Summary
Background
Gray matter heterotopia (GMH) is a malformation of the central nervous system characterized by interruption of normal neuroblasts migration between the 7th and 16th week of fetal development.
The aim of the study was the analysis of clinical symptoms, prevalence rate and the most common concurrent central nervous system (CNS) developmental disorders as well as assessment of characteristic morphological changes of gray matter heterotopia in children hospitalized in our institution between the year 2001 and 2012.
Material/Methods
We performed a retrospective analysis of patients’ data who were hospitalized in our institution between the year 2001 and 2012. We assessed clinical data and imaging exams in children diagnosed with gray matter heterotopia confirmed in MRI (magnetic resonance imaging).
Results
GMH occurred in 26 children hospitalized in our institution between the year 2001 and 2012. Among children with gray matter heterotopia most common clinical symptoms were: epilepsy, intellectual disability and hemiparesis.
The commonest location of heterotopic gray matter were fronto-parietal areas of brain parenchyma, mostly subependymal region.
Gray matter heterotopia occurred with other developmental disorders of the central nervous system rather than solely and in most cases it was bilateral.
Schizencephaly and abnormalities of the corpus callosum were the most often developmental disorders accompanying GMH.
Conclusions
1. Subependymal gray matter heterotopia was more common than subcortical GMH. Subependymal GMH showed tendency to localize in the region of the bodies of the lateral ventricles. The least common was laminar GMH. 2. Gray matter heterotopia occurred more often with other developmental disorders of the central nervous system rather than solely. The most frequent concurrent disorders of the central nervous system were: schizencephaly, developmental abnormalities of the corpus callosum, arachnoid cyst, abnormalities of the septum pellucidum and the fornix. 3. GMH foci were more often bilateral than unilateral. 4. In the diagnostics of cell migration abnormalities, gray matter heterotopia included, MR imaging remains the method of choice.
MeSH Keywords: Brain Abscess, Developmental Disabilities, Magnetic Resonance Imaging
Background
Gray matter heterotopia is a central nervous system malformation characterized by interruption of normal neuroblasts migration between the 7th and 16th week of fetal development. The inhibition of neuroblast migration during their movement from germinal matrix to the superficial layers of the cerebrum causes the formation of foci of gray matter located within the cerebrum. Ectopic islands of gray matter can be visible anywhere between the ependymal layer and subcortical layer of the white matter [1]. Neuroblast migration from the periventricular matrix along the primary glial “scaffold” towards the superficial layers of the cerebrum starts from the second month of fetal development. In the beginning neural cells are deposited in the phylogenetically older structures, then in younger structures in the following sequence: in the spinal cord, brain stem, hypothalamus, striatum, cerebellum and pallium of the cerebral hemispheres. Around the fourth month of fetal development, the cerebral gyri and sulci are progressively formed, from the stage of lissencephaly to pachygyri to final formation of full gyri, layers and differentiation of cortical cells that are fully developed a few months after birth. The time of increased metabolic activity in a specific area of the central nervous system involved in migration causes a high sensitivity for a damaging factor. The destruction of glial fibers that are part of the migration leads to immobilization of neuroblasts and their further maturation in deeper structures.
The group of cellular migration disorders is composed of: heterotopias of the gray matter, schizencephaly, porencephaly, lissencephaly, agyria, macrogyria, pachygyria, microgyria, polymicrogyria, agenesis of the corpus callosum, and agenesis of the cranial nerves. These defects can very often coexist with each other.
The risk factors for the development of this disorder can be divided into: genetic and epigenetic.
The epigenetic mechanisms are quite common in the etiology of periventricular heterotopias. They are: hemorrhages, periventricular leukomalacia, hypoxic-ischemic changes, physical and chemical factors, radiation, thermal injuries.
Genetic research allowed to identify a few genes (Table 1) associated with developmental disorders of the cerebral cortex that could disrupt each of the main phases of cellular proliferation, specification, migration of neurons, and later organization of the cerebral cortex [3].
Table 1.
Genetic risk factors of abnormal neuronal migration including gray matter heterotopia.
| Type of heterotopia | Gene mutation | Characteristics |
|---|---|---|
| Paraventricular heterotopia |
|
|
|
|
|
|
| ||
| Subcortical heterotopia |
|
|
|
|
|
Source: Jeffrey A. Golden & Brian N. Harding. (2004). Developmental Neuropathology. The International Society of Neuropathology.
