Abstract
Background and Objectives:
Laparoscopic preperitoneal hernia repair with mesh has been reported to result in improved patient outcomes. However, there are few published data on the use of a totally extraperitoneal (TEP) approach. The purpose of this study was to present our experience and evaluate early outcomes of TEP inguinal hernia repair with self-adhesive mesh.
Methods:
This cohort study was a retrospective review of patients who underwent laparoscopic TEP inguinal hernial repair from April 4, 2010, through July 22, 2014. Data assessed were age, sex, body mass index (BMI), hernia repair indications, hernia type, pain, paresthesia, occurrence (bilateral or unilateral), recurrence, and patient satisfaction. Descriptive and regression analyses were performed.
Results:
Six hundred forty patients underwent laparoscopic preperitoneal hernia surgery with self-adhesive mesh. The average age was 56 years, nearly all were men (95.8%), and the mean BMI was 26.2 kg/m2. Cases involved primary hernia more frequently than recurrent hernia (94% vs 6%; P < .05). After surgery, 92% of the patients reported no more than minimal pain, <1% reported paresthesia, and 0.2% had early recurrence. There were 7 conversions to an open procedure. The patients had no adverse reactions to anesthesia and no bladder injury. Postoperative acute pain or recurrence was not explained by demographics, BMI, or preoperative pain. There were significant associations of hernia side, recurrence, occurrence, and sex with composite end points. Nearly all patients (98%) were satisfied with the outcome.
Conclusion:
The use of self-adhesive, Velcro-type mesh in laparoscopic TEP inguinal hernia repair is associated with reduced pain; low rates of early recurrence, infection, and hematoma; and improved patient satisfaction.
Keywords: Laparoscopic hernia surgery, Original research, Self-adhesive mesh, Totally extraperitoneal
INTRODUCTION
The incidence of inguinal hernia continues to increase, with 500,000 new inguinal hernias diagnosed annually.1 The most recent data available show that approximately 800,000 inguinal hernia operations, not including bilateral or recurrent repair, were performed in 2003.2 Inguinal hernia repair is one of the cornerstones of general surgery practice, and in some practices, the most commonly performed elective procedure. Because the procedure is common, surgeons continue to look for innovative ways to improve outcomes. Several open techniques are still being used, and many surgeons believe that those are the most appropriate techniques for hernia repair in general.3
The most commonly used open techniques include herniotomy (in children) and the Bassini, Shouldice, McVay, and Lichtenstein methods. Increasingly, both physicians and patients prefer minimally invasive inguinal hernia repair to open procedures,4,5 most likely because of the association of laparoscopic operations with decreased pain,6 quicker return to work,6 better cosmesis,4 less inflammation, lower rates of infection,7 and higher rates of overall satisfaction.4 It has been estimated that 15% to 20% of inguinal hernia surgeries in the United States are repaired using a laparoscopic technique.3 Tension-free repair has become the gold standard for inguinal hernias because of lower recurrence rates and improved patient comfort.8 The two common variations of laparoscopic inguinal hernia repair are the transabdominal preperitoneal (TAPP) and the total extraperitoneal (TEP) approaches.3 Of the two, TEP is the preferred approach because TAPP, which involves entry through the abdomen into the peritoneal cavity, has been shown to have more postsurgical complications.9
As minimally invasive inguinal hernia repair becomes more common, the surgical community now debates the utility of mesh fixation versus nonfixation.10,11 The type of mesh that has been used most often is a smooth polyester or polypropylene mesh, which may move or slide if not secured.12 Fixation of mesh with tacks, screws, or clips has led to numerous postoperative complications, including bowel obstruction, vascular injury, and migration into the bladder.13,14 More commonly, fixation devices are strongly implicated as a cause of postherniorrhaphy pain and chronic inguinodynia (inguinal pain).3,13 Glues, such as cyanoacrylate and fibrin tissue glue, have also been proposed as viable alternatives to the more standard tissue-disrupting fixation method. However, glues have limitations ranging from concerns over cytotoxicity to increased cost.3,13
Self-adhesive meshes are a relatively new advancement in inguinal hernia repair. They have been on the market since 2006 and have been used in both open and laparoscopic operations.15 Their use eliminates the complication risk, increased operation time, and expense that come with the mechanical fixation of implanted mesh. The popularity and increased use of self-adhesive mesh have been attributed to growing evidence of low rates of recurrence and postsurgical pain.3 A recent meta-analysis comparing ProGrip (self-adhesive) mesh (Covidien, North Haven, CT, USA) to suture mesh revealed that self-adhesive mesh outcomes are equivalent to those obtained with suture mesh in open inguinal hernia repair.16
Based on these considerations, many surgeons regard the use of mesh in inguinal hernia repair as beneficial, and advances in this area will benefit the field. However, there are limited published data on the use of self-adhesive mesh during TEP hernia repair.12 We wanted to investigate this specific question, and thus, the purpose of this study was to present our experience and evaluate early outcomes of patients who had undergone TEP inguinal hernia repair with self-adhesive mesh.
