and their results should be subjected to external quality assurance’44. The same, therefore, should apply for measurement of cervical length by TVS, and even more so for interventions such as pessary application.
Goya et al.29 reported the first multicenter RCT on pessary use in unselected women screened by TVS and showed that in women with a short cervical length (< 25 mm) between 18 and 22 weeks the pessary reduced the rate of poor outcome and prolonged pregnancy compared with controls. In their study, 385 women were randomized to receive a pessary (n = 192) or expectant management (n = 193). Women with a major fetal abnormality, painful regular uterine contractions, active vaginal bleeding, ruptured membranes, placenta previa or a history of cone biopsy or cervical cerclage in situ were not included. In the pessary group, there were fewer births before 34 weeks (6% vs 27%; relative risk (RR), 0.24; 95% CI, 0.13–0.43), before 37 weeks (22% vs 59%; RR, 0.36; 95% CI, 0.27–0.49) and before 28 weeks (2% vs 8%; RR, 0.25; CI, 0.09–0.73), with a significant difference in the occurrence of composite poor neonatal outcome.
In a smaller RCT, 108 Asian women with a singleton pregnancy and a cervical length < 25 mm at routine second-trimester TVS were randomized to a pessary (n = 53) and a control (n = 55) group. Women with a major fetal abnormality, surgical cerclage in the current or a previous pregnancy, presence of cervical dilatation, painful uterine contractions, PPROM or even a history of cervical incompetence were excluded. The investigators attempted to blind the patients to their assigned treatment group by simulating the insertion of a pessary in controls. The mean gestational age at delivery was 38.1 weeks in the pessary group compared with 37.8 weeks in the expectant management group, with no significant differences in the rates of delivey before 28, 34 or 37 weeks45.
Assuming that, for the foreseeable future, cervical TVS of low-risk women will remain largely sporadic and confined to research settings or high-resource countries, relatively few women will present with a short cervix as the only indication for cervical pessary (or progesterone or both). At present, there seems to be no alternative but to manage them in the same way in which we manage women in whom the indication for TVS and any following treatment is previous history or cervical surgery.
Singleton pregnancy with a history of SPTB and cervical shortening
It seems appropriate to perform TVS as early as possible in this group, since the same cut off-values used before 20 weeks have a higher likelihood ratio for SPTB than they do later in gestation46. The use of centiles or Z-scores instead of fixed cut-off values allows the individual course of precocious cervical ripening to be followed47. However, as yet, no RCT has compared the effect of the cervical pessary with that of cerclage or progestogens. Alfirevic et al.48 compared retrospectively three cohorts of women with previous SPTB < 34 weeks and short cervix treated with cerclage (n = 142), vaginal progesterone (n = 59) or a pessary (n = 42). There were no significant differences in rates of perinatal loss, neonatal morbidity or SPTB, apart from a higher rate of SPTB before 34 weeks' gestation in the vaginal progesterone vs pessary groups. It was concluded that randomized comparisons of these three management strategies, or combinations thereof, are needed to determine the optimal management of these women49. Possible advantages of a pessary may be that it can be inserted at a later gestational age, when cerclage is no longer performed, or after an unsuccessful cervical cerclage.
Twin pregnancy
In a pilot case–control study in which, for the first time, pessaries were applied on the basis of TVS findings, it was suggested that the pessary could significantly reduce SPTB in twin pregnancies with a short cervical length20. Twenty-three women with a short cervical length < 25 mm before 24 weeks and expectant management were matched with 23 women treated with pessary. The mean gestational age at delivery was 35 + 6 weeks in the pessary group and 33 + 2 weeks in the control group (P = 0.02). Another pilot study suggested a significant reduction of SPTB in monochorionic twin pregnancies with short cervical length (< 25 mm) in which a pessary was inserted following laser treatment for twin–twin transfusion syndrome, with a median gestational age at delivery 4 weeks later than that in comparable historic controls50. However, the sample size in both groups was very small (n = 8). Both pilot studies concluded that RCTs would be necessary to evaluate the effectiveness of pessaries in twin pregnancy. Such trials are particularly important given that there is as yet no firm evidence that either 17-hydroxyprogesterone caproate, vaginal progesterone or cerclage has a beneficial effect in prolonging twin gestation; in fact, they might even have an adverse impact51–54.
