Abstract
Objectives
Understanding the dynamics of feeding is essential for preventing accelerated weight gain during infancy, a risk factor for obesity. Because infants satiate on larger volumes of cow milk formula (CMF) than CMF enriched with the free amino acid glutamate (CMF+glu), we used this model system to determine whether infants displayed consistent behaviors despite satiating on lower volumes.
Methods
In this laboratory-based, within-subject experimental study of ≤4-month-old infants (N=41) and their mothers, infants were videotaped while feeding to satiation CMF on one test day and CMF+glu on the other, in counterbalanced order. Each video-recording was analyzed frame-by-frame for frequency and timing of behaviors.
Results
Infants’ behaviors were consistent in types and frequency but were displayed sooner when feeding CMF+glu compared with CMF. The less responsive the mother’s feeding style, the less consistently the infant displayed behaviors across the two formula meals (p=0.05). Infants who spat up (a possible sign of overfeeding) consumed more formula (p=0.01) and had less responsive mothers (p=0.04) compared with the other infants.
Conclusions
Infants are consistent in their behavioral displays during feeding at this developmental age. Regulation of intake and signaling of satiation during bottle-feeding are associated with formula composition and maternal feeding style.
Keywords: infant feeding, formula-feeding, bottle-feeding, satiation signaling, intake regulation, free amino acid, glutamate
INTRODUCTION
Because accelerated weight gain during the first year postpartum increases risks for later obesity, metabolic syndrome, and mortality from cardiovascular disease,1,2 understanding what contributes to the regulation of feeding and growth during early life, and how to measure it, is key. Central to this issue is determining why infants who are fed cow milk formula (CMF, the most common formula consumed by infants in the U.S.) consume more and exhibit faster rates of growth compared with infants fed breast milk3 or an isocaloric, extensive protein hydrolysate formula (ePHF, a type of formula typically fed to infants who have cow milk protein allergy or intolerance to intact protein).4
How (breast vs. bottle) and/or what (breast milk vs. formula) infants are fed are hypothesized factors underlying overfeeding. A recent prospective study revealed that feeding from a bottle was related to accelerated weight gain,5 perhaps because mothers sometimes feed in response to the amount in the bottle rather than feeding responsively to their infants’ cues.6 Maternal feeding styles characterized by low levels of responsiveness to feeding cues may impair their infants’ response to internal cues of hunger and satiation, which may lead to less healthy weight gain trajectories during early life.7–10
However, recent evidence suggests that in addition to the bottle, the composition of formulas (CMF vs ePHF) affects intake and satiation,4,11,12 as well as growth trajectories during the first year of life.4,13 CMF usually includes combinations of intact casein and whey protein and very low levels of free amino acids (FAAs), whereas the milk proteins in ePHF are treated with enzymes to break down their structure to reduce allergenicity resulting in a formula that contains small peptides and many FAAs.14 As a point of reference, breast milk contains substantially higher levels of most FAAs, particularly glutamate, than does CMF,14, and both contain substantially lower levels of most FAAs than do ePHF.14,15
Using an infant-led feeding paradigm, we discovered that infants satiated on smaller volumes of ePHF than on isocaloric CMF4,12 and that levels of the free amino acid glutamate, when added to CMF, were sufficient to account for the intake differences,16 possibly because free glutamate exerts is effect though satiation signaling in the gastrointestinal tract.17 The present study used this model system to objectively determine how and when infants signal satiation, an unexplored research area that is critical to our understanding of contributors to early growth. We aimed to determine: 1) whether the timing, frequency, and types of behaviors displayed differ when the same infants fed isocaloric formulas with differing satiation properties; 2) whether infants are consistent in their display of these behaviors, regardless of how much formula they consume; and 3) the relationship between maternal feeding styles and infant self-regulation of intake and behavioral displays during feeding.
METHODS
Subjects
Subjects were mothers with healthy infants ≤4 months of age who were born term and were exclusively (n=37) or predominantly (>80% of the feeds were formula; n=4) formula feeding but had no prior exposure to ePHF. Mothers were recruited for an infant feeding study of different formulas through ads and Women, Infants, and Children offices; they were unaware of the hypothesis being tested. Some participated in past research using an identical paradigm16 but their video-recordings had not been analyzed. All study procedures were approved by the Office of Regulatory Affairs at the University of Pennsylvania, and informed consent was obtained from each mother at study entry.
