Abstract
Objective
Assess the performance of ultrasound (US) in pregnant patients presenting with acute abdominal pain concerning for appendicitis.
Methods
Descriptive analysis of pregnant patients who underwent an US for acute abdominal pain over a 6-year period using data from a statewide quality improvement collaborative and a single center.
Results
Statewide, 131 pregnant patients underwent an appendectomy and 85% had an US. In our single-center case series, 49 pregnant patients underwent an US for acute abdominal pain and four patients had appendicitis (8%). Of those, three were definitively diagnosed with US. The appendix was visualized by US in five patients (3 appendicitis/2 normal). Mean gestational age was 11 weeks for visualization of the appendix versus 20 weeks for non-visualization (p < 0.001). Concordance between US and pathology was similar statewide and at our institution (43%).
Conclusions
US appears to play a central role in the evaluation of appendicitis in pregnant women, especially in the first trimester, and often contributes to definitive disposition. US performed less well in excluding appendicitis; however, in certain clinical settings, providers appeared to trust US findings. From these results, we developed a multidisciplinary imaging pathway for pregnant patients who present with acute abdominal pain concerning for appendicitis.
Keywords: Appendicitis, diagnostic imaging, pregnancy
Introduction
Concern for appendicitis in the pregnant patient is an especially challenging clinical scenario. Appropriately identifying those who require an operation in a timely fashion and preventing unnecessary operations that expose mother and fetus to the risks of surgery can be competing imperatives [1]. Judicious use of diagnostic imaging is a useful adjunct to history, examination, and laboratory studies, but avoiding unnecessary imaging is both a safety and cost issue. In non-pregnant women, there is ample evidence that the use of advanced imaging in suspected appendicitis can reduce the frequency of performing an appendectomy where the final pathology reveals a normal appendix, known as a negative appendectomy (NA), without an associated increase in the frequency of perforation [2,3]. Much less about the use of imaging in pregnant patients is known, with at least one recent report calling for a multi-center trial to investigate optimal imaging strategies for pregnant patients in the setting of suspected appendicitis [4]. Although computed tomography (CT) scans are highly accurate in patients with acute appendicitis, the American College of Radiology Appropriateness Criteria published in 2011 state ‘‘ionizing radiation from CT should be avoided during pregnancy. Ultrasound is clearly a safer imaging option’’ [5]. For this reason, ultrasound (US) is often the favored first-line imaging modality.
The purpose of this report was to evaluate diagnostic performance of US in pregnant patients with acute abdominal pain concerning for appendicitis as a baseline for the development of a standardized imaging protocol in this population. This quality improvement initiative was designed to evaluate two separate data sources. The first data source is a large, statewide hospital collaborative, the Surgical Care and Outcomes Assessment Program (SCOAP), aimed at improving the quality of surgical care in Washington State. SCOAP includes data from patients who underwent appendectomy at 55 hospitals in Washington State and tracks concordance of US findings with pathology results. This database represents more than 85% of the appendectomies performed in Washington State. The second source of data is a review of pregnant patients presenting to our institution with acute abdominal pain potentially representing appendicitis. The case review was designed to assess three specific issues: the ability of US to accurately detect appendicitis in pregnant patients, the ability of US to assist in excluding appendicitis (and make accurate alternative diagnoses), and the ability of US to contribute to the safe discharge of patients who do not require inpatient observation and care.
Methods
Analysis of statewide SCOAP database
The SCOAP database was queried to characterize performance of US within a population of pregnant patients. Data collection began in 2006 and, currently, 55 hospitals contribute to the database. Clinical and demographic information was collected by trained abstractors directly from patient charts. The database was used to quantify the number of pregnant women who underwent appendectomy in Washington State from 1 January 2006 to 21 December 2011 as well as the diagnostic imaging utilized in their pre-operative evaluations. The NA rate among all pregnant patients who underwent appendectomy was calculated. SCOAP also measures ‘‘concordance’’, which is defined as agreement between the final radiology and pathology reports. ‘‘Indeterminate’’ imaging studies are considered discordant by SCOAP.