An RCT was recently completed in The Netherlands in which 403 women with multiple pregnancy who were treated with a pessary were compared with 410 women managed expectantly. In unselected women with a dichorionic twin pregnancy, prophylactic use of the pessary did not reduce poor perinatal outcome. However, in a subgroup analysis among women with a cervical length < 25th percentile before 20 weeks (38 mm), the incidence of poor neonatal outcomes was 12% (9/78) for the pessary group and 29% (16/55) for the no-pessary group (RR, 0.40; 95% CI, 0.19–0.83). This was accompanied by a significantly reduced rate of delivery before 32 weeks (14% vs 29%; RR, 0.49; 95% CI, 0.24–0.97) and of neonatal mortality (child level) before discharge (2% vs 15%; RR, 0.13; 95% CI, 0.03–0.60)55,56. This Dutch trial will be followed by an implementation study in The Netherlands, in which women with twin pregnancy and a cervical length < 38 mm before 20 weeks will receive a pessary and the outcome will be compared to that of a previous expectantly managed cohort (B.W. Mol et al., pers. comm.).
Patients with a previous large cone biopsy
This group of women tend to be referred early in pregnancy. A healthy cervix consists of around 30% smooth muscle tissue at the internal os, but only 6% at the external os57. Consequently, a radical cone biopsy removes the collagen-rich part of the cervix, compromising its integrity. There is a significant association between a large loop excision procedure and the risk of subsequent SPTB, although no significant association was found in one study when the comparison was adjusted for possible confounding factors using a cohort of women who underwent biopsy during colposcopy after having given birth58. It is, however, probable that the risk is higher after deep conization or repeated treatment in patients at high risk for invasive cancer59.
Until now, both prophylactic and emergency cerclage procedures have been found to fail to reduce the rate of SPTB in this group of patients60–62. For this reason a cervical pessary, possibly combined with vaginal progesterone, may be an option, as demonstrated in an observational pilot study63 in which 12 women with one or more previous surgical conizations and a cervical length of 6–36 mm were treated with a pessary, and additional progesterone if the cervical length was < 15 mm. The mean gestational age at delivery was 37 + 6 (range, 33–41) weeks and the mean interval from insertion to delivery was 181 (range, 84–219) days or 24 + 2 weeks.
What are the contraindications?
Contraindications include the presence of lethal fetal abnormality, suspicion of chorioamnionitis, ballooning of membranes outside the cervix into the vagina and painful, regular uterine contractions. In patients with uterus bicollis (i.e. two cervices) fitting of a pessary is problematic. In pregnant women with mild or moderate prolapse, the cervical pessary might release the feeling of discomfort and pressure pain; however, in women with severe prolapse during pregnancy, there is a small risk of uterine prolapse through the opening of the pessary. In the author's (B.A.) experience, this happened once in 20 years; there were no signs of incarceration and the cervical pessary was cut, removed and replaced with a pessary designed for genital vault prolapse.
MANAGEMENT OF PATIENTS WITH PESSARY IN SITU
What information should be provided to women?
It is important to inform women and their healthcare providers regarding up-to-date study results and the certification status of pessaries. The Arabin pessary is certified for the prevention of SPTB in countries of the European Union (Identification number: MED/CERT0482 EN ISO13485 Council directive 93/42/EEC concerning medical devices), Scandinavia, the Russian Federation, Indonesia and the Arabian Emirates. In other countries, physicians should obtain information from the Medical Boards to determine whether the Conformité Européenne (CE) certification is acknowledged or whether patients have to be informed about off-label use until the treatment is accepted by the local authorities.
Women and their care providers have to be informed about the possibility of vaginal discharge and it should be explained that this is due to collection of fluid behind the pessary, which is released incidentally. This should not be mistaken for either PPROM or cervical infection and is no reason to discontinue the use of a pessary. Intercourse is not generally contraindicated and reported rates were similar in the study and control groups of the RCT by Goya et al.29.
It is advisable to confirm appropriate placement by clinical and sonographic examination after insertion of a pessary. In case of displacement, which may depend on operator experience and skill in selection and placement of the pessary and may vary between different populations, it should be refitted, possibly with the help of a speculum examination, or another size should be chosen. The pessary should stay in place until around 37 weeks unless there are indications for removal (see above). The patient should be advised to see her physician in case of discomfort, painful contractions, bleeding or suspicion of PPROM. Once appropriate placement of the pessary is confirmed, regular vaginal assessments either by digital examination, speculum or ultrasound are not necessary unless the findings could influence further management.
Should a patient with a pessary be hospitalized?
Women in whom a pessary is indicated only due to cervical shortening, without contractions or other comorbidity, are usually not hospitalized, particularly if the social conditions at home allow restriction of physical activities in a supportive environment. In fact, treatment with a pessary can additionally reassure patients and encourage them to stay at home instead of being hospitalized. With early cervical shortening and/or additional risk factors such as sludge, severe funneling, membrane dissociation or even some degree of external dilatation, it is prudent to admit the patient initially and follow the course of clinical symptoms and the cervical appearance by TVS according to the technique described by Goya et al.21.
Can additional medication be applied?
