Abstract
Background/Objectives:
Mother's body mass index (BMI) is a strong predictor of child BMI. Whether mother's BMI correlates with child's food intake is unclear. We investigated associations between mother's BMI/overweight and child's food intake using data from two German birth cohorts.
Subjects/Methods:
Food intakes from 3230 participants were derived from parent-completed food frequency questionnaires. Intakes of 11 food groups were categorized into three levels using group- and sex-specific tertile cutoffs. Mother's BMI and overweight were calculated on the basis of questionnaire data. Multinomial regression models assessed associations between a child's food intake and mother's BMI/overweight. Linear regression models assessed associations between a child's total energy intake and mother's BMI. Models were adjusted for study region, maternal education, child's age, sex, pubertal status and energy intake and the BMIs of the child and father.
Results:
Mothers' BMI was associated with high meat intake in children (adjusted relative risk ratio (RRR (95% confidence interval))=1.06 (1.03; 1.09)). Mothers' overweight was associated with the meat intake (medium versus low RRR=1.30 (1.07; 1.59); high versus low RRR=1.50 (1.19; 1.89)) and egg intake (medium versus low RRR=1.24 (1.02; 1.50); high versus low RRR=1.30 (1.07; 1.60)) of children. There were no consistent associations for rest of the food groups. For every one-unit increase in mothers' BMI, the total energy intake in children increased by 9.2 kcal (3.7; 14.7). However, this effect was not significant after adjusting for children's BMI.
Conclusions:
Our results suggest that mother's BMI and mother's overweight are important correlates of a child's intake of energy, meat and eggs.
Introduction
Obesity is a major public health concern.1 According to the 2010 International Obesity Task Force analysis, ~200 million school-aged children are overweight or obese around the world.2 Childhood obesity often persists into adulthood and is associated with increased adult morbidities.3
Parental body mass indices (BMIs) are associated with offspring's BMI and weight status.4, 5, 6 A child's BMI has been shown to be more strongly associated with his/her mother's BMI than the father's BMI.5,7 The observed associations between parental BMIs and the development of obesity in offspring may be mediated through genetic and environmental influences.8
Food intake, as a major environmental factor influencing obesity, has been considered in many studies on the etiology of obesity.9,10 Obesity is mainly believed to be a consequence of an unbalanced energy status.11 It is known that parents have a role in shaping their child's eating patterns and eating behavior.12,13 Given that eating behavior differs among obese and normal weight individuals14 and that parental eating behavior traits are correlated with offspring's BMI,15 overweight and normal weight mothers probably impose different influences on the food intake patterns of their children.
Previous studies have focused on maternal/parental influences on a child's eating behavior,16, 17, 18, 19 but very few have considered the mother's BMI at the same time.19 It is currently unclear whether mother's BMI correlates with a child's food intake, especially specific food groups. The present study aims to investigate the association between mother's BMI and a child's food intake at the age of 10 years using data from the population-based German birth cohorts GINIplus (German Infant Nutritional Intervention plus environmental and genetic influences on allergy development) and LISAplus (influences of lifestyle-related factors on the immune system and the development of allergies in childhood plus air pollution and genetics).
Materials and methods
Study population
Data from two population-based German birth cohort studies were analyzed. GINIplus is an ongoing birth cohort study initiated to prospectively investigate the influence of a nutritional intervention during infancy, as well as air pollution and genetics, on allergy development. GINIplus participants (N=5991 newborns) were recruited from obstetric clinics in Munich and Wesel between September 1995 and July 1998. Details of the study design are described elsewhere.20
LISAplus is an ongoing birth cohort examining the impact of lifestyle-related factors, air pollution and genetics on immune system and childhood allergy development. In total, 3097 neonates were recruited from 14 obstetrical clinics in Munich, Leipzig, Wesel and Bad Honnef between November 1997 and January 1999. A detailed description of the study's screening and recruitment has been described previously.21
This analysis includes 3230 children who participated in the 10-year food frequency questionnaire survey, and for whom data on mother's BMI and socioeconomic status variables were available.
Approval by the respective local ethics committees (Bavarian General Medical Council, University of Leipzig, Medical Council of North-Rhine-Westphalia) and written consent from all participating families were obtained for both studies.
Definition of outcomes: total energy intake and intake of 11 food groups
The outcomes of interest were derived from the food frequency questionnaire. The details and effectiveness of the food frequency questionnaire have been published elsewhere.22,23 Briefly, information on food intake frequencies and portion sizes for 82 food items were collected using parent-completed questionnaires. Seventy-nine food items were clustered into 11 food groups according to the Codex General Standard for Food Additives' food category system.24 We excluded three food items: nut-nougat-cream, water and syrup. Nut-nougat-cream has a complex composition and could not be adequately classified into one food group. Syrup intake was very low in the current study. Water intake was excluded as its consumption does not yield energy. However, we used water intake as an additional adjustment variable when assessing the association between beverage intake and the outcomes, as beverage intake may be associated with water intake.25 Information on the intake of sweeteners, salts, spices, soups, sauces, salads and foodstuffs intended for particular nutritional use was not available in the current study.
Details of the grouping of food items into food groups are given in Table 1. The 11 food groups were labeled as dairy and dairy products, fats and oils, fruits and vegetables, confectionery, cereal, bakery products, meat and meat products, fish and fish products, eggs and egg products, beverages and ready-to-eat savories.
Table 1. Definition of food groupsa.
| Food groups | Food items |
|---|---|
| Dairy and dairy products | Cheeses, milk and yogurts, cream and fresh cream |
| Fats and oils | Butter and margarines, oils |
| Fruit and vegetables | Cooked potatoes, nuts, pumpkin, pine seeds, sunflower seeds, carrots, peppers, spinach, chard, cabbage, lettuce, apples, pears, citrus fruits and berries |
| Confectionery | Chocolate, chocolate bars and soft sweets |
| Cereal | Muesli, cereals, corn flakes, crispy, rice, pasta and noodles |
| Bakery products | Bread, toast, multigrain bread, whole-wheat bread, white rolls, pretzels, croissants, chocolate rolls, cakes, pastries, cookies and biscuits |
| Meat and meat products | Pork, beef, veal, poultry, organ meats, wiener, sausage and salami |
| Fish and fish products | Freshwater fish, saltwater fish, herring, fish sticks and canned fish |
| Eggs and egg products | Egg, scrambled egg, fried egg, semolina, pudding and rice pudding |
| Beverages | Fruit juices, fruit nectars, vegetable juices, diluted juices, sparkling drinks, lemonade, cola, ice tea, sport drinks, energy drinks and tea |
| Ready-to-eat savories | Crisps, chips, croquettes and pizza |
Defined according to the Codex General Standard for Food Additives food category system.24
Total energy intake in kilocalories per day was calculated on the basis of the intake frequencies and portion sizes of the food items. For each of the 11 food groups, the average intake in grams per day was calculated. Because the distributions of the food intakes were positively skewed, and linear associations with BMI z-scores were only observed for some of the 11 food groups, the food intakes were categorized into three levels (low, medium and high) using food group and sex-specific tertile cutoffs. Low intake levels were used as the reference group in all models.