Test Formulas
Based on our prior research,16 two isocaloric (68kcal/100ml) formulas were used: CMF (Enfamil; Mead Johnson Nutrition) and CMF with 105mg/100ml added monosodium glutamate (USBioAnalyzed, Cleveland, OH; hereafter referred to as CMF+glu). Levels of free glutamate were 2mg/100ml16 and 84mg/100ml, respectively. The latter was slightly lower than that found in ePHF (107mg/100ml)16 but allowed for similar sodium levels (18–32mg/100ml) and molarities (8–14mM) between the two isocaloric formulas (see also 16). An adult sensory panel found no differences in taste between CMF and CMF+glu.16
Experimental Design
Mother-infant dyads came to the Monell Center at the same time of day on two different days separated by, on average, two days. The within-subject factor was type of formula fed. Infants were videotaped as their mothers fed them, in randomized order, CMF on one test day and CMF+glu on the other. To minimize possible effects due to different levels of hunger, the two testing sessions took place at the same time of day that the infants were typically fed formula.
Procedures
At the beginning of each test session, infants and mothers were weighed and measured after which we determined the infants’ age- and sex-specific percentiles18 and maternal BMI (weight[kg]/height[m2]). We used an infant-led feeding paradigm that controls for a number of factors and allows assessment of infants’ behavioral responses during feeding.4,12 In brief, infants acclimated to the testing room for at least 30 min. When they displayed hunger by exhibiting such behaviors as sucking on hands or fussing, and mothers verified babies were hungry, infants were fed at their customary pace. A video camera was placed 1.75m in front of the dyad, and the experimenter sat behind a partition, out of sight of the dyad. The feeding ended after the infant displayed one or more behavior types listed in Table 1 on at least three consecutive occasions or fell asleep (and did not awaken when the bottle was offered again). Immediately after each test meal, mothers rated how similar the meal was to the infant’s typical formula feeding and how much the infant enjoyed the formula.
Table 1.
Coded behaviors types
| Behavior | Description |
|---|---|
| Waves arm(s) | The infant waves one or both hands/arms but does not make contact with the bottle or mother (contacting the bottle would be considered “pushes bottle away”). |
| Displays negative facial expressions | The infant’s eyes are squinted and/or mouth turned downward. |
| Leans away or arches back | The infant leans away from the bottle and/or arches the back when bottle is offered. |
| Turns head and/or body away from bottle | The infant turns the head sideways or tilts the head back, resulting in detachment from the nipple. |
| Bites or chews nipple | The infant chews or bites (but is not sucking) on the nipple of the bottle. |
| Pushes bottle away | The infant pushes the bottle out of the mouth by hitting the bottle or the mother’s arm with his or her hand. |
| Spits out nipple | The infant actively ejects the nipple from the mouth with the lips or tongue. |
| Gags, coughs, or chokes | The infant gags, coughs, or chokes during active feeding. |
| Spits out formula or spits up | The infant actively ejects the formula from the mouth. |
| Crying bout | The infant emits a cry and displays characteristic facial responses and tears. |
| Sleeping bout | The infant’s eyes are closed. |
Five minutes later, on both testing days, infants were offered a bottle of CMF and allowed to consume this formula ad libitum to determine whether they had satiated during the formula test meals (hereafter referred to as the satiation check). Intake was determined by weighing bottles immediately before and after test meal and satiation check. The length of time that elapsed between initial acceptance of the bottle and display of the last satiation behavior (meal duration) was determined by analysis of the video-recordings. Mothers completed the Infant Feeding Styles Questionnaire,19 from which we focused on the responsive and pressuring feeding subscales, each with possible scores of 0–5.
Video-record analyses
Each video-recording was analyzed frame-by-frame using an event recorder program (Observer XT, version 10.5). Raters (N=3), unaware of the experimental conditions, coded 11 mutually exclusive behavior types (Table 1) in real time, focusing on 1) the first quartile of the meal duration, to determine whether initial acceptance of the two formulas differed, and 2) the second half of the meal duration, to determine whether infants were consistent in their timing and display of behaviors to signal satiation.