Case series review
A case review was performed of all pregnant patients who presented to our institution over the same 6-year period with acute abdominal pain and who underwent US. All US were performed on Philips, IU-22 System (Bothell, WA) with linear (5–10 MHz) and curvilinear (1–5 MHz) transducers by sonographers with more than 5 years of experience and attending radiologists in real time. Dedicated images of the right lower quadrant were obtained. If the appendix was visualized, the diameter, vascularity and peri-appendiceal fluid were assessed.
A database maintained by the University of Washington Medical Center, Department of Radiology, was queried by indication to identify patients. Patients with palpable abdominal masses (e.g. clinically obvious hernias) or post-operative concerns were excluded. The electronic medical records of identified patients were evaluated for clinical information including: age, gestational age (GA) of the fetus, white blood cell (WBC) count, US findings, additional imaging modalities and associated radiographic interpretations, disposition, surgical findings, and discharge diagnosis. For surgical patients, the pathology report was utilized to reach a final diagnosis of acute appendicitis, perforated appendicitis, or normal appendix (NA). For patients discharged without a specific diagnosis, chart review was continued for the remainder of the pregnancy to assess for readmission with appendicitis. Continuous variables were compared using Student’s t-test and proportional data compared using Pearson’s chi-square test. Statistical significance was set at p < 0.05. All analysis was carried out in STATA version 12 (StataCorp, College Station, TX).
The University of Washington Medical Center Human Subjects Division determined that neither analysis required IRB review.
Results
Statewide results
A total of 131 pregnant patients underwent appendectomy in a SCOAP hospital between 2006 and 2011. Of these, 130 (99.2%) underwent imaging: 85% had an US, 10% had a CT scan, and 30% had an MRI (some had multiple modalities of imaging). The NA rate was 16.8% and the perforation rate was 13%. US concordance was 42.7%, CT concordance was 66.7%, and MRI concordance was 61.1%.
Case review
Forty-nine patients met inclusion criteria. Each patient was pregnant, between the age of 16 and 43 (mean age, 28 years), and underwent abdominal US for acute abdominal pain and/or suspected appendicitis. Seven patients had surgery for suspected appendicitis (Table 1). Four patients had pathology-confirmed appendicitis, with one case of perforated appendicitis. Three of the four patients with appendicitis had US studies positive for appendicitis and did not undergo any further imaging prior to surgery. All the three were in the first trimester (Table 1). The fourth patient with pathology-confirmed appendicitis (16 weeks GA) had a non-diagnostic US and a CT scan demonstrating acute appendicitis.
Table 1.
Characteristics of patients undergoing appendectomy.
| Indication for US | Year | US findings | Age | WBC | EGA | Follow-up imaging and findings | Pathology |
|---|---|---|---|---|---|---|---|
| RLQ pain, rule-out appendicitis | 2010 | Dilated appendix (9.4 mm) and 2 appendicoliths | 21 | 16.3 | 12 4/7 | None | Acute appendicitis |
| RLQ pain, increased WBC | 2008 | 10 mm, non-compressible appendix, consistent with appendicitis | 29 | 12.2 | 11 0/7 | None | Acute appendicitis |
| Worsening pelvic pain, positive peritoneal signs | 2007 | 15 mm, non-compressible appendix, consistent with appendicitis | 35 | 11.7 | 12 6/7 | None | Perforated appendix |
| RLQ pain | 2010 | Normal right ovary, appendix could not be visualized | 34 | 11.8 | 16 0/7 | CT. Mild enhancing, thickened appendiceal wall consistent with early AA. | Acute appendicitis |
| Rule-out appendicitis | 2008 | No dilated tubular structure in RLQ; mild hydronephrosis. | 29 | 12.9 | 35 1/7 | MRI. Appendix not definitively identified but evidence of RLQ inflammation consistent with AA. | Normal appendix |
| Right flank pain in setting of chronic UTIs. Pain/chills despite broad abx. | 2011 | Right kidney unchanged from prior exam; appendix not visualized, no secondary signs; pain over cecum. | 28 | 15.2 | 31 0/7 | MRI. Slightly enlarged appendix (9 mm) with fluid and irregular signal in peri-appendiceal fat consistent with acute appendicitis. | Normal appendix |
| RLQ pain, known R ovarian cystic mass | 2008 | No evidence of torsion of known mass; appendix not visualized. | 28 | 10.0 | 25 0/7 | None. Taken to OR based on clinical suspicion for acute appendicitis. | Normal appendix |
US indication and findings, clinical characteristics, other imaging and pathology results for the 7 patients who underwent appendectomy in this series (4 with appendicitis, 3 with NA). WBC, white blood cell count. EGA, estimated gestational age.
