Abstract
Purpose:
This study compares the prognosis (the survival rate and marginal bone loss) of resorbable blasting media (RBM) surface implants and sandblasting with large-grit and acid-etching (SLA) surface implants in the early loading.
Methods:
This study targeted 123 patients treated by implants installation from January 2008 to March 2010. The loading was initiated in the maxilla within three to four months and in the mandible within one to two months. The types of restoration were single crown and fixed partial prosthesis. Those functioned over one year. The implants were classified by the surface of implants as Group 1: RBM surface (GS III; OSSTEM, Busan, Korea) and, Group 2: SLA surface (Superline; Dentium, Seoul, Korea). The groups were categorized by maxilla and mandible and compared by survival rate, marginal bone loss through clinical records evaluation, and radiographic measurements.
Results:
The marginal bone loss in the maxilla was 0.14±0.34 mm (Group 1) and 0.30±0.37 mm (Group 2), a statistically significant difference (P <0.05). In the mandible those were 0.28±0.54 mm (Group 1) and 0.20±0.33 mm (Group 2), not significant (P >0.05). There was no significant difference of marginal bone loss between maxilla and mandible by groups. During observation there was no implant failure, a survival rate of 100%.
Conclusion:
Both surfaces showed an excellent survival rate, and the marginal bone loss was not substantial.
Keywords: Early dental implant loading, Resorbable blasting media, Sandblasting with large-grit and acid-etching
Introduction
Obtaining excellent primary stability with an absence of micromotion during secondary bone healing is very important for successful implant placement[1]. Early implant loading was thought to impede the osseointegration of implants, so the delayed loading technique (gradual loading after a three to six month wait), is used[2,3]. Despite this conventional wisdom, there have been several recent studies on the stability of immediate or early loading. These studies report success rates up to 88% to 100%, and a tendency toward decreasing postsurgical treatment period[4–9].
In the third International Team for Implantology (ITI) consensus conference, immediate loading was defined as the insertion of a prosthesis within 48 hours of implant placement, which is loaded by biting with the opposite dentition. Early loading was defined as the initiation of function between 48 hours and 3 months after implant placement[10]. However, because of improvements in the implant surface treatment process, the loading period tends to be shortened; there is a trend of early loading within two months in the mandible and within four months in the maxilla.
Implant surface treatment is important for success, and several surface treatments have been developed. The resorbable blasting media (RBM) surface has been the subject of several reports. In 2003, Mazor and Cohen[11] reported that for single crowns observed over 48 months, the marginal bone loss was less than 1 mm, and the success rate was 100%. Sandblasting with large-grit and acid-etching (SLA) surfaces showed stronger bony union in comparison with the machined surface[12,13]. The topography of the implant surface has important effects on bone response[14]. In early loading cases particularly, implant surface treatment is important for implant success.
This study compared the survival rate and marginal bone loss of the early loading of RBM surface implants and that of SLA surface implants.
Materials and Methods
The study included patients who were loaded three to four months after implant placement in the maxilla and one to two months after implant placement in the mandible at the Bundang Seoul National University Dental Clinic from January 2008 to March 2010. The informed consents for this study were explained to the patients before treatment. This study was approved by Seoul National University Bundang Hospital Institutional Review Board (IRB: B-0810-062-010).
Smoking and oral habits were not considered, and patients with controllable systemic diseases were included as study subjects. The type of maxillary prosthesis was either a single crown or fixed partial denture that functioned for over a year.
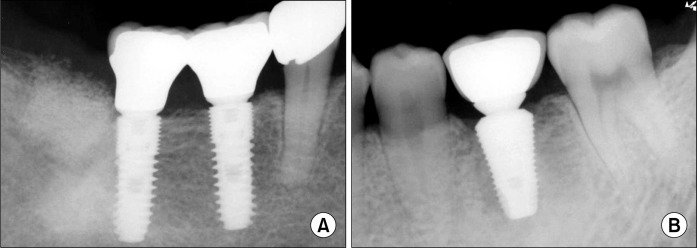
The subjects were divided by implant surface treatment into Group 1: RBM surface (GS III; OSSTEM, Busan, Korea) and Group 2: SLA surface (Superline; Dentium, Seoul, Korea) (Fig. 1). Both the GS III and Superline system were of the internal hex and tapered body type. The mean observation period was 19.05±7.13 months for the maxilla and 18.06±7.88 months for the mandible. During the first year post-treatment, exams was performed at three month intervals, then lengthened to six month intervals thereafter.