METHODS
Data Collection and Analysis
Institutional review board approval was obtained. Patients for the study were identified by staff from the surgical group's database by using laparoscopic hernia repair, Parietex ProGrip Mesh, preperitoneal inguinal hernia repair, and total extraperitoneal as search terms. For this retrospective study, data were collected for all patients who underwent elective TEP laparoscopic inguinal hernia repair with Parietex ProGrip mesh from April 4, 2010, through July 22, 2014. Patients were further screened by using the International Classification of Diseases, Ninth Version, code 550.90 (550.92 in recurrent hernia repairs) and the Current Procedural Terminology code 49650 for inguinal hernia repair. All cases were elective, same-day, outpatient surgery. Emergent cases, minors (age, <18 years), and patients who had not undergone TEP with ProGrip mesh were excluded from the study. The only absolute contraindication for this procedure was a high suspicion of strangulated hernia.17 Relative contraindications include lack of fitness for general anesthesia because of comorbidities (ie, severe chronic obstructive pulmonary disease or severe coronary arterial disease), pregnancy, and a history of lower abdominal surgery.
Preoperative, intraoperative, and postoperative variables were recorded. Patient variables included demographics, body mass index (BMI), indication for hernia repair, surgical approach, type of hernia, conversion from laparoscopic surgery to open, and complications. The average operation time from incision to closure was calculated. A routine follow-up appointment was defined as a clinic appointment scheduled 2 weeks after the operation. Outcomes assessed included postoperative complications (infection, hematoma, notable perioperative pain, paresthesia, numbness, and early recurrence), hospital length of stay, time to return to work, and patient satisfaction. The primary end point was a composite score, which was the sum of events, including early recurrence, conversion, infection, paresthesia, postoperative pain, and mortality.
Details of the Operative Technique
1. All patients received cefazolin as a preoperative prophylactic antibiotic. The patients were under general anesthesia during the entire surgery. All patients were catheterized to empty the bladder before the abdomen was prepped and draped.
Entrance Into the Preperitoneal Space
2. A 2-cm transverse infraumbilical skin incision was made, and dissection was carried down to identify the anterior rectus sheath, which was then penetrated.
3. A finger was placed just below the anterior rectus sheath which was penetrated and passed inferiorly, staying above the rectus muscle.
4. The Spacemaker Dissection Balloon (Covidien) was inserted through a port, followed by the camera. Under direct visualization with a 10-mm laparoscope, the balloon was distended to expose the preperitoneal space.
5. The blunt-tip balloon was inserted in the same plane and connected to the CO2 supply, and the preperitoneal space was distended, allowing visualization of all anatomic landmarks: the inferior epigastric vessels, Cooper's ligament, Poupart's ligament, the pubic symphysis, and the lateral abdominal wall.
6. Two working 5-mm ports were inserted distal to the distended balloon in the midline. The spermatic cord, with the vas deferens medially and testicular vessels laterally, was identified. The hernia sac was then visualized, identified as direct or indirect, and reduced.
Dissection Steps
7. The sac was dissected completely and mobilized posteriorly until the psoas muscle was identified.
8. The bed was prepared before mesh placement. The abdominal wall was exposed laterally, the psoas muscle posteriorly, and Cooper's ligament medially.