Three of the seven patients taken for surgery did not have pathology-confirmed appendicitis, resulting in a NA rate of 43%. All the three had non-visualization of the appendix and no secondary signs of appendicitis on US. Two underwent MRI that suggested appendicitis; in one, the appendix was not visualized on MRI but there was inflammation in the expected location of the appendix, and in the other case, MRI noted appendiceal enlargement and signs of inflammation consistent with early/mild appendicitis. The third NA in this series had a non-diagnostic US, no further imaging was taken to the OR based on clinical suspicion. All three of these patients had medically complex pregnancies and a history of pelvic abnormalities.
US correctly identified three of the four patients with appendicitis. There were no definitive US studies that reported false positives; however, two US studies in which the appendix was not visualized reported equivocal, non-specific findings potentially concerning for appendicitis. Neither patient was ultimately diagnosed with appendicitis. There were no definitive false negatives, although one patient with appendicitis underwent non-diagnostic US (non-visualization of the appendix) and had a CT concerning for appendicitis. Two US scans, both in the first trimester, definitively reported a normal appendix. Forty-four (90%) of the 49 patients in this series had a non-visualized appendix on US.
In all five of the cases in which the appendix was identified, definitive disposition was reached based on clinical and US findings without additional imaging (Table 2). Two were discharged home from the emergency department (ED), and three proceeded to surgery for appendectomy. Comparing the patients with visualized versus non-visualized appendices, mean GA was 11 versus 20.3 weeks, respectively (p < 0.001). Of those in the first trimester, the appendix was visualized in 33.3%. The appendix was not visualized in any patients in the second or third trimester.
Table 2.
Patients in whom US visualized the appendix.
| Appendix visualized | US diagnosis | EGA | Follow-up imaging | Ultimate Diagnosis | Ultimate disposition |
|---|---|---|---|---|---|
| Yes (n = 3) | Appendicitis | 11; 0/7 | None | Appendicitis | Surgery |
| 12; 4/7 | Appendicitis | Surgery | |||
| 12; 6/7 | Perforated appendicitis | Surgery | |||
| Yes (n = 1) | No appendicitis; no additional dx | 10; 5/7 | None | Abdominal Pain (NOS) | Discharged home |
| Yes (n = 1) | No appendicitis; additional dx noted | 8; 0/7 | None | Subchorionic hemorrhage | Discharged home |
For 41 of the 44 patients (93%) without appendix visualization, the US report specified an absence of concerning secondary signs for appendicitis (although one of these patients actually did have appendicitis). For 16 of the patients with a non-visualized appendix (36%), a potential alternative diagnosis was suggested by US. Forty-one percent of those patients, who initially underwent US, had follow-up imaging by CT scan (n = 9) or MRI (n = 9). The presence of sonographic abnormalities was not predictive of whether a patient would undergo additional imaging: 40% of those without abnormal findings proceeded to additional imaging versus 47% of those with abnormal US findings (p = 0.68). For those patients in whom US suggested a possible alternative diagnosis, US findings matched the discharge diagnosis in 56% of patients (Table 3). About 83.3% of patients found to have an obstetrical or gynecologic lesion on US (such as a fibroid, subchorionic hemorrhage, or ruptured corpus luteum) did not require follow-up imaging.