Fig. 1.
Periapical views of implants. (A) Group 1: Resorbable blasting media surface implant (GS III). (B) Group 2: Sandblasting with large-grit and acid-etching surface implant (Superline).
Analysis of the medical records and measurements on radiographs, the implant survival rate and the marginal bone loss between the maxilla and the mandible were evaluated along with the implant system.
The marginal bone loss was measured by comparing the marginal bone level around the implant fixture on the periapical radiograph taken at initial implant installation with those of the final follow-up radiograph. For the marginal bone loss, bone height from the implant shoulder to the most distinct radio-opaque area in the mesiodistal alveolar ridge was measured vertically on the radiograph taken by the parallel imaging method and the average was calculated by obtaining the mesiodistal height. Considering the magnification by measuring the height of fixture in the radiograph, the marginal bone loss was calculated. In each group, the gender distribution, the distribution of the length of implant used, and the diameter were examined. In addition, the survival rate of implants, success rate, and marginal bone loss of the groups were compared by devided into groups of maxilla and mandible. In addition, the survival rate and the marginal bone loss in the maxilla and the mandible of each group were compared.
The survival rate and success rate of implants for the two groups were compared by the Pearson’s chi-square test. The mean bone resorption level of the two groups was compared by Student’s t-test. The SPSS program version 12.0 (SPSS Inc., Chicago, IL, USA) was used for statistical analysis. Null hypotheses of no difference were rejected if P-values were less than 0.05, or, equivalently, if the 95% confidence intervals of risk point estimates excluded 1.
The criteria for implant success were as follows: (1) no detection of mobility by clinical test; (2) the absence of radiolucency around implants; (3) vertical bone defects during the first year after prosthesis restoration less than 1.5 mm bone loss and less than 0.2 mm of annual bone loss 1 year after function; and (4) the absence of continuous and irreversible symptoms, such as pain, infection, and neurological problems. Using these criteria, the success of implant was evaluated in this study[14].
Results
The average loading times after placement of the final prosthesis in the maxilla were 17.37±5.32 months in Group 1 and 16.6±17.32 months in Group 2. Averages for the mandible were 17.76±5.82 months in Group 1, and 15.31±9.88 months in Group 2. The number of implants in the maxilla and the mandible of each group and the gender distribution of the patients are shown in Table 1, 2. The mean age of the subjects for the evaluation of the maxilla was 54.29±12.64 years, and the mean age of the subjects for the evaluation of the mandible was 54.92±13.00 years. The distribution of the length and diameter of the implants in each group is shown in Table 3. In the maxilla, the marginal bone loss around implants was 0.14±0.34 mm in Group 1 and 0.30±0.37 mm in Group 2, and a statistically significant difference between groups was found (P <0.05). In the mandible, the marginal bone loss was 0.29±0.54 mm in Group 1 and 0.20±0.34 mm in Group 2, no significant difference. In each group, there was no significant difference of the marginal bone loss between the maxilla and mandible (Table 4). There was a 100% survival rate of the implants in both groups. For the maxilla, the success rate was 98% for Group 1 and 97% for Group 2. For the mandible, the success rate was 97% in Group 1 and 100% in Group 2 (Table 5), not a significant difference in the survival rate and success rate.
Table 1.