We determined the primary outcome measures for each of the 11 coded behaviors, for each infant, and for each meal: 1) frequency of each behavior type during the meal’s (a) first quartile and (b) second half; 2) summed frequency of all behaviors (i.e., number of behaviors) displayed during the meal’s (a) first quartile and (b) second half; 3) number of behavior types (regardless of frequency) during the meal’s (a) first quartile and (b) second half; 4) during the second half of the meal, the type of (a) first behavior and (b) last three behaviors displayed; 5) the time (in minutes) from the initial acceptance of the bottle (start of meal) to the (a) first behavior of the meal and (b) last behavior displayed during the second half; and 6) during the second half of the meal, the time (in minutes) between the first and last behavior displayed. Inter-coder reliability was established by the common scoring of a total of 51 videos by at least two raters. The mean Pearson’s Rho for the scoring of all coded behaviors was ρ(49df)=0.97 and for the duration of the feed was ρ(49df)>0.99, indicating good reliability.
Statistical Analyses
All analyses were conducted using SAS (version 9.3; SAS Institute Inc., Cary, NC). All data were assessed for normality. Distributions for most primary outcome measures were positively skewed and thus were normalized using log or square root transformations. After analysis, data were back-transformed by calculating the antilog or square of the estimate.20 Repeated-measures analyses of variance (ANOVAs) were conducted on primary outcome measures with formula type (CMF, CMF+glu) as the within-subjects factor; time elapsed since the last feeding and infant age was covaried in models that tested the influence of formula type on intake and meal duration. Pearson’s correlations and ANOVAs were conducted to test for associations among infant feeding behaviors and maternal characteristics; we averaged primary outcome measures across the two meals and controlled for time since last feeding. Results are presented as means or least squared means ± standard errors. P-values≤0.05 indicated significant effects.
RESULTS
Sample Characteristics
Mothers (N=41) averaged 27.5±0.9 years of age, and their infants (56% female) averaged 2.2±0.1 months of age. Infants’ average weight-for-length percentile was 58.8±4.7 and mothers’ average BMI was 28.7±1.0 kg/m2. Sixty-one percent of mothers were non-Hispanic black, 20% non-Hispanic white, 15% Hispanic white, 2% Hispanic black, and 2% Asian. The majority (46%) attended or graduated from college, 37% graduated from high school whereas 17% did not complete high school. About 15% reported an annual family income above $75,000; 54% were between $15,000 and $74,999; and 31% were below $15,000. Maternal responsive and pressuring feeding style scores were 4.1±0.1 (range: 2.4–4.9) and 2.2±0.1 (range: 1.2–3.5), respectively.
Feeding and Satiation Behaviors
As shown in Table 2, infants consumed less CMF+glu and tended to feed for shorter periods of time compared with CMF. There were no differences in number of behaviors or behavior types during the first quartile of the meals or amount of formula infants consumed during the satiation check, suggesting that infants were equally accepting of and satiated by both formulas. Mothers reported their infants enjoyed both formulas and the meals were typical for their infants.
We found notable consistency in the behavior types displayed during the second half of the meal but differences in the timing of the behaviors. Analyses of the video-records confirmed that every infant exhibited at least three behaviors (range: 3–35) during the second half of each test meal. The number of behavior types ranged from 2 to 9 per meal. There were no differences in number of behaviors or behavior types between the two meals (Table 2). The greater the number of behaviors and behavior types during the CMF meal, the greater the number of behaviors (r[39]=0.40, p=0.01) and behavior types (r[39]=0.34, p=0.03) during the CMF+glu meal. Further, there were no significant differences between the two meals for frequency of each behavior (all p’s>0.05) or in the amount of time that elapsed between the first and last behaviors displayed during the second half of the meal. However, infants tended to display the first and final behaviors earlier when feeding CMF+glu than when feeding CMF.
Table 2.