Table 3.
Discharge diagnosis in patients with positive US findings (if appendix not visualized).
| Alternative US findings if appendix not visualized | F/U imaging: modality and findings | Disposition from ED | Discharge diagnosis | Agree |
|---|---|---|---|---|
| Subchorionic hemorrhage | None | Home | Possible threatened miscarriage, subchorionic hemorrhage | Y |
| Asymmetric hydronephrosis, physiologic pelvic fluid | None | Home | Possible nephrolithiasis | Y |
| Right renal cyst, unchanged in size. Normal right ovary | MRI – acute appendicitis | Admission; appendectomy | Chronic pyelonephritis (Underwent NA) | N |
| Multiple gallbladder polyps, no stones or evidence of cholecystitis | CT – no abnormal findings | Admission | Round ligament pain assoc. with preterm contractions | N |
| Large fibroid at site of pain | None | Home | Degenerating fibroid | Y |
| Epiploic appendigitis | CT – bilateral hydronephrosis and hydrouretor related to uterine compression | Admission | Epiploic appendigitis | Y |
| Small right hydronephrosis, otherwise normal US | None | Admission | Round ligament versus musculoskeletal pain | N |
| Large, tender uterine fibroid | MRI – appendix mildly enlarged but no fat stranding or fluid collection. Possible early appendicitis | Admission | Round ligament pain versus fibroid pain | Y |
| Mild right hydronephrosis | None | Home | Mild hydronephrosis | N |
| Complex right ovarian mass (without evidence of torsion) | None | Admission; appendectomy | Discharge: appendicitis Pathology: negative for Appendicitis | N |
| Right side of uterine wall thickened with sonolucency – fibroid versus contraction | CT pelvis – normal appendix, slight right hydroureter and hydronephrosis | Admission | No clear diagnosis for abdominal pain | N |
| Mild right hydronephrosis | MRI – RLQ inflammation in expected location of appendix (but not visualized) | Admission; appendectomy | Discharge: appendicitis Pathology: negative for appendicitis | N |
| Mild right hydronephrosis | None | Admission | Pyelonephritis, possible nephrolithiasis | Y |
| Edematous left kidney consistent with pyelonephritis | None | Admission | Pyelonephritis | Y |
| Small umbilical hernia | CT – no abnormal findings | Admission | No clear etiology, pain possibly related to umbilical hernia | Y |
| Right corpus luteum and trace free fluid | None | Home | Possible ruptured corpus luteum | Y |
Table 3 describes the ultimate diagnosis for those patients in whom the appendix was not visualized but US did have positive findings; the final column states whether the US findings and discharge diagnosis agreed.
Nine patients underwent CT and nine underwent MRI. The appendix was visualized on all CT scans, and one early case of appendicitis was detected. Five patients had negative CT scans, of which, one was discharged home from the ED. Two patients had CT scans that were negative for appendicitis, but additional diagnoses were detected. One CT was equivocal. The appendix was visualized in six of the nine patients with follow-up MRI (78%). MRI erroneously suggested two cases of appendicitis, resulting in two of the three NAs in this series. Five patients with MRIs negative for appendicitis and one with an equivocal examination were admitted for inpatient, non-surgical care. One was discharged immediately following negative MRI results.
Overall, 19 patients (39%) were discharged home from the ED or clinic. All other patients were admitted for observation, in-patient care, or surgery. US was the only imaging modality deployed for 17 of those discharged. Among those with any findings and no appendix visualized, 27% were discharged home; comparatively, 36% of those who had no US findings were discharged home (p = 0.54). Among the 18 patients who had follow-up MRI or CT scan, two were discharged home.
Chart review was performed for all patients who were discharged without a definitive diagnosis to assess for readmission for appendicitis (n = 14). Complete follow-up through the end of pregnancy was achieved in eight patients, and there were no reported cases of appendicitis. One patient was followed through 34 weeks GA and five were lost to follow-up after evaluation for RLQ pain.