Clinically and morphologically there are three big groups of heterotopias of the gray matter:
Subependymal heterotopia;
Subcortical heterotopias;
Clinical symptoms and the beginning of their occurrence depend on the type of heterotopias and sex:
a. Subependymal heterotopia
In women they appear clinically in the second decade of life as partial seizures. In men they have a different clinical picture depending whether they are inherited in autosomal or allosomal pattern. In men with heterotopias associated with the chromosome X, other diseases of the central nervous system also occur; these patients are usually diagnosed during childhood because of developmental delay. The course of the disease inherited in an autosomal pattern is similar to women with symptomatic heterotopias.
b. Subcortical hetertotopias
Persistent neurological deficits occur in both men and women and they develop partial seizures in the second part of the first decade of their lives. It is believed that the larger the subcortical heterotopias, the bigger the neurological deficits. Bilateral occurrence of the malformation is associated with almost always severe developmental delay and mental retardation.
c. Band heterotopias
There are observed almost exclusively in women; male fetuses with the mutation responsible for the development of the disorder in gene XLIS (DCX) usually die in utero or are born with much more severe defects of the cerebrum [6,7]. The symptoms in women may not appear, may be mild or severe, depending on the thickness of the layers inhibited in the migration of neurons. In patients with GMH, the main symptom leading to a diagnosis is a seizure attack [8–10]. The seizure attacks are characterized as partial or generalized attacks or have atypical presentation with loss of consciousness. Drop attacks are observed in some more severely ill patients.
Heterotopias of the gray matter are often a part of the clinical picture of some congenital syndromes and disorders. Cortical anomalies can be observed in Zellweger’s syndrome, tuberous sclerosis, Walker-Warburg syndrome, Fukuyama muscular dystrophy [5] and many others.
Magnetic Resonance Imaging (MRI) is the method of choice for the evaluation of heterotopic foci of gray matter, especially because of high contrast resolution. The signal from heterotopic foci and plaques of gray matter is uniform with the true gray matter from other parts of the cerebrum. MRI allows to additionally visualize abnormal flow and dilation of veins draining the heterotopic areas and coexistence of pachygyri and polymicrogyria in cases of subcortical heterotopias [2]. Heterotopic foci of gray matter do not undergo contrast enhancement and do not have calcifications. Similar to GMH foci are present in tuberous sclerosis, but they do have calcifications and can express contrast enhancement [1].
The goal of this research was to analyze the clinical symptoms, incidence and most common comorbid developmental deficits of the central nervous system and the evaluation of characteristic morphological patterns of heterotopias of gray matter in children hospitalized in our center between 2001–2012.
Material and Methods
The data of patients hospitalized from 2001 to 2012 was analyzed retrospectively. Clinical data and imaging results were evaluated in children in whom MRI of the cerebrum showed a presence of the heterotopic foci of gray matter. During the analyzed period of time (years 2001–2012) the disorders of cellular migration seen on MRI were present in 104 patients, and the presence of heterotopias of the gray matter was present in 26 of them, the sex profile was equal – 13 cases were among girls and 13 among boys, in the age range between 10 months and 18 year.
MRI imaging was performed using Philips 1.5T ACHIVA with spin echo sequences, T1-weighted images in native resolution in the transverse plane and after contrast medium administration in the transverse, sagittal and frontal plane, and in T2-weighted images in the transverse, sagittal, and frontal plane.
Results
There were no significant deviations in the lab results or imaging studies of children involving other parts of the body besides central nervous system, except for two cases of neurogenic bladder in children after surgery for meningomyelocele (MMC).
Most of the children with heterotopias of the gray matter were born at term (80%), after second and consecutive pregnancies (72%), with birth weight in the range of 2700–3600 g (average 3100 g) and Apgar score 7–10 (average 8).
In the group of patients with heterotopias of the gray matter the most commonly diagnosed clinical symptoms were: seizures (23%), mental delay (27%) and hemiparesis (27%) (Table 2).
Table 2.