Distribution of implant in Group 1 (GS III) and Group 2 (Superline)
| Maxilla | Mandible | |||
|---|---|---|---|---|
|
|
|
|||
| Group 1 | Group 2 | Group 1 | Group 2 | |
| Anterior (n) | 14 | 0 | 2 | 0 |
| Premolar (n) | 13 | 6 | 14 | 1 |
| Molar (n) | 27 | 32 | 52 | 43 |
| Total (n) | 54 | 38 | 68 | 44 |
Table 2.
Distribution of patients in maxilla and mandible groups in Group 1 (GS III) and Group 2 (Superline)
| Maxilla | Mandible | |||
|---|---|---|---|---|
|
|
|
|||
| Group 1 | Group 2 | Group 1 | Group 2 | |
| Female (n) | 13 | 11 | 15 | 14 |
| Male (n) | 16 | 15 | 15 | 24 |
| Total (n) | 29 | 26 | 30 | 38 |
Table 3.
Distribution of implant length and width in Group 1 (GS III) and Group 2 (Superline)
| Group 1 | Group 2 | |||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||||||||||||||||
| Length (mm) | Width (mm) | Length (mm) | Width (mm) | |||||||||||||||||||||
|
|
|
|
|
|||||||||||||||||||||
| 7.0 | 8.5 | 10.0 | 11.5 | 12.0 | 13.0 | Total | 3.5 | 4.0 | 4.5 | 5.0 | Total | 8.0 | 10.0 | 12.0 | 14.0 | Total | 3.4 | 3.8 | 4.3 | 4.8 | 5.8 | 6.0 | Total | |
| Maxilla (n) | 0 | 2 | 12 | 17 | 1 | 22 | 54 | 9 | 17 | 4 | 24 | 54 | 6 | 14 | 17 | 1 | 38 | 1 | 4 | 5 | 25 | 3 | 0 | 38 |
| Mandible (n) | 10 | 18 | 19 | 21 | 0 | 0 | 68 | 2 | 17 | 17 | 32 | 68 | 17 | 26 | 1 | 0 | 44 | 0 | 1 | 0 | 40 | 2 | 1 | 44 |
Table 4.
Comparison of marginal bone loss between groups/maxilla and mandible in each group
Values are presented as mean±standard deviation. -: not significant.
Student’s t-test.
P <0.05.
Table 5.
Success rate in each group
| Success rate | GS III | Superline | Siga |
|---|---|---|---|
| Maxilla (%) | 98 | 97 | - |
| Mandible (%) | 97 | 100 | - |
-: not significant.
Pearson’s chi-square test. P <0.05.
In Group 1, one case of maxilla and two cases of mandible were excluded from the successful cases. In the maxilla cases, implants were placed in the premolar area, and bone grafts were not performed. One year after function, 1.5 mm of marginal bone loss was observed. All mandible cases were restored with a fixed partial prosthesis at molar area. One year after function, 1.9 mm of marginal bone loss was observed in Group 1 and 1.5 mm in Group 2. In Group 2, a case in which the maxilla was restored by a fixed partial prosthesis lost 1.7 mm of bone one year after treatment. The case was therefore excluded from the successful cases. Biological and mechanical complications, such as infection after surgery or function and the destruction of the prosthesis did not occur.
Discussion
Unlike the conventional loading procedure in which loading occurs three to six months after implant placement for osseointegration, the immediate/early loading procedure has the advantage of shortening treatment periods by reducing the healing time after implant placement. During initial bone healing, the duration of removable prosthesis placement and the edentulous period is shortened, and the function, comfort, and stability of the implants for the patients increased. Bergkvist et al.[6] reported the marginal bone loss of fixed prostheses supported by ITI SLA screw type implants and placed within 24 hours in 28 patients with edentulous maxilla. Eight months after function, there was an average marginal bone loss of 3.2 mm, and the survival rate was 98%. Nordin et al.[7] reported on SLA Straumann implants of 116 patients that were placed in maxillae and restored with a fixed implant-supported prosthesis within 10 to 14 days. The patients were observed for two to three years, and achieved a 98% success rate. Roccuzzo et al.[8] reported that in over five years of observation, SLA implants that were loaded early were reliable at around six weeks in both the maxilla and mandible. In both groups in our study, a 100% implant survival rate was seen.