There are no contraindications for the use of additional medication such as indomethacin, antibiotics or vaginal progesterone. The decision regarding whether to use any such treatment before, during or after pessary placement depends on the clinical situation and is based on anecdotal evidence and clinical observations, rather than on prospective studies.
In patients with a singleton pregnancy and a history of SPTB, prophylactic intramuscular treatment with 17-hydroxyprogesterone caproate has been associated with a significant reduction in the rate of SPTB. In the USA, it has been advised to perform a cerclage if these patients demonstrate subsequent cervical shortening64. It might be an option to use a cervical pessary instead, but good comparative data are lacking.
In patients with a singleton pregnancy and a short cervical length a cervical pessary may be the first choice. If follow-up TVS demonstrates further significant shortening, additional vaginal progesterone may be considered. The alternative approach is to start with vaginal progesterone and eventually also insert a pessary at follow-up examination, or even to indicate both simultaneously in patients with a cervical length < 15 or 20 mm.
In selected patients with extreme funneling and no inner cervical length, but sufficient external cervical tissue, indomethacin and possibly vaginal progesterone may be used for 24–48 hours before pessary insertion, and the patient placed in Trendelenburg position. This is intended to reduce amniotic fluid volume, pressure on the internal os and prostaglandin release before insertion of a pessary, and the interval allows the application of corticosteroids and exclusion of the possibility of early labor or rapidly progressing chorioamnionitis.
IMPLICATIONS FOR FURTHER RESEARCH
In high-resource settings, in which TVS of the cervix is readily available, the indication for a pessary should be based on cervical length. Nevertheless, a short mid-trimester cervical length does not tell the whole story65. New technologies such as ultrasound-derived elastography may help to evaluate tissue hydration, collagen structure and tissue elasticity and possibly become clinically useful to indicate and monitor specific interventions66,67. This could give us an opportunity to evaluate possible effects of the pessary on stabilization of the collagen tissue and the extracellular matrix. The extent to which the tilting or compression of the cervix has a preventive effect for SPTB and whether the cervical mucus is preserved in patients with a pessary remains to be established.
It might be more vision than reality to anticipate an individualized approach in the decisions regarding the best possible treatment for a ‘malfunctioning’ cervix. The new insights obtained by metabolic profiling and genetic studies of maternal and fetal candidate genes for SPTB and PPROM are exciting33,68. We are looking forward to the time when progressive changes in cervical length, the presence of sludge, concomitant clinical symptoms and findings of vaginal swabs, cervical fibronectin and placenta-derived biomarkers in maternal blood will play a role in deciding whether pessary, progesterone, cerclage or some other novel therapy is the most appropriate treatment strategy for an individual patient.
In developing countries, on the other hand, there is an urgent need for low-cost, low-tech preventative interventions that can be applied easily by various types of community health practitioner. At this stage, pessaries should only be administered within randomized or carefully planned and monitored population-based studies. If TVS is not available, other methods to measure cervical length could be considered69,70.
Ultimately, it is difficult to see how we can establish the definitive lack or presence of evidence supporting pessary use without properly conducted randomized studies that include long-term follow-up of children exposed to antenatal preventative strategies for SPTB. It is rewarding to see that our research community has embraced this methodology, including individual patient meta-analysis71. However, there is a long way go. We do not collect the same demographic data, do not use the same definitions for key clinical outcomes and remain reluctant to share study data for all sorts of reasons. Usually, there is no funding for long-term follow-up and, even when there is, the methodology used varies far too much between studies.
We all agree that the best answers to clinical problems will come from large international collaboration and, increasingly, our funders, both public and industry, are prepared to listen. Whether we can all speak with one voice, only time will tell.
Acknowledgments
We thank all those who have discussed with us their experience, particularly Dick Bekedam, Elena Carreras, Maria Goya, Jacques Jani, Jesús Rodriguez Calvo and Ariel Zimerman.
DISCLOSURE
The first author has a direct ownership interest in the company that designed, produces and now distributes the Arabin pessary. The company is held privately and the profit is used to support the Clara Angela Foundation. The second author has no conflicts of interest.
