Abstract
Fractures of the mandible occur with a greater frequency in the elderly. This study reports three cases of edentulous atrophic mandible fracture in elderly patients treated with open reduction technique. Three patients who presented with edentulous atrophic mandible fractures underwent surgical management using open reduction and internal fixation. After treatment, clinical evaluations and postoperative complications were examined with postoperative x-ray. Patients were followed with clinical and radiographic examinations. In the postoperative clinical evaluation, two male patients healed well, but one female patient complained of pain and swelling. In radiographic examinations, no union delay or lack of fusion was observed in the edentulous area. Open reduction technique is a viable treatment option for the edentulous atrophic mandible fractures in geriatric patients.
Keywords: Aged, Edentulous jaw, Mandibular fractures, Mandibular reconstruction, Bone plates
Introduction
The Korea Statistics Bureau notes that people older than 65 years represent 12.2% of the Korean population [1]. They predict that by 2050 the geriatric population will exceed 37%.
Trauma etiologies include motor vehicle trauma, falls, and assaults [2].
The incidence rate of maxillofacial trauma is increasing in the elderly, among which mandible fractures appear with a greater frequency [3].
Old age has long been considered a risk factor for poor outcomes following trauma. The elderly often have co-morbid illness. Co-morbid diseases, most commonly high blood pressure, diabetes mellitus, stroke, or dementia, limit their functional capacity to endure the stress of surgery and postoperative recovery. The elderly also have delayed bone healing with a compromised blood supply.
As one ages, loss of teeth and decreased vascularity contribute to the atrophy of residual alveolar bone, decreasing the strength of the mandible and creating a mandible more prone to fracture [4]. In addition, alveolar bone resorption and the loss of connective tissues around nerves allow the neurovascular surfaces to be more easily damaged [5]. The decreased vascular supply in the mandible coupled with reduced bone volume can compromise bony healing in the elderly patients.
Treatment of fractures can be more difficult because of partial or complete edentulism [6].
Luhr et al. [7] developed a classification for atrophic mandible fractures based on bone height at the fracture site. Luhr describe the atrophic mandible as having a vertical height <20 mm. He further classified them as follows: class I, 16∼20 mm; class II, 11∼15 mm; class III, ≤10 mm.
The techniques of edentulous atrophic mandible fracture management are by closed reduction (CR), open reduction/internal fixation, or both. Conservative treatments such as Gunning splints and external pin fixation have been proposed to manage edentulous atrophic mandible fractures due to weakened systemic condition of the elderly and low technical skills in the plate system. However, advances in anesthetic technique decrease the risk of the surgery in the elderly. Also, the technology of plate systems is remarkably developed. Recent open reduction techniques have an important role in edentulous atrophic mandible fracture treatment.
These reports present three cases of edentulous atrophic mandible fracture in older patients treated with open reduction technique. Two patients are treated with the two miniplates method; a third patient is managed with a reconstruction plate and miniplate technique.
Case Report
1. Case study 1
A 68-year-old male came to the emergency room (ER) of Haeundae Paik Hospital after a fall in the bathroom. He suffered from pain in the left chin area. Radiographs showed an atrophic mandible with left body fracture (Fig. 1). The alveolar bone height was 12-mm in the fracture area.
Fig. 1.
Preoperative panoramic x-ray depicting mandible fracture of left body portion.
The medical history included hypertension, diabetes, chronic obstructive pulmonary disease. To assess feasibility of general anesthesia, we consulted with cardiology, endocrinology, and pulmonology. The consensus was that risk was low, and the anesthesiologist agreed with operation under general anesthesia.
During the operation, the open reduction and internal fixation (ORIF) was achieved through extraoral access. Internal fixation with a 2.0-mm 6-hole miniplate and a 2.0-mm 4-hole miniplate were applied. This was a double miniplate method for load-sharing.
The patient recovered well from the surgical procedure. Postoperatively, there were no complaints about pain or signs of infection. The postoperative panoramic radiograph revealed a good plate position (Fig. 2). At the four month visit, the surgical site was healed. The radiographic examination confirmed the formation of a bone callus.