Histological analysis of implants placed in humans after four and eight weeks of implant placement, with or without immediate loading, found high bone-to-implant contact percentages with mineralized tissues in the interface, and no impairment of early bone healing[15].
Marginal bone loss around implants is an important clinical marker for the success of implants because gradual marginal bone loss may lead to the failure of implants by ultimately destroying the osseointegration of implants to the bone. Evaluation of marginal bone loss around implants one year after function, found that the marginal bone loss of the group with early loading was statistically significantly lower than that of the group with delayed loading[16]. Esposito et al.[16] compared early, immediate, and conventional loading after implant placement, and did not observe statistically significant clinical differences. The bone quality at the time of implant placement and the primary stability were the most important factors. When rough surface implants were placed with vertical augmentation using expanded polytetrafluoroethylene membranes and early loading was performed, the marginal bone loss was 0.9 mm, one year after function and 0.98 mm, 2 year after function and stable results were shown[17].
Lemmerman and Lemmerman[18] observed no significant differences in survival rates in 1,003 implants with different surface treatments. In addition, for successful immediate loading, initial implant stability, bone quality, and patient compliance had major effects[19].
In the maxilla, after the placement of the Straumann implant, a fixed implant-supported prosthesis was placed within 10 to 14 days, and the marginal bone loss was 0.8±1.2 mm. Makkonen et al.[20] in a five year retrospective study of implants with cervical microthread, observed an average marginal bone loss of 0.48 mm, and a survival rate at 98.7%. Those results meant successful prognosis. The marginal bone loss of the structure with or without a machined collar in the neck of implants with a chemically modified SLA surface was evaluated one year after function. The marginal bone loss of the structure with the machined collar averaged 1.0 mm, and the structure without the machined collar showed an average of 1.1 mm bone gain[21]. Implants with a microthread neck resist marginal bone loss more than implants with a polished neck during the first healing period[22].
Blasting methods are advantageous because surface area increases as particles are blasted on the surface, the degree of osseointegration increases due to the concavoconvex effect, and cell reactions on the rough surface are activated. Additionally, concerning removal torques and the bone contact rate, RBM surface implants with an appropriately rough surface yielded better results than machined surface implants. Wennerberg and Albrektsson[13] reported that a surface roughness of Ra (1.3∼1.5 μm) is optimal for osseointegration. The SLA surface is a moderately rough surface, and compared to a machined surface, it showed stronger osseointegration with the bone and even more than the titanium plasma sprayed surface in several reports[23]. The survival rate following early loading of implants with an SLA surface and 6 mm in length was 95% for two years, with moderate marginal bone loss of 0.23±0.33 mm one year after function and 0.21±0.39 mm after two years[24].
The Superline implants used in this study were of the SLA surface and tapered type. These are designed to be placed in cases with poor bone quality or in cases with a bone graft in the maxillary sinus. They have a double-threaded design and an internal hex structure. In the GS III implants, the RBM surface was selected, the surface roughness was Ra 1.2 to 1.8 μm, the structure was the internal hex connection with a tapered body and had microthreads in the fixture top. In this study, in both surface-type implants, the crestal bone level was maintained stably after early loading. The implants were evaluated according to the success criteria suggested by Albrektsson et al.[25], and the success rate was 97% to 100% in the early loading groups, both in the maxilla and mandible. There was no statistically significant difference between the groups in the crestal bone loss.
The limitations of this retrospective study are that the deviation of cases in the anterior tooth and posterior tooth was large, the length and diameter of implants were diverse, and the variables of bone mass and bone quality were not considered. Despite such limitations, the early loading protocol, in which the final prosthesis was placed at 3 to 4 months in the maxilla and 1 to 2 months in the mandible, yielded stable clinical outcomes.