Least squares mean (SE) differences for infants’ feeding, behavioral outcomes, and mothers’ perceptions: CMF versus CMF+glu meals (N=41 infants)
| Type of Formula | F-value | ||
|---|---|---|---|
| CMF | CMF+glu | ||
| Infant Feeding: | |||
|
| |||
| Formula Meal: | |||
| Amount consumed (ml) | 170.0 (10.3) | 152.2 (9.0) | 4.45* |
| Meal duration (min) a,b | 10.3 (0.9) | 9.3 (0.6) | 3.36Ŧ |
| Satiation check: | |||
| Amount consumed (ml) | 13.1 (3.6) | 10.4 (2.5) | 0.42 |
|
| |||
| Behavioral Outcomes: | |||
|
| |||
| First quartile of formula meal: | |||
| Number of behaviors a | 1.6 (0.6) | 1.8 (0.5) | 0.92 |
| Number of behavior types a | 1.4 (0.2) | 1.6 (0.2) | 1.55 |
| Second half of formula meal: | |||
| Number of behaviors a,c | 9.5 (1.1) | 9.6 (1.3) | 0.01 |
| Number of behavior types a,d | 4.3 (0.2) | 4.6 (0.3) | 0.80 |
| Latency to first behavior (min) a,e | 6.9 (0.5) | 6.2 (0.4) | 2.78 |
| Latency to last behavior (min) a,b | 10.3 (0.9) | 9.3 (0.6) | 3.36 |
| Time elapsed between first and last behavior (min) a | 3.4 (0.5) | 2.9 (0.3) | 1.43 |
|
| |||
| Maternal Perceptions | |||
|
| |||
| How similar was this feed to your infant’s typical formula feeding? f | 7.3 (0.3) | 7.1 (0.3) | 0.29 |
| How much did your infant like the formula? g | 7.4 (0.3) | 7.1 (0.3) | 1.06 |
p<.05;
p<.10
Note: All analyses were adjusted for time since last fed. Analyses with amount consumed and meal duration were also adjusted for infant age.
Distributions were positively skewed and thus were normalized by log or square root transformations prior to analysis. Data presented are back-transformations.
Defined as length of time elapsed between initial acceptance of the bottle and display of the last satiation behavior for each test meal.
Sample range = 3–35 behaviors
Sample range = 2–9 behavior types
Defined as length of time elapsed between initial acceptance of the bottle and display of the first satiation behavior during the second half of each meal.
Responses range from 1 (not at all similar) to 9 (very similar)
Responses range from 1 (extreme dislike) to 5 (neutral) to 9 (extreme like)
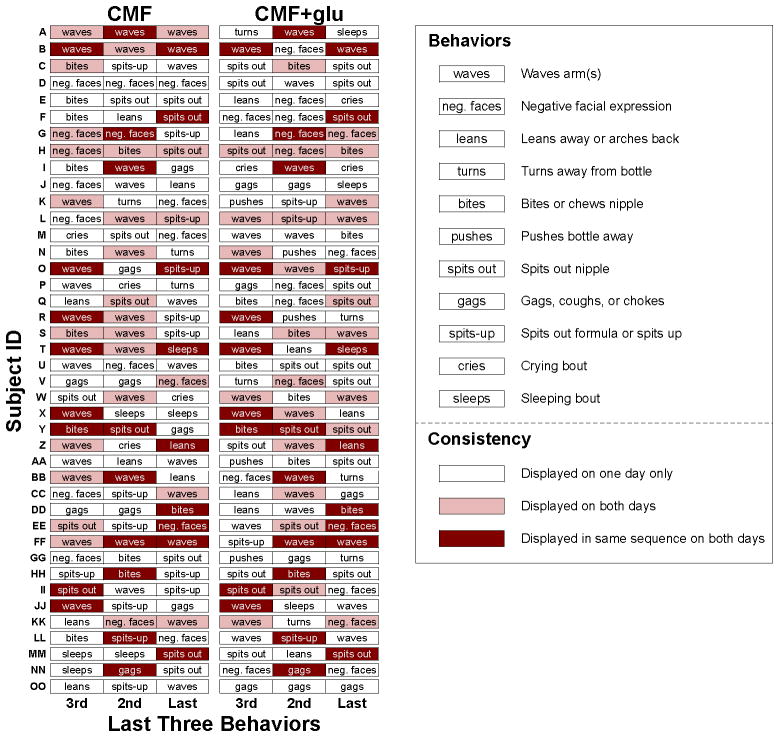
Although the type of formula differed between the meals, significantly greater percentages of infants were consistent than were not consistent across the two meals in their display of all but three behaviors (leans away; pushed bottle away; gags, coughs, chokes) during the second half of the meals (Table S1). On average, infants were consistent in their display of 7.5±0.2 (range: 5–10) of 11 coded behaviors. The greater number of behaviors (p=0.04) and behavior types (p=0.01) displayed the less consistent the infant was in the behaviors displayed across the two meals (Table 3). The final three behaviors displayed had at least one behavior in common for the vast majority of infants (78%), albeit in different order (Figure 1). The most frequent final behaviors were arm waving (22%), spitting out the nipple (21%), and negative facial expressions (15%). Infants were as likely to fall asleep (F[1,40]=0.11, p=0.74) or spit up (F[1,40]=0.13, p=0.72) when feeding CMF as when feeding CMF+glu.