Fig. 2.
Postoperative panoramic x-ray. Note plate adaptation. Fracture reduction was adequate.
2. Case study 2
A 76-year-old male visited the ER after a motorcycle accident. He suffered from pain in his left cheek and right side of the chin. Radiographs showed an atrophic mandible with left ramus and right body fractures (Fig. 3). The alveolar bone height in the right body was 20 mm in the fracture area.
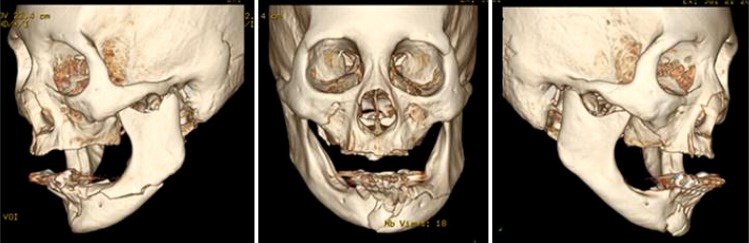
Fig. 3.
Preoperative 3-dimensional computed tomography images of mandible fracture of left subcondyle and right body portion.
The medical history included cerebral infarction.
During the operation, the patient was treated via extraoral incisions. The fracture segments on right body were fixed with a 2.0-mm 6-hole miniplate and a 2.0-mm 4-hole miniplate. The fracture segments on left ramus were fixed with a 2.0-mm 4-hole miniplate.
The postoperative mandible x-rays revealed the plates to be in a favorable position (Fig. 4). At the one month visit, the patient had healed in the right body reduction area, but developed a displacement in the left ramus reduction area on the orthopantomogram. The patient was instructed to chew with less effort. The nonunion site showed bony consolidation without any further treatment after three to five months. At the six month visit, a clinical examination showed stable fracture segments. The patient was satisfied and had good function without complications.
Fig. 4.
Postoperative mandible plain x-ray (A: right oblique, B: antero-posterior, C: left oblique) of good reduction and stabilization.
3. Case study 3
A 77-year-old female was referred to the ER after a fall. She suffered from pain in her chin and both preauricular areas. Radiographs showed a mandible with from symphysis to left body comminuted fracture, and 3-dimensional computed tomography images demonstrated both condyle neck fractures associated with facial fractures (Fig. 5). The alveolar bone height in the left body was 20 mm in the fracture area.
Fig. 5.
Preoperative 3-dimensional computed tomography images of mandible fracture of symphysis, left body portion and both condyle neck.
The medical history included Parkinson’s disease.
The surgical approach was through a transcervical approach. A 2.3-mm reconstruction plate and a 2.0-mm 4-hole miniplate were applied in the fracture segments. The condyle neck fractures were treated nonsurgically as a conservative treatment. A facial bandage was used to limit mandibular movement.
Postoperatively, there were complaints about pain and swelling. Although she was mentally drowsy, there were no signs of infection. The postoperative mandible x-rays revealed an adequate position of the plates (Fig. 6). At the one month visit, there were no complaints about pain and swelling, but she was losing her vigor due to a diarrhea and fever. Uncomplicated bony union was achieved in the symphysis and left body fracture area. However, the patient died two months postoperatively from a pseudo-membranous colitis.
Fig. 6.
Postoperative mandible plain x-ray (A: right oblique, B: antero-posterior, C: left oblique). 2.3-mm plate and 2.0-mm plate provide prolonged stability.
Discussion
Different opinions exist regarding the approach for proper treatment of the edentulous mandible fracture. Edentulous mandible fracture reduction methods are CR, ORIF, or both.
Many maxilla and mandible fractures are treated with CR techniques. Concurrent medical conditions in the elderly may necessitate secondary repair of facial injuries, so conservative management must always be considered.
Ideally, CR technique is best accomplished with a mandible that is at least 30 mm in height [6]. It is more difficult to control atrophic segments when mandible height is ≤10 mm.