Conclusion
When the maxilla and the mandible were restored with a single crown and a partial fixed prosthesis and when the early loading procedure was performed, survival rates for both the RBM surface and SLA surface were excellent, and the marginal bone loss was not large. If early loading is performed for the appropriate cases, results can be excellent.
References
- 1.Albrektsson T, Brånemark PI, Hansson HA, Lindström J. Osseointegrated titanium implants. Requirements for ensuring a long-lasting, direct bone-to-implant anchorage in man. Acta Orthop Scand. 1981;52:155–70. doi: 10.3109/17453678108991776. [DOI] [PubMed] [Google Scholar]
- 2.Babbush CA. Titanium plasma spray screw implant system for reconstruction of the edentulous mandible. Dent Clin North Am. 1986;30:117–31. [PubMed] [Google Scholar]
- 3.Brånemark PI, Hansson BO, Adell R, et al. Osseointegrated implants in the treatment of the edentulous jaw. Experience from a 10-year period. Scand J Plast Reconstr Surg Suppl. 1977;16:1–132. [PubMed] [Google Scholar]
- 4.Lee SY, Kim YK, Yun PY, Yi YJ, Yeo IS. Retrospective Clinical study of immediate or early loading of implants. J Korean Dent Assoc. 2010;48:119–26. [Google Scholar]
- 5.Kwon MJ, Yeo IS, Kim YK, Yi YJ, Yang JH. Use of separate single-tooth implant restorations to replace two or more consecutive posterior teeth: a prospective cohort study for up to 1 year. J Adv Prosthodont. 2010;2:54–7. doi: 10.4047/jap.2010.2.2.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bergkvist G, Sahlholm S, Karlsson U, Nilner K, Lindh C. Immediately loaded implants supporting fixed prostheses in the edentulous maxilla: a preliminary clinical and radiologic report. Int J Oral Maxillofac Implants. 2005;20:399–405. [PubMed] [Google Scholar]
- 7.Nordin T, Graf J, Frykholm A, Helldén L. Early functional loading of sand-blasted and acid-etched (SLA) Straumann implants following immediate placement in maxillary extraction sockets. Clinical and radiographic result. Clin Oral Implants Res. 2007;18:441–51. doi: 10.1111/j.1600-0501.2007.01387.x. [DOI] [PubMed] [Google Scholar]
- 8.Roccuzzo M, Aglietta M, Bunino M, Bonino L. Early loading of sandblasted and acid-etched implants: a randomized-controlled double-blind split-mouth study. Five-year results. Clin Oral Implants Res. 2008;19:148–52. doi: 10.1111/j.1600-0501.2007.01426.x. [DOI] [PubMed] [Google Scholar]
- 9.Van de Velde T, Collaert B, De Bruyn H. Immediate loading in the completely edentulous mandible: technical procedure and clinical results up to 3 years of functional loading. Clin Oral Implants Res. 2007;18:295–303. doi: 10.1111/j.1600-0501.2007.01340.x. [DOI] [PubMed] [Google Scholar]
- 10.Cochran DL, Morton D, Weber HP. Consensus statements and recommended clinical procedures regarding loading protocols for endosseous dental implants. Int J Oral Maxillofac Implants. 2004;19(Suppl):109–13. [PubMed] [Google Scholar]
- 11.Mazor Z, Cohen DK. Preliminary 3-dimensional surface texture measurement and early loading results with a micro-textured implant surface. Int J Oral Maxillofac Implants. 2003;18:729–38. [PubMed] [Google Scholar]
- 12.Hsu SH, Liu BS, Lin WH, Chiang HC, Huang SC, Cheng SS. Characterization and biocompatibility of a titanium dental implant with a laser irradiated and dual-acid etched surface. Biomed Mater Eng. 2007;17:53–68. [PubMed] [Google Scholar]