Table 3.
Correlations among infant feeding behaviors and mother characteristics
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
|---|---|---|---|---|---|---|---|
| Infant Feeding Behaviors a | |||||||
| 1. Amount consumed b | |||||||
| 2. Meal duration b | 0.67** | ||||||
| 3. Number of behaviors b,c | 0.25 | 0.20 | |||||
| 4. Number of behavior types b,c | 0.17 | 0.08 | 0.84** | ||||
| 5. Consistency score d | −0.11 | −0.11 | −0.33* | −0.47** | |||
| Mother Characteristics | |||||||
| 6. Age | −0.32* | −0.31* | 0.23 | 0.18 | −0.17 | ||
| 7. Responsive feeding score e | 0.04 | 0.02 | −0.05 | −0.17 | 0.31* | 0.11 | |
| 8. Pressuring feeding score e | 0.15 | 0.28 | 0.08 | −0.04 | −0.03 | −0.35* | 0.14 |
p<.05;
p<.01
All analyses involving infant feeding behaviors were adjusted for time since last feeding.
Averaged across both testing days.
During the second half of the feeding.
Consistency score was calculated by first determining for each individual behavior whether the infant was consistent (i.e., either did or did not exhibit the behavior on both test days) or inconsistent (i.e., exhibited the behavior on only one of the two test days). We then calculated a consistency score for each infant by summing the number of consistent behaviors, ranging from 0 (no consistency for any behavior) to 11 (complete consistency for all behaviors).
From the responsive and pressuring feeding style subscales of the Infant Feeding Styles Questionnaire19
Figure 1. Patterning of the last three behaviors displayed by each individual infant.
Each row represents an individual infant; subject IDs were randomly assigned. The left and right columns display the third to last (3rd), second to last (2nd), and last behaviors during the CMF and CMF+glu meal, respectively. A white cell indicates a behavior that an infant displayed on one day only. A pink cell indicates a behavior that an infant displayed on both days. A maroon cell indicates a behavior that an infant displayed in the same sequence (e.g., as the first behavior) on both days.
Consistent with previous research, pressuring feeding style scores were not significantly associated with responsive feeding style scores;19 however, both were independently related to outcome measures (Table 3). The older the mother, the less formula her infant consumed, the shorter the meal duration, and the lower she scored on pressuring feeding style. The less responsive her feeding style, the less consistent the infant was in his or her behavioral display. Infants who spat up at the end of feeding (n=19), which is a possible sign of overfeeding, consumed significantly more formula (187.1±14.5ml vs. 138.7±10.5ml; F[1,40]=7.56, p=0.01) and had mothers who scored significantly lower in responsive feeding (4.1±0.1 vs 4.4±0.1; F[1,40]=4.66, p=0.04) compared with remaining dyads. There was no association between spitting up and infant weight status.
DISCUSSION
Infants 4 months of age and younger are not passive recipients of formula fed from a bottle. Rather, each exhibits a changing repertoire of behaviors during feeding and, at least during this developmental stage, is consistent in how often and what behaviors are displayed. By testing infants on two separate days and varying only the type of formula in the bottle, we demonstrated that infants satiated on lower volumes of formula and tended to signal satiation sooner when feeding CMF+glu than when feeding CMF. Infants were equally accepting of and satiated by both formulas: the number of behaviors or behavior types that infants displayed during the beginning or end of the feed, the duration of signaling, or how much formula was consumed during the satiation check did not differ between formula meals. Mothers reported their babies enjoyed both formulas. Thus, both our direct, observational measures and mothers’ indirect, subjective reports indicate that infants displayed consistent behaviors across the two different feedings, despite the decreased intake and latency to meal termination during the CMF+glu meal.
Such findings add to a growing body of research showing that formula-fed infants, as a group, can sense and respond to compositional differences in formulas.4,11,16 In the present study, compositional differences in the levels of the FAA glutamate decreased intake, perhaps through its ability to trigger satiation when detected by glutamate receptors in the gastrointestinal tract.17,21 In another study, compositional differences in levels of another amino acid, tryptophan, decreased sleep latency in young infants but did not influence the display or patterning of other behaviors (e.g., orienting to light).22 Taken together, these data suggest that the FAA content of the formula consumed can influence select aspects of behavior.