Definition of predictors: mother's BMI and mother's weight status
On the basis of the mothers' weight and height information collected at the 10-year questionnaire survey, mothers' BMIs (weight in kg/(height in m)2) were calculated. Four categories for mothers' weight status were initially defined (underweight: BMI<18.5 kg/m2; normal weight: BMI: 18.5–24.9 kg/m2; overweight: BMI: 25–29.9 kg/m2 and obese: BMI⩾30 kg/m2). However, as the number of underweight mothers was relatively small (n=83) and analyses excluding these participants did not yield substantially different results, the underweight and normal weight categories were combined as ‘normal weight'. Furthermore, as preliminary results showed similar effect estimates for the overweight and obese categories (results not shown), these two groups were also combined as ‘overweight'. Ultimately, two categories were available for this variable (normal weight versus overweight).
Potential confounding factors
Study region (Munich, Wesel, Bad Honef and Leipzig), maternal education, child's sex, age and pubertal status and BMIs of the child and father were considered as potential covariates in the analysis. The parents were asked to indicate whether their child exhibited characteristics indicative of puberty onset (yes/no). The child's age in months was calculated using the birth date and date of the 10-year questionnaire. Maternal education was defined according to the highest number of years the mother attended school and grouped into three categories (low <10 years, medium=10 years and high >10 years). BMIs of the child and father were calculated on the basis of weight and height information collected at the 10-year questionnaire survey.
Statistical analysis
Differences between male and female subjects were tested using the Pearson χ2-test for categorical variables, the Student's t-test for normally distributed continuous variables and the Mann–Whitney test for non-normally distributed continuous variables (that is, intake of 11 food groups). Study characteristics are described using means and s.d. or percentages (n/N, %). The food intake characteristics are described using median and percentiles. Statistical significance was set at the conventional P-value <0.05. All analyses were performed using the statistical software package R, version 2.14.1.26
For each of the 11 food groups, crude and adjusted multinomial regression models were used to examine associations between child's food intake with mother's BMI and mother's overweight. As preliminary analyses indicated no major differences by sex or interactions among the covariates, pooled analyses were conducted. Three types of models were initially calculated: (A) crude models, (B) models adjusted for study region, maternal education, child's sex, age, pubertal status and partition energy intake27 and (C) models additionally adjusted for the BMIs of the child and father. The partition energy intake was calculated from the food group itself and the energy intake from all other food groups. Each model for the association between the energy intake of a specific group with mother's BMI and mother's overweight was adjusted for the respective energy intake from all other food groups. As a child's BMI is likely to be affected by his/her food intake, results of model C may be over-adjusted. Therefore, we additionally conducted stratified analyses by child weight status (overweight versus non-overweight). Finally, we presented coefficients from model B in the results section. For comparison purposes, we also present results from model C in the figures. Model results are presented as relative risk ratios (RRRs) with corresponding 95% confidence intervals (RRR (95% CI)).
Crude and adjusted linear regression models were used to study the association of child's total energy intake with mother's BMI and mother's overweight. The same three types of models were calculated as described above. Model results are presented as linear regression coefficients (β) with corresponding 95% confidence intervals (β (95% CI)). For models in which the mother's BMI is the predictor, the β-coefficient represents the mean increase in total energy intake for a one-unit increase in the mother's BMI. For models in which mother's weight status is the predictor, the β-coefficient represents the difference in total energy intake between mother's overweight and mother's normal weight.
Results
The characteristics of the participants are summarized in Table 2. Female participants comprised 48.7% of the sample. The mean age of children was 120.6 months (s.d.=2.4) and 28.9% of participants exhibited signs of puberty (11.6% and 47.2% for males and females, respectively, P<0.001). The average total energy intake of children was 2106 kcal (s.d.=673). Males had higher total energy intake than females (2278 kcal (723) versus 1927 kcal (560), P<0.001). Over half of the participants had mothers with a high level of education (50.4%). The mean mothers' BMI was 23.8 (s.d.=4.1), and 20.2% of the mothers were overweight and 8.0% were obese.
Table 2. Characteristics of the study population at 10 years of age, mean (s.d.) or % (n/N).
| Males (n=1684) | Females (n=1596) | Overall (n=3280) | |
|---|---|---|---|
| Study | |||
| GINIplus | 63.1 (1062/1684) | 65.6 (1047/1596) | 64.3 (2109/3280) |
| LISAplus | 36.9 (622/1684) | 34.4 (549/1596) | 35.7 (1171/3280) |
| Study region | |||
| Munich | 50.7 (853/1684) | 50.5 (806/1596) | 50.6 (1659/3280) |
| Leipzig | 7.7 (129/1684) | 7.4 (118/1596) | 7.5 (247/3280) |
| Bad Honnef | 4.2 (71/1684) | 4.8 (76/1596) | 4.5 (147/3280) |
| Wesel | 37.5 (631/1684) | 37.3 (596/1596) | 37.4 (1227/3280) |
| Maternal educationa | |||
| Low | 9.8 (164/1674) | 8.6 (137/1592) | 9.2 (301/3266) |
| Medium | 41.5 (695/1674) | 39.1 (623/1592) | 40.4 (1318/3266) |
| High | 48.7 (815/1674) | 52.3 (832/1592) | 50.4 (1647/3266) |
| Maternal BMI, kg/m2 | 23.8 (4.2) | 23.7 (4.1) | 23.8 (4.2) |
| Maternal weight statusb | |||
| Normal weight | 71.4 (1203/1684) | 71.9 (1147/1596) | 71.6 (2350/3280) |
| Overweight | 28.6 (481/1684) | 28.2 (449/1596) | 28.3 (930/3280) |
| Child BMI, kg/m2 | 16.9 (2.3) | 16.7 (2.3) | 16.8 (2.3) |
| Age, months | 120.6 (2.4) | 120.7 (2.4) | 120.6 (2.4) |
| Puberty onsetc, % | 11.6 (193/1665) | 47.2 (743/1574)d | 28.9 (936/3239) |
| Total energy intake, kcal/day | 2278 (723) | 1927 (560)d | 2107 (672) |
| Paternal BMI, kg/m2 | 25.9 (3.3) | 26.0 (3.4) | 25.9 (3.3) |
Abbreviations: BMI, body mass index; GINIplus, German infant nutritional intervention plus environmental and genetic influences on allergy development; LISAplus, influences of lifestyle-related factors on the immune system and the development of allergies in childhood plus air pollution and genetics.
Categorized according to the highest number of years the mother attended school: low <10 years, medium=10 years and high >10 years.
Normal weight: BMI<25 kg/m2; overweight: BMI⩾25 kg/m2.
Indicated by the parents whether their child exhibited characteristics indicative of puberty onset (yes/no).
