Abstract
Background
The Systemic Capillary Leak Syndrome is a highly rare disorder of unknown etiology. The disease is characterized by episodes of transient vascular collapse, which leads to hypotensive shock and anasarca. Previous treatment of this potentially devastating condition has been largely ineffective. We evaluated IVIG prophylactic therapy in a cohort of 29 patients with Systemic Capillary Leak Syndrome in a longitudinal follow up study.
Methods
All patients received treatments at the discretion of their primary providers and retrospectively via questionnaire recorded symptoms beginning with their first documented episode of the Systemic Capillary Leak Syndrome until May 31, 2014.
Results
Twenty-two out of 29 patients responded to the questionnaire, and 18 out of the 22 respondents received monthly prophylaxis with IVIG during the study period for a median interval of 32 months. The median annual attack frequency was 2.6/patient prior to IVIG therapy and 0/patient following initiation of IVIG prophylaxis (P = 0.001). 15 out of 18 subjects with a history of one or more acute Systemic Capillary Leak Syndrome episodes experienced no further symptoms while on IVIG therapy.
Conclusions
IVIG prophylaxis is associated with a dramatic reduction in the occurrence of Systemic Capillary Leak Syndrome attacks in most patients, with minimal side effects.
Keywords: Systemic Capillary Leak Syndrome, intravenous immunoglobulin, vascular leak
A prospective, randomized trial may be necessary to fully assess the benefits of IVIG for the Systemic Capillary Leak Syndrome and to determine optimal dosage and duration of therapy.
First described in 1960 by Clarkson, the Systemic Capillary Leak Syndrome is a rare disorder diagnosed on the basis of unexplained hypotension and edema, which is accompanied by hemoconcentration and hypoproteinemia as a result of the loss of plasma into the extravascular space 1-4. Fewer than 300 cases of the Systemic Capillary Leak Syndrome have been reported since 1960, and the 5-year mortality has been estimated to be 20-35% 2,3.
Owing to disease rarity, prospective therapeutic studies are challenging. In a report by the Mayo Clinic, treatment of eight patients over a period of 18 years with oral theophylline and terbutaline was associated with thirty-fold reduction in the frequency and severity of Systemic Capillary Leak Syndrome episodes 5; however, many patients continued to experience acute attacks, and the regimen was difficult to tolerate. A European registry of 28 patients studied over 15 years demonstrated a significant survival advantage in patients receiving prophylactic therapies (including IVIG or theophylline/terbutaline) compared to untreated subjects 4. Here, we evaluated the efficacy of IVIG as prophylactic therapy in a cohort of patients with the Systemic Capillary Leak Syndrome.
Methods
Study Population and Design
Subjects were included in the study if they were > 16 years of age and met the criteria for the Systemic Capillary Leak Syndrome as described by Gousseff et al. 2011 4. We obtained written informed consent from each patient, and the protocol (09-I-0184) was approved by the Institutional Review Board (IRB) of the NIAID. A voluntary, retrospective questionnaire was approved by the IRB and provided to all adult patients who signed the original study protocol consent.
Data Analysis and Statistics
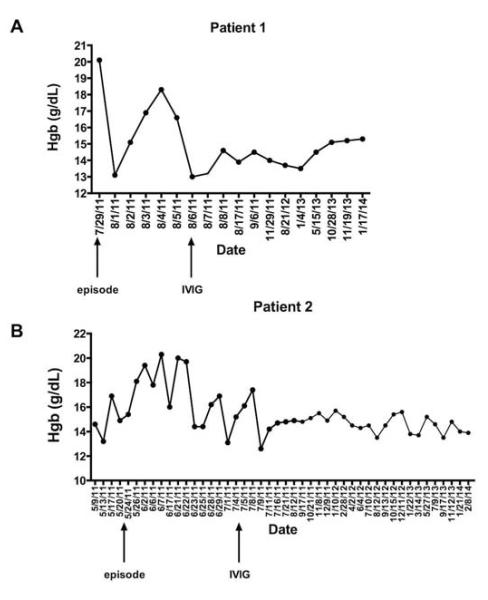
In Figure 1, hemoglobin measurements were obtained by automated analysis (Patient 1) or a HemoCue hemoglobin analyzer photomer (Patient 2). Statistical analysis was performed using GraphPad Prism software. Non-parametric tests (Mann-Whitney for two groups, Kruskal-Wallis for multiple groups) were used; P values < 0.05 were considered significant.