The CR of an edentulous mandible is accomplished with a pre-existing denture. The use of the patient’s denture allows for immobilization. If no denture is available, a Gunning splint is manufactured. The full denture or Gunning splint is fixed to the mandible with circum-mandibular wires.
The advantage of CR technique is that no surgical incision is required. Therefore, the periosteal blood supply to the bone can be preserved. If there is a medical contra-indication to ORIF, this technique is helpful.
There are disadvantages to CR technique of the mandible. The circum-mandibular technique must be done carefully since the mental foramen is often on the superior border of the mandible. It is difficult for a patient to get sufficient nutrition in the CR with intermaxillary fixation. In addition, the intermaxillary fixation can cause airway obstruction, and lead to problems in the temporomandibular joint. The length of intermaxillary fixation time (four to six weeks) can make circum-mandibular wires loosen. Intermaxillary fixation will interfere with the oral medication intake, and elderly patients often take many. Often CR techniques do not fully reduce fractured segments, and immobilization is incomplete.
External pin fixation, or Joe Hall Morris Appliance/Biphasic Pin Device, is another CR management technique. The biphasic pin fixation technique is useful with a comminuted fracture. The external pins are placed on either side of the fracture site, and after fracture reduction, an external appliance is placed to retain the bone segments in the correct position.
The advantages include the ability to stabilize fractured segments while eliminating the necessity for intermaxillary fixation. The disadvantages are the need to drill bone holes. The drilling of holes for external pin placement needs to be away from the inferior alveolar canal. To maintain a proper reduction can be challenging for unstable fractures. As a general rule, external pins are able to provide stabilization of mandibles of at least 10 mm of bone height.
Open reduction techniques are currently important in edentulous atrophic mandible fracture treatment. The indications include continuity defects and unstable fractured segments. An experimental study shows that a supraperiosteal dissection entails little risk of irreparable injury to the vascularity of the surrounding bone [8].
Surgical treatment can be either intraorally or extraorally. Plates can be removed after a time, differing depending upon the length reduced.
The advantages of open reduction are direct visualization and immobilization of fractured segments. Therefore, it is possible to get excellent reduction. This is important with fractures in areas with decreased healing ability. Other advantages include immediate function and nutrition. This is significant because most elderly feel that function is more important than aesthetics.
The disadvantage with open reduction technique is the surgical insult and the frequent need for general anesthesia. It poses a greater challenge to the patient’s cardiac, pulmonary, and wound healing abilities. Prosthodontic treatment after open reduction is difficult in the presence of rigid fixation plates and screws. The plates and screws disturb the placement of dental implants or the adaptation of the denture border.
The treatment of the fractured edentulous atrophic mandible is a controversial issue. The nub of the dispute is focused on the considerations over underlying systemic disease in the elderly patient resulting in increased complications, the diminished vascular supply and insufficient bone buttressing of the atrophic mandible [2].
Comorbid disease makes it difficult to proceed with open reduction surgery. Undoubtedly, the elderly for whom general anesthesia is inappropriate need CR via preexisting dentures or Gunning splints. Poor blood supply of the fractured bone and the incomplete buttressing at the fracture site pose further challenges for surgery. Efforts to obtain open reduction need adequate surgical exposure, which can weaken the bloody supply of surrounding bone. On the other hand, sustaining the blood supply without surgical approach compromises the capability to attain rigid immobilization.
Historically, conservative management such as Gunning splints, external pin fixation, and soft diet were recommended in the treatment of edentulous atrophic mandible fracture. In 1975, Bradley [9] stated that the body area of the edentulous atrophic mandible was mainly reliant on a periosteal blood supply. This understanding favored the use of CR techniques. Even though Gunning splints or external pin fixation have often been successful, inadequate reductions, fibrous unions, and nonunions were not uncommon.
Developments in anesthetic technique have lowered the risk of open reduction surgery in the elderly. Multiple studies demonstrate that open reduction does not increase the risk of nonunion in atrophic fractures [9–11]. Many maxillofacial surgeons recommend open reduction of edentulous atrophic mandible fractures as better choice to closed techniques.