Mesh Placement
9. A previously rolled 3.5 × 6-inch portion of ProGrip mesh was placed through the camera port directed toward the lateral abdominal wall.
10. The mesh was opened with the polylactic acid microgrip Velcro surface facing the tissue. Brief steady pressure was applied by the surgeon to allow self-fixation while the mesh was unrolled. The mesh was affixed to the anterior abdominal wall, medial to the midline, covering the direct defect. The surgeon then proceeded to open the entire mesh to cover the internal ring, femoral ring, and touch the psoas muscle posteriorly.
11. Most important, the surgeon ensured adherence of the mesh to the psoas muscle, to prevent the hernia sac from slipping beneath the mesh, which would have caused a recurrence.
Statistical Analysis
Descriptive statistical analysis was performed with SPSS, version 16 (SPSS Inc., Chicago, IL, USA) statistical software. Continuous variables are presented as the mean ± standard deviation. Proportions are presented as percentages. The χ2 test was used for categorical variables, and logistic regression was used to analyze data with dichotomous outcomes. P < .05 was statistically significant.
RESULTS
Patient Characteristics and TEP Hernia Operation Variables
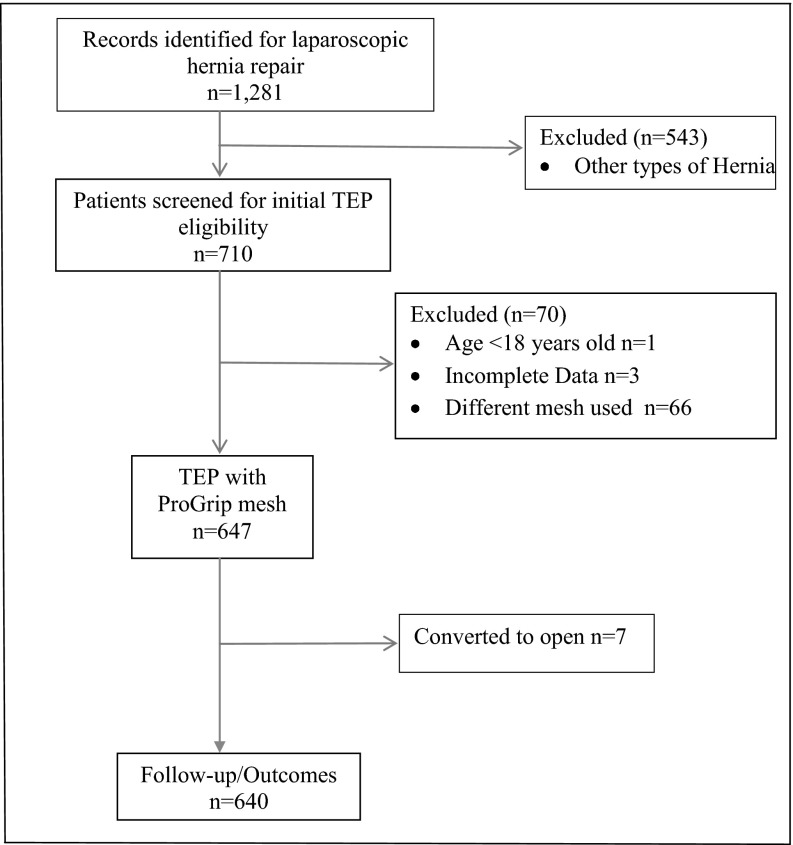
The initial database search identified 1281 patients for laparoscopic hernia repair from April 4, 2010, through July 22, 2014, of which 543 were excluded because they had undergone other types of hernia repair (Figure 1). Seven hundred ten patients were screened for TEP eligibility, and 70 were excluded because they had undergone TEP with Marlex mesh (Phillips Petroleum Co., Bartlesville, OK, USA), were under the age of 18, or had incomplete data. Further review excluded 7 patients because of conversion to open during surgery due to severe adhesions, an irreducible hernia sac, or a densely attached rectus sheath. Thus, 640 patients who underwent TEP hernia repair with ProGrip self-adhesive mesh were analyzed. The patient variables are presented in Table 1. Average age was 56 years (±16; range, 19–92). There were 613 (95.8%) male and 27 (4.2%) female patients. The percentage of obese patients (BMI ≥ 30) in the study was 24.4%, and 75.6% were not obese (BMI <30). The mean BMI was 26.2 kg/m2 (±4.2). There were 94 patients with direct hernia, 462 with indirect hernia, and 84 with a combination of direct and indirect hernias. Of those, 440 patients had unilateral and 200 had bilateral hernias. Thirty-nine patients had recurrent hernia. The more frequent indication for repair was primary hernia (601; 93.9%) compared to recurrent hernia (39; 6.1%). There were no deaths, bladder injury, or adverse reactions to anesthesia. Average operation time from incision to closure was 43.9 minutes (±17; range, 20–90). All patients were discharged the same day and were scheduled for a 2-week follow-up.