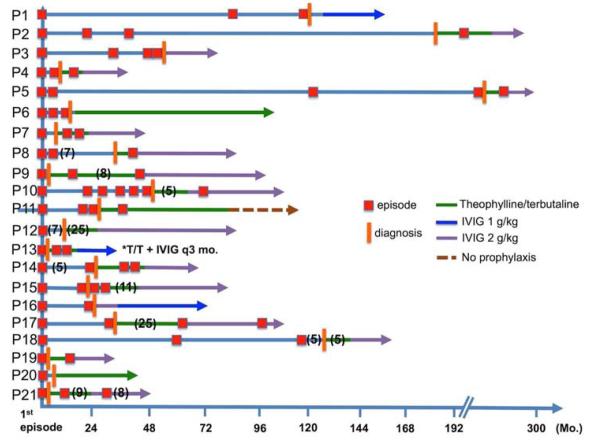
Figure 1.
Longitudinal follow up of 21 adults with classic acute Systemic Capillary Leak Syndrome. Clinical course, date of formal diagnosis of the Systemic Capillary Leak Syndrome, and treatments were recorded following the initial presenting episode over the time periods indicated as denoted by each symbol.
Results
Demographics and disease characteristics
Of 29 adult subjects with classic acute Systemic Capillary Leak Syndrome enrolled in the protocol from 2008 to May 31, 2014, 22 patients completed and returned the questionnaire. One patient with atypical disease features, who experiences near weekly, stereotyped episodes consisting of hypotension but no edema, was excluded from analysis of treatments due to the uncertain diagnosis 6 and incomplete documentation of symptoms. All but two patients are Caucasian (one African American and one of Middle Eastern origin), and 82% are male, which reflects the overall demographics of our cohort (77% male), but is somewhat higher than what is reported in the recent literature 2,3. Although the median age of disease onset was 46 years (range 32-66 years), formal diagnosis was delayed (≥ 2 years after the initial episode) in 41% of patients. Five patients, who are enrolled in in the protocol but receive IVIG, did not return the questionnaire despite repeated follow up and thus were also excluded from the analysis.
The median follow up interval between the date of the first attack and the end of the study in the 21 respondents with stereotypical Systemic Capillary Leak Syndrome was 84 months (range, 29-300 months). The clinical course in relation to the diagnosis and the prophylactic therapy for each subject is presented in Figure 1. Collectively, these patients experienced a total of 195 “significant” episodes of Systemic Capillary Leak Syndrome (defined here as requiring medical attention in a provider’s office, emergency room, and/or hospital admission) during the follow up interval, with a median of six per patient (range, 1-32), and the median annual episode frequency per patient was 1.26 (range, 0.14-4.9). Disease-related complications were common (Table I); by far, compartment syndrome of the extremities occurred most frequently, which required fasciotomies in the majority of cases and resulted in residual neurological damage (neuropathy, contractures, foot drop) in 45% of patients.
Table I.
Complications of Systemic Capillary Leak Syndrome attacks
| Event | Percentage of patients |
|---|---|
| Compartment syndrome/fasciotomies/limb amputation |
50% |
| Sensorimotor neuropathy/foot drop | 33% |
| Renal failure | 14% |
| Thrombosis/pulmonary embolism | 14% |
| Pericardial effusion/tamponade | 9% |
Prophylactic therapy of the Systemic Capillary Leak Syndrome (non-IVIG)
19 out of 21 of the respondents were treated with oral theophylline alone or in combination with a beta-adrenergic agonist (terbutaline or albuterol) following diagnosis for a median interval of 24 months (range, 3-96 months). Two of these subjects remain on this therapy while another has discontinued all prophylactic medications. The median number of attacks/patient in those receiving theophylline as central therapy was 3 (range, 0-26), and the median annual attack frequency over this interval was 3.4/patient (range, 0-15.8). Self-reported side effects of theophylline/beta agonist therapy were common, including anxiety/irritability/mood changes (39%), tremor (28%), and insomnia (33%).
IVIG maintenance therapy
18 subjects commenced monthly maintenance therapy with IVIG (1-2 g/kg/month) during the study period for a median duration of 32 months (range, 10-59). Most (16 out of 18) subjects were treated once monthly while two subjects received half the monthly dose (0.5-1 g/kg) every two weeks. Most patients did not experience significant adverse effects during infusions, and only a minority reported minor post-infusion side effects, with transient headache, rash, fatigue being the most common.