Our within-subjects design, objective measurement of infant behaviors, and use of an infant-led feeding paradigm allowed us to describe both between- and within-infant variation in the infants’ behavioral display during feeding. In the present study, we objectively measured 11 behavior types, chosen based on prior experimental23 and observational24 research, that characterized some, but not all, of the behaviors that infants of this age exhibit during feeding. We acknowledge that some behaviors might be specific signs of satiation while others (e.g., waving arms, crying) are not specific but, rather, reflect changes in overall arousal or motivation. We found a negative correlation between consistency score and number of behaviors and number of behavior types, which likely resulted from the tendency for infants not to display a behavior on both days: significantly more infants displayed 8 of the 11 coded behaviors consistently (i.e., on neither or on both days) than inconsistently (i.e., on either day but not both), but failure to display was the primary source of consistency for less frequent behaviors.
Which types of behaviors were displayed changed over the course of the feeding: those that may be regarded as more indicative of satiation and rejection of the bottle, such as spitting out the nipple, were more prevalent toward the end. There was wide between-infant variation in the overall number of behaviors displayed and the number of behavior types; some behaviors (e.g., waving) were displayed by most infants, whereas others (e.g., fell asleep) were not. Despite this between-infant variation, there was notable within-infant consistency in the numbers of behaviors and behavior types displayed. For most infants, the last three behaviors during both meals had at least one behavior in common, albeit in different orders, and the majority of infants were consistent in which behaviors they displayed. Why infants were not consistent in the display of some behaviors is unknown. It is possible that some behaviors (e.g., leans away, pushes bottle away) become more consistent with increasing age and motor development, while others (e.g., gagging) are more consistent earlier in infancy. Nonetheless, these findings indicate that infants’ overall behavioral responses may be more a characteristic of the infant and less a reaction to changing environmental stimuli such as the type of formula. We caution that the present study focused on a limited age range, and longitudinal studies would better inform how age, sex, weight status, or feeding transitions influence feeding behaviors over developmental time and how socioeconomic and anthropometric measures of mothers are related to feeding styles and infant outcomes.8,9,25
In the present study, we purposely observed infants within an infant-led feeding paradigm to assess their behavioral responses and intake on repeated occasions independent of the mother and experimenter. In reality, infants’ feeding behaviors and mothers’ feeding practices are intertwined, and at the time of testing the baby brings to the experimental paradigm a history of past experiences and learning. This is supported by the finding that those infants who spat up at the end of feeding consumed significantly more, regardless of the formula type in the bottle, and had mothers who scored lower on responsive feeding. Spitting up is common for infants of this age group, but it may also be a sign of overfeeding26 and inability to regulate intake, possibly as a result of low maternal responsiveness.8 Although the analysis of video-recordings for types and frequency of behaviors that infants use to signal hunger and satiation is laborious, it provides objective measures that current questionnaire-based assessments of infant behavior may not.27,28 Because the study of one member of the dyad in isolation creates an incomplete understanding of formula feeding during infancy,10 research using objective measures of both members of the dyad is needed. Additionally, because free glutamate is abundant in human milk;15 its role in feeding and satiation signaling by breastfed infants is another important question for future research.
Supplementary Material
Percentage (n) of infants who were consistenta versus inconsistentb for behaviors displayed during the second half of the formula meals
What is already known about this subject
Complex issues related to mode of feeding (breast vs. bottle), milk composition, and parents’ feeding practices and styles affect how much infants consume and how fast they grow.
Infants feed more cow milk formula to satiation than a formula with higher levels of free amino acids, such as glutamate, demonstrating that bottle-feeding infants can self-regulate intake in response to formula composition.
Maternal responsiveness to infant cues promotes positive developmental outcomes, such as effective self-regulation of emotional reactivity.
What this study adds
We identified a model system that can be used to objectively study within- and between-infant variation in feeding behaviors, self-regulation of intake, and satiation signaling.
Young infants exhibit a changing repertoire of behaviors during feeding and are consistent in how often and what behaviors they display, despite decreased intake and latency to meal termination when feeding a more versus less satiating formula.
The more responsive the feeding style of the mother, the more consistently the infant displays types of behaviors across two formula meals.
Infants who spat up at the end of the feeding (which may be a sign of overfeeding) consumed significantly more formula and had mothers with significantly lower responsive feedings scores compared with other infants.
