Abstract
Uniportal video-assisted thoracoscopic surgery (VATS) has recently been introduced as an acceptable alternative to the traditional three-port VATS. Uniportal VATS lobectomy and segmentectomy actually gained increasing popularity. Until now there have been few reports about uniportal VATS basilar segmentectomy; we herein reported our experience with a patient who suffered from recurrent hemoptysis with 1-cm nodule in the basilar segment of the left lower lobe. A left basilar segmentectomy was performed through a single port. Operating time was 90 minutes, and postoperative course was uneventful. Pathology revealed cryptococcosis. Follow-up at 6 months after surgery demonstrated a normal chest computed tomographic (CT) scan and complete recovery without complications.
Keywords: Lobectomy, segmentectomy, wedge resection, postoperative complications, surgery/incisions/exposure/techniques, thoracoscopy/video-assisted thoracoscopic surgery (VATS)
Introduction
Uniportal video-assisted thoracoscopic surgery (VATS) has recently been introduced as an alternative to the traditional three-port VATS. Uniportal VATS lobectomy and segmentectomy actually gained increasing popularity (1-4). Until now there have been few reports about uniportal VATS basilar segmentectomy. Herein we reported our experience with a patient who suffered from recurrent hemoptysis with a 1-cm nodule in the basilar segment of the left lower lobe, and received VATS basilar segmentectomy of the left lower lobe through a single port.
Clinical summary
A 48-year-old male patient was referred to our department because of recurrent hemoptysis for 3 months, refractory to medications. Past history and physical examination were unremarkable. Chest computed tomographic (CT) scan revealed a poorly demarcated nodule with a diameter of 1 cm (Figure 1); a low-grade malignancy could not be excluded. Bronchoscopy did not show visible lesions. Pulmonary function tests and other systemic examinations were unremarkable. The patient underwent a left basilar segmentectomy through a single port. Postoperative pathologic examination revealed cryptococcosis. He was well at 6-month follow-up, and chest CT scan revealed excellent healing without any complications.
Figure 1.
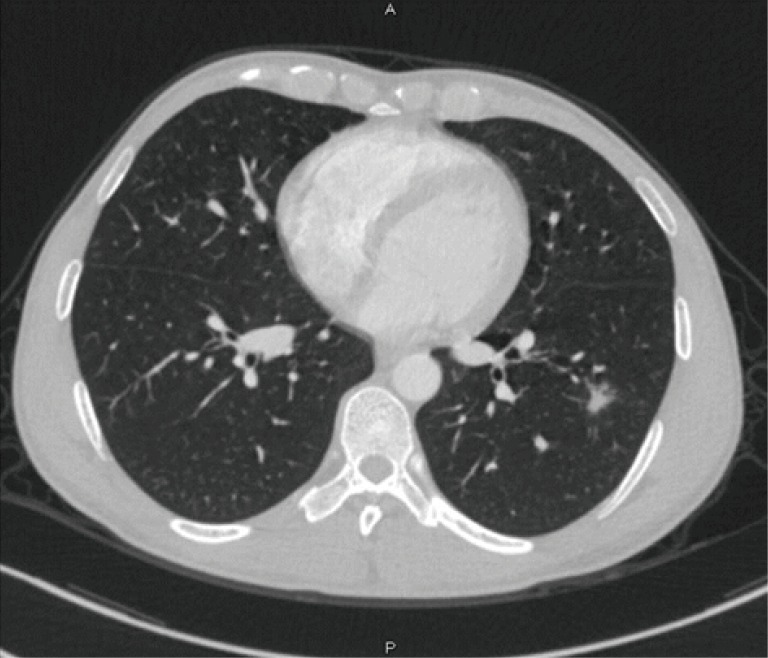
Chest CT scan showed one 1-cm spiculated nodule in the basilar segment of the left lower lobe. CT, computed tomographic.
Surgical technique (Figure 2)
Figure 2.