Discussion
Statewide and at our institution, US has been the most frequently utilized imaging test employed in the evaluation of pregnant women with acute abdominal pain and concern for appendicitis. Our results indicate that US plays a central role in these evaluations, detects appendicitis relatively well in the first trimester, and often contributes to definitive disposition. However, the non-visualization rate of US is high, especially in the later trimesters.
Given the retrospective nature of this project, the small number of patients included in the detailed case review, and the lack of a priori defined criteria for negative, positive, and indeterminate studies, we attempted to make a practical assessment of the performance characteristics of US in our pregnant population. In this study, specificity of US (true negatives/[true negative + false positive]) was 95.7% (44/46), considering the two equivocal studies as false positives. If only scans with definitive visualization of the appendix are considered, specificity was 100% (two true negatives, no false positives) and sensitivity was also 100% (three true positives, no definitive false negatives). From a practical standpoint, we considered the sensitivity of US to be 75%, given that four patients had pathology-proven appendicitis and US correctly detected three of these patients. Positive predictive value (PPV) and specificity were both 100% given that three patients were definitively diagnosed with appendicitis on US and all three of these patients had appendicitis.
Negative predictive value (NPV), in practical terms, reflects the certainty with which a negative result can be trusted. If the appendix was definitively visualized, NPV was 100%. However, this reflects results from just two patients. The fact that the appendix could not be visualized in 90% of patients makes ruling out appendicitis USs most limiting performance characteristic. Interestingly, our data show that patients in whom US suggested an alternative diagnosis were just as likely to undergo follow-up imaging as those in whom there are no alternative findings. Ultimately, given that US is a test without purely binary results, assessing sensitivity alongside the frequency of indeterminate results (recognizing that ‘‘indeterminate’’ can be defined broadly) may be the best way to judge how well US does in practice when used to assess pregnant women with acute abdominal pain.
Our analysis of statewide and single institution data are generally consistent with other small series of diagnostic imaging in pregnant women. Graded compression US is the most frequently utilized modality for evaluating suspected appendicitis. Despite this, many studies report poor performance, usually related to inability of US to visualize the appendix [6]. In a recent study of 99 women in the second or third trimester, US was unable to locate the appendix in 97% of the patients. Of these 99 patients, seven had appendicitis and only two had a positive US. In other recent studies, US fared little better in pregnant patients: non-visualization of the appendix ranged from 88% to 96% [7,8].
Because US so frequently fails to identify the appendix and CT scan exposes the developing fetus to radiation, MRI has emerged as useful option in suspected appendicitis [9]. A recent systematic review of eight studies compared CT and MRI in the second and third trimester. MRI had a pooled sensitivity of 80% and specificity of 99% while CT was 85.7% and 97.4%, respectively [10]. In a 2011 meta-analysis of MRI that includes two additional large studies not included in the above review, pooled sensitivity was 91%, specificity 98%, PPV 86%, and NPV 99%. In this meta-analysis, indeterminate results (in which the appendix was not visualized and there was no peri-cecal fat stranding) were interpreted as negative results for the purposes of calculating performance characteristics [4]. In another report, the routine use of MRI in a single institution decreased the NA by 47% without significantly changing the perforation rate [11]. In Washington State, SCOAP data suggest that MRI is being increasingly utilized in the evaluation of pregnant women for possible appendicitis, as nearly one-third of pregnant patients in the database underwent MRI.
This analysis has some limitations. Data from SCOAP are not stratified by GA and come from many different hospitals with different US equipment, protocols, and operators. These differences may have influenced our results; however, this ‘‘real-world’’ dataset may more accurately reflect the experience of clinicians taking care of pregnant patients. The case series, while approximately the same size as other series published in the literature, is not large, only four patients had appendicitis and patients proceeding directly to the OR based on clinical suspicion alone were not included. Follow-up for those patients who did not undergo appendectomy was accomplished by chart review only. If patients with missed diagnosis of appendicitis presented to a different hospital after discharge from our institution, they would have been misclassified in our study. Combining analysis of statewide data and single-institution data was one attempt to ameliorate some of these limitations. Notably, radiology–pathology concordance estimated for US in the statewide SCOAP dataset (42.7%) is nearly identical to concordance in pregnant appendectomy patients at our institution (42.9%).