The most frequent clinical symptoms in children with GMH.
| Clinical symptoms | Percentage of patients |
|---|---|
| Developmental delay | 27% |
| Hemiparesis | 27% |
| Seizures | 23% |
| Autism and emotional disturbances | 11.5% |
| Disorders of muscular tension | 7% |
| Psychomotor overactivity | 7% |
| Cerebral palsy | 4% |
| Intelectual disability | 4% |
In MRI images the heterotopic areas of the gray matter were most commonly located around the fronto-parietal region (76%), including subcortical nuclei (2%), rarely in the occipital area (19%) or temporal area (5%).
Subependymal heterotopias were more commonly observed (57%) than subcortical heterotopias (43%) and in the case of subependymal heterotopias, interestingly there was a tendency to appear in the areas of the bodies of lateral ventricles (33%) (Figures 1 and 2). The least commonly observed disorders were band heterotopias that existed only in two cases – one for each sex.
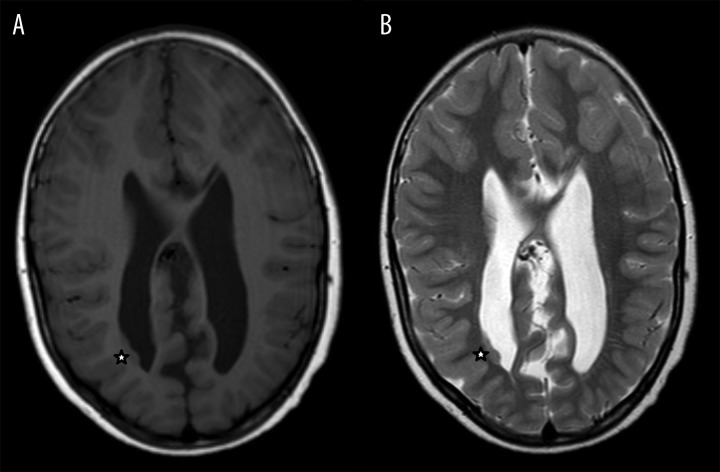
Figure 1.
A 9-year-old boy. (A) Clinical symptoms: psychomotor retardation, epilepsy, headache, hemiparesis (MMC history). MR image. (A) T1-weighted image, axial plane. (B) T2-weighted, axial plane. Heterotopic gray matter in lateral aspect of the right lateral ventricle body, type II Arnold-Chiari malformation (asterisk).
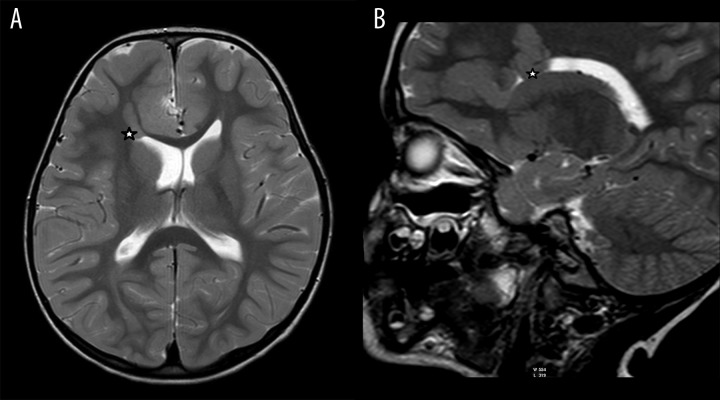
Figure 2.
A 5-year-old boy. Clinical symptoms: retarded speech development. MR image. (A) T2-weighted image, axial plane. (B) T2-weighted image, sagittal plane. Heterotopic gray matter within the white matter of the right cerebral hemisphere and in the subependymal region of the frontal horn of the right lateral ventricle (asterisk).
Heterotopias of the gray matter often existed as disorders associated with other developmental changes of the cerebrum (69%) (Figure 3) than as isolated changes (31%), wherein the most common developmental central nervous system disorders associated with heterotopias were: cerebral fissure (20%), developmental anomalies of the corpus callosum (25%), arachnoid cyst (20%), disorders of the septum pellucidum and the vault (20%) (Table 3). More often (56%) the foci of heterotopias were localized bilaterally.
