Introduction
Medical management (MM) with antiplatelet (AP) and statin therapy is recommended for most patients undergoing vascular surgery. We evaluated the preoperative use of these on postoperative myocardial infarction (MI) in patients undergoing high-risk procedures within the Vascular Quality Initiative (VQI).
Methods
We studied VQI patients undergoing elective suprainguinal (n = 3039) and infrainguinal bypass (n = 8323) and open abdominal aortic aneurysm repair (n = 3007) from 2005 to 2014. We examined the use of MM (AP or statin, or both) on postoperative MI and postoperative death. Multivariable analyses were performed to identify factors associated with preoperative MM use as well as and MI and MI/death rates across procedures and cardiac risk strata (using Vascular Study Group of New England cardiac risk criteria).
Results
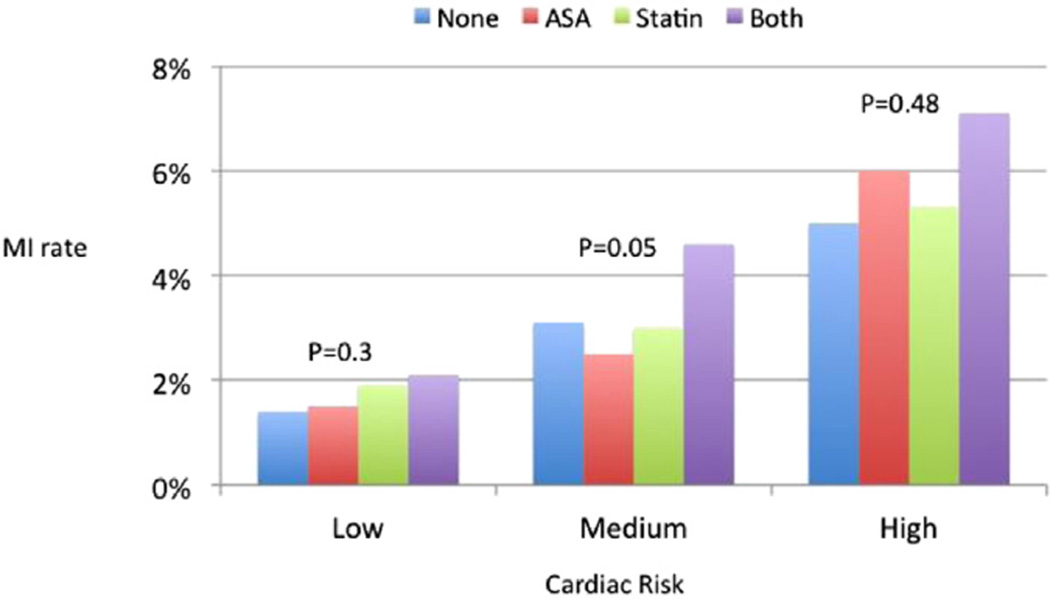
Overall, most patients were on both AP and statin at the time of surgery (56% vs 12% neither agent, 19% AP only, 17% statin only), and MM was similar across procedure groups. Rates of MI were similar despite MM strategy, with slightly higher rates in patients on both agents (neither AP or statin, 2.4%; AP only, 2.6%; statin only, 2.8%; both, 3.7%; P = .003). MI increased with cardiac risk (1.8% vs 3.8% vs 6.5% for low, medium, and high risk; P < .01). When MI was stratified by cardiac risk, MM did not reduce MI rates and was slightly higher for patients on both agents (Fig). After multivariable adjustment for MI, MM was not associated with reduced MI compared with those on neither medication (AP only: odds ratio [OR], 1.0; 95% confidence interval [CI], 0.6–1.5; statin only: OR, 0.9; 95% CI, 0.5–1.4; both agents, OR, 1.0; 95% CI, 0.7–1.5; P > .05 for all). Findings were similar for combined outcome of MI/death. Finally, analysis demonstrated that APs and statins were used more often in patients with known cardiovascular risk factors.
Fig.
Rates of myocardial infarction (MI) by treatment with antiplatelet and statin medications across cardiac risk. ASA, Acetylsalicylic acid.
Conclusions
These data confirm that MI events are highly associated with a patient’s estimated cardiac risk. However, lack of MM did not result in higher rates of MI. It appears that higher-risk patients are currently selected for MM in VQI but that this is not associated with reduced postoperative MI or MI-related mortality.
Footnotes
Author Disclosures: R. R. DeMartino: None; A. W. Hoel: None; A. W. Beck: None; J. W. Hallett: None; S. Arya: None; G.H. Upchurch: None; J. L. Cronenwett: None; P. P. Goodney: None.