Figure 1.
Cohort study flow diagram showing patient selection and exclusion criteria and the number of patients included in the study analysis.
Table 1.
Preoperative and Intraoperative Variables
| Variable | Patients |
|---|---|
| Demographics | |
| Gender | |
| Male | 613 (95.8) |
| Female | 27 (4.2) |
| Mean Age (years) | 56 (±16) |
| Mean BMI (kg/m2) | 26.2 (±4.2) |
| Ethnicity (n = 499) | |
| Caucasian | 475 (95.2) |
| African American | 2 (0.4) |
| Hispanic | 11 (2.2) |
| Asian | 3 (0.6) |
| Native American | 1 (0.2) |
| Other | 7 (1.4) |
| Insurance (n = 636) | |
| Medicare | 29 (4.6) |
| Medicaid | 22 (3.5) |
| Commercial | 583 (91.7) |
| None | 2 (0.6) |
| Pre-existing conditions | |
| Medical history (n = 639) | |
| Hypertension | 65 (10.2) |
| COPD | 3 (0.5) |
| Stroke | 3 (0.5) |
| Diabetes | 11 (1.7) |
| CHF | 1 (0.2) |
| MI | 5 (0.8) |
| Other | 429 (67.1) |
| None | 122 (19.1) |
| Surgical history (n = 635) | |
| Hernia | 42 (6.6) |
| Abdominal | 21 (3.3) |
| Other | 52 (8.2) |
| None | 520 (81.9) |
| Indication for hernia | |
| Symptomatic pain | 550 (86) |
| Bulge | 90 (14) |
| Type of inguinal hernia | |
| Direct | 94 (14.7) |
| Indirect | 462 (72.2) |
| Direct and indirect | 84 (13.1) |
| Occurrence | |
| Unilateral | 440 (68.8) |
| Bilateral | 200 (31.2) |
| Side | |
| Left | 163 (25.5) |
| Right | 186 (29.1) |
| Both | 291 (45.4) |
| Recurrent hernia | 39 (6.1) |
| Operation time (min) | 43.9 (±17) |
n = 640. Characteristics of patients who underwent TEP inguinal hernia repair with self-adhesive, Velcro-type ProGrip mesh (Covidien, North Haven, CT, USA). Unless otherwise specified, data are the number of patients, with the percentage of the study sample in parentheses. Group sizes for categories that are less than the total sample are shown. The remaining categories include the total group.
Abbreviations: CHF, congestive heart failure; COPD, chronic obstructive pulmonary disease; MI, myocardial infarction; TEP, totally extraperitoneal.
TEP Outcome Variables
We describe TEP surgical outcomes and their prevalence in the study group. Four patients (0.6%) in the study reported paresthesia. Early recurrence was reported by 1 patient (0.2%), who had recurrence within 2 weeks caused by slippage of the mesh and underwent reoperation. Eight patients (1.2%) had a surgical wound infection. Seventeen had hematoma; of those, 2 underwent drainage at 2 weeks, 19 were treated expectantly, and 2 underwent drainage later. At the 2-week follow-up, most of the patients (92.2%) reported no more than minimal pain, whereas 7.8% had notable pain that was managed conservatively with oral analgesics. The various surgical outcomes are listed in Table 2.