REFERENCES
- 1.Villar J, Papageorghiou AT, Knight HE, Gravett MG, Iams J, Waller SA, Kramer M, Culhane JF, Barros FC, Conde-Agudelo A, Bhutta ZA, Goldenberg RL. The preterm birth syndrome: a prototype phenotypic classification. Am J Obstet Gynecol. 2012;206:119–123. doi: 10.1016/j.ajog.2011.10.866. [DOI] [PubMed] [Google Scholar]
- 2.Goldenberg RL, Gravett MG, Iams J, Papageorghiou AT, Waller SA, Kramer M, Culhane J, Barros F, Conde-Agudelo A, Bhutta ZA, Knight HE, Villar J. The preterm birth syndrome: issues to consider in creating a classification system. Am J Obstet Gynecol. 2012;206:113–118. doi: 10.1016/j.ajog.2011.10.865. [DOI] [PubMed] [Google Scholar]
- 3.Romero R, Mazor M, Munoz H, Gomez R, Galasso M, Sherer DM. The preterm labor syndrome. Ann N Y Acad Sci. 1994;734:414–429. doi: 10.1111/j.1749-6632.1994.tb21771.x. [DOI] [PubMed] [Google Scholar]
- 4.Blencowe H, Cousens S, Oestergaard MZ, Chou D, Moller AB, Narwal R, Adler A, Vera Garcia C, Rohde S, Say L, Lawn JE. National, regional, and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: a systematic analysis and implications. Lancet. 2012;379:2162–2172. doi: 10.1016/S0140-6736(12)60820-4. [DOI] [PubMed] [Google Scholar]
- 5.Bick D. Born too soon: The global issue of preterm birth. Midwifery. 2012;28:341–342. doi: 10.1016/j.midw.2012.06.010. [DOI] [PubMed] [Google Scholar]
- 6.Liu L, Johnson HL, Cousens S, Perin J, Scott S, Lawn JE, Rudan I, Campbell H, Cibulskis R, Li M, Mathers C, Black RE. Global, regional, and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. Lancet. 2012;379:2151–2161. doi: 10.1016/S0140-6736(12)60560-1. [DOI] [PubMed] [Google Scholar]
- 7.Pott-Grinstein E, Newcomer JR. Gynecologists' patterns of prescribing pessaries. J Reprod Med. 2001;46:205–208. [PubMed] [Google Scholar]
- 8.Culligan PJ. Nonsurgical management of pelvic organ prolapse. Obstet Gynecol. 2012;119:852–860. doi: 10.1097/AOG.0b013e31824c0806. [DOI] [PubMed] [Google Scholar]
- 9.Cross R. Treatment of habitual abortion due to cervical incompetence. Lancet. 1959;274:127. [Google Scholar]
- 10.Dharan VB, Ludmir J. Alternative treatment for a short cervix: the cervical pessary. Semin Perinatol. 2009;33:338–342. doi: 10.1053/j.semperi.2009.06.008. [DOI] [PubMed] [Google Scholar]
- 11.Vitsky M. Pessary treatment of the incompetent cervical os. Obstet Gynecol. 1968;31:732–733. doi: 10.1097/00006250-196805000-00024. [DOI] [PubMed] [Google Scholar]
- 12.Vitsky M. The incompetent cervical os and the pessary. Am J Obstet Gynecol. 1963;87:144–147. doi: 10.1016/s0002-9378(16)35168-7. [DOI] [PubMed] [Google Scholar]
- 13.Oster S, Javert CT. Treatment of the incompetent cervix with the Hodge pessary. Obstet Gynecol. 1966;28:206–208. doi: 10.1097/00003081-196608000-00011. [DOI] [PubMed] [Google Scholar]
- 14.Jiratko K, Baran P, Zabransky F. Useful treatment of imminent precocious delivery. Confrontation of the results gained by cerclage and by insertion of a pessary (author's transl) Cesk Gynekol. 1976;41:184–186. [PubMed] [Google Scholar]
- 15.Seyffarth K. Non-invasive cerclage using supportive pessaries for prevention and therapy of premature birth. Zentralbl Gynakol. 1978;100:1566–1570. [PubMed] [Google Scholar]
- 16.Gmoser G, Girardi F, Mayer HO, Hermann J, Haas J. The support pessary-a therapeutic possibility in premature opening of the uterine cervix. Gynakol Rundsch. 1991;31(Suppl 2):117–119. [PubMed] [Google Scholar]
- 17.Forster F, During R, Schwarzlos G. [Therapy of cervix insufficiency-cerclage or support pessary?] Zentralbl Gynakol. 1986;108:230–237. [PubMed] [Google Scholar]
- 18.Abdel-Aleem H, Shaaban OM, Abdel-Aleem MA. Cervical pessary for preventing preterm birth. Cochrane Database Syst Rev. 2010;9 doi: 10.1002/14651858.CD007873.pub2. : CD007873. [DOI] [PubMed] [Google Scholar]
- 19.Arabin H. Pessartherapie (Therapy with pessaries) In: Martius G, editor. Gynäkologie. Thieme: Stuttgart-New York; 1991. pp. 263–276. [Google Scholar]