Wittwer et al. [10] suggests that the management of atrophic mandible fractures should be based on the degree of atrophy. They found that Luhr Class I and II edentulous atrophic mandibles had a higher complication rate. They concluded that more rigid fixation is necessary in mandibles with atrophy less than 15 mm bone height.
Internal fixation techniques of obtaining excellent reduction through a more rigid plate are more popular despite the requirement of more periosteal stripping [12].
There is controversy about which plate system is most stable for reduction of the atrophic mandible fracture [13]. Incomplete buttressing resulting from decreased bone height is central to this question [14]. Choi et al. [13] evaluated the stability of miniplates in varying degrees of atrophic mandible in bovine ribs. They recommended the use of two miniplates with open reduction technique for appropriate buttressing at the fracture site of the edentulous atrophic mandible. Sikes et al. [15] compared miniplates and reconstruction plates in a bovine rib model. They concluded that the atrophic mandible fracture may be better treated with reconstruction plates.
Some maxillofacial surgeons use a large reconstruction plate with screws. This technique requires a large incision and a large area of dissection. In this case, there is a smaller contact area between the periosteum and bone because of the large reconstruction plate. The larger screws increase the possibility for inferior alveolar nerve injury and additional fracture around the screw holes.
Current recommendations include using a small reconstruction plate. The use of 2.4-mm reconstruction plates and bicortical screws has gained acceptance as a fixation system in the edentulous atrophic mandible fracture [12]. The 2.0-mm reconstruction plate is a good option in fixating the edentulous atrophic mandible fracture [11], providing excellent stability and increased strength. Ellis and Price [16] proposed a reconstruction plate with six holes and three bicortical screws on each side of the fracture. They recommended placing the reconstruction plate at the inferior border of the mandible for rigid fixation. The advantage of a small reconstruction plate is improvement of the jaw contour and ease of incision closure.
Intraoral versus extraoral approach to open reduction offer differing considerations, depending on the patient’s situation and the surgeon’s preference. Intraoral open reduction offers a simple, direct approach [17]. This technique makes it easy to dissect and close. Disadvantages of the intraoral approach include unintended injury of the mental nerve because the mental foramen often lies close to the alveolar ridge crest in an atrophic mandible. In addition, there is contamination that results from saliva.
An extraoral approach facilitates handling and maintaining the correct position of the fractured segments during fixation and makes it easy to adapt the plates. Disadvantages include a facial scar, although the scar can be often hidden in a facial rhytid in the elderly. Another important disadvantage when using extraoral access is the risk of injury to the facial nerve.
There are several options for the most appropriate form of treatment, whether closed or open technique, the use of miniplates or reconstruction plates, intraoral or extraoral approach. Advanced age is a surgical risk for patients with pathologic conditions. However, chronologic age should not be considered a contraindication to an anesthetic and invasive surgery [5]. Identifying co-morbid illness is very important for decreasing morbidity and mortality in older trauma patients.
Open reduction technique can be a viable treatment option for the edentulous atrophic mandible fractures in geriatric patients. As the technology of plate systems is developed, the dependence on the open reduction technique with the use of rigid plate has increased.
Cautious placement of plates and screws away from the inferior alveolar nerve is recommended when open reduction technique is used. In addition, there is possibility of injuring facial nerve.
References
- 1. Senior Citizen Statistics, 2013 [Internet]. Daejeon: Korea Statistics; [cited 2014 Mar]. Available from: http://kostat.go.kr/portal/korea/kor_nw/2/6/1/index.board?bmode=download&bSeq=&aSeq=308688&ord=3.