Significant difference between males and females.
The average food intakes in grams per day are shown in Table 3. The median intake of meat products was 97 g per day (33rd and 66th percentile (75; 122)), which corresponds to a median percent energy (%En) of 12.0% (9.7; 14.7). The median egg intake was 18 g per day ((12; 24), %En=1.4% (1.0; 1.9)). Compared with males, females had significantly lower intakes of all 11 food groups (for example, median meat intake: 108 versus 86 g per day; median egg intake: 19 versus 16 g per day), except for fruit and vegetables (median intake: 270 versus 287 g per day). Compared with males, females had a significantly lower %En of dairy products as well as meat and meat products (14.4% versus 15.2% and 11.3% versus 12.4%, respectively), but a significantly higher %En of fats and oils, fruit and vegetables as well as bakery products (4.0% versus 3.8%, 8.1% versus 6.6% and 18.8% versus 17.8%, respectively).
Table 3. Intake of the 11 food groups, stratified by sex.
| Food intake, g/day | Males (N=1684) | Females (N=1596) | Overall (N=3280) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Median |
Percentiles |
%En | Median |
Percentiles |
%En | Median |
Percentiles |
%En | ||||
| |
|
33rd |
66th |
|
|
33rd |
66th |
|
|
33rd |
66th |
|
| Dairy products | 369 | 271 | 511 | 15.2 | 293a | 216 | 380 | 14.4a | 324 | 245 | 441 | 14.8 |
| Fats and oils | 15 | 11 | 20 | 3.8 | 13a | 10 | 18 | 4.0a | 14 | 10 | 19 | 3.9 |
| Fruits and vegetables | 270 | 215 | 327 | 6.6 | 287a | 234 | 343 | 8.1a | 278 | 224 | 335 | 7.3 |
| Confectionery | 16 | 11 | 25 | 3.0 | 14a | 10 | 20 | 2.9 | 15 | 10 | 22 | 3.0 |
| Cereals | 83 | 65 | 106 | 13.5 | 75a | 58 | 93 | 14.4 | 78 | 62 | 99 | 14.0 |
| Bakery products | 147 | 121 | 176 | 17.8 | 134a | 110 | 159 | 18.8a | 141 | 116 | 168 | 18.3 |
| Meat and meat products | 108 | 86 | 137 | 12.4 | 86a | 67 | 108 | 11.3a | 97 | 75 | 122 | 12.0 |
| Fish and fish products | 17 | 12 | 24 | 1.1 | 14a | 10 | 21 | 1.1 | 16 | 11 | 22 | 1.1 |
| Eggs and egg products | 19 | 13 | 26 | 1.4 | 16a | 12 | 22 | 1.4 | 18 | 12 | 24 | 1.4 |
| Beverages | 603 | 387 | 839 | 8.1 | 522a | 335 | 721 | 7.7 | 560 | 357 | 781 | 7.9 |
| Ready-to-eat savories | 44 | 35 | 54 | 4.9 | 38a | 30 | 47 | 5.0 | 42 | 33 | 51 | 4.9 |
Food groups were defined according to the Codex General Standard for Food Additives food category system;24 %En: Percent energy provided from the food group;
Significant differences between males and females were tested by the Mann–Whitney test.
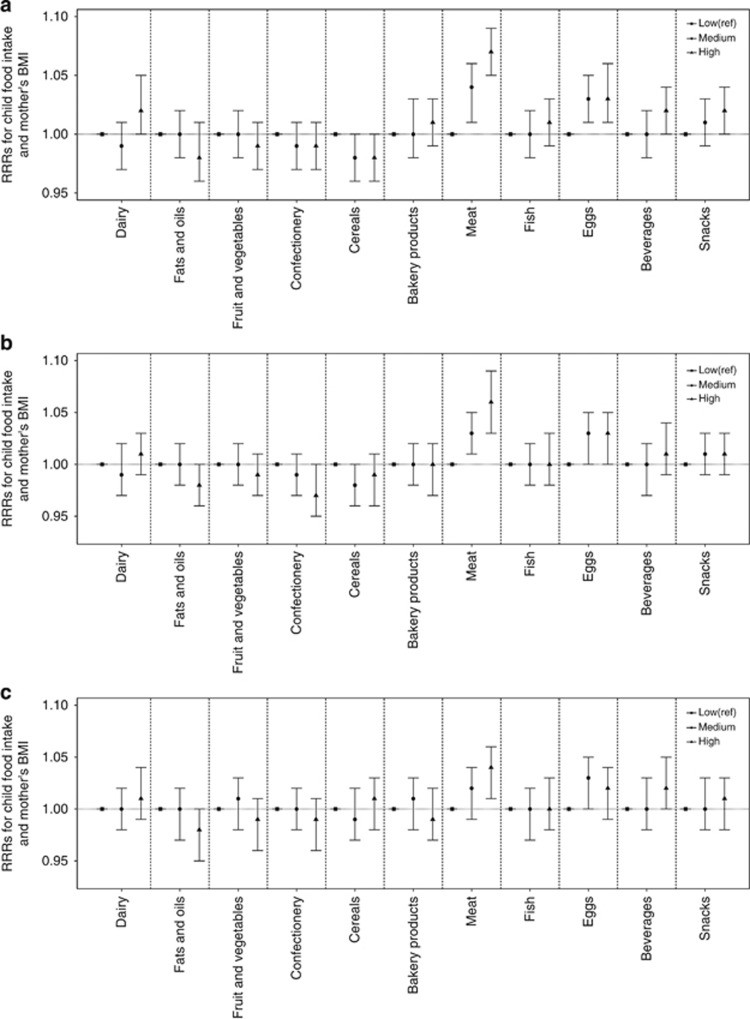
Crude and adjusted RRRs for the associations between child's intake of the 11 food groups and mother's BMI are shown in Table 4 and Figure 1. The crude RRRs for the comparison of low intake with medium and high intake are presented in Figure 1a, partially adjusted RRRs in Figure 1b and fully adjusted RRRs in Figure 1c. Mothers' BMI was associated with high meat intake in children (adjusted RRR=1.06 (1.03; 1.09)). In addition, mothers' BMI was marginally associated with a high intake of fats and oils as well as intake of eggs (adjusted RRR=0.98 (0.96; 1.00) and 1.03 (1.00; 1.05), respectively). No consistent associations between mother's BMI and child's intake of the other food groups were observed.