Table 2.
Surgical Outcomes
| Variable | Patients |
|---|---|
| Conversion to opena | 7 (1.1) |
| Mean length of stay (days) | 1 |
| Hematoma | 17 (2.7) |
| Infection | 8 (1.2) |
| Notable pain | 50 (7.8) |
| Numbness (burning/prickling sensation) | 1 (0.2) |
| Paresthesia | 4 (0.6) |
| Recurrence | 1 (0.2) |
| Satisfied with outcome | 631 (98.6%) |
n = 640, unless otherwise specified. Data are for hernia procedure outcomes in patients treated with TEP inguinal hernia repair with self-adhesive, Velcro-type ProGrip mesh. Unless otherwise specified, data are the number of patients, with the percentage of the study sample in parentheses.
n = 647.
Relationship Between Patient Variables and TEP Outcomes
Binary logistic regression analysis was performed to determine the relationship between the patient variables and composite score end points. The composite end point was dichotomized: no complications versus ≥1 complication. We found that age, ethnicity, BMI, and type of insurance were not associated with composite score. Recurrent hernia, unilateral versus bilateral hernia, and anatomic side were associated with composite score. Compared with the left-side hernia group, patients who had right-side hernia were 1.54 times more likely to have 1 or more complications (composite end point), but the difference was not statically significant. However, when unilateral occurrence was used as the reference point, patients who had bilateral hernia were 2.8 times more likely to have 1 or more complications (95% CI 1.39–5.80; P < .004).
DISCUSSION
The laparoscopic TAPP approach was first used in 1982 and was modified in the early 1990s.18,19 Its rapid rise in popularity worldwide was tempered by increased postoperative complications—especially nerve and vascular injuries. With the increasing trend toward laparoscopic repair of inguinal hernia, few studies, either retrospective or prospective, have reported the efficacy of TEP repair with ProGrip mesh. The present study represents a large private practice group's experience in patients with inguinal hernia who underwent this procedure. The principal finding of the study is that the TEP approach is safe and effective.
The cases showed no mortality and a low early recurrence rate. Comparison of complications such as nerve damage, small bowel obstruction, bladder injury, vascular injury, chronic pain, and hernia recurrence in both open and laparoscopic inguinal hernia repair with fixation are well chronicled.20–22 ProGrip is a polyester mesh with a top layer of resorbable polylactic acid microgrips that integrates into the tissue, providing an alternative to mesh fixation complications in both open and laparoscopic inguinal hernia repair. Furthermore, the anticipated challenge in obtaining the technical skill (increased learning curve for TEP compared with that for Lichtenstein and TAPP)23 needed for the TEP method did not result in a significant increase in complication rates. We agree in our surgical practice that the learning curve for TEP is longer than that needed for TAPP and open inguinal hernia repair.9,23 As reported by others, once the TEP method was mastered, the learning curve for the placement of ProGrip mesh was reduced considerably.12 The mean operative time in our study was 43.9 minutes. Erbella and Erbella12 retrospectively reviewed 116 patients who underwent TEP repair. In their study, there was one case of conversion to open due to adhesion, with operation time from incision to closure ranging from 17 to 80 minutes. The results of our study compare favorably with theirs.
The surgical appeal of the laparoscopic TEP approach is the low rate of postoperative pain and a faster return to work.23 It is the ideal method for inspection of bilateral or recurrent hernia cases.24 The repair is much more durable than that of open approaches (recurrence range, 6.2%–10%).20 In our study we recorded a recurrence rate of 0.6%. In the surgical literature, the major downsides of laparoscopic hernia repair are reported to be the increased risk of specific complications, including vascular injury, nerve injury, and migration of mesh; the necessity for mesh fixation with clips or screws; and increased operative time.25 The ProGrip self-adhesive mesh is engineered to avoid glue or fixation complications. It provides an alternative to mesh fixation, thereby eliminating possible glue or hardware complications with no increase in the recurrence rate.26 The findings in our study contribute to the growing body of knowledge that mesh can be used effectively most of the time without tacking, suturing, or fixation by other devices. In our experience, deployment of self-adhesive mesh did not require additional time compared to fixation of nongripping meshes.