Uniportal VATS basilar segmentectomy of the left lower lobe (5). Available online: http://www.asvide.com/articles/400
In December 2013, a 4-cm incision was made in the fourth intercostal anterior axillary line, after achievement of general anesthesia with a double-lumen endobronchial tube. After placement of a wound protector, a 30-degree video scope provided visualization. There were no pleural adhesions and no evidence of pleural metastasis in the left thoracic cavity. The nodule was located by palpation in the basilar segment of the left lower lobe, and marked with electrocautery. We first opened the oblique fissure to isolate the superior and basilar branches of the lower lobe artery, and transected the basilar branches using 3-cm EndoGIA linear white stapler (Covidien, Mansfield, MA, USA). The basilar bronchus of the left lower lobe was mobilized, and several station 11 lymph nodes were dissected. After division of inferior pulmonary ligament, basilar tributary of the inferior pulmonary vein was isolated and divided with 3-cm white stapler, sparing the superior tributary. Then, the basilar bronchus was divided with 4.5-cm green stapler. After inflating the residual superior segment of the lower lobe to demarcate the intersegmental plane, the basilar segment was divided along the plane, and removed in a specimen bag, sent for frozen section, which confirmed a benign lesion. Two chest tubes were routinely placed in the chest (Figure 3). Operation time was 90 minutes, and operative blood loss 50 mL. After an uncomplicated recovery, the patient was discharged home 3 days after operation (Figure 4).
Figure 3.

Chest X-ray examination showed the left lung was fully expanded and two chest tubes properly positioned.
Figure 4.

Postoperative examinations revealed satisfactory healing of the chest incision.
Discussion
Operative uniportal VATS is an interesting approach to malignant and benign lung diseases, with both a diagnostic and therapeutic intention, especially in patients with borderline cardiorespiratory function or advanced age. According to our clinical experiences, uniportal VATS patients had a shorter hospital stay and generated lower postoperative costs and a better aesthetic result than conventional VATS, and the technique might suffice for most situations treated by conventional VATS. Herein we reported our experience with a uniportal VATS left basilar segmentectomy of the left lower lobe.
Uniportal VATS segmentectomy is technically demanding operation whose difficulties are compounded by the inherent disadvantages of VATS though single port, including the limited maneuverability, unsatisfactory ergonomic characteristic of the instruments, poor visualization, and instrument-videothoracoscope interference. The placement of the incision in the fourth intercostal anterior axillary line depends on the location of the nodule in the chest, bearing in mind that an adequate distance between the single port and the target area. During the surgical procedure, it was easier to divide the basilar artery and vein branches firstly, which provided enough space to pass the straight anvil of an endoscopic stapler for division of the bronchus. Finally, because we sometimes find one of these tubes being obstructed, we routinely place two chest tubes through the same incision as video shows, to provide best chest drainage, with one tube directing upward for removal of air, the other downward for evacuation of fluid.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- 1.Gonzalez-Rivas D, Fernandez R, Fieira E, et al. Uniportal video-assisted thoracoscopic bronchial sleeve lobectomy: first report. J Thorac Cardiovasc Surg 2013;145:1676-7. [DOI] [PubMed] [Google Scholar]
- 2.Gonzalez-Rivas D, Paradela M, Fernandez R, et al. Uniportal video-assisted thoracoscopic lobectomy: two years of experience. Ann Thorac Surg 2013;95:426-32. [DOI] [PubMed] [Google Scholar]
- 3.Gonzalez-Rivas D, Fieira E, Mendez L, et al. Single-port video-assisted thoracoscopic anatomic segmentectomy and right upper lobectomy. Eur J Cardiothorac Surg 2012;42:e169-71. [DOI] [PubMed] [Google Scholar]
- 4.Gonzalez-Rivas D, Fieira E, Delgado M, et al. Uniportal video-assisted thoracoscopic lobectomy. J Thorac Dis 2013;5:S234-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jiang L, Bao Y, Liu M, et al. Uniportal VATS basilar segmentectomy of the left lower lobe. Asvide 2014;1:366. Available online: http://www.asvide.com/articles/400