The median annual attack frequency was 2.6/patient (range, 0.25-15.4) from disease onset to initiation of IVIG (median interval of 45 months (range, 10-286). Following IVIG prophylaxis, the median annual frequency of attacks was 0/patient (range, 0-3.3; P < 0.0001). 15 out of 18 subjects did not experience any significant Systemic Capillary Leak Syndrome episodes at all on IVIG treatment. Variable and elevated hemoglobin/hematocrit (Hgb/Hct) values, which are hallmarks of acute Systemic Capillary Leak Syndrome, were noticeably absent for periods of up to three years following initiation of IVIG prophylaxis (Figure 2). IVIG did not have a significant impact on the frequency and severity of episodes in two subjects: one with classic Systemic Capillary Leak Syndrome (included in the analysis) and another with highly atypical disease features as discussed previously 6.
Figure 2.
Hemoglobin measurements in the Systemic Capillary Leak Syndrome (A-B) Hemoglobin (Hgb) was recorded by standard laboratory methods (A) or Hemocue readings (B) in the intervals prior to and following initiation of IVIG prophylaxis in two patients with stereotypical Systemic Capillary Leak Syndrome and frequent episodes.
Discussion
Our results suggest that monthly IVIG prophylaxis is highly successful in preventing acute Systemic Capillary Leak Syndrome flares. IVIG is generally well tolerated and is also associated with a sharp reduction in the frequency of residual symptoms related to the Systemic Capillary Leak Syndrome such as fatigue and limb swelling. Although many of our patients experienced breakthrough severe episodes while receiving other treatments (principally theophylline plus terbutaline), which is consistent with the available literature [4,7-9], our sample size is too small to formally compare the efficacy of the IVIG and theophylline-based regimens.
Previous case reports also demonstrate the effectiveness of IVIG for the Systemic Capillary Leak Syndrome (Table II). Based on clearly documented studies, IVIG (0.4-2 g/kg/month) prophylaxis was associated with an 89% decrease in the number of Systemic Capillary Leak Syndrome flares (252 pre-treatment to 29 post-treatment) in 27 patients for periods of up to thirteen years (median duration of follow up 32 months) [4, 7-12]. 15 out of 27 patients receiving IVIG experienced no Systemic Capillary Leak Syndrome episodes for periods of up to twelve years, and 24 out of 27 subjects had at least a 50% reduction in the number of flares.
Table II.
Use of IVIG for the Systemic Capillary Leak Syndrome in the literature
|
Reference
(#) |
# Pts. |
#Episodes
pre-IVIG (aggregate) |
#Episodes
post IVIG (aggregate) |
IVIG dose |
Longest
duration of follow up (months) |
|---|---|---|---|---|---|
| Lassoued et al 1997 (4) |
1 | 8 | 0 | 0.4 g/kg/mo. | NR |
| Lambert et al. 2008 (4) |
1 | 2 | 0 | 2 g/kg/mo. | 144 |
| Abgueguen et al. 2010 (7) |
1 | 11 | 0 | NR (6 week intervals) |
24 |
| Govig et al. 2011 ( 8) |
1 | 16 | 1 | NR | 23 |
| Pecker et al. 2011 (9) |
2 | 42 | 0 | 2 g/kg/mo. | 20 |
| Gousseff et al. 2011 (4) |
18 | 131 | 32 | 0.4-2 g/kg/mo. |
161 |
| Almagro et al. 2012 (10) |
1 | 29 | 0 | 2 g/kg/6 weeks |
72 |
| Rabbolini et al. 2013 (11) |
1 | 3 | 0 | 2 g/kg/mp. | 18 |
| Marra et al. 2014 (12) |
1 | 3 | 0 | 1-2 g/k/g/mo. |
40 |
not reported
The optimal dose, schedule, and duration of IVIG therapy remain to be determined. While most patients (78%) received 2 g/kg/month, three patients have remained episode-free for greater than two years on 1-1.25 g/kg/month. Further experience with more patients will be necessary to determine whether this lower dose is sufficient to prevent acute Systemic Capillary Leak Syndrome. We can draw no conclusions about the duration of IVIG therapy required to induce remission of the Systemic Capillary Leak Syndrome, or whether a permanent disease remission is possible at all. Although most subjects note rapid diminution of Systemic Capillary Leak Syndrome-related symptoms, none of the subjects in our cohort, who have initiated this therapy and responded favorably, have discontinued it for any reason.
The limitations of the study are the small sample size, its retrospective nature, and reliance on historical data. However, the rarity of the disease, its unpredictable course, and the catastrophic nature of acute Systemic Capillary Leak Syndrome episodes make the prospect of a randomized, placebo-controlled trial unlikely.
Conclusions
Our case series, a European registry, and numerous individual case reports suggest that monthly administration of IVIG is associated with a marked reduction in the number of episodes of hypovolemic shock and edema in patients with classic acute Systemic Capillary Leak Syndrome. These studies indicate that IVIG may be considered as frontline therapy for subjects with a clear-cut diagnosis of the Systemic Capillary Leak Syndrome and recurrent attacks.