We chose ProGrip mesh to circumvent mesh migration, which can result in early recurrence. ProGrip is a lightweight (38 g/m2), macroporous (1.1 × 1.7 mm), polyester mesh with resorbable polylactic acid microgrips. Its hydrophilic, macroporous, polyester monofilament features enhance fast and durable tissue ingrowth.27 Also its characteristic stickiness offers the crucial advantage that it can adhere to the psoas muscle posteriorly and the peritoneum cannot slip beneath the mesh, which is one of the principal causes of early recurrence.
The follow-up period in this study was 2 weeks; mesh migration usually appears as an early recurrence, as in the case of 1 patient in this series. Morrison and Jacobs28 examined recurrence at 1, 3, and 52 weeks after surgery. Only one patient had recurrence at 1 week, with no additional recurrence in the 3- and 52-week follow-ups. Another study, however, showed no recurrence at 2 weeks, 1 month, and 1 year after surgery.29 Koch et al26 reported that nonfixation (self-adhesive) mesh was not associated with an increased recurrence rate, postoperative complications, or increased cost. Messaris et al29 reported that general laparoscopic surgeons using the TEP approach can obtain improved patient outcomes with less pain, low recurrence rates, and a low prevalence of chronic pain. These results are not limited to specialized hernia centers but appear to be consistent with the observations described in our study.
The study is limited in that it is retrospective, without a long-term follow-up. The typical long-term follow-up after inguinal hernia repair is from 2.5 to 5 years.30 Our evaluation of the short-term recurrence rate is a measure of the surgeon's technical skill, which may be a proxy indicator for long-term effectiveness of the repair, since a poorly performed surgical repair with short-term recurrence is unlikely to have a favorable outcome 2 to 3 years after the surgery. However, the studies referenced in this paper demonstrate that recurrence with the TEP procedure occurs early, with no additional recurrence during long-term follow-up. In routine surgical practice, these procedures are performed as elective outpatient surgeries, and most patients have a 2-week follow-up. Our patients were counseled before and after surgery by one of our authors (C.J.S.), who is a nurse practitioner. At their 2-week follow-up, the patients were given instructions by the nurse to return as needed with any problems, such as hematoma, infection, numbness, paresthesia, pain, seroma, or any recurrent or new bulge. We purport that our outcome would have been the same if we had observed the patients up to a year or longer. We did not perform a head-to-head comparison of ProGrip mesh to other meshes in our study. In a limited study comparing ProGrip and polypropylene mesh in 60 patients, there was no statistically significant difference between the two meshes in recurrence, vessel injury, hematoma, infection, and complications from anesthesia. However, patients with ProGrip hernia repair returned to daily activities earlier than those having polypropylene repair (4 days vs 20 days).27
CONCLUSION
In our recent single-practice experience using ProGrip mesh, we conclude that the use of self-adhesive, Velcro-type mesh in laparoscopic TEP hernia repair is associated with reduced pain, low rates of early recurrence, infection, hematoma, and improved patient satisfaction. In our experience, laparoscopic TEP with ProGrip mesh is safe and effective. This study lays the foundation for prospective and long-term follow-up studies that could include application of innovative technologies such as single-port TEP in hernia repair.
Acknowledgments
The authors thank Dipesh Solanky, Michael-Owen Panzarella and Chester Hayes III, MS, PA-C, for assistance.
Contributor Information
Alicia Mangram, John C. Lincoln North Mountain Hospital, Phoenix, Arizona..
Olakunle F. Oguntodu, Valley Surgical Clinics, Ltd, Phoenix, Arizona..
Francisco Rodriguez, Valley Surgical Clinics, Ltd, Phoenix, Arizona..
Roozbeh Rassadi, Valley Surgical Clinics, Ltd, Phoenix, Arizona..
Michael Haley, John C. Lincoln North Mountain Hospital, Phoenix, Arizona..