Table 4. Relative risk ratios (RRRs) for the associations between intake of food groups and mothers' BMI.
| Food groupsa | Intake levelb | Model A | Model B | Model C | |||
|---|---|---|---|---|---|---|---|
| |
|
RRR |
95% CI |
RRR |
95% CI |
RRR |
95% CI |
| Dairy products | Low | Ref. | Ref. | Ref. | |||
| Medium | 0.99 | (0.97;1.01) | 0.99 | (0.97; 1.02) | 1.00 | (0.98; 1.02) | |
| High | 1.02 | (1.00; 1.05) | 1.01 | (0.99; 1.03) | 1.01 | (0.99; 1.04) | |
| Fats and oils | Low | Ref. | Ref. | Ref. | |||
| Medium | 1.00 | (0.98; 1.02) | 1.00 | (0.98; 1.02) | 1.00 | (0.97; 1.02) | |
| High | 0.98 | (0.96; 1.01) | 0.98 | (0.96; 1.00) | 0.98 | (0.95; 1.00) | |
| Fruits and vegetables | Low | Ref. | Ref. | Ref. | |||
| Medium | 1.00 | (0.98; 1.02) | 1.00 | (0.98; 1.02) | 1.01 | (0.98; 1.03) | |
| High | 0.99 | (0.97; 1.01) | 0.99 | (0.97; 1.01) | 0.99 | (0.96; 1.01) | |
| Confectionery | Low | Ref. | Ref. | Ref. | |||
| Medium | 0.99 | (0.97; 1.01) | 0.99 | (0.97; 1.01) | 1.00 | (0.98; 1.02) | |
| High | 0.99 | (0.97; 1.01) | 0.97 | (0.95; 1.00) | 0.99 | (0.96; 1.01) | |
| Cereals | Low | Ref. | Ref. | Ref. | |||
| Medium | 0.98 | (0.96; 1.00) | 0.98 | (0.96; 1.00) | 0.99 | (0.97; 1.02) | |
| High | 0.98 | (0.96; 1.00) | 0.99 | (0.96; 1.01) | 1.01 | (0.98; 1.03) | |
| Bakery products | Low | Ref. | Ref. | Ref. | |||
| Medium | 1.00 | (0.98; 1.03) | 1.00 | (0.98; 1.02) | 1.01 | (0.98; 1.03) | |
| High | 1.01 | (0.99; 1.03) | 1.00 | (0.97; 1.02) | 0.99 | (0.97; 1.02) | |
| Meat and meat products | Low | Ref. | Ref. | Ref. | |||
| Medium | 1.04 | (1.01; 1.06) | 1.03 | (1.01; 1.05) | 1.02 | (0.99; 1.04) | |
| High | 1.07 | (1.05; 1.09) | 1.06 | (1.03; 1.09) | 1.04 | (1.01; 1.06) | |
| Fish and fish products | Low | Ref. | Ref. | Ref. | |||
| Medium | 1.00 | (0.98; 1.02) | 1.00 | (0.98; 1.02) | 1.00 | (0.97; 1.02) | |
| High | 1.01 | (0.99; 1.03) | 1.00 | (0.98; 1.03) | 1.00 | (0.98; 1.03) | |
| Eggs and egg products | Low | Ref. | Ref. | Ref. | |||
| Medium | 1.03 | (1.01; 1.05) | 1.03 | (1.00; 1.05) | 1.03 | (1.00; 1.05) | |
| High | 1.03 | (1.01; 1.06) | 1.03 | (1.00; 1.05) | 1.02 | (0.99; 1.04) | |
| Beverages | Low | Ref. | Ref. | Ref. | |||
| Medium | 1.00 | (0.98; 1.02) | 1.00 | (0.97; 1.02) | 1.00 | (0.98; 1.03) | |
| High | 1.02 | (1.00; 1.04) | 1.01 | (0.99; 1.04) | 1.02 | (1.00; 1.05) | |
| Ready-to-eat savories | Low | Ref. | Ref. | Ref. | |||
| Medium | 1.01 | (0.99; 1.03) | 1.01 | (0.99; 1.03) | 1.00 | (0.98; 1.03) | |
| High | 1.02 | (1.00; 1.04) | 1.01 | (0.99; 1.03) | 1.01 | (0.98; 1.03) | |
Abbreviations: BMI, body mass index; CI, confidence interval; Ref., reference.
Model A—crude model, Model B—adjusted for study region, maternal education, child's sex, age, pubertal status and energy intake from other food groups, Model C—additionally adjusted for the BMIs of the child and father
.
Food groups were defined according to the Codex General Standard for Food Additives food category system.24
Defined using sex- and group-specific tertile cutoffs.
Figure 1.
Relative risk ratios (RRRs) for the associations between intake of food groups and mother's BMI. (a) Crude, (b) adjusted for study region, maternal education, childs' sex, age, pubertal status and energy intake from other food groups, (c) additionally adjusted for the BMIs of the child and father.
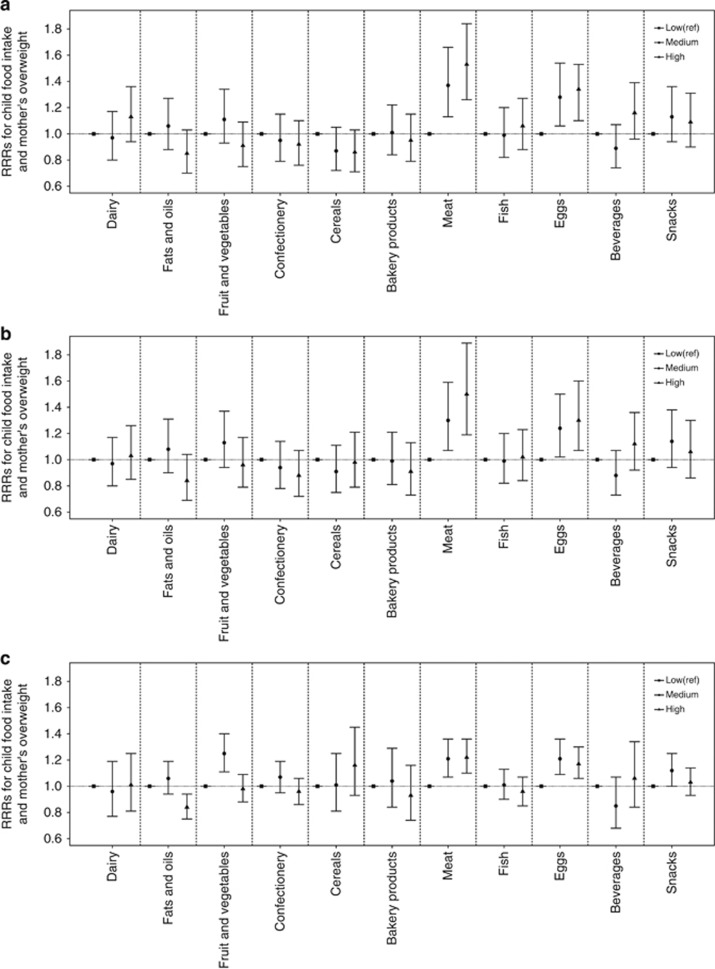
Crude and adjusted RRRs for the association of a child's intake of 11 food groups with mother's overweight are shown in Table 5 and Figure 2. The crude RRRs for the comparison of low intake with medium and high intake are presented in Figure 2a, partially adjusted RRRs in Figure 2b and fully adjusted RRRs in Figure 2c. Mother's overweight was associated with child's meat intake (medium versus low RRR=1.30 (1.07; 1.59); high versus low RRR=1.50 (1.19; 1.89)) and egg intake (medium versus low RRR=1.24 (1.02; 1.50); high versus low RRR=1.30 (1.07; 1.60)). No consistent associations between mother's overweight and child's intake of the other food groups were observed.