- 13.Wennerberg A, Albrektsson T. Effects of titanium surface topography on bone integration: a systematic review. Clin Oral Implants Res. 2009;20(Suppl 4):172–84. doi: 10.1111/j.1600-0501.2009.01775.x. [DOI] [PubMed] [Google Scholar]
- 14.Shalabi MM, Gortemaker A, Van’t Hof MA, Jansen JA, Creugers NH. Implant surface roughness and bone healing: a systematic review. J Dent Res. 2006;85:496–500. doi: 10.1177/154405910608500603. [DOI] [PubMed] [Google Scholar]
- 15.Degidi M, Piattelli A, Shibli JA, Perrotti V, Iezzi G. Bone formation around immediately loaded and submerged dental implants with a modified sandblasted and acid-etched surface after 4 and 8 weeks: a human histologic and histomorphometric analysis. Int J Oral Maxillofac Implants. 2009;24:896–901. [PubMed] [Google Scholar]
- 16.Esposito M, Grusovin MG, Willings M, Coulthard P, Worthington HV. The effectiveness of immediate, early, and conventional loading of dental implants: a Cochrane systematic review of randomized controlled clinical trials. Int J Oral Maxillofac Implants. 2007;22:893–904. [PubMed] [Google Scholar]
- 17.Canullo L, Sisti A. Early implant loading after vertical ridge augmentation (VRA) using e-PTFE titanium-reinforced membrane and nano-structured hydroxyapatite: 2-year prospective study. Eur J Oral Implantol. 2010;3:59–69. [PubMed] [Google Scholar]
- 18.Lemmerman KJ, Lemmerman NE. Osseointegrated dental implants in private practice: a long-term case series study. J Periodontol. 2005;76:310–9. doi: 10.1902/jop.2005.76.2.310. [DOI] [PubMed] [Google Scholar]
- 19.Gedrange T, Hietschold V, Mai R, Wolf P, Nicklisch M, Harzer W. An evaluation of resonance frequency analysis for the determination of the primary stability of orthodontic palatal implants. A study in human cadavers. Clin Oral Implants Res. 2005;16:425–31. doi: 10.1111/j.1600-0501.2005.01134.x. [DOI] [PubMed] [Google Scholar]
- 20.Makkonen TA, Holmberg S, Niemi L, Olsson C, Tammisalo T, Peltola J. A 5-year prospective clinical study of Astra Tech dental implants supporting fixed bridges or over-dentures in the edentulous mandible. Clin Oral Implants Res. 1997;8:469–75. doi: 10.1034/j.1600-0501.1997.080605.x. [DOI] [PubMed] [Google Scholar]
- 21.Valderrama P, Jones AA, Wilson TG, Jr, et al. Bone changes around early loaded chemically modified sandblasted and acid-etched surfaced implants with and without a machined collar: a radiographic and resonance frequency analysis in the canine mandible. Int J Oral Maxillofac Implants. 2010;25:548–57. [PubMed] [Google Scholar]
- 22.Bratu EA, Tandlich M, Shapira L. A rough surface implant neck with microthreads reduces the amount of marginal bone loss: a prospective clinical study. Clin Oral Implants Res. 2009;20:827–32. doi: 10.1111/j.1600-0501.2009.01730.x. [DOI] [PubMed] [Google Scholar]
- 23.Abrahamsson I, Berglundh T. Effects of different implant surfaces and designs on marginal bone-level alterations: a review. Clin Oral Implants Res. 2009;20(Suppl 4):207–15. doi: 10.1111/j.1600-0501.2009.01783.x. [DOI] [PubMed] [Google Scholar]
- 24.Rossi F, Ricci E, Marchetti C, Lang NP, Botticelli D. Early loading of single crowns supported by 6-mm-long implants with a moderately rough surface: a prospective 2-year follow-up cohort study. Clin Oral Implants Res. 2010;21:937–43. doi: 10.1111/j.1600-0501.2010.01942.x. [DOI] [PubMed] [Google Scholar]
- 25.Albrektsson T, Zarb G, Worthington P, Eriksson AR. The long-term efficacy of currently used dental implants: a review and proposed criteria of success. Int J Oral Maxillofac Implants. 1986;1:11–25. [PubMed] [Google Scholar]