Cynthia J. Shively, Valley Surgical Clinics, Ltd, Phoenix, Arizona..
James K. Dzandu, John C. Lincoln North Mountain Hospital, Phoenix, Arizona..
References:
- 1. Everhart JE, ed. Digestive diseases in the United States: epidemiology and impact. U.S. Department of Health and Human Services, Public Health Service, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases. Washington, DC: U.S. Government Printing Office, 1994; NIH publication no. 94-1447. [Google Scholar]
- 2. Rutkow IM. Demographic and socioeconomic aspects of hernia in the United States in 2003. Surg Clin North Am. 2003;83:1045. [DOI] [PubMed] [Google Scholar]
- 3. Mathavan VK, Arregui ME. Fixation versus no fixation in laparoscopic TEP and TAPP. The SAGES Manual of Hernia Repair. New York: Springer, 2013;203–212. [Google Scholar]
- 4. Lauscher JC, Yafaei K, Buhr HJ, Ritz JP. Laparoscopic and open inguinal hernia repair with alloplastic material: do the subjective and objective parameters differ in the long-term course? Surg Laparosc Endosc Percutan Tech. 2008;18:457–463. [DOI] [PubMed] [Google Scholar]
- 5. Kuhry E, Veen RN, Langeveld HR, Steyerberg EW, Jeekel J, Bonjer HJ. Open or endoscopic total extraperitoneal inguinal hernia repair?—a systematic review. Surg Endosc. 2007;21:161–166. [DOI] [PubMed] [Google Scholar]
- 6. Andersson B, Hallen M, Bergenfelz A, Westerdahl J. Laparoscopic extraperitoneal inguinal hernia repair versus open mesh repair: a prospective randomized controlled trial. Surgery. 2003;133:464–472. [DOI] [PubMed] [Google Scholar]
- 7. Park A, Birch DW, Lovrics P. Laparoscopic and open incisional hernia repair: a comparison study. Surgery. 1998;124:816–822. [DOI] [PubMed] [Google Scholar]
- 8. Amid PK, Shalman AG, Lichtenstein IL. Open “tension-free” repair of inguinal hernias: the Lichtenstein technique. Eur J Surg. 1996;162:447–453. [PubMed] [Google Scholar]
- 9. Kald A, Anderburg B, Smedh K, Kalsson M. Transperitoneal or totally extraperitoneal approach in laparoscopic hernia repair: results of 491 consecutive herniorrhaphies. Surg Laparosc Endosc. 1997;7:86–89. [PubMed] [Google Scholar]
- 10. Beattie GC, Kumar S, Nixon SJ. Laparoscopic total extraperitoneal hernia repair: mesh fixation is unnecessary. J Laparoendosc Adv Surg Tech. 2000;10:71–73. [DOI] [PubMed] [Google Scholar]
- 11. Garg P, Rajagopal M, Varghese V, Ismail M. Laparoscopic total extraperitoneal inguinal hernia repair with nonfixation of the mesh for 1,692 hernias. Surg Endosc. 2009;23:1241–1245. [DOI] [PubMed] [Google Scholar]
- 12. Erbella J, Erbella A. Laparoscopic extraperitoneal inguinal hernia repair using a novel mesh with self-fixating properties. Surg Sci. 2013;4:289–291. [Google Scholar]
- 13. Kaul A, Hutfless S, Le H, et al. Staple versus fibrin glue fixation in laparoscopic total extraperitoneal repair of inguinal hernia: a systematic review and meta-analysis. Surg Endosc. 2012;26:1269–1278. [DOI] [PubMed] [Google Scholar]
- 14. Fitzgerald HL, Orenstein SB, Novitsky YW. Small bowel obstruction owing to displaced spiral tack after laparoscopic TAPP inguinal hernia repair. Surg Laparosc Endosc Percutan Tech. 2010;20:E132–E135. [DOI] [PubMed] [Google Scholar]
- 15. Birk D, Hess S, Garcia-Pardo C. Low recurrence rate and low chronic pain associated with inguinal hernia repair by laparoscopic placement of Parietex ProGrip(TM) Mesh: clinical outcomes of 220 hernias with mean follow-up at 23 months. Hernia. 2013;17:313–320. [DOI] [PubMed] [Google Scholar]
