An 82-year-old female with a history of situs inversus totalis visited our hospital with complaints of abdominal pain and fever for 2 days. She had history of diabetes mellitus, cerebral infarction, and Alzheimer’s disease, and underwent Billroth-ll (B-II) gastrectomy due to stomach cancer 15 years previously. General appearance was acute ill looking and there was tenderness on right upper quadrant of abdomen. Laboratory findings were as follows: white blood cell, 22,120/mm3; total bilirubin, 3.63 mg/dL; direct bilirubin, 3.57 mg/dL; aspartate aminotransferase, 625 IU/L; alanine aminotransferase, 629 IU/L; alkaline phosphatase, 2,132 IU/L; and γ-glutamyl transpeptidase, 363 IU/L. An abdominal computed tomography scan revealed transposition of the visceral organs from the right to left side and a stone in the dilated common bile duct (CBD) (Fig. 1). Endoscopic retrograde cholangiopancreatography (ERCP) was performed with a cap-assisted forward-viewing endoscope (Olympus, Tokyo, Japan) in patient with gastrojejunostomy (Fig. 2). A cholangiogram revealed transposition of the pancreatic duct oriented to the right side and the gallbladder and dilated CBD with a floating stone to the left side (Fig. 3). After biliary cannulation using catheter with a straight end at the 7 o’clock direction of major papilla, a guidewire was placed across the ampullary orifice (Fig. 4). Following endoscopic papillary balloon dilatation (EPBD) using a controlled radial expansion balloon (10 mm; Boston Scientific Microvasive, Cork, Ireland), a CBD stone was successfully retrieved using a basket (Fig. 5).
Fig. 1.

Abdominal computed tomography scan (coronal view) showing situs inversus totalis and a bile duct stone (white arrow) and multiple gall bladder stones.
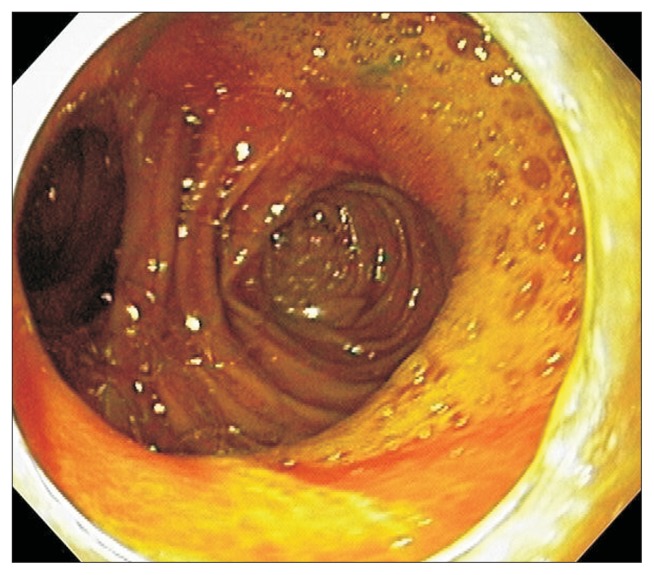
Fig. 2.
A cap-fitted forward-viewing endoscope demonstrating Billroth-II gastrectomy with gastrojejunostomy status.
Fig. 3.
A cholangiogram of endoscopic retrograde cholangiopancreatography demonstrating transposition of pancreatic duct oriented to the right side and gallbladder and dilated common bile duct with a movable filling defect to the left side.
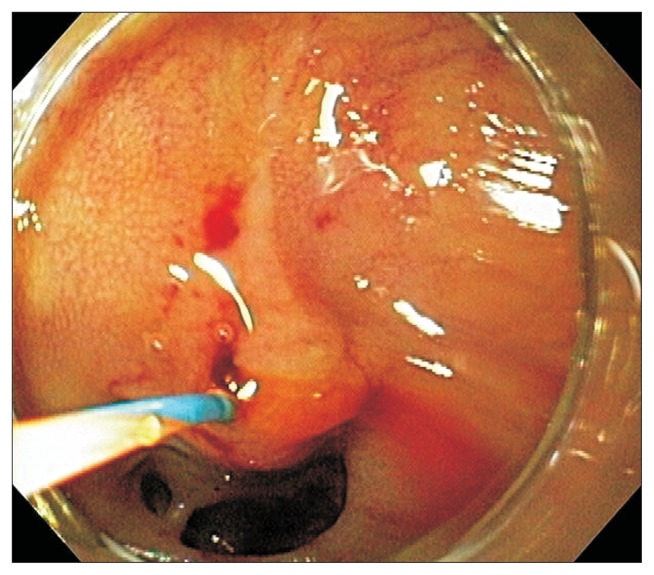
Fig. 4.