Table 5. Relative risk ratios (RRRs) for the associations between intake of food groups and mothers' overweight.
| Food groupsa | Intake levelb | Model A | Model B | Model C | |||
|---|---|---|---|---|---|---|---|
| |
|
RRR |
95% CI |
RRR |
95% CI |
RRR |
95% CI |
| Dairy products | Low | Ref. | Ref. | Ref. | |||
| Medium | 0.97 | (0.80; 1.17) | 0.97 | (0.80; 1.17) | 0.96 | (0.77; 1.19) | |
| High | 1.13 | (0.94; 1.36) | 1.03 | (0.85; 1.26) | 1.01 | (0.81; 1.25) | |
| Fats and oils | Low | Ref. | Ref. | Ref. | |||
| Medium | 1.06 | (0.88; 1.27) | 1.08 | (0.90; 1.31) | 1.06 | (0.94; 1.19) | |
| High | 0.85 | (0.70; 1.03) | 0.84 | (0.69; 1.04) | 0.84 | (0.75; 0.94) | |
| Fruits and vegetables | Low | Ref. | Ref. | Ref. | |||
| Medium | 1.11 | (0.93; 1.34) | 1.13 | (0.94; 1.37) | 1.25 | (1.11; 1.40) | |
| High | 0.91 | (0.75; 1.09) | 0.96 | (0.79; 1.17) | 0.98 | (0.88; 1.09) | |
| Confectionery | Low | Ref. | Ref. | Ref. | |||
| Medium | 0.95 | (0.79; 1.15) | 0.94 | (0.78; 1.14) | 1.07 | (0.95; 1.19) | |
| High | 0.92 | (0.76; 1.10) | 0.88 | (0.72; 1.07) | 0.96 | (0.86; 1.06) | |
| Cereals | Low | Ref. | Ref. | Ref. | |||
| Medium | 0.87 | (0.72; 1.05) | 0.91 | (0.75; 1.11) | 1.01 | (0.81; 1.25) | |
| High | 0.86 | (0.71; 1.03) | 0.98 | (0.79; 1.21) | 1.16 | (0.93; 1.45) | |
| Bakery products | Low | Ref. | Ref. | Ref. | |||
| Medium | 1.01 | (0.84; 1.22) | 0.99 | (0.81; 1.21) | 1.04 | (0.84; 1.29) | |
| High | 0.95 | (0.79; 1.15) | 0.91 | (0.73; 1.13) | 0.93 | (0.74; 1.16) | |
| Meat and meat products | Low | Ref. | Ref. | Ref. | |||
| Medium | 1.37 | (1.13; 1.66) | 1.30 | (1.07; 1.59) | 1.21 | (1.07; 1.36) | |
| High | 1.53 | (1.26; 1.84) | 1.50 | (1.19; 1.89) | 1.22 | (1.10; 1.36) | |
| Fish and fish products | Low | Ref. | Ref. | Ref. | |||
| Medium | 0.99 | (0.82; 1.20) | 0.99 | (0.82; 1.20) | 1.01 | (0.90; 1.13) | |
| High | 1.06 | (0.88; 1.27) | 1.02 | (0.84; 1.23) | 0.96 | (0.85; 1.07) | |
| Eggs and egg products | Low | Ref. | Ref. | Ref. | |||
| Medium | 1.28 | (1.06; 1.54) | 1.24 | (1.02; 1.50) | 1.21 | (1.09; 1.36) | |
| High | 1.34 | (1.10; 1.53) | 1.30 | (1.07; 1.60) | 1.17 | (1.06; 1.30) | |
| Beverages | Low | Ref. | Ref. | Ref. | |||
| Medium | 0.89 | (0.74; 1.07) | 0.88 | (0.73; 1.07) | 0.85 | (0.68; 1.07) | |
| High | 1.16 | (0.96; 1.39) | 1.12 | (0.92; 1.36) | 1.06 | (0.84; 1.34) | |
| Ready-to-eat savories | Low | Ref. | Ref. | Ref. | |||
| Medium | 0.97 | (0.80; 1.17) | 0.97 | (0.80; 1.17) | 0.96 | (0.77; 1.19) | |
| High | 1.13 | (0.94; 1.36) | 1.03 | (0.85; 1.26) | 1.01 | (0.81; 1.25) | |
Abbreviations: CI, confidence interval; Ref., reference.
Model A—crude model; Model B—adjusted for study region, maternal education, child's sex, age, pubertal status and energy intake from other food groups; Model C—additionally adjusted for the BMIs of the child and father.
Food groups were defined according to the Codex General Standard for Food Additives food category system.24
Defined using sex- and group-specific tertile cutoffs.
Figure 2.
Relative risk ratios (RRRs) for the associations between intake of food groups and mother's overweight. (a) Crude; (b) adjusted for study region, maternal education, child's sex, age, pubertal status and energy intake from other food groups; (c) additionally adjusted for the BMIs of the child and father.
In addition, the significant associations for meat and eggs were observed in both overweight and non-overweight subgroups with similar effect sizes (results not shown).
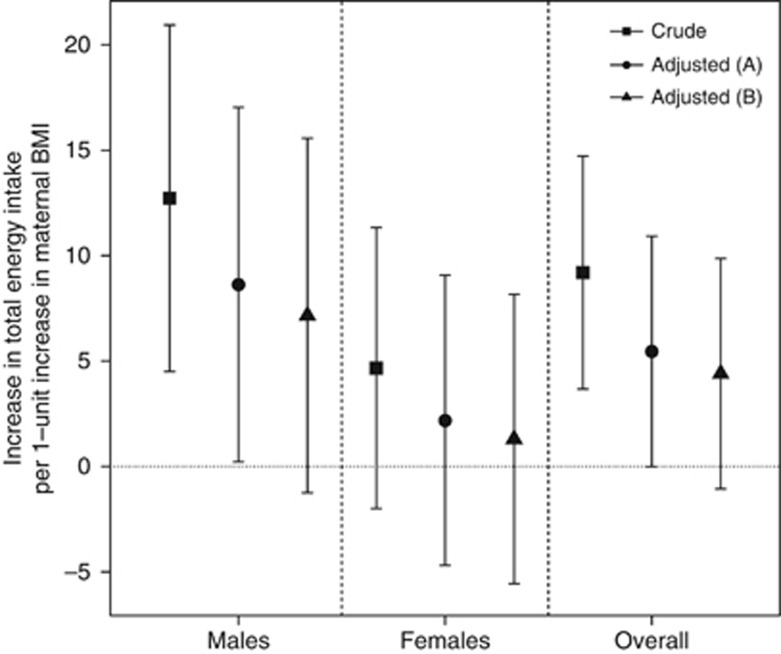
Sex-specific and pooled increases in child's total energy intake per one-unit increase in mother's BMI are shown in Figure 3. In the pooled crude models, every one-unit increase in mother's BMI was associated with a total energy intake increase of 9.2 kcal (3.67~14.72). However, this effect was not significant after full adjustment (4.2 kcal (−1.9; 10.3)). In addition, this effect was more pronounced among males. Associations among females were of smaller magnitude and not significant. No association between mother's overweight and energy intake was observed (results not shown).