Acknowledgments
AKV aided in the design of the study; collected data, analyzed and interpreted data and wrote the manuscript. LBI assisted with data collection and analysis, and revision of the manuscript. JAM conceived and designed the study; analyzed and interpreted data; and wrote the manuscript. All authors approved the final version of the manuscript.
The project described was supported by NIH grants R01HD072307 and R01HD37119, an American Recovery and Reinvestment Act supplement (3R01HD037119-10S1), a National Research Service Award F32HD063343 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development and an investigator-initiated grant from Ajinomoto, Inc. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Eunice Kennedy Shriver National Institute of Child Health and Human Development or the National Institutes of Health. The funding agencies had no role in the design and conduct of the study; in the collection, analysis, and interpretation of the data; or in the preparation, review, or approval of the manuscript.
We thank Dr. Leann Birch for comments on an earlier version of the manuscript; Mariya Keselman, Sehris Khawaja, Jillian Fink, Shawna Comalli, and Nicole Halfin (whose position was created by supplement 3R01HD037119-10S1 received under the ARRA) for technical assistance; Linda Kilby PhD, RD, LDN and the staff at the Philadelphia WIC Program for their assistance with subject recruitment; and Ms. Patricia J. Watson for her valuable editorial assistance.
Abbreviations
- CMF
cow milk formula
- CMF+glu
cow milk formula with added glutamate
- ePHF
extensive protein hydrolysate formula
- FAA
free amino acid
Footnotes
Trial Registry: This trial was registered at clinicaltrials.gov as NCT00957892.
CONFLICTS OF INTEREST STATEMENT
The authors have no conflicts of interest to declare.
References
- 1.Stettler N, Iotova V. Early growth patterns and long-term obesity risk. Curr Opin Clin Nutr Metab Care. 2010;13:294–299. doi: 10.1097/MCO.0b013e328337d7b9. [DOI] [PubMed] [Google Scholar]
- 2.Khuc K, Blanco E, Burrows R, et al. Adolescent metabolic syndrome risk is increased with higher infancy weight gain and decreased with longer breast feeding. Int J Pediatr. 2012;2012:478610. doi: 10.1155/2012/478610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dewey KG, Heinig MJ, Nommsen LA, Peerson JM, Lönnerdal B. Growth of breast-fed and formula-fed infants from 0 to 18 months: the DARLING Study. Pediatrics. 1992;89:1035–1041. [PubMed] [Google Scholar]
- 4.Mennella JA, Ventura AK, Beauchamp GK. Differential growth patterns among healthy infants fed protein hydrolysate or cow-milk formulas. Pediatrics. 2011;127:110–118. doi: 10.1542/peds.2010-1675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li R, Magadia J, Fein SB, Grummer-Strawn LM. Risk of bottle-feeding for rapid weight gain during the first year of life. Arch Pediatr Adolesc Med. 2012;166:431–436. doi: 10.1001/archpediatrics.2011.1665. [DOI] [PubMed] [Google Scholar]
- 6.Crow RA, Fawcett JN, Wright P. Maternal behavior during breast- and bottle-feeding. J Behav Med. 1980;3:259–277. doi: 10.1007/BF00845051. [DOI] [PubMed] [Google Scholar]
- 7.Brown A, Lee MD. Early influences on child satiety-responsiveness: the role of weaning style. Pediatr Obes. 2013 doi: 10.1111/j.2047-6310.2013.00207.x. Epub 2013/12/19. [DOI] [PubMed] [Google Scholar]
- 8.DiSantis KI, Hodges EA, Johnson SL, Fisher JO. The role of responsive feeding in overweight during infancy and toddlerhood: a systematic review. Int J Obes (Lond) 2011;35:480–492. doi: 10.1038/ijo.2011.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Black MM, Aboud FE. Responsive feeding is embedded in a theoretical framework of responsive parenting. J Nutr. 2011;141:490–494. doi: 10.3945/jn.110.129973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hurley KM, Cross MB, Hughes SO. A systematic review of responsive feeding and child obesity in high-income countries. J Nutr. 2011;141:495–501. doi: 10.3945/jn.110.130047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fomon SJ, Filmer LJ, Thomas LN, Anderson TA, Nelson SE. Influence of formula concentration on caloric intake and growth of normal infants. Acta Paediatr Scand. 1975;64:172–181. doi: 10.1111/j.1651-2227.1975.tb03818.x. [DOI] [PubMed] [Google Scholar]