A cap-fitted forward-viewing endoscope showing guide wire placed in orifice of bile duct at 7 o’clock position.
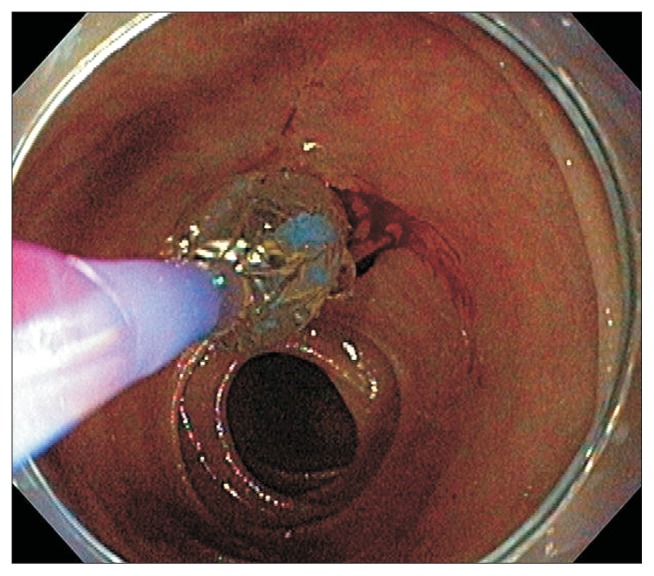
Fig. 5.
A complete stone removal using endoscopic papillary balloon dilatation.
Although a few cases of modified ERCP techniques in situs inversus have been reported,1–5 this is the first report of ERCP in situs inversus totalis combined with B-II gastrectomy. Comparing ERCP using conventional duodenoscope in situs inversus totalis, access to the major papilla with forward-viewing endoscope in situs inversus with B-ll gastrectomy status seems to be technically safer and easier. In this case, neither a patient nor an endoscopist require any positional change during ERCP. Our case demonstrates that CBD stone removal by EPBD can be safely performed, even in a case of B-II gastrectomy combined with situs inversus totalis.
Footnotes
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
REFERENCES
- 1.Çoban Ş, Yüksel I, Küçükazman M, Başar Ö. Successful ERCP in a patient with situs inversus. Endoscopy. 2014;46(Suppl 1):UCTN:E222. doi: 10.1055/s-0034-1365289. [DOI] [PubMed] [Google Scholar]
- 2.Fiocca F, Donatelli G, Ceci V, et al. ERCP in total situs viscerum inversus. Case Rep Gastroenterol. 2008;2:116–120. doi: 10.1159/000119713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.García-Fernández FJ, Infantes JM, Torres Y, Mendoza FJ, Alcazar FJ. ERCP in complete situs inversus viscerum using a “mirror image” technique. Endoscopy. 2010;42(Suppl 2):E316–E317. doi: 10.1055/s-0030-1255813. [DOI] [PubMed] [Google Scholar]
- 4.Patel KS, Patel JN, Mathur S, Moshenyat Y. To twist or not to twist: a case of ERCP in situs inversus totalis. Endoscopy. 2014;46(Suppl 1):UCTN:E304–E305. doi: 10.1055/s-0034-1377213. [DOI] [PubMed] [Google Scholar]
- 5.Sheikh I, Heard R, Tombazzi C. Technical factors related to endoscopic retrograde cholangiopancreatography in patients with situs inversus. Gastroenterol Hepatol (N Y) 2014;10:277–278. [PMC free article] [PubMed] [Google Scholar]