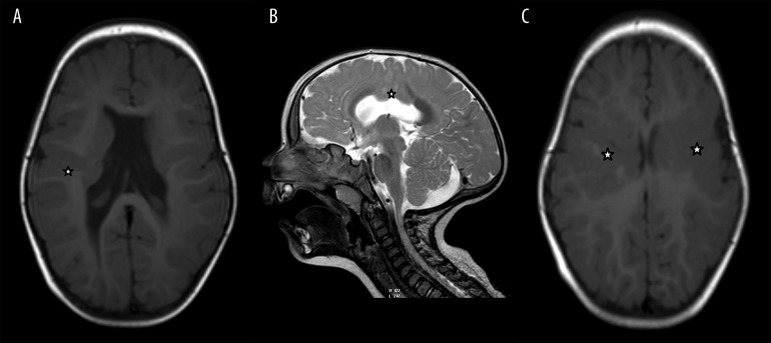
Figure 3.
A 1-year-old boy. Clinical symptoms: psychomotor retardation. MR image. (A). T1-weighted image, axial plane. (B) T2-weighted image, sagittal plane. (C) T1-weighted image, axial plane. Heterotopic gray matter bilaterally in parietal regions (asterisk), pachygyria, agenesis of the septum pellucidum, hypoplasia of the corpus callosum.
Table 3.
Developmental disorders of CNS accompanying GMH.
| Type of disorder | Percentage of patients (%) |
|---|---|
| Anomalies of the development of corpus callosum | 25 |
| Cerebral fissure | 20 |
| Arachnoid cyst | 20 |
| Disorder of the septum pellucidum and the vault | 20 |
| Others | 20 |
| Arnold-Chiari II malformation | 10 |
| Pachygyria | 10 |
| Epidermal cyst of the olfactory groove | 5 |
| Polimicrogyria | 5 |
| Dandy-Walker syndrome | 5 |
| Hippocampal sclerosis | 5 |
Discussion
Heterotopias of the gray matter are relatively rare developmental disorders of the brain, although contributing to the occurrence of seizures, psychomotor retardation and the expression of speech, and thus strongly influencing the future of the child.
Etiology of heterotopias of the gray matter is complex, often multi-factorial, and in order to establish it, there needs to be some data about the course of pregnancy, obstetric history, very often it might be necessary to look at the genetic studies. Despite a wide array of diagnostic possibilities both in the laboratory and imaging studies, the reason for the disease occurrence is still unknown. Unfortunately, also in our evaluation due to difficult access to data about full obstetric and gynecological patient’s history (for example, the data about the course of pregnancy in mothers whose children had heterotopias, obstetric patient’s history) it was impossible to analyze the etiology of heterotopias of the gray matter.
The analysis of available clinical data showed that the majority of children with diagnosed heterotopias of the gray matter is composed of children born at term, after second and consecutive pregnancies, with a mean birth weight of 3100 g and mean Apgar score of 8 whereas the lower number in Apgar score more often appeared in children with heterotopias and other coexisting disorders of the central nervous system (developmental or ischemic changes). Lack of significant deviation in Apgar score in children with isolated heterotopias of the gray matter may result from the fact that in significant majority of cases, the disorders associated with heterotopias such as seizures and psychomotor retardation are observed in later stages of the child’s development.
In the whole group of patients with heterotopias of the gray matter, the most commonly diagnosed clinical symptoms were: seizures, intellectual disability and hemiparesis, also supported in research of the cited authors [6,8,10]. There was a correlation between the type of heterotopias, the size of their foci and the clinical symptoms – subcortical heterotopia was more commonly associated with seizures or seizures associated with psychomotor retardation than subependymal heterotopias. On the other hand, subependymal heterotopia was more commonly associated with isolated disorders of speech and psychomotor retardation. Larger areas of heterotopic gray matter foci seen on imaging studies and the bilateral occurrence were observed in patients with more severe and complex clinical picture. The above observations related to the correlation between the type of heterotopia and the size of its foci with the type and severity of clinical symptoms are consistent with the results published in literature [8,10].
In MRI imaging, the areas of heterotopias of the gray matter were most commonly located in the fronto-parietal areas including the subcortical nuclei and rarely in the occipital and temporal areas.
Subependymal heterotopias were more commonly observed than subcortical heterotopias, and in the case of subependymal heterotopias interestingly there was a tendency to appear in the bodies of the lateral ventricles. Band heterotopias were the least commonly observed type which according to literature occur only in women [6,7] whereas in our study we described two cases, one in each sex.