Figure 3.
Linear regression coefficients for the association between mother's BMI and child's total energy intake in the total population and stratified by sex. A—adjusted for study region, maternal education, child's age and pubertal status, B—additionally adjusted for the BMIs of the child and father. Pooled models were additionally adjusted for sex.
Discussion
In the current study, we analyzed associations between mother's BMI/overweight and child's food intake using data from two German birth cohorts. We observed significantly positive associations between mother's BMI/overweight and child's intake of meat, eggs and energy.
Currently, little is known regarding associations between child's food intake and mother's BMI. To the best of our knowledge, no other published studies exist with which we can compare our results. Nevertheless, we provide here several possible explanations for the trends observed.
As parents appear to have a strong influence on their child's eating behavior and patterns,12,13 children are likely to have similar dietary patterns as their parents. Results from the National Health and Nutrition Examination Survey study have shown a positive association between meat intake and obesity in adults.28 It is possible that a child may imitate his/her overweight mother's eating pattern, and thus may consume more meat. It is also possible that overweight mothers include more meat products in the family meals compared with mothers of normal weight. Hence, their children have an increased availability to meat, which may contribute to a higher meat intake.29,30 On the basis of our previous research using the same study population (under review), a high meat intake appears to be associated with being overweight at 10 years of age. These associations suggest a potential pathway of the mother–child weight relationship, although any causal relationship between food intake and being overweight may be bidirectional.
There is also limited evidence for the association between egg intake and BMI. A breakfast that includes eggs is reported to be beneficial for weight loss.31 However, it is unclear whether the satiating effect of eggs32 or the fact that a high-protein breakfast is consumed instead of a high-carbohydrate breakfast is responsible for this beneficial effect. Information on whether overweight mothers consume or prepare more eggs than mothers of normal weight is not available in the current study.
We observed significant associations between mother's BMI and total energy intake in male children in the crude models. This effect was no longer significant after adjustment for child's BMI. This result was not replicated among females of the same age. There are very few studies that have investigated associations between mothers' BMI and energy intake in children. Thus, it is challenging to compare our results with previous works. We attempt here to provide some possible explanations for the observed results.
In a sample of 563 mother–child (2–11 years of age) pairs, mothers with higher BMI levels were reported to have a lower level of control on their children's diet than mothers with normal BMI levels.33 A lower level of control may lead to a higher food intake. In addition, mothers' perception and concern of their children's weight may also have an important role on the investigated association.16,34 Parental feeding control was reported to have a greater impact on girls than on boys in an American mid–high socioeconomic population.35,36 This may have led to the observed sex differences. Also, a mother's perception of child's weight status may differ by sex (for example, mothers may be more sensitive to their daughters weight status), although these associations are also likely to vary by culture.37,38
Previous studies have focused on associations between mother's feeding practices (that is, restriction to eat less or pressure to eat more food) and child's food intake or child's weight,16,33,39, 40, 41, 42 which are believed to be mediated by a mother's concern for her child's weight and the perception of her child's weight.16,34 Mothers' feeding practices were reported to explain 22.2–26.9% of the variance in food intake of children aged 3–6 years who were at risk for becoming overweight.39 It was reported that a higher child weight at 7–9 years of age was associated with a lower ‘pressure to eat' and a higher ‘restriction score' from mothers.16 Another study reported that perceived child's weight and concern for child's weight explains around 40% of the variance of the BMI z-score changes at 12 years of age.40 Moreover, the results from a study on 296 low-income African-American children suggested that feeding strategies may differ according to mother's weight status.43 Factors such as mother's food intake,41 child's weight,39 ethnicity,33 family income and parental education level39,42 may also influence a mother's feeding practices.
The current study investigated associations between mother's BMI and child's energy and food intake using data from two large population-based cohorts from Germany, which included the use of the qualified food frequency questionnaire. Energy and food intake were classified into 11 food groups according to the Codex General Standard for Food Additives' food category system, which will allow our results to be compared with future studies. Instead of providing isocaloric interpretations, the multivariate energy partition models allowed us to interpret our results while taking both energy and non-energy effects of foods into account.
Our study has some limitations. First, as the data were collected using questionnaires completed by the parents, reporting bias is possible. A parent's perception of their child's food intake might be a biased measure of true consumption. Second, the cross-sectional design of this study prevents us from establishing causal relationships. Third, some of our analyses may have been over-adjusted. As child food intake is likely to be in the pathway between mother's BMI and child's BMI, adjusting for child's BMI may represent an over-adjustment. However, the associations between mother's overweight and child's high intakes of meat and eggs remained significant, even after adjustment for child's BMI. Finally, we lack information on important mediators such as mother's concern for child's weight, mother's perception of child's weight, and child's own perception and concerns. Future studies should consider these factors.
Conclusion
Mother's BMI and mother's overweight appear to be important correlates of a child's intake of meat and egg products. The potential impact of mother's weight status should be considered in diet counseling. Moreover, a mother's participation in dietary counseling may be a helpful method for improving a child's diet pattern and weight status.