- 20.Arabin B, Halbesma JR, Vork F, Hubener M, van Eyck J. Is treatment with vaginal pessaries an option in patients with a sonographically detected short cervix? J Perinat Med. 2003;31:122–133. doi: 10.1515/JPM.2003.017. [DOI] [PubMed] [Google Scholar]
- 21.Goya M, Pratcorona L, Higueras T, Perez-Hoyos S, Carreras E, Cabero L. Sonographic cervical length measurement in pregnant women with a cervical pessary. Ultrasound Obstet Gynecol. 2011;38:205–209. doi: 10.1002/uog.8960. [DOI] [PubMed] [Google Scholar]
- 22.Kubli F, Arabin B. Frühgeburt (Preterm delivery) In: Dudenhausen JW, editor. Praxis der Perinatalmedizin (Practice of Perinatal Medicine) Thieme: Stuttgart-New York; 1982. pp. 148–184. [Google Scholar]
- 23.Quaas L, Hillemanns HG, du Bois A, Schillinger H. The Arabin cerclage pessary-an alternative to surgical cerclage. Geburtshilfe Frauenheilkd. 1990;50:429–433. doi: 10.1055/s-2008-1026276. [DOI] [PubMed] [Google Scholar]
- 24.Acharya G, Eschler B, Grønberg M, Hentemann M, Ottersen T, Maltau JM. Noninvasive cerlage for the management of cervical incompetence: a prospective study. Arch Gynecol Obstet. 2006;273:283–287. doi: 10.1007/s00404-005-0082-2. [DOI] [PubMed] [Google Scholar]
- 25.Sieroszewski P, Jasinski A, Perenc M, Banach R, Oszukowski P. The Arabin pessary for the treatment of threatened mid-trimester miscarriage or premature labour and miscarriage: a case series. J Matern Fetal Neonatal Med. 2009;22:469–472. doi: 10.1080/14767050802531748. [DOI] [PubMed] [Google Scholar]
- 26.Kimber-Trojnar Z, Patro-Malysza J, Leszczynska-Gorzelak B, Marciniak B, Oleszczuk J. Pessary use for the treatment of cervical incompetence and prevention of preterm labour. J Matern Fetal Neonatal Med. 2010;23:1493–1499. doi: 10.3109/14767051003678093. [DOI] [PubMed] [Google Scholar]
- 27.Ting YH, Lao TT, Law LW, Hui SY, Chor CM, Lau TK, Leung TY. Arabin cerclage pessary in the management of cervical insufficiency. J Matern Fetal Neonatal Med. 2012;25:2693–2695. doi: 10.3109/14767058.2012.712559. [DOI] [PubMed] [Google Scholar]
- 28.Newcomer J. Pessaries for the treatment of incompetent cervix and premature delivery. Obstet Gynecol Surv. 2000;55:443–448. doi: 10.1097/00006254-200007000-00023. [DOI] [PubMed] [Google Scholar]
- 29.Goya M, Pratcorona L, Merced C, Rodo C, Valle L, Romero A, Juan M, Rodriguez A, Munoz B, Santacruz B, Bello-Munoz JC, Llurba E, Higueras T, Cabero L, Carreras E. Cervical pessary in pregnant women with a short cervix (PECEP): an open-label randomised controlled trial. Lancet. 2012;379:1800–1806. doi: 10.1016/S0140-6736(12)60030-0. [DOI] [PubMed] [Google Scholar]
- 30.Cannie MM, Dobrescu O, Gucciardo L, Strizek B, Ziane S, Sakkas E, Schoonjans F, Divano L, Jani JC. Arabin cervical pessary in women at high risk of preterm birth: a magnetic resonance imaging observational follow-up study. Ultrasound Obstet Gynecol. 2013;42:426–433. doi: 10.1002/uog.12507. [DOI] [PubMed] [Google Scholar]
- 31.Arabin B, Roos C, Kollen B, van Eyck J. Comparison of transvaginal sonography in recumbent and standing maternal positions to predict spontaneous preterm birth in singleton and twin pregnancies. Ultrasound Obstet Gynecol. 2006;27:377–386. doi: 10.1002/uog.2694. [DOI] [PubMed] [Google Scholar]
- 32.Romero R, Chaiworapongsa T, Alpay Savasan Z, Xu Y, Hussein Y, Dong Z, Kusanovic JP, Kim CJ, Hassan SS. Damage-associated molecular patterns (DAMPs) in preterm labor with intact membranes and preterm PROM: a study of the alarmin HMGB1. J Matern Fetal Neonatal Med. 2011;24:1444–1455. doi: 10.3109/14767058.2011.591460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Romero R, Friel LA, Velez Edwards DR, Kusanovic JP, Hassan SS, Mazaki-Tovi S, Vaisbuch E, Kim CJ, Erez O, Chaiworapongsa T, Pearce BD, Bartlett J, Salisbury BA, Anant MK, Vovis GF, Lee MS, Gomez R, Behnke E, Oyarzun E, Tromp G, Williams SM, Menon R. A genetic association study of maternal and fetal candidate genes that predispose to preterm prelabor rupture of membranes (PROM) Am J Obstet Gynecol. 2010;203:361.e1–30. doi: 10.1016/j.ajog.2010.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Becher N, Adams Waldorf K, Hein M, Uldbjerg N. The cervical mucus plug: structured review of the literature. Acta Obstet Gynecol Scand. 2009;88:502–513. doi: 10.1080/00016340902852898. [DOI] [PubMed] [Google Scholar]