In the nearly 50 pregnant women, we reviewed who underwent US for acute abdominal pain, US performed relatively well in detection of appendicitis and accuracy in diagnosing the disease. It performed less well in ruling out the disease, but within certain clinical settings, clinicians appeared to trust an US that did not visualize the appendix: less than half the patients in whom the appendix was not visualized proceeded to further imaging, and over half of those who did not receive additional imaging were discharged home. US identified the appendix more frequently in early gestation, consistent with previous literature. Surprisingly, among the three NAs reported in this series, two had false-positive MRIs. However, because we did not evaluate all pregnant patients who underwent CT or MRI, we are unable to directly compare these modalities to US.
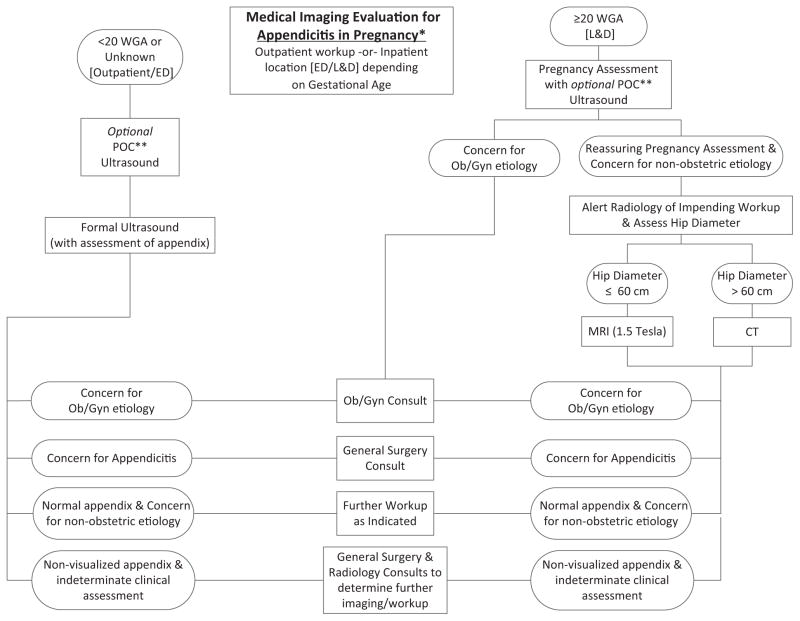
Based on these data, we have developed an imaging protocol for pregnant women (Figure 1). A prospective study utilizing this protocol will assess the correlation between imaging findings and pathology, factors contributing to indeterminate imaging, pregnancy outcome, timing of workup, and the role imaging plays in patient disposition. Our hypothesis is that a streamlined protocol will assist in avoiding imaging that is unlikely to be useful (i.e. attempting to visualize the appendix with US at a later gestational age), avoiding unnecessary radiation exposure, and expediting the diagnostic workup. Collectively, a successful protocol should decrease cost, increase patient satisfaction and safety, and increase provider confidence in the diagnostic pathway.
Figure 1.
Imaging protocol developed based on the results of this data analysis. This protocol is under evaluation in a prospective research study to characterize diagnostic accuracy, length of evaluation prior to disposition (discharge, observation, surgery, or other intervention), and contribution to clinical decision-making. As data are collected and analyzed, alterations may be made to the algorithm. *Pregnancy: defined by documented pregnancy test and/or previous clinical exam and/or ultrasound consistent with intrauterine pregnancy. **POC = Point of Care: An optional assessment performed by qualified ED or OB provider using a portable trans-abdominal and/or trans-vaginal ultrasound to confirm IUP with cardiac activity, assess for free fluid in posterior cul-de-sac, assess placental location (if appropriate) and adnexa. If adnexal and/or abdominal pathology is suspected, a formal ultrasound should be obtained at the discretion of the health care provider.