- 2.Goldschmidt MJ, Castiglione CL, Assael LA, Litt MD. Craniomaxillofacial trauma in the elderly. J Oral Maxillofac Surg. 1995;53:1145–9. doi: 10.1016/0278-2391(95)90620-7. [DOI] [PubMed] [Google Scholar]
- 3.Halpern LR, Flynn TR. Oral and maxillofacial trauma in the geriatric patient. In: Fonseca RJ, Walker RV, Betts NJ, Barber HD, Powers MP, editors. Oral and maxillofacial trauma. 3rd ed. Vol. 2. St Louis: Saunders Elsevier; 2005. pp. 1001–5. [Google Scholar]
- 4.Barber HD. Conservative management of the fractured atrophic edentulous mandible. J Oral Maxillofac Surg. 2001;59:789–91. doi: 10.1053/joms.2001.24734. [DOI] [PubMed] [Google Scholar]
- 5.Sidal T, Curtis DA. Fractures of the mandible in the aging population. Spec Care Dentist. 2006;26:145–9. doi: 10.1111/j.1754-4505.2006.tb01715.x. [DOI] [PubMed] [Google Scholar]
- 6.Ruggiero SL, Schneider RE. Treatment of maxillofacial fractures in the geriatric population. In: Marciani RD, Carlson ER, Braun TW, editors. Oral and maxillofacial surgery. 2nd ed. Vol. 2. St Louis: Saunders Elsevier; 2009. pp. 374–94. [Google Scholar]
- 7.Luhr HG, Reidick T, Merten HA. Results of treatment of fractures of the atrophic edentulous mandible by compression plating: a retrospective evaluation of 84 consecutive cases. J Oral Maxillofac Surg. 1996;54:250–4. doi: 10.1016/s0278-2391(96)90733-8. [DOI] [PubMed] [Google Scholar]
- 8.Fonseca RJ, editor. Oral and maxillofacial surgery. Philadelphia: WB Saunders; 1997. [Google Scholar]
- 9.Bradley JC. A radiological investigation into the age changes of the inferior dental artery. Br J Oral Surg. 1975;13:82–90. doi: 10.1016/0007-117x(75)90027-x. [DOI] [PubMed] [Google Scholar]
- 10.Wittwer G, Adeyemo WL, Turhani D, Ploder O. Treatment of atrophic mandibular fractures based on the degree of atrophy--experience with different plating systems: a retrospective study. J Oral Maxillofac Surg. 2006;64:230–4. doi: 10.1016/j.joms.2005.10.025. [DOI] [PubMed] [Google Scholar]
- 11.Farwell DG, Kezirian EJ, Heydt JL, Yueh B, Futran ND. Efficacy of small reconstruction plates in vascularized bone graft mandibular reconstruction. Head Neck. 2006;28:573–9. doi: 10.1002/hed.20455. [DOI] [PubMed] [Google Scholar]
- 12.Kunz C, Hammer B, Prein J. Fractures of the edentulous atrophic mandible. Fracture management and complications. Mund Kiefer Gesichtschir. 2001;5:227–32. doi: 10.1007/s100060100304. [DOI] [PubMed] [Google Scholar]
- 13.Choi BH, Huh JY, Suh CH, Kim KN. An in vitro evaluation of miniplate fixation techniques for fractures of the atrophic edentulous mandible. Int J Oral Maxillofac Surg. 2005;34:174–7. doi: 10.1016/j.ijom.2003.10.024. [DOI] [PubMed] [Google Scholar]
- 14.Marciani RD. Invasive management of the fractured atrophic edentulous mandible. J Oral Maxillofac Surg. 2001;59:792–5. doi: 10.1053/joms.2001.24736. [DOI] [PubMed] [Google Scholar]
- 15.Sikes JW, Jr, Smith BR, Mukherjee DP. An in vitro study of the effect of bony buttressing on fixation strength of a fractured atrophic edentulous mandible model. J Oral Maxillofac Surg. 2000;58:56–61. doi: 10.1016/s0278-2391(00)80017-8. [DOI] [PubMed] [Google Scholar]
- 16.Ellis E, 3rd, Price C. Treatment protocol for fractures of the atrophic mandible. J Oral Maxillofac Surg. 2008;66:421–35. doi: 10.1016/j.joms.2007.08.042. [DOI] [PubMed] [Google Scholar]
- 17.Klein JC. Intraoral open reduction. Arch Otolaryngol. 1977;103:645–7. doi: 10.1001/archotol.1977.00780280045005. [DOI] [PubMed] [Google Scholar]