- 35.Lee DC, Hassan SS, Romero R, Tarca AL, Bhatti G, Gervasi MT, Caruso JA, Stemmer PM, Kim CJ, Hansen LK, Becher N, Uldbjerg N. Protein profiling underscores immunological functions of uterine cervical mucus plug in human pregnancy. J Proteomics. 2011;74:817–828. doi: 10.1016/j.jprot.2011.02.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ferguson JKW. A study of the motility of the intact uterus at term. Surg Gynecol Obstet. 1941;73:359–366. [Google Scholar]
- 37.Liem SM, van Pampus MG, Mol BW, Bekedam DJ. Cervical pessaries for the prevention of preterm birth: a systematic review. Obstet Gynecol Int. 2013;2013:576723. doi: 10.1155/2013/576723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fonseca EB, Celik E, Parra M, Singh M, Nicolaides KH. Progesterone and the risk of preterm birth among women with a short cervix. N Engl J Med. 2007;357:462–469. doi: 10.1056/NEJMoa067815. [DOI] [PubMed] [Google Scholar]
- 39.Hassan SS, Romero R, Vidyadhari D, Fusey S, Baxter JK, Khandelwal M, Vijayaraghavan J, Trivedi Y, Soma-Pillay P, Sambarey P, Dayal A, Potapov V, O'Brien J, Astakhov V, Yuzko O, Kinzler W, Dattel B, Sehdev H, Mazheika L, Manchulenko D, Gervasi MT, Sullivan L, Conde-Agudelo A, Phillips JA, Creasy GW. Vaginal progesterone reduces the rate of preterm birth in women with a sonographic short cervix: a multicenter, randomized, double-blind, placebo-controlled trial. Ultrasound Obstet Gynecol. 2011;38:18–31. doi: 10.1002/uog.9017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Romero R, Nicolaides KH, Conde-Agudelo A, Tabor A, O'Brien JM, Cetingoz E, Da Fonseca E, Creasy GW, Klein K, Rode L, Soma-Pillay P, Fusey S, Cam C, Alfirevic Z, Hassan SS. Vaginal progesterone in women with an asymptomatic sonographic short cervix in the midtrimester decreases preterm delivery and neonatal morbidity: a systematic review and metaanalysis of individual patient data. Am J Obstet Gynecol. 2012;206:124.e121–119. doi: 10.1016/j.ajog.2011.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Campbell S. Universal cervical-length screening and vaginal progesterone prevents early preterm births, reduces neonatal morbidity and is cost saving: doing nothing is no longer an option. Ultrasound Obstet Gynecol. 2011;38:1–9. doi: 10.1002/uog.9073. [DOI] [PubMed] [Google Scholar]
- 42.Practice bulletin no. 130. prediction and prevention of preterm birth. Obstet Gynecol. 2012;120:964–973. doi: 10.1097/AOG.0b013e3182723b1b. [DOI] [PubMed] [Google Scholar]
- 43.Berghella V, Baxter JHK, Hendrix NW. Cervical assessment by ultrasound for preventing preterm delivery. Cochrane Database Syst Rev. 2013;1 doi: 10.1002/14651858.CD007235.pub3. : CD007235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Nicolaides KH. Nuchal translucency and other first-trimester sonographic markers of chromosomal abnormalities. Am J Obstet Gynecol. 2004;191:45–67. doi: 10.1016/j.ajog.2004.03.090. [DOI] [PubMed] [Google Scholar]
- 45.Hui SY, Chor CM, Lau TK, Lao TT, Leung TY. Cerclage pessary for preventing preterm birth in women with a singleton pregnancy and a short cervix at 20 to 24 weeks: a randomized controlled trial. Am J Perinatol. 2013;30:283–288. doi: 10.1055/s-0032-1322550. [DOI] [PubMed] [Google Scholar]
- 46.Honest H, Bachmann LM, Coomarasamy A, Gupta JK, Kleijnen J, Khan KS. Accuracy of cervical transvaginal sonography in predicting preterm birth: a systematic review. Ultrasound Obstet Gynecol. 2003;22:305–322. doi: 10.1002/uog.202. [DOI] [PubMed] [Google Scholar]