Acknowledgments
The Comparative Effectiveness Research Translation Network (CERTAIN) is supported by the Life Discovery Fund of Washington State and the Agency for Healthcare Research and Quality (AHRQ). Dr. Kotagal and Dr. Drake are supported by a University of Washington Department of Surgery T32 training fellowship grant from the National Institute of Diabetes & Digestive & Kidney Diseases (grant number 5T32DK070555-03). The administrative home for the Surgical Care and Outcomes Assessment Program (SCOAP) is the Foundation for Healthcare Quality.
The authors acknowledge Dr. Michael Gravett for his assistance in editing this manuscript.
Footnotes
This paper has not been previously presented. The authors have no disclaimers.
Declaration of interest
The authors report no declarations of interest. There was no source of financial support for this research.
References
- 1.Ito K, Ito H, Whang EE, Tavakkolizadeh A. Appendectomy in pregnancy: evaluation of the risks of a negative appendectomy. Am J Surg. 2012;203:145–50. doi: 10.1016/j.amjsurg.2011.02.010. [DOI] [PubMed] [Google Scholar]
- 2.Walker S, Haun W, Clark J, et al. The value of limited computed tomography with rectal contrast in the diagnosis of acute appendicitis. Am J Surg. 2000;180:450–4. doi: 10.1016/s0002-9610(00)00540-7. [DOI] [PubMed] [Google Scholar]
- 3.Santos DA, Manunga J, Jr, Hohman D, et al. How often does computed tomography change the management of acute appendicitis? Am Surg. 2009;75:918–21. [PubMed] [Google Scholar]
- 4.Long SS, Long C, Lai H, Macura KJ. Imaging strategies for right lower quadrant pain in pregnancy. AJR Am J Roentgenol. 2011;196:4–12. doi: 10.2214/ajr.10.4323. [DOI] [PubMed] [Google Scholar]
- 5.Rosen MP, Ding A, Blake MA, et al. ACR appropriateness criteria right lower quandrant pain – suspected appendicitis. J Am Coll Radiol. 2011;8:749–55. doi: 10.1016/j.jacr.2011.07.010. [DOI] [PubMed] [Google Scholar]
- 6.Lehnert BE, Gross JA, Linnau KF, Moshiri M. Utility of ultrasound for evaluating the appendix during the second and third trimester of pregnancy. Emerg Radiol. 2012;19:293–9. doi: 10.1007/s10140-012-1029-0. [DOI] [PubMed] [Google Scholar]
- 7.Israel GM, Malguria N, McCarthy S, et al. MRI versus ultrasound for suspected appendicitis during pregnancy. J Magn Reson Imaging. 2008;28:428–33. doi: 10.1002/jmri.21456. [DOI] [PubMed] [Google Scholar]
- 8.Cobben LP, Groot I, Haans L, et al. MRI for clinically suspected appendicitis during pregnancy. AJR Am J Roentgenol. 2004;183:671–5. doi: 10.2214/ajr.183.3.1830671. [DOI] [PubMed] [Google Scholar]
- 9.Pedrosa I, Zeikus EA, Levine D, Rofsky NM. MR imaging of acute right lower quadrant pain in pregnant and nonpregnant patients. Radiographics. 2007;27:721–43. doi: 10.1148/rg.273065116. [DOI] [PubMed] [Google Scholar]
- 10.Basaran A, Basaran M. Diagnosis of acute appendicitis during pregnancy: a systematic review. Obstet Gynecol Surv. 2009;64:481–8. doi: 10.1097/OGX.0b013e3181a714bf. [DOI] [PubMed] [Google Scholar]
- 11.Rapp E, Naim F, Kadivar K, et al. Integrating MR imaging into the clinical workup of pregnant patients suspected of having appendicitis is associated with a lower negative laparotomy rate: single-institution study. Radiology. 2013;267:137–44. doi: 10.1148/radiol.12121027. [DOI] [PubMed] [Google Scholar]