- 12.Mennella JA, Beauchamp GK. Developmental changes in the acceptance of protein hydrolysate formula. J Dev Behav Pediatr. 1996;17:386–391. doi: 10.1097/00004703-199612000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Rzehak P, Sausenthaler S, Koletzko S, et al. Short- and long-term effects of feeding hydrolyzed protein infant formulas on growth at < or = 6 y of age: results from the German Infant Nutritional Intervention Study. Am J Clin Nutr. 2009;89:1846–1856. doi: 10.3945/ajcn.2008.27373. [DOI] [PubMed] [Google Scholar]
- 14.Ventura AK, Gabriel AS, Hirota M, Mennella JA. Free amino acid content in infant formulas. Nutr Food Sci. 2012;42:271–278. [Google Scholar]
- 15.Baldeon ME, Mennella JA, Flores N, Fornasini M, San Gabriel A. Free amino acid content in breast milk of adolescent and adult mothers in Ecuador. Springerplus. 2014;3:104. doi: 10.1186/2193-1801-3-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ventura AK, Beauchamp GK, Mennella JA. Infant regulation of intake: the effect of free glutamate content in infant formulas. Am J Clin Nutr. 2012;95:875–881. doi: 10.3945/ajcn.111.024919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.San Gabriel AM, Maekawa T, Uneyama H, Yoshie S, Torii K. mGluR1 in the fundic glands of rat stomach. FEBS letters. 2007;581:1119–1123. doi: 10.1016/j.febslet.2007.02.016. [DOI] [PubMed] [Google Scholar]
- 18.WHO Child Growth Standards. Length/height-for-age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age: Methods and development. 2006 http://www.who.int/childgrowth/standards/en/
- 19.Thompson AL, Mendez MA, Borja JB, Adair LS, Zimmer CR, Bentley ME. Development and validation of the Infant Feeding Style Questionnaire. Appetite. 2009;53:210–221. doi: 10.1016/j.appet.2009.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bland JM, Altman DG. Transforming data. BMJ. 1996;312:770. doi: 10.1136/bmj.312.7033.770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Niijima A. Reflex effects of oral, gastrointestinal and hepatoportal glutamate sensors on vagal nerve activity. J Nutr. 2000;130:971S–973S. doi: 10.1093/jn/130.4.971S. [DOI] [PubMed] [Google Scholar]
- 22.Steinberg LA, O’Connell NC, Hatch TF, Picciano MF, Birch LL. Tryptophan intake influences infants’ sleep latency. J Nutr. 1992;122:1781–1791. doi: 10.1093/jn/122.9.1781. [DOI] [PubMed] [Google Scholar]
- 23.Mennella JA, Forestell CA, Morgan LK, Beauchamp GK. Early milk feeding influences taste acceptance and liking during infancy. Am J Clin Nutr. 2009;90:780S–788S. doi: 10.3945/ajcn.2009.27462O. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hodges EA, Johnson SL, Hughes SO, Hopkinson JM, Butte NF, Fisher JO. Development of the responsiveness to child feeding cues scale. Appetite. 2013;65:210–219. doi: 10.1016/j.appet.2013.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gibbs BG, Forste R. Socioeconomic status, infant feeding practices and early childhood obesity. Pediatr Obes. 2014;9:135–146. doi: 10.1111/j.2047-6310.2013.00155.x. [DOI] [PubMed] [Google Scholar]
- 26.Bergman NJ. Neonatal stomach volume and physiology suggest feeding at 1-h intervals. Acta Paediatr. 2013;102:773–777. doi: 10.1111/apa.12291. [DOI] [PubMed] [Google Scholar]
- 27.Forestell CA, Mennella JA. More than just a pretty face. The relationship between infant’s temperament, food acceptance, and mothers’ perceptions of their enjoyment of food. Appetite. 2012;58:1136–1142. doi: 10.1016/j.appet.2012.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sacco LM, Bentley ME, Carby-Shields K, Borja JB, Goldman BD. Assessment of infant feeding styles among low-income African-American mothers: comparing reported and observed behaviors. Appetite. 2007;49:131–140. doi: 10.1016/j.appet.2007.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Percentage (n) of infants who were consistenta versus inconsistentb for behaviors displayed during the second half of the formula meals