- 47.Salomon LJ, Diaz-Garcia C, Bernard JP, Ville Y. Reference range for cervical length throughout pregnancy: non-parametric LMS-based model applied to a large sample. Ultrasound Obstet Gynecol. 2009;33:459–464. doi: 10.1002/uog.6332. [DOI] [PubMed] [Google Scholar]
- 48.Alfirevic Z, Owen J, Carreras Moratonas E, Sharp AN, Szychowski JM, Goya M. Vaginal progesterone, cerclage or cervical pessary for preventing preterm birth in asymptomatic singleton pregnant women with history of preterm birth and a sonographic short cervix. Ultrasound Obstet Gynecol. 2013;41:146–151. doi: 10.1002/uog.12300. [DOI] [PubMed] [Google Scholar]
- 49.Makrydimas G. Re: Vaginal progesterone, cerclage or cervical pessary for preventing preterm birth in asymptomatic singleton pregnant women with history of preterm birth and a sonographic short cervix. Ultrasound Obstet Gynecol. 2013;41:130. doi: 10.1002/uog.12300. [DOI] [PubMed] [Google Scholar]
- 50.Carreras E, Arevalo S, Bello-Munoz JC, Goya M, Rodo C, Sanchez-Duran MA, Peiro JL, Cabero L. Arabin cervical pessary to prevent preterm birth in severe twin-to-twin transfusion syndrome treated by laser surgery. Prenat Diagn. 2012;32:1181–1185. doi: 10.1002/pd.3982. [DOI] [PubMed] [Google Scholar]
- 51.Caritis SN, Simhan HN, Zhao Y, Rouse DJ, Peaceman AM, Sciscione A, Spong CY, Varner MW, Malone FD, Iams JD, Mercer BM, Thorp JM, Jr SorokinY, Carpenter M, Lo J, Ramin SM, Harper M. Relationship between 17-hydroxyprogesterone caproate concentrations and gestational age at delivery in twin gestation. Am J Obstet Gynecol. 2012;207:396.e391–398. doi: 10.1016/j.ajog.2012.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Norman JE, Mackenzie F, Owen P, Mactier H, Hanretty K, Cooper S, Calder A, Mires G, Danielian P, Sturgiss S, MacLennan G, Tydeman G, Thornton S, Martin B, Thornton JG, Neilson JP, Norrie J. Progesterone for the prevention of preterm birth in twin pregnancy (STOPPIT): a randomised, double-blind, placebo-controlled study and meta-analysis. Lancet. 2009;373:2034–2040. doi: 10.1016/S0140-6736(09)60947-8. [DOI] [PubMed] [Google Scholar]
- 53.Berghella V, Odibo AO, To MS, Rust OA, Althuisius SM. Cerclage for short cervix on ultrasonography: meta-analysis of trials using individual patient-level data. Obstet Gynecol. 2005;106:181–189. doi: 10.1097/01.AOG.0000168435.17200.53. [DOI] [PubMed] [Google Scholar]
- 54.Rode L, Klein K, Nicolaides KH, Krampl-Bettelheim E, Tabor A. Prevention of preterm delivery in twin gestations (PREDICT): a multicenter, randomized, placebo-controlled trial on the effect of vaginal micronized progesterone. Ultrasound Obstet Gynecol. 2011;38:272–280. doi: 10.1002/uog.9093. [DOI] [PubMed] [Google Scholar]
- 55.Liem S, Schuit E, Bais J, de Boer K, Bloemenkamp K, Brons J, Duvekot J, Bijvank BN, Franssen M, Gaugler I, Molkenboer J, Oudijk M, Papatsonis D, Pernet P, Porath M, Scheepers H, Sikkema M, Sporken J, Visser H, van Wijngaarden W, Woiski M, van Pampus M, Mol BW. Bekedam D for the ProTWIN study group. Pessaries in multiple pregnancy as a prevention of preterm birth (ProTWIN): a randomized controlled trial. Am J Obstet Gynecol. 2013;208(Suppl) [Google Scholar]
- 56.Liem S, Schuit E, Hegeman M, Bais J, de Boer K, Bloemenkamp K, Brons J, Duvekot H, Bijvank BN, Franssen M, Gaugler I, de Graaf I, Oudijk M, Papatsonis D, Pernet P, Porath M, Scheepers L, Sikkema M, Sporken J, Visser H, van WijngaardenW WoiskiM, van Pampus M, Mol BW, Bekedam D. Cervical pessaries for prevention of preterm birth in women with a multiple pregnancy (ProTWIN): a multicentre, open-label randomised controlled trial. Lancet. 2013 doi: 10.1016/S0140-6736(13)61408-7. DOI 10.1016/S0140-6736(13)61408-7. [DOI] [PubMed] [Google Scholar]
- 57.Danforth DN. The distribution and functional activity of the cervical musculature. Am J Obstet Gynecol. 1954;68:1261–1271. [PubMed] [Google Scholar]