- 16. Zhixue F, Jianping Z, Feng R, Dongcai L. Self-gripping mesh versus sutured mesh in open inguinal hernia repair: system review and meta-analysis. Am J Surg. 2014;207:773–781. [DOI] [PubMed] [Google Scholar]
- 17. Chowbey PK, Khullar R, Sharma A, Soni V, Baijal M. Total extraperitoneal repair of inguinal hernia: SGRH technique. J Minim Access Surg. 2006;2:160–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ger R. The management of certain abdominal hernia by intra-abdominal closure of the neck of the sac. Ann R Coll Surg Engl. 1982;64:242–244. [PMC free article] [PubMed] [Google Scholar]
- 19. Read R. Crucial steps in the evolution of the preperitoneal approaches to the groin: an historical review. Hernia. 2011;15:1–5. [DOI] [PubMed] [Google Scholar]
- 20. Junsheng L, Zhenling J, Yinxiang L. Comparison of laparoscopic versus open procedure in the treatment of recurrent inguinal hernia: a meta-analysis of the results. Am J Surg. 2014;207:602–612. [DOI] [PubMed] [Google Scholar]
- 21. Sajid MS, Kalra L, Parampalli U, Sains PS, Baig MK. A systematic review and meta-analysis evaluating the effectiveness of lightweight mesh against heavyweight mesh in influencing the incidence of chronic groin pain following laparoscopic inguinal hernia repair. Am J Surg. 2013;205:726–736. [DOI] [PubMed] [Google Scholar]
- 22. Voyles CR, Hamilton BJ, Johnson DW, Kano N. Meta-analysis of laparoscopic inguinal hernia trials favor open hernia repair with preperitoneal mesh prosthesis. Am J Surg. 2002;184:6–10. [DOI] [PubMed] [Google Scholar]
- 23. Liem MS, Van Steensel CJ, Boelhouwer RU, et al. The learning curve for totally extraperitoneal laparoscopic inguinal hernia repair. Am J Surg 1996;171:281–285. [DOI] [PubMed] [Google Scholar]
- 24. Kozol R, Lange PM, Kosir M, et al. A prospective, randomized study of open vs laparoscopic inguinal hernia repair: an assessment of postoperative pain. Arch Surg. 1997;132:292–295. [DOI] [PubMed] [Google Scholar]
- 25. Lal P, Kaijla RK, Chandler J, Saha R, Ramteke VK. Randomized controlled study of laparoscopic total extraperitoneal versus open Lichtenstein inguinal hernia repair. Surg Endosc. 2003;17:850–856. [DOI] [PubMed] [Google Scholar]
- 26. Koch CA, Greenlee SM, Larson DR, Harrington JR. Randomized prospective study of totally extraperitoneal inguinal hernia repair: fixation versus no fixation of mesh. JSLS. 2006;10:457–460. [PMC free article] [PubMed] [Google Scholar]
- 27. Cobb WS, Kercher KW, Heniford BT. The argument for lightweight polypropylene mesh in hernia repair. Surg Innov. 2005;12:63–69. [DOI] [PubMed] [Google Scholar]
- 28. Morrison JE, Jacobs VR. Laparoscopic preperitoneal inguinal hernia repair using preformed polyester mesh without fixation: prospective study with 1-year follow-up results in a rural setting. Surg Laparosc Endosc Percutan Tech. 2008;18:33–39. [DOI] [PubMed] [Google Scholar]
- 29. Messaris E, Nicastri G, Dudrick SJ. Total extraperitoneal laparoscopic inguinal hernia repair without mesh fixation. Arch Surg. 2010;145:334–338. [DOI] [PubMed] [Google Scholar]
- 30. Nielson M, Kehlet H. Re-recurrence after operation for recurrent inguinal hernia; a nationwide 8-year follow-up study on the role of type of repair Ann Surg. 2008;247:707–711. [DOI] [PubMed] [Google Scholar]