Acknowledgments
GINIplus study group: Helmholtz Zentrum München, German Research Center for Environmental Health, Institute of Epidemiology I, Munich (Joachim Heinrich, Heinz-Erich Wichmann, Stefanie Sausenthaler, Anne Zutavern, Chih-Mei Chen, Markus Schnappinger and Peter Rzehak); Department of Pediatrics, Marien-Hospital, Wesel (Dietrich Berdel, Andrea von Berg, Christina Beckmann and Irene Gross); Department of Pediatrics, Ludwig Maximilians University, Munich (Sibylle Koletzko, Dietrich Reinhardt and Susanne Krauss-Etschmann); Department of Pediatrics, Technical University, Munich (Carl-Peter Bauer, Inken Brochow, Armin Grübl and Ute Hoffmann); IUF—Institut für Umweltmedizinische Forschung at the Heinrich-Heine-University, Düsseldorf (Ursula Krämer, Elke Link and Claudia Cramer). LISAplus study group: Helmholtz Zentrum München, German Research Center for Environmental Health, Institute of Epidemiology I, Munich (Joachim Heinrich, Heinz-Erich Wichmann, Stefanie Sausenthaler, Chih-Mei Chen and Markus Schnappinger); Department of Pediatrics, Municipal Hospital ‘St Georg', Leipzig (Michael Borte and Ulrike Diez), Marien-Hospital Wesel, Department of Pediatrics, Wesel (Andrea von Berg, Christina Beckmann and Irene Gross); Pediatric Practice, Bad Honnef (Beate Schaaf); Helmholtz Centre for Environmental Research—UFZ, Department of Environmental Immunology/Core Facility Studies, Leipzig (Irina Lehmann, Mario Bauer, Carolin Gräbsch, Stefen Röder and Maik Schilde); University of Leipzig, Institute of Hygiene and Environmental Medicine, Leipzig (Olf Herbarth, Christian Dick and Juliane Magnus); IUF—Institut für Umweltmedizinische Forschung, Düsseldorf (Ursula Krämer, Elke Link and Claudia Cramer); Technical University Munich, Department of Pediatrics, Munich (Carl-Peter Bauer and Ute Hoffmann); ZAUM—Center for Allergy and Environment, Technical University, Munich (Heidrun Behrendt, Johanna Grosch and Franziska Martin). The GINIplus study was mainly supported for the first 3 years by the Federal Ministry for Education, Science, Research and Technology (interventional arm) and Helmholtz Zentrum Munich (former GSF) (observational arm). The 4-year, 6-year and 10-year follow-up examinations of the GINIplus study were covered from the respective budgets of the five study centers (Helmholtz Zentrum Munich (former GSF), Research Institute at Marien-Hospital Wesel, LMU Munich, TU Munich and from 6 years onwards also from IUF—Leibniz Research Institute for Environmental Medicine at the University of Düsseldorf) and a grant from the Federal Ministry for Environment (IUF Düsseldorf, FKZ 20462296). The LISAplus study was mainly supported by grants from the Federal Ministry for Education, Science, Research and Technology and in addition from Helmholtz Zentrum Munich (former GSF), Helmholtz Centre for Environmental Research—UFZ, Leipzig, Research Institute at Marien-Hospital Wesel, Pediatric Practice, Bad Honnef for the first 2 years. The 4-year, 6-year and 10-year follow-up examinations of the LISAplus study were covered from the respective budgets of the involved partners (Helmholtz Zentrum Munich (former GSF), Helmholtz Centre for Environmental Research—UFZ, Leipzig, Research Institute at Marien-Hospital Wesel, Pediatric Practice, Bad Honnef, IUF—Leibniz Research Institute for Environmental Medicine at the University of Düsseldorf) and in addition by a grant from the Federal Ministry for Environment (IUF Düsseldorf, FKZ 20462296). This work was supported by the Kompetenznetz Adipositas (Competence Network Obesity) funded by the Federal Ministry of Education and Research (FKZ: 01GI1121A).
The authors declare no conflict of interest.
References
- James PT, Leach R, Kalamara E, Shayeghi M. The worldwide obesity epidemic. Obes Res. 2001;9:228S–233S. doi: 10.1038/oby.2001.123. [DOI] [PubMed] [Google Scholar]
- International Obesity Taskforce. Obesity the global epidemic. 2011. Available at: http://www.iaso.org/iotf/obesity/obesitytheglobalepidemic/ .
- Biro FM, Wien M. Childhood obesity and adult morbidities. Am J Clin Nutr. 2010;91:1499S–1505S. doi: 10.3945/ajcn.2010.28701B. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birbilis M, Moschonis G, Mougios V, Manios Y. Obesity in adolescence is associated with perinatal risk factors, parental BMI and sociodemographic characteristics. Eur J Clin Nutr. 2013;67:115–121. doi: 10.1038/ejcn.2012.176. [DOI] [PubMed] [Google Scholar]
- Danielzik S, Langnase K, Mast M, Spethmann C, Muller MJ. Impact of parental BMI on the manifestation of overweight 5-7 year old children. Eur J Clin Nutr. 2002;41:132–138. doi: 10.1007/s00394-002-0367-1. [DOI] [PubMed] [Google Scholar]
- Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH. Predicting obesity in young adulthood from childhood and parental obesity. N Engl J Med. 1997;337:869–873. doi: 10.1056/NEJM199709253371301. [DOI] [PubMed] [Google Scholar]
- Linabery AM, Nahhas RW, Johnson W, Choh AC, Towne B, Odegaard AO, et al. Stronger influence of maternal than paternal obesity on infant and early childhood body mass index: the Fels Longitudinal Study. Pediatr Obes. 2013;8:159–169. doi: 10.1111/j.2047-6310.2012.00100.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maffeis C. Aetiology of overweight and obesity in children and adolescents. Eur J Pediatr. 2000;159:S35–S44. doi: 10.1007/pl00014361. [DOI] [PubMed] [Google Scholar]
- Bradlee ML, Singer MR, Qureshi MM, Moore LL. Food group intake and central obesity among children and adolescents in the Third National Health and Nutrition Examination Survey (NHANES III) Public Health Nutr. 2010;13:797–805. doi: 10.1017/S1368980009991546. [DOI] [PubMed] [Google Scholar]
- Kral TV, Stunkard AJ, Berkowitz RI, Stallings VA, Brown DD, Faith MS. Daily food intake in relation to dietary energy density in the free-living environment: a prospective analysis of children born at different risk of obesity. Am J Clin Nutr. 2007;86:41–47. doi: 10.1093/ajcn/86.1.41. [DOI] [PubMed] [Google Scholar]
- Hill JO, Wyatt HR, Peters JC. Energy balance and obesity. Circulation. 2012;126:126–132. doi: 10.1161/CIRCULATIONAHA.111.087213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Savage JS, Fisher JO, Birch LL. Parental influence on eating behavior: conception to adolescence. J Law Med Ethics. 2007;35:22–34. doi: 10.1111/j.1748-720X.2007.00111.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell GL, Farrow C, Haycraft E, Meyer C. Parental influences on children's eating behaviour and characteristics of successful parent-focussed interventions. Appetite. 2013;60:85–94. doi: 10.1016/j.appet.2012.09.014. [DOI] [PubMed] [Google Scholar]
- Laessle RG, Lehrke S, Duckers S. Laboratory eating behavior in obesity. Appetite. 2007;49:399–404. doi: 10.1016/j.appet.2006.11.010. [DOI] [PubMed] [Google Scholar]