- 58.Castanon A, Brocklehurst P, Evans H, Peebles D, Singh N, Walker P, Patnick J, Sasieni P. Risk of preterm birth after treatment for cervical intraepithelial neoplasia among women attending colposcopy in England: retrospective-prospective cohort study. BMJ. 2012;345:e5174. doi: 10.1136/bmj.e5174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Bruinsma FJ, Quinn MA. The risk of preterm birth following treatment for precancerous changes in the cervix: a systematic review and meta-analysis. BJOG. 2011;118:1031–1041. doi: 10.1111/j.1471-0528.2011.02944.x. [DOI] [PubMed] [Google Scholar]
- 60.Fox NS, Gelber SE, Kalish RB, Chasen ST. History-indicated cerclage: practice patterns of maternal-fetal medicine specialists in the USA. J Perinat Med. 2008;36:513–517. doi: 10.1515/JPM.2008.083. [DOI] [PubMed] [Google Scholar]
- 61.Lee SM, Jun JK. Prediction and prevention of preterm birth after cervical conization. J Gynecol Oncol. 2010;21:207–208. doi: 10.3802/jgo.2010.21.4.207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Nam KH, Kwon JY, Kim YH, Park YW. Pregnancy outcome after cervical conization: risk factors for preterm delivery and the efficacy of prophylactic cerclage. J Gynecol Oncol. 2010;21:225–229. doi: 10.3802/jgo.2010.21.4.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kyvernitakis I, Arabin B. Is there a place for the Arabin pessary and abdominal cerclage? Lisbon: COGI congress; 2012. Early treatment of cervical shortening after conization. http://www.congressmed.com/cogilisbon/program/e-posters.html (P299) [Google Scholar]
- 64.Society of Maternal Fetal Medicine assisted by Vinceco Berghella. Progesterone and preterm birth prevention: translating clinical trials data into clinical practice. Am J Obstet Gynecol. 2012;206:376–386. doi: 10.1016/j.ajog.2012.03.010. [DOI] [PubMed] [Google Scholar]
- 65.Feltovich H, Hall TJ, Berghella V. Beyond cervical length: emerging technologies for assessing the pregnant cervix. Am J Obstet Gynecol. 2012;207:345–354. doi: 10.1016/j.ajog.2012.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Feltovich H, Hall TJ. Quantitative imaging of the cervix: setting the bar. Ultrasound Obstet Gynecol. 2013;41:121–128. doi: 10.1002/uog.12383. [DOI] [PubMed] [Google Scholar]
- 67.Hernandez-Andrade E, Hassan SS, Ahn H, Korzeniewski SJ, Yeo L, Chaiworapongsa T, Romero R. Evaluation of cervical stiffness during pregnancy using semiquantitative ultrasound elastography. Ultrasound Obstet Gynecol. 2013;41:152–161. doi: 10.1002/uog.12344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Romero R, Mazaki-Tovi S, Vaisbuch E, Kusanovic JP, Chaiworapongsa T, Gomez R, Nien JK, Yoon BH, Mazor M, Luo J, Banks D, Ryals J, Beecher C. Metabolomics in premature labor: a novel approach to identify patients at risk for preterm delivery. J Matern Fetal Neonatal Med. 2010;23:1344–1359. doi: 10.3109/14767058.2010.482618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Burwick RM, Zork NM, Lee GT, Ross MG, Kjos SL. Cervilenz assessment of cervical length compared to fetal fibronectin in the prediction of preterm delivery in women with threatened preterm labor. J Matern Fetal Neonatal Med. 2011;24:127–131. doi: 10.3109/14767058.2010.529201. [DOI] [PubMed] [Google Scholar]
- 70.Burwick RM, Lee GT, Benedict JL, Ross MG, Kjos SL. Blinded comparison of cervical portio length measurements by digital examination vs Cervilenz. Am J Obstet Gynecol. 2009;200:e37–39. doi: 10.1016/j.ajog.2008.11.026. [DOI] [PubMed] [Google Scholar]
- 71.Conde-Agudelo A, Romero R, Nicolaides KH, Chaiworapongsa T, O'Brien JM, Cetingoz E, da Fonseca E, Creasy G, Soma-Pillay P, Fusey S, Cam C, Alfirevic Z, Hassan SS. Vaginal progesterone vs. cervical cerclage for the prevention of preterm birth in women with a sonographic short cervix, previous preterm birth, and singleton gestation: a systematic review and indirect comparison metaanalysis. Am J Obstet Gynecol. 2013;208:42.e1–18. doi: 10.1016/j.ajog.2012.10.877. [DOI] [PMC free article] [PubMed] [Google Scholar]