After analysis of the clinical data and the results of imaging studies performed by other authors there was also more common occurrence of subependymal heterotopias, but their location was related more to the occipital horns of the lateral ventricles [8].
Heterotopias of the gray matter more commonly existed as disorders associated with other developmental changes of the brain than as isolated changes. The most common central nervous system disorders associated with heterotopias were: cerebral fissure, developmental anomalies of the corpus callosum, arachnoid cyst, disorders of the septum pellucidum and the vault. The foci of heterotopias were more commonly located bilaterally - similarly to the results of other authors [8].
Conclusions
Subependymal heterotopias were observed more commonly than subcortical heterotopias, and in the case of subependymal heterotopias there is an interesting tendency to appear in the bodies of the lateral ventricles. Band heterotopias were the least commonly observed changes.
Heterotopias of the gray matter more often coexisted with other developmental changes of the cerebrum than isolated changes, wherein the most common central nervous system changes associated with heterotopias were: cerebral fissure, developmental anomalies of the corpus callosum, arachnoid cyst, disorders of the septum pellucidum and the vault.
The heterotopic foci were more commonly located bilaterally than unilaterally.
In the diagnostics of the cellular migration disorders including heterotopias of the gray matter, the method of choice is MRI (mostly because of its high contrast resolution), but the imaging studies allowing to confirm or rule out the presence of developmental disorders of the central nervous system or other deviations in clinical picture should be performed in all children with neurological disorders or psychomotor retardation.
References
- 1.Lempert TE, Gaemsler EHL. Neuroradiologia pediatryczna. In: Brant WE, Helms CA, editors. Podstawy diagnostyki radiologicznej. Medipage; Warszawa: 2007. pp. 235–65. [in Polish] [Google Scholar]
- 2.Sikorska J, Kluczewska E. Zaburzenia rozwojowe OUN. In: Walecki J, editor. Postępy neuroradiologii. Polska Fundacja Upowszechniania Nauki; Warszawa: 2007. pp. 169–223. [in Polish] [Google Scholar]
- 3.Barkovich AJ, Guerrini R, Battaglia G. Band heterotopia: correlation of outcome with MR imaging parameters. Ann Neurol. 1994;36(4):609–17. doi: 10.1002/ana.410360409. [DOI] [PubMed] [Google Scholar]
- 4.Guerrini R, Marini C. Genetic malformations of cortical development. Exp Brain Res. 2006;173(2):322–33. doi: 10.1007/s00221-006-0501-z. [DOI] [PubMed] [Google Scholar]
- 5.Barkovich AJ, Jackson DE, Jr, Boyer RS. Band heterotopias: a newly recognized neuronal migration anomaly. Radiology. 1989;171(2):455–58. doi: 10.1148/radiology.171.2.2468173. [DOI] [PubMed] [Google Scholar]
- 6.Barkovich AJ, Guerrini R, Battaglia G, et al. Band heterotopia: correlation of outcome with MR imaging parameters. Ann Neurol. 1994;57:609–17. doi: 10.1002/ana.410360409. [DOI] [PubMed] [Google Scholar]
- 7.Ono J, Mano T, Andermann E, et al. Band heterotopia or double cortex in a male: bridging structures suggest abnormality of the radial glial guide system. Neurology. 1997;48:1701–3. doi: 10.1212/wnl.48.6.1701. [DOI] [PubMed] [Google Scholar]
- 8.Raymond AA, Fish DR, Stevens JM, et al. Subependymal heterotopia: a distinct neuronal migration disorder associated with epilepsy. J Neurol Neurosurg Psychiatry. 1994;57:1195–202. doi: 10.1136/jnnp.57.10.1195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Smith AS, Weinstein MA, Quencer RM, et al. Association of heterotopic gray matter with seizures: MR imaging. Radiology. 1988;168:195–98. doi: 10.1148/radiology.168.1.3132731. [DOI] [PubMed] [Google Scholar]
- 10.Barkovich AJ, Kjos BO. Gray matter hereotopias: MR characteristics and correlation with developmental and neurological manifestations. Radiology. 1992;182:493–99. doi: 10.1148/radiology.182.2.1732969. [DOI] [PubMed] [Google Scholar]