- Gallant AR, Tremblay A, Perusse L, Despres JP, Bouchard C, Drapeau V. Parental eating behavior traits are related to offspring BMI in the Quebec Family Study. Int J Obes (Lond) 2013;37:1422–1426. doi: 10.1038/ijo.2013.14. [DOI] [PubMed] [Google Scholar]
- Webber L, Hill C, Cooke L, Carnell S, Wardle J. Associations between child weight and maternal feeding styles are mediated by maternal perceptions and concerns. Eur J Clin Nutr. 2010;64:259–265. doi: 10.1038/ejcn.2009.146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Francis LA, Birch LL. Maternal influences on daughters' restrained eating behavior. Health Psychol. 2005;24:548–554. doi: 10.1037/0278-6133.24.6.548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Francis LA, Birch LL. Maternal weight status modulates the effects of restriction on daughters' eating and weight. Int J Obes (Lond) 2005;29:942–949. doi: 10.1038/sj.ijo.0802935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birch LL, Fisher JO. Mothers' child-feeding practices influence daughters' eating and weight. Am J Clin Nutr. 2000;71:1054–1061. doi: 10.1093/ajcn/71.5.1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- von Berg A, Filipiak-Pittroff B, Kramer U, Hoffmann B, Link E, Beckmann C, et al. Allergies in high-risk schoolchildren after early intervention with cow's milk protein hydrolysates: 10-year results from the German Infant Nutritional Intervention (GINI) study. J Allergy Clin Immunol. 2013;131:1565–1573. doi: 10.1016/j.jaci.2013.01.006. [DOI] [PubMed] [Google Scholar]
- Heinrich J, Bolte G, Holscher B, Douwes J, Lehmann I, Fahlbusch B, et al. Allergens and endotoxin on mothers' mattresses and total immunoglobulin E in cord blood of neonates. Eur Respir J. 2002;20:617–623. doi: 10.1183/09031936.02.02322001. [DOI] [PubMed] [Google Scholar]
- Kohlboeck G, Sausenthaler S, Standl M, Koletzko S, Bauer CP, von Berg A, et al. Food intake, diet quality and behavioral problems in children: results from the GINI-plus/LISA-plus studies. Ann Nutr Metab. 2012;60:247–256. doi: 10.1159/000337552. [DOI] [PubMed] [Google Scholar]
- Stiegler P, Sausenthaler S, Buyken AE, Rzehak P, Czech D, Linseisen J, et al. A new FFQ designed to measure the intake of fatty acids and antioxidants in children. Public Health Nutr. 2010;13:38–46. doi: 10.1017/S1368980009005813. [DOI] [PubMed] [Google Scholar]
- Food and Agriculture Organization of the United Nations/World Health Organization. Codex General Standard for Food Additives food category system. 2011. Available at: http://www.codexalimentarius.net/gsfaonline/docs/CXS_192e.pdf .
- Sichieri R, Yokoo EM, Pereira RA, Veiga GV. Water and sugar-sweetened beverage consumption and changes in BMI among Brazilian fourth graders after 1-year follow-up. Public Health Nutr. 2013;16:73–77. doi: 10.1017/S1368980012001309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Development Core Team R: a language and environment for statistical computing. Vienna, Austria, 2010 ISBN 3-900051-07-0. Available at: http://www.R-project.org .
- Willett WC, Howe GR, Kushi LH. Adjustment for total energy intake in epidemiologic studies. Am J Clin Nutr. 1997;65:1220S–1228S. doi: 10.1093/ajcn/65.4.1220S. [DOI] [PubMed] [Google Scholar]
- Wang Y, Beydoun MA. Meat consumption is associated with obesity and central obesity among US adults. Int J Obes (Lond) 2009;33:621–628. doi: 10.1038/ijo.2009.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arcan C, Hannan PJ, Fulkerson JA, Himes JH, Rock BH, Smyth M, et al. Associations of home food availability, dietary intake, screen time and physical activity with BMI in ysoung American-Indian children. Public Health Nutr. 2013;16:146–155. doi: 10.1017/S136898001200033X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raynor HA, Polley BA, Wing RR, Jeffery RW. Is dietary fat intake related to liking or household availability of high- and low-fat foods. Obes Res. 2004;12:816–823. doi: 10.1038/oby.2004.98. [DOI] [PubMed] [Google Scholar]
- Vander Wal JS, Gupta A, Khosla P, Dhurandhar NV. Egg breakfast enhances weight loss. Int J Obes (Lond) 2008;32:1545–1551. doi: 10.1038/ijo.2008.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vander Wal JS, Marth JM, Khosla P, Jen KL, Dhurandhar NV. Short-term effect of eggs on satiety in overweight and obese subjects. J Am Coll Nutr. 2005;24:510–515. doi: 10.1080/07315724.2005.10719497. [DOI] [PubMed] [Google Scholar]
- Cachelin FM, Thompson D. Predictors of maternal child-feeding practices in an ethnically diverse sample and the relationship to child obesity. Obesity (Silver Spring) 2013;21:1676–1683. doi: 10.1002/oby.20385. [DOI] [PubMed] [Google Scholar]
- Francis LA, Hofer SM, Birch LL. Predictors of maternal child-feeding style: maternal and child characteristics. Appetite. 2001;37:231–243. doi: 10.1006/appe.2001.0427. [DOI] [PubMed] [Google Scholar]
- Birch LL, Fisher JO. Development of eating behaviors among children and adolescents. Pediatrics. 1998;101:539–549. [PubMed] [Google Scholar]
- Johnson SL, Birch LL. Parents' and children's adiposity and eating style. Pediatrics. 1994;94:653–661. [PubMed] [Google Scholar]
- Hughes SO, Power TG, Orlet Fisher J, Mueller S, Nicklas TA. Revisiting a neglected construct: parenting styles in a child-feeding context. Appetite. 2005;44:83–92. doi: 10.1016/j.appet.2004.08.007. [DOI] [PubMed] [Google Scholar]
- Spruijt-Metz D, Li C, Cohen E, Birch L, Goran M. Longitudinal influence of mother's child-feeding practices on adiposity in children. J Pediatr. 2006;148:314–320. doi: 10.1016/j.jpeds.2005.10.035. [DOI] [PubMed] [Google Scholar]
- Kroller K, Warschburger P. Associations between maternal feeding style and food intake of children with a higher risk for overweight. Appetite. 2008;51:166–172. doi: 10.1016/j.appet.2008.01.012. [DOI] [PubMed] [Google Scholar]
- Mulder C, Kain J, Uauy R, Seidell JC. Maternal attitudes and child-feeding practices: relationship with the BMI of Chilean children. Nutr J. 2009;8:37. doi: 10.1186/1475-2891-8-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hart CN, Raynor HA, Jelalian E, Drotar D. The association of maternal food intake and infants' and toddlers' food intake. Child Care Health Dev. 2010;36:396–403. doi: 10.1111/j.1365-2214.2010.01072.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Topham GL, Page MC, Hubbs-Tait L, Rutledge JM, Kennedy TS, Shriver L, et al. Maternal depression and socio-economic status moderate the parenting style/child obesity association. Public Health Nutr. 2010;13:1237–1244. doi: 10.1017/S1368980009992163. [DOI] [PubMed] [Google Scholar]
- Powers SW, Chamberlin LA, van Schaick KB, Sherman SN, Whitaker RC. Maternal feeding strategies, child eating behaviors, and child BMI in low-income African-American preschoolers. Obesity (Silver Spring) 2006;14:2026–2033. doi: 10.1038/oby.2006.237. [DOI] [PubMed] [Google Scholar]