Clinical significance.
The Systemic Capillary Leak Syndrome is associated with substantial morbidity, including chronic sensorimotor defects of the extremities.
Theophylline-based therapy of the Systemic Capillary Leak Syndrome was frequently associated with breakthrough symptoms and substantial side effects.
Monthly prophylaxis with high dose intravenous immunoglobulins (IVIG) was associated with a sharp reduction in the number of acute SCLS attacks with few side effects.
Acknowledgements
We thank Laura Wisch and Michael Young for patient care and recruitment and Dr. Helene Rosenberg for reviewing the manuscript.
Funding: This work was supported by the Intramural Research Program of the National Institute of Allergy and Infectious Diseases (NIAID), National Institutes of Health (NIH) (Project AI001830, K.M.D).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest: The authors declare no conflicts of interest.
Authorship: All authors had access to the data and a role in writing the manuscript.
References
- 1.Clarkson B, Thompson D, Horwith M, Luckey EH. Cyclical edema and shock due to increased capillary permeability. Am J Med. 1960 Aug;29:193–216. doi: 10.1016/0002-9343(60)90018-8. [DOI] [PubMed] [Google Scholar]
- 2.Druey KM, Greipp PR. Narrative review: the systemic capillary leak syndrome. Ann Intern Med. 2010 Jul 20;153(2):90–98. doi: 10.1059/0003-4819-153-2-201007200-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kapoor P, Greipp PT, Schaefer EW, et al. Idiopathic systemic capillary leak syndrome (Clarkson’s disease): the Mayo clinic experience. Mayo Clin Proc. 2010 Oct;85(10):905–912. doi: 10.4065/mcp.2010.0159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gousseff M, Arnaud L, Lambert M, et al. The Systemic Capillary Leak Syndrome: A Case Series of 28 Patients From a European Registry. Ann Intern Med. 2011 Apr 5;154(7):464–471. doi: 10.7326/0003-4819-154-7-201104050-00004. [DOI] [PubMed] [Google Scholar]
- 5.Tahirkheli NK, Greipp PR. Treatment of the systemic capillary leak syndrome with terbutaline and theophylline. A case series. Ann Intern Med. 1999 Jun 1;130(11):905–909. doi: 10.7326/0003-4819-130-11-199906010-00015. [DOI] [PubMed] [Google Scholar]
- 6.Xie Z, Ghosh CC, Parikh SM, Druey KM. Mechanistic classification of the systemic capillary leak syndrome: Clarkson disease. Am J Respir Crit Care Med. 2014 May 1;189(9):1145–1147. doi: 10.1164/rccm.201310-1746LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Abgueguen P, Chennebault JM, Pichard E. Immunoglobulins for treatment of systemic capillary leak syndrome. Am J Med. 2010 Jun;123(6):e3–4. doi: 10.1016/j.amjmed.2009.09.034. [DOI] [PubMed] [Google Scholar]
- 8.Govig BA, Javaheri S. The systemic capillary leak syndrome. Ann Intern Med. 2010 Dec 7;153(11):764. doi: 10.7326/0003-4819-153-11-201012070-00014. [DOI] [PubMed] [Google Scholar]
- 9.Pecker M, Adams M, Graham W. The systemic capillary leak syndrome. Ann Intern Med. 2011 Sep 6;155(5):335. doi: 10.7326/0003-4819-155-5-201109060-00016. author reply 335-336. [DOI] [PubMed] [Google Scholar]
- 10.Almagro P, Marti JM, Garcia Pascual L, Rodriguez-Carballeira M. Successful treatment of systemic capillary leak syndrome with intravenous immunoglobulins. Revista clinica espanola. 2012 Apr;212(4):218–219. doi: 10.1016/j.rce.2011.08.004. [DOI] [PubMed] [Google Scholar]
- 11.Rabbolini DJ, Ange N, Walters GD, Pidcock M, Randall KL. Systemic capillary leak syndrome: recognition prevents morbidity and mortality. Internal medicine journal. 2013 Oct;43(10):1145–1147. doi: 10.1111/imj.12271. [DOI] [PubMed] [Google Scholar]
- 12.Marra AM, Gigante A, Rosato E. Intravenous immunoglobulin in systemic capillary leak syndrome: a case report and review of literature. Expert review of clinical immunology. 2014 Mar;10(3):349–352. doi: 10.1586/1744666X.2014.882771. [DOI] [PubMed